Percutaneous Patent Foramen Ovale and Atrial Septal Defect
![Total number of patients with atrial septal defect= 40 Baseline characteristics Age (years) [mean±SD] Total number of patients with atrial septal defect= 40 Baseline characteristics Age (years) [mean±SD]](https://slidetodoc.com/presentation_image_h/a37b1fdc47945d6fbfe83714c0e66191/image-15.jpg)
- Slides: 17
Percutaneous Patent Foramen Ovale and Atrial Septal Defect Occlusion Under Intracardiac Echocardiography Guidance C. Kavvouras 1 , E. Vavouranakis 2, S. Vaina 2, K. Lampropoulos 1 , N. Karamichalakis 1 , G. Bazoukis 1 , D. Tousoulis 2 1 Department of Cardiology, Evaggelismos, General Hospital of Athens, Greece 2 A Cardiology Department, University of Athens
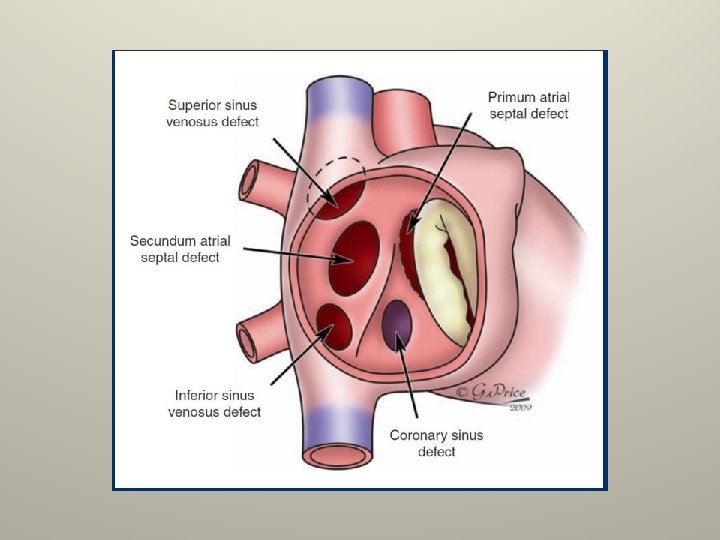
Introduction I • Patent foramen ovale (PFO) and atrial septal defects (ASDs) are relatively common congenital heart defects associated with a range of symptoms. • The foramen ovale, a component of fetal cardiovascular circulation • A communication between the right and left atrium that functions as a vascular bypass of the uninflated lungs. • Over a course of months after birth, an increase in left atrial pressure and a decrease in right atrial pressure result in permanent closure of the foramen ovale in most individuals. However, a PFO is a common finding in 25% of normal adults. • In some epidemiologic studies, PFO has been associated with cryptogenic stroke. Studies have also shown an association between PFO and migraine headache.
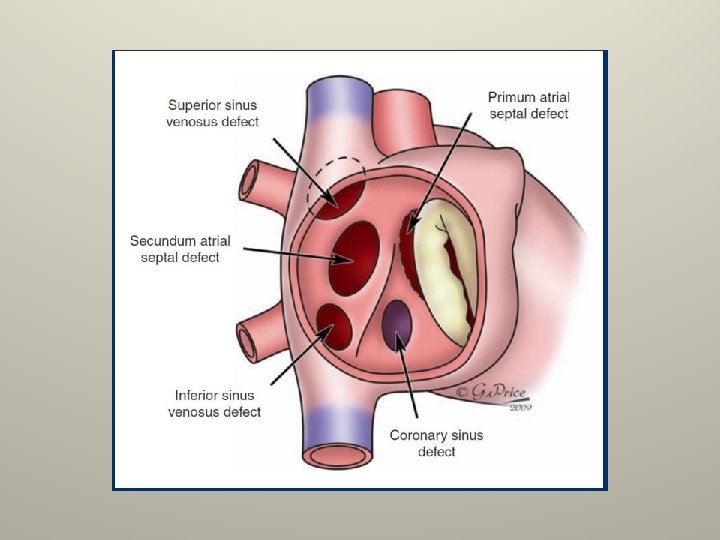
Introduction II • ASDs are categorized by their anatomy. • Ostium primum defects lie immediately adjacent to the atrioventricular valves and are within the spectrum of atrioventricular septal defects. Primum defects occur commonly in patients with Down syndrome. • Ostium secundum describes defects located midseptally and are typically near the fossa ovalis
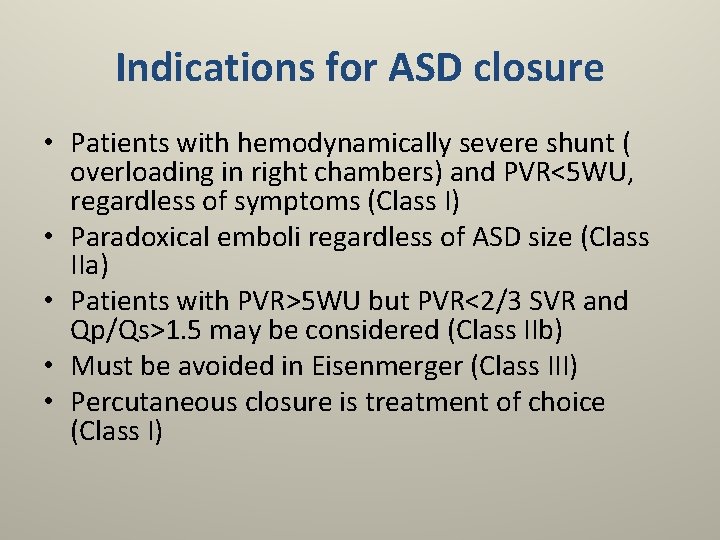
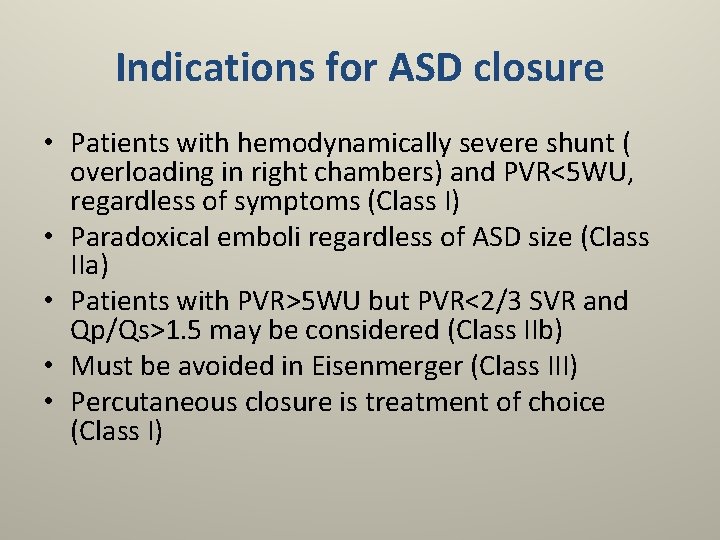
Indications for ASD closure • Patients with hemodynamically severe shunt ( overloading in right chambers) and PVR<5 WU, regardless of symptoms (Class I) • Paradoxical emboli regardless of ASD size (Class IIa) • Patients with PVR>5 WU but PVR<2/3 SVR and Qp/Qs>1. 5 may be considered (Class IIb) • Must be avoided in Eisenmerger (Class III) • Percutaneous closure is treatment of choice (Class I)
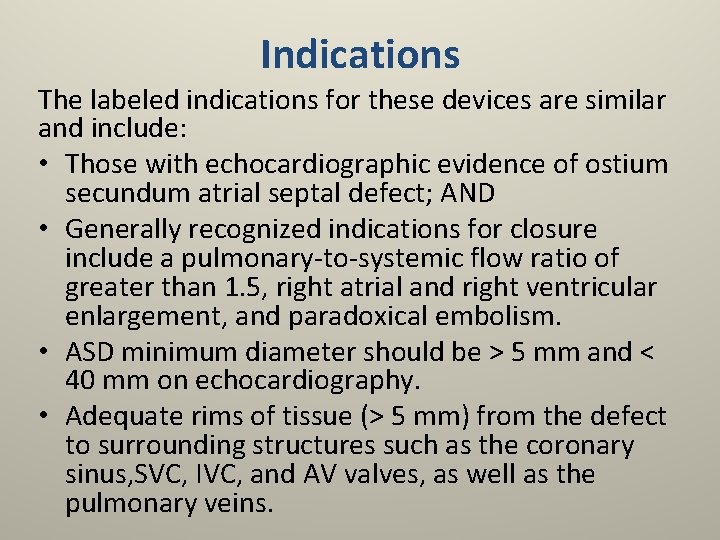
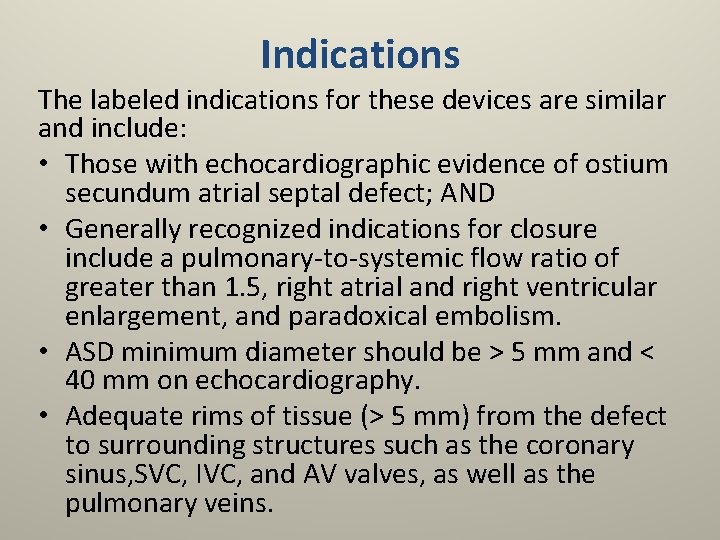
Indications The labeled indications for these devices are similar and include: • Those with echocardiographic evidence of ostium secundum atrial septal defect; AND • Generally recognized indications for closure include a pulmonary-to-systemic flow ratio of greater than 1. 5, right atrial and right ventricular enlargement, and paradoxical embolism. • ASD minimum diameter should be > 5 mm and < 40 mm on echocardiography. • Adequate rims of tissue (> 5 mm) from the defect to surrounding structures such as the coronary sinus, SVC, IVC, and AV valves, as well as the pulmonary veins.
Contra-indications • Aortic rim absence or severe deficiency confirmed in multiple TEE views. Absence of rims documented in multiple views of 30º, 40º, 50º+. • IVC rim absence or severe deficiency. • Pulmonary vascular resistance > 15 Woods units is an absolute contraindication. • Mitral valve impingement by the device with evidence of new-onset or increasing mitral insufficiency. Try a smaller device, if feasible. • Development of AV block after device deployment
Complications (<1%) • • • Stroke Cardiac tamponade from cardiac perforation Device-associated thrombus Device embolization Device erosion Incomplete defect closure
• Debate is on-going whether echocardiographic guidance is required for percutaneous PFO and ASD closure. • Transoesophageal echocardiography yields the best picture but it is uncomfortable for the patient lying on his back on the catheterisation table. • Only when it is undertaken in combination with intubation and general anaesthesia does it provide a comfortable working environment for the operator without having the patient suffer unnecessarily. • However, it turns a relatively simple 15 minute procedure into a demanding intervention for the patient with a prolonged recovery period, not to mention a sore throat.
• A more convenient alternative is intracardiac ultrasound. • However, this increases the cost of the already expensive device implantation. • In addition it requires a second large (12 French) venous access, which increases the risk of an arteriovenous fistula at the puncture site, an already not too rare complication of the procedure, occurring in about 1% of cases.
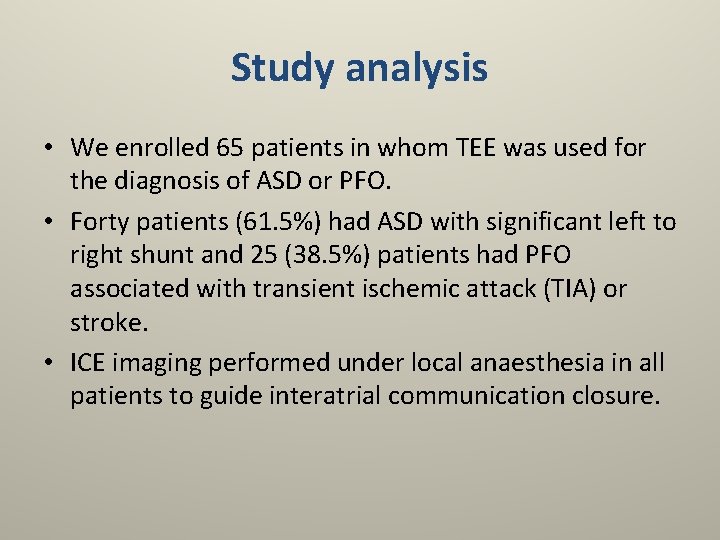
Advantages of intracardiac echo (ICE) • The interventional cardiologist can independently perform the imaging • No need for general anaesthesia and intubation • Good visualization of the atrial septum, the pulmonary veins, the left ventricle and the mitral valve • Higher resolution • Shorter procedural time and fast patient turnaround time • Reduced radiation dose
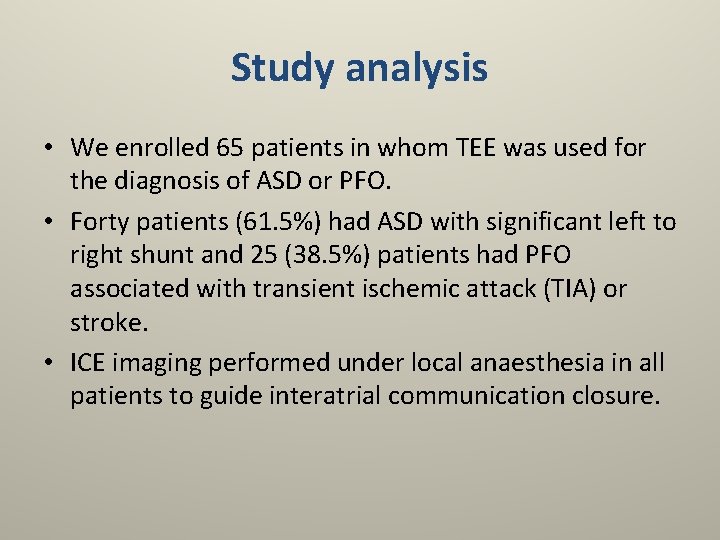
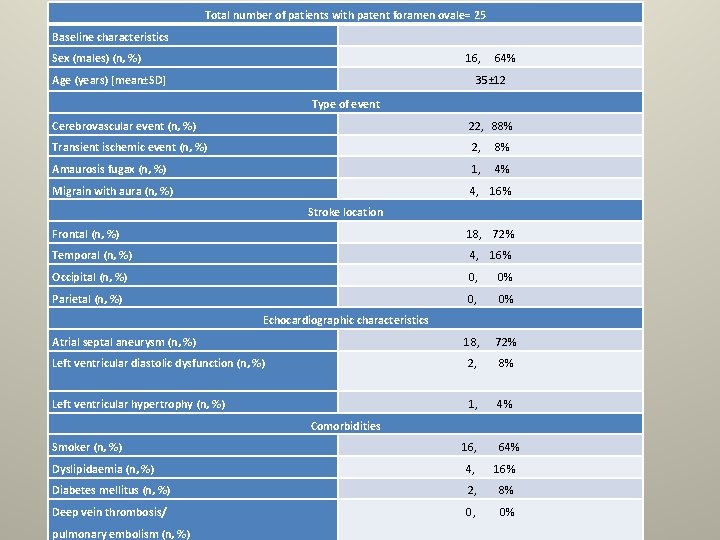
Study analysis • We enrolled 65 patients in whom TEE was used for the diagnosis of ASD or PFO. • Forty patients (61. 5%) had ASD with significant left to right shunt and 25 (38. 5%) patients had PFO associated with transient ischemic attack (TIA) or stroke. • ICE imaging performed under local anaesthesia in all patients to guide interatrial communication closure.
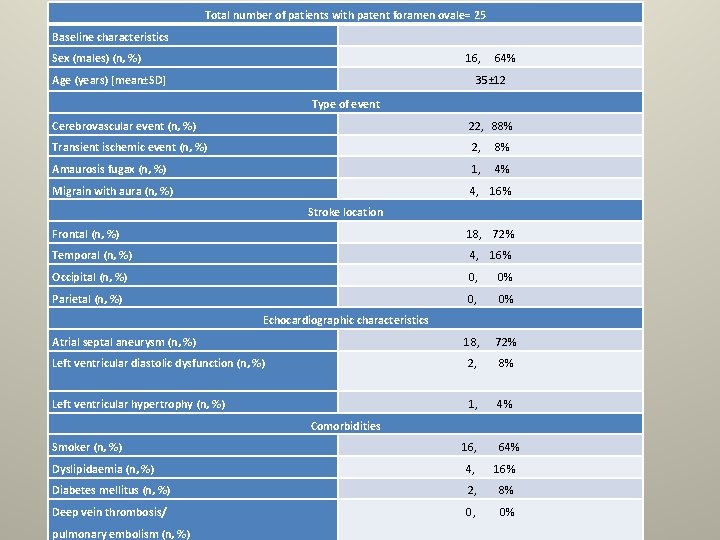
Total number of patients with patent foramen ovale= 25 Baseline characteristics Sex (males) (n, %) 16, 64% Age (years) [mean±SD] 35± 12 Type of event Cerebrovascular event (n, %) 22, 88% Transient ischemic event (n, %) 2, 8% Amaurosis fugax (n, %) 1, 4% Migrain with aura (n, %) 4, 16% Stroke location Frontal (n, %) 18, 72% Temporal (n, %) 4, 16% Occipital (n, %) 0, 0% Parietal (n, %) 0, 0% Echocardiographic characteristics Atrial septal aneurysm (n, %) 18, 72% Left ventricular diastolic dysfunction (n, %) 2, 8% Left ventricular hypertrophy (n, %) 1, 4% Comorbidities Smoker (n, %) 16, 64% Dyslipidaemia (n, %) 4, 16% Diabetes mellitus (n, %) 2, 8% Deep vein thrombosis/ 0, 0% pulmonary embolism (n, %)
![Total number of patients with atrial septal defect 40 Baseline characteristics Age years meanSD Total number of patients with atrial septal defect= 40 Baseline characteristics Age (years) [mean±SD]](https://slidetodoc.com/presentation_image_h/a37b1fdc47945d6fbfe83714c0e66191/image-15.jpg)
Total number of patients with atrial septal defect= 40 Baseline characteristics Age (years) [mean±SD] 52± 16 Sex (males) (n, %) 28, 70% Symptoms Dyspnoea (n, %) 18, 45% Chest Pain (n, %) 19, 48% Palpitations (n, %) 24, 60% Fatigue (n, %) 30, 75% Atrial fibrillation (n, %) 2, 5% Cardiomegaly (n, %) 15, 37. 5%
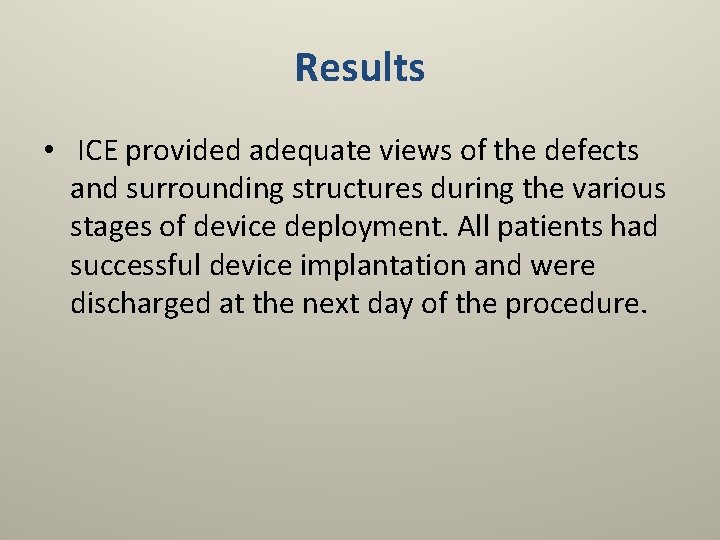
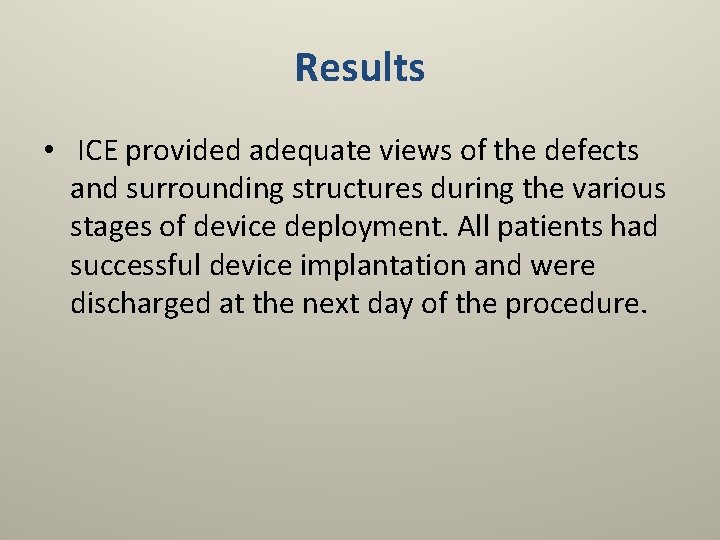
Results • ICE provided adequate views of the defects and surrounding structures during the various stages of device deployment. All patients had successful device implantation and were discharged at the next day of the procedure.
Conclusion ICE is a safe and high-quality imaging technique to guide transcatheter ASD and PFO occlusion. Additionally, ICE can both facilitate device implantation and detect cardiac abnormalities that are not identified with TEE during the initial diagnostic investigation.
 Tetralogia fallot definitie
Tetralogia fallot definitie Nursing management of atrial septal defect
Nursing management of atrial septal defect Atrial septal defect
Atrial septal defect Patent foramen ovale
Patent foramen ovale Trabeculated part of right ventricle
Trabeculated part of right ventricle Sinus venorum
Sinus venorum Handoout
Handoout Crocodin
Crocodin Diff between schottky and frenkel defects
Diff between schottky and frenkel defects Kroger vink notation examples
Kroger vink notation examples Vacancy defect and interstitial defect
Vacancy defect and interstitial defect Percutaneous transhepatic cholangiography and drainage
Percutaneous transhepatic cholangiography and drainage Percutaneous image-guided lumbar decompression (pild)
Percutaneous image-guided lumbar decompression (pild) Percutaneous balloon pericardiotomy
Percutaneous balloon pericardiotomy Operative cholangiography
Operative cholangiography Amnio vs cvs
Amnio vs cvs Pleural effusion ellis curve
Pleural effusion ellis curve Trypanosoma bruzi
Trypanosoma bruzi