Petroclival meningiomas Anatomic landmarks The clivus localization Part


- Slides: 15
Petroclival meningiomas
Anatomic landmarks • The clivus – localization: • Part of the skull base, behind the dorsum sellae. • The posterior end of the midline sphenoid bone and the neighboring anterior occipital bone (the basilar part of the occipital bone) together form the clivus. It is a bony slope heading oblique posteriorly on which the pons lies. Lateral to it you can find foramen lacerum, the entrance point of the internal carotid artery into the skull.

Dural insertion • Clival meningiomas: along the superior 2/3 of the midline of clivus • Petroclival meningiomas: along the 2/3 of the petro-clival junction, medial to the internal auditory meatus and posterior to the gasserian ganglion.
Clinical features • Epidemiology: affects predominantly middle-aged and older women; they develop insidiously. • Main complaints: ØCranial nerves palsies cerebellar and brainstem compression signs. (trigeminal nerve dysfunction: trigeminal neuralgia, facial pain, hyperesthesia or anesthesia; diplopia, hearing loss, vertigo, dysphonia, facial weakness, dysphagia, visual loss through cavernous sinus involvement through Meckel’s cave) ØHeadache and gait problems: slow onset ØObstructive hydrocephalus
Diagnostic approach Tumor diameter: between 2 and 8 cm. MRI with and without contrast T 1 -WI: Isointense extraaxial lesion T 2 -WI: variable intensity With contrast: the lesion enhances homogeneously + the dural tail Pial invasion brainstem edema Relationship to the basilar artery, jugular tubercle, cavernous sinus, parasellar region, internal auditory meatus. • 4 -vessel angiogram: recommended to see the venous sinus patency, anatomy of the temporal draining veins, the tumor blood supply. Embolisation is not recommended regardless of the dimensions of the tumor. • •

Preoperative (nf) and postoperative (lower row) MR images demonstrating a large petroclival meningioma extending below the IAM in a patient with intact hearing, prompting a posterior petrosal approach for resection. The postoperative images demonstrate complete resection via the posterior approach.
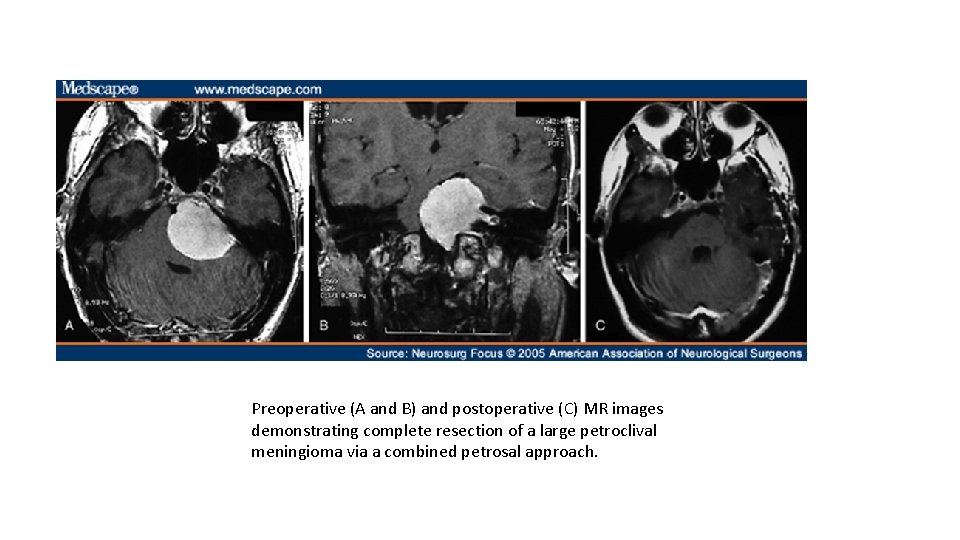
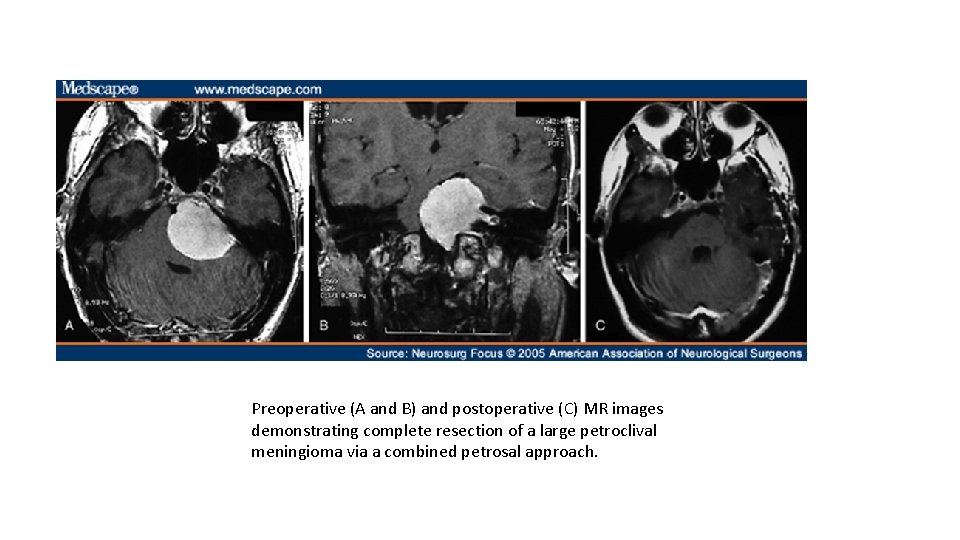
Preoperative (A and B) and postoperative (C) MR images demonstrating complete resection of a large petroclival meningioma via a combined petrosal approach.
1. Microsurgical resection • Approaches: üOrbitozygomatic approach üAnterior transpetrosal + pterional or subtemporal approach (extended middle fossa approach) üPosterior petrosal approach (with ligation of the superior petrosal sinus, but preservation of drainage of vein of Labbé) üCombined petrosal approach üRetrosigmoid approach
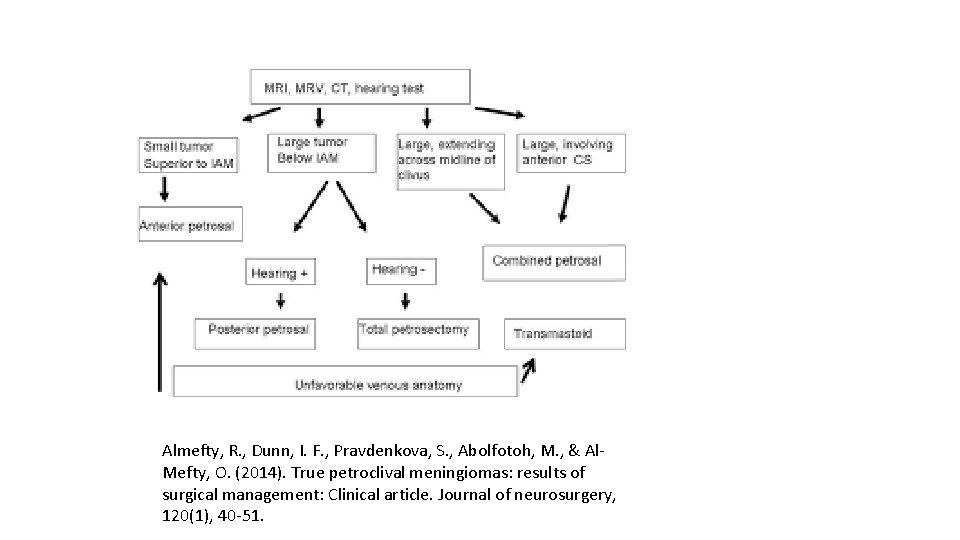
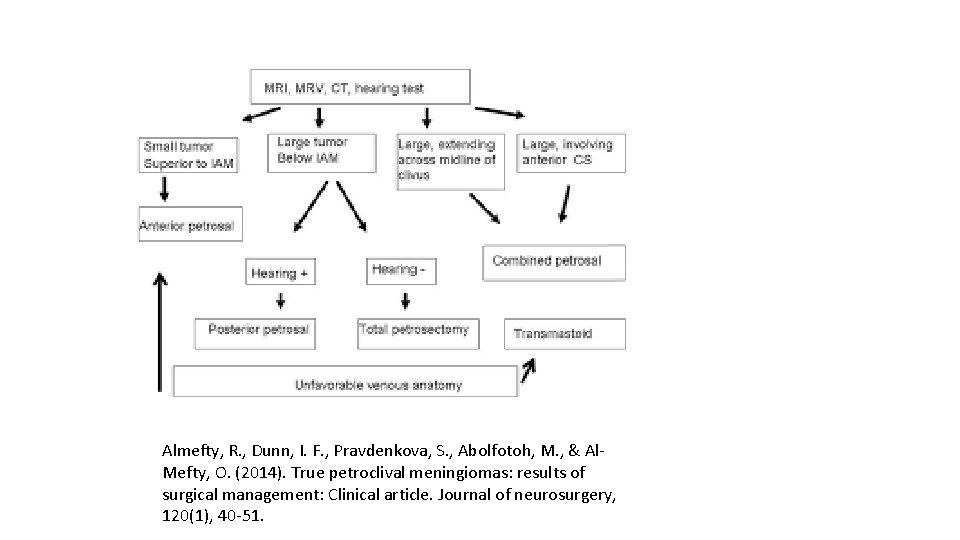
Almefty, R. , Dunn, I. F. , Pravdenkova, S. , Abolfotoh, M. , & Al. Mefty, O. (2014). True petroclival meningiomas: results of surgical management: Clinical article. Journal of neurosurgery, 120(1), 40 -51.
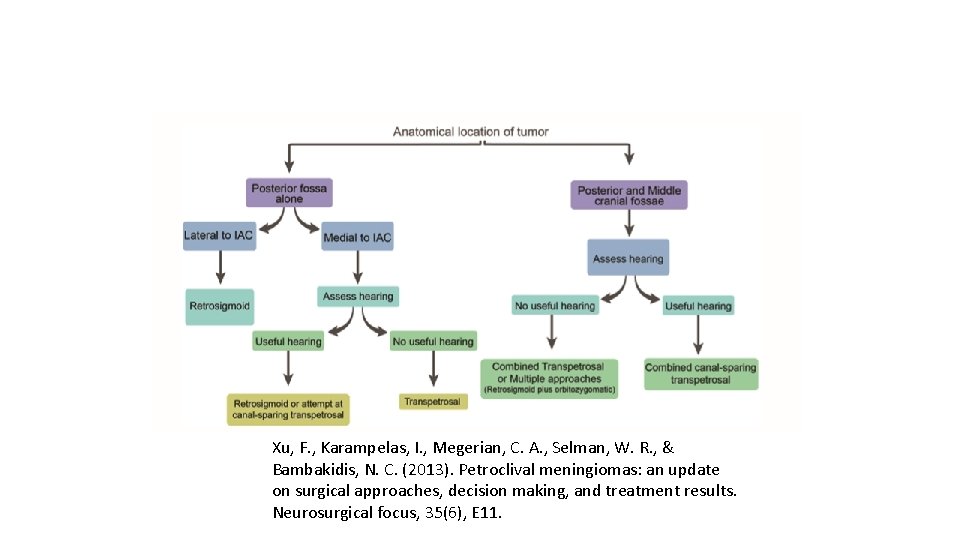
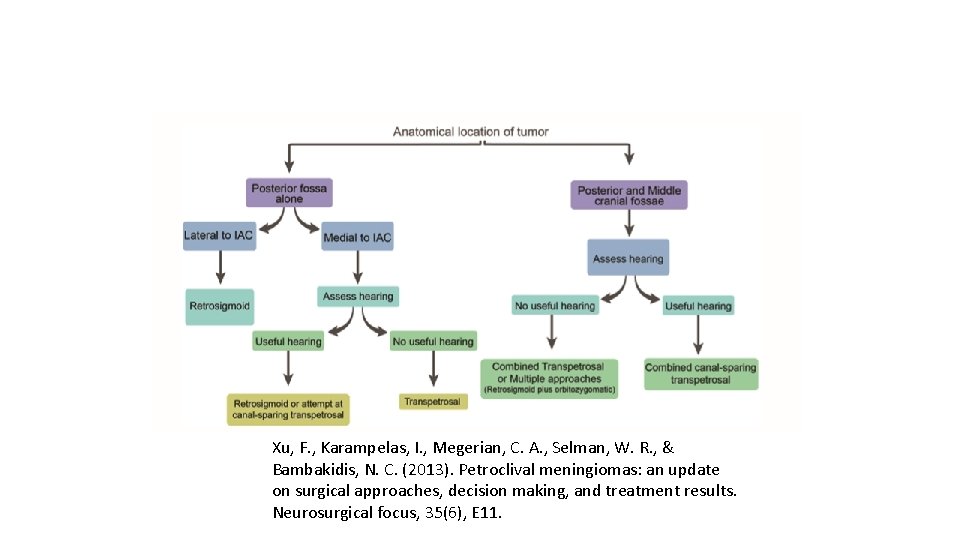
Xu, F. , Karampelas, I. , Megerian, C. A. , Selman, W. R. , & Bambakidis, N. C. (2013). Petroclival meningiomas: an update on surgical approaches, decision making, and treatment results. Neurosurgical focus, 35(6), E 11.
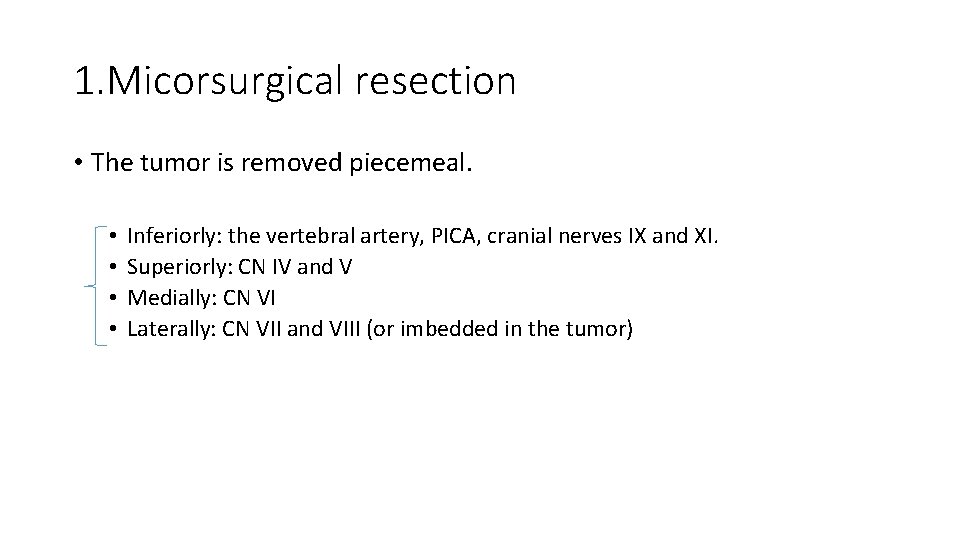
1. Micorsurgical resection • The tumor is removed piecemeal. • • Inferiorly: the vertebral artery, PICA, cranial nerves IX and XI. Superiorly: CN IV and V Medially: CN VI Laterally: CN VII and VIII (or imbedded in the tumor)
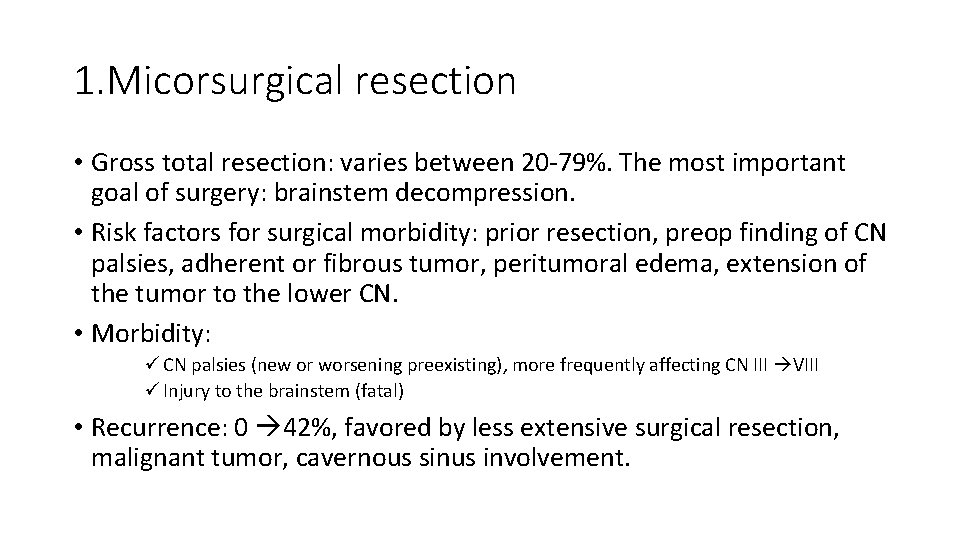
1. Micorsurgical resection • Gross total resection: varies between 20 -79%. The most important goal of surgery: brainstem decompression. • Risk factors for surgical morbidity: prior resection, preop finding of CN palsies, adherent or fibrous tumor, peritumoral edema, extension of the tumor to the lower CN. • Morbidity: ü CN palsies (new or worsening preexisting), more frequently affecting CN III VIII ü Injury to the brainstem (fatal) • Recurrence: 0 42%, favored by less extensive surgical resection, malignant tumor, cavernous sinus involvement.
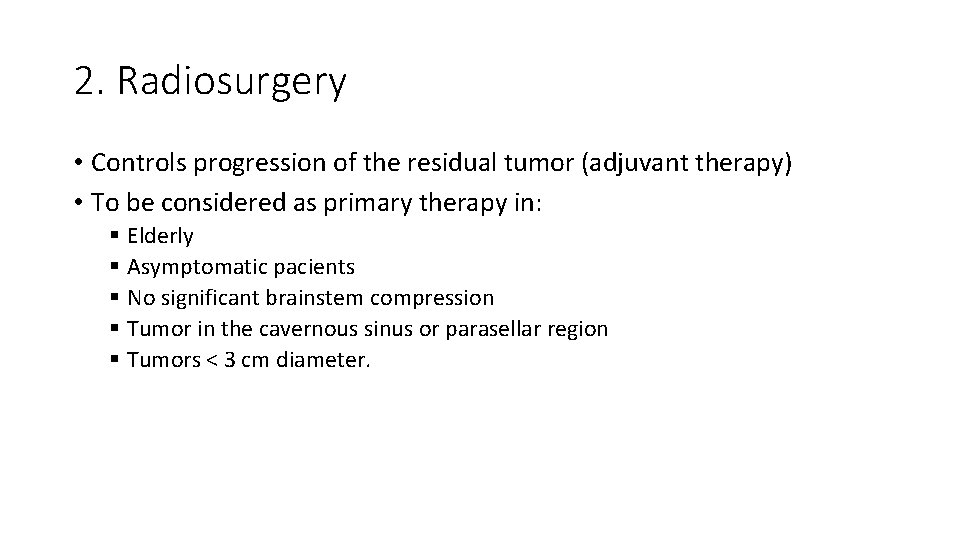
2. Radiosurgery • Controls progression of the residual tumor (adjuvant therapy) • To be considered as primary therapy in: § Elderly § Asymptomatic pacients § No significant brainstem compression § Tumor in the cavernous sinus or parasellar region § Tumors < 3 cm diameter.
3. Conventionally fractioned radiation therapy • Adjuvant therapy: controls tumor recurrence and progression
 Clivus
Clivus Clivus multrum composting toilet
Clivus multrum composting toilet Anatomic
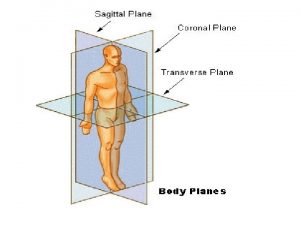
Anatomic Anatomic descriptors and fundamental body structure
Anatomic descriptors and fundamental body structure Which is dorsal side
Which is dorsal side Anatomic end arteries
Anatomic end arteries Anatomic dead space
Anatomic dead space Anatomic adjective for thigh
Anatomic adjective for thigh What is anatomical modifier
What is anatomical modifier Unit 4 anatomic references
Unit 4 anatomic references Unilateral balanced occlusion
Unilateral balanced occlusion Quality management in anatomic pathology
Quality management in anatomic pathology Non anatomic teeth indications
Non anatomic teeth indications Functional cusps
Functional cusps In anatomic lever systems, the fulcrum is the
In anatomic lever systems, the fulcrum is the Anatomic impression technique
Anatomic impression technique