Pediatric POST Practical Approaches Potential Pitfalls and Poignant





- Slides: 56
Pediatric POST: Practical Approaches, Potential Pitfalls and Poignant Moments Melody J. Cunningham, MD Director, Pediatric Palliative Care Le Bonheur Children’s Hospital January 14, 2014
Disclosures • No financial disclosures • No off-label uses of medications
Pediatric Palliative Care and POST “Helping children live as well as possible for as long as possible. ”
Practical Approaches • • American Academy of Pediatrics guidance Sentinel study Disease trajectory and prognosis Relationship – Family-centered – Communication • Approach without relationship
AAP Policy Statement • Enhance quality of life • Ultimately terminal conditions • Relief of symptoms • Dyspnea, pain • Relief from conditions • Loneliness, fear • Bereavement • Ensure family can remain intact
AAP Policy Statement • Integrated Model: “the components of palliative care offered at diagnosis and continued throughout the course of illness, whether the outcome ends in cure or death. ”
Sentinel Study-NEJM Early Palliative Care for Patients with Metastatic Non-Small Cell Lung CA • • 151 patients Method • Randomized, Prospective • • • Standard Oncologic Care only Standard Oncologic Care with early integrated palliative care Baseline and 12 week assessments • Decisions, quality of life NEJM 2010; 363: 733 -42
Sentinel Study-NEJM • Results: • 107 completed assessments Better Quality of Life (98. 0 vs 91. 5; P=0. 03) • FACT-L scale range 0 -136 • Less Depression (16% vs. 38%; P=0. 01) • Less Aggressive End of Life Care (33% vs. 54%; P=0. 05) • Longer Median Survival (11. 6 vs. 8. 9 mos; P=0. 02) • NEJM 2010; 363: 733 -42
Unique aspects inform discussions • Causes of death in children • Illness trajectories and prognoses
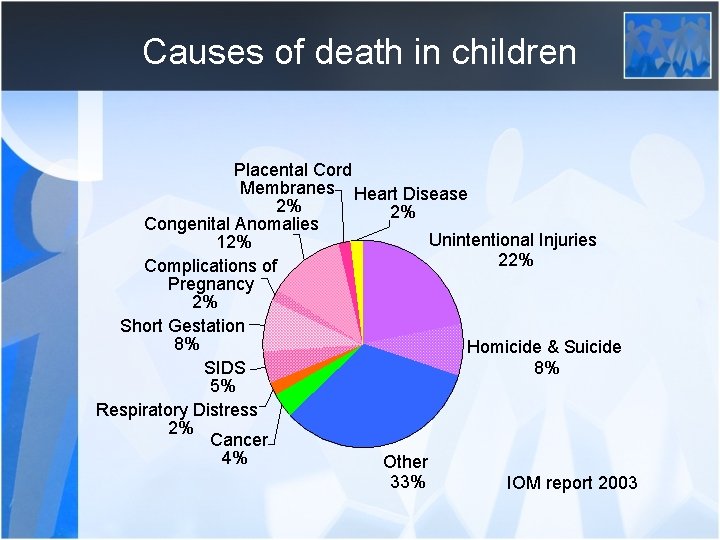
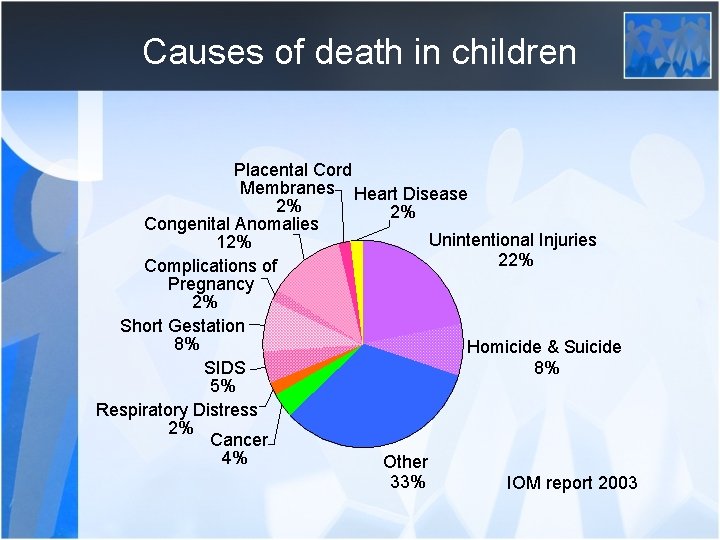
Causes of death in children Placental Cord Membranes Heart Disease 2% 2% Congenital Anomalies Unintentional Injuries 12% 22% Complications of Pregnancy 2% Short Gestation 8% Homicide & Suicide SIDS 8% 5% Respiratory Distress 2% Cancer 4% Other 33% IOM report 2003
Unique aspects inform decisions • Causes of death in children • Illness trajectories and prognoses
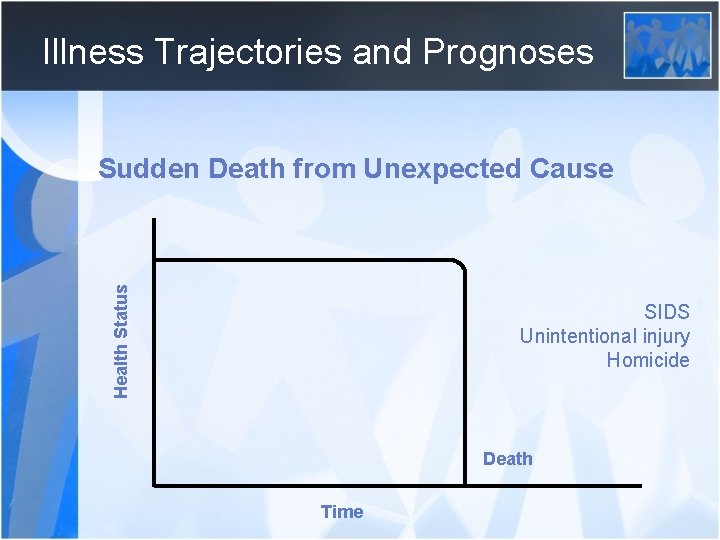
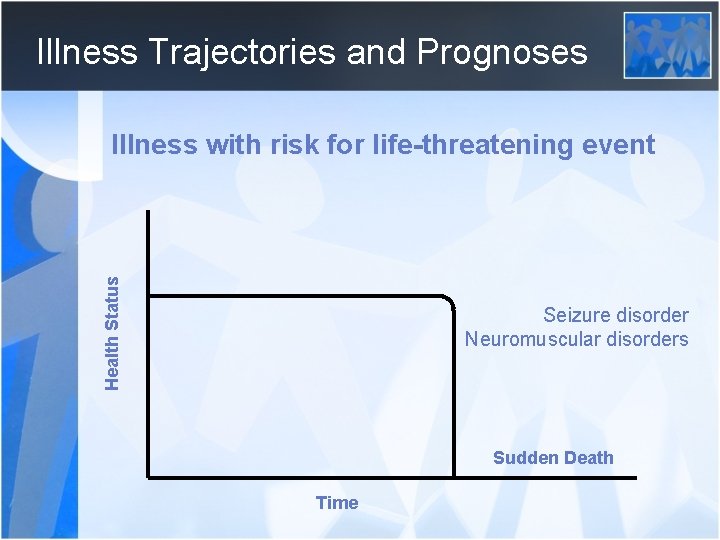
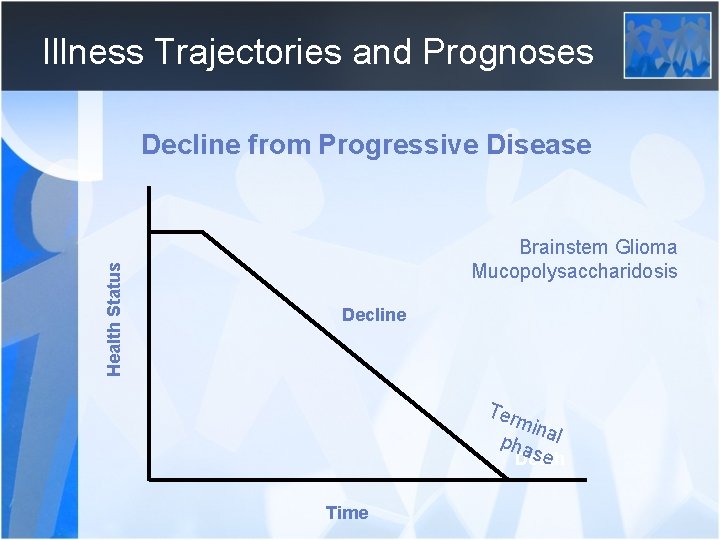
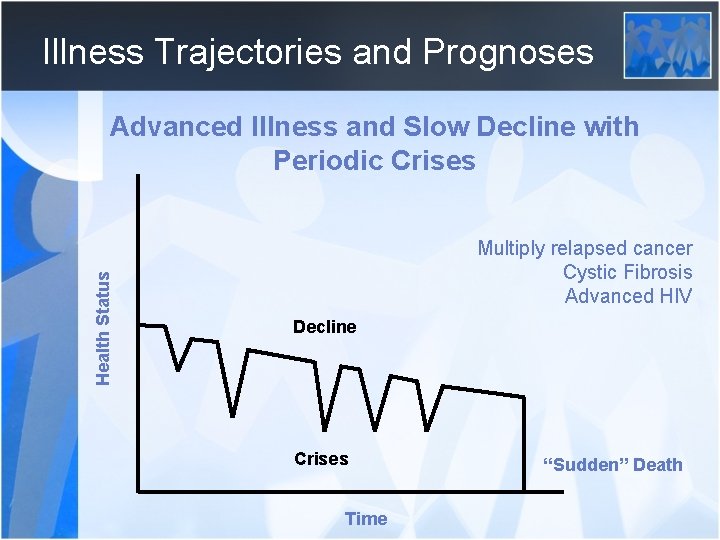
Illness Trajectories and Prognoses • Variation in cause of death and prognosis • Four basic trajectories exist • Infants and Children • Timeline differs IOM Committee on Palliative and End-of-Life care for Children and their families, 2003
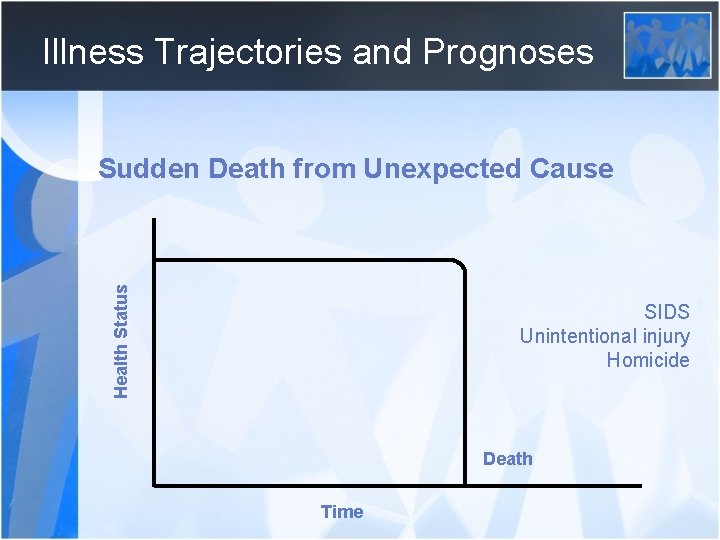
Illness Trajectories and Prognoses Health Status Sudden Death from Unexpected Cause SIDS Unintentional injury Homicide Death Time
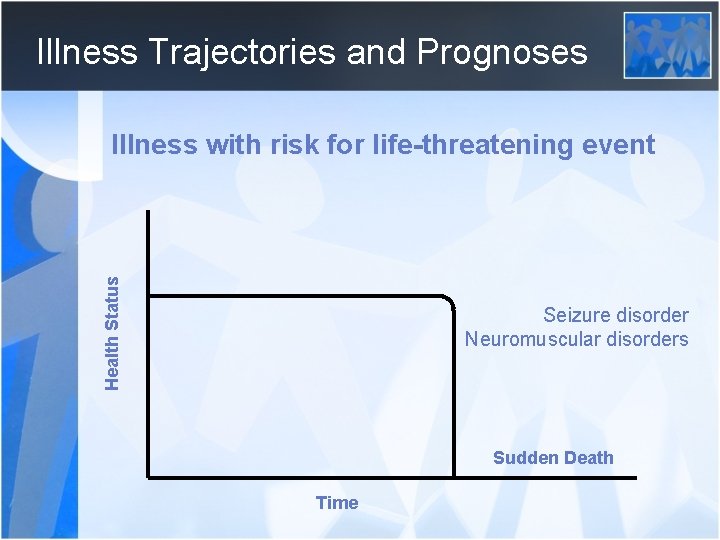
Illness Trajectories and Prognoses Health Status Illness with risk for life-threatening event Seizure disorder Neuromuscular disorders Sudden Death Time
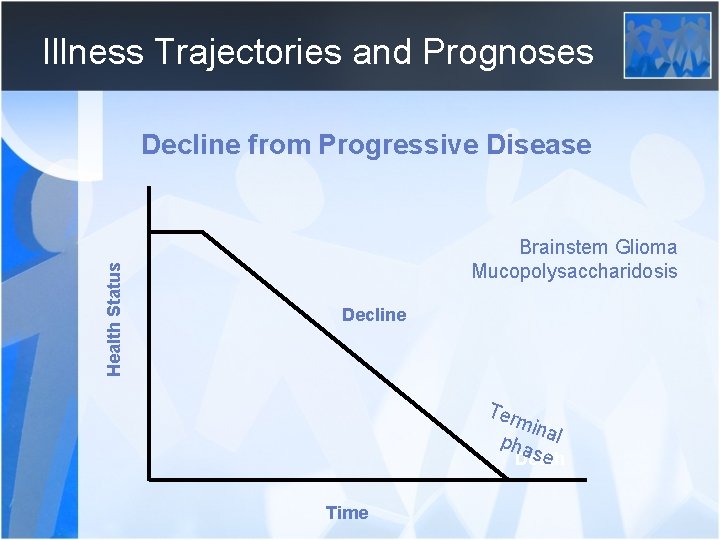
Illness Trajectories and Prognoses Health Status Decline from Progressive Disease Brainstem Glioma Mucopolysaccharidosis Decline T er mi n pha al se Death Time
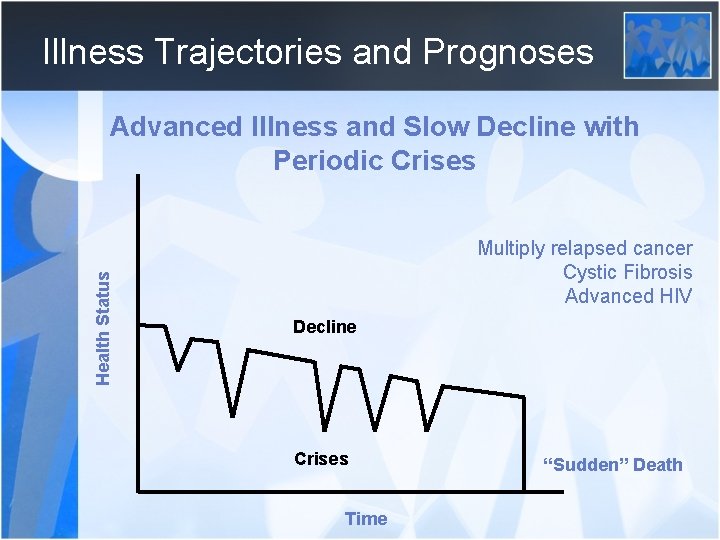
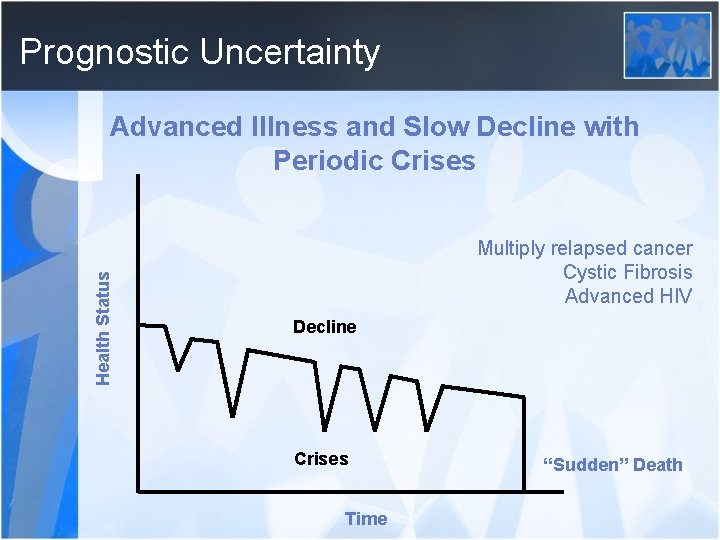
Illness Trajectories and Prognoses Health Status Advanced Illness and Slow Decline with Periodic Crises Multiply relapsed cancer Cystic Fibrosis Advanced HIV Decline Crises Time “Sudden” Death
Family and Patient-centered “Dear Me! What a troublesome business a family is!” -The Water-Babies, Charles Kingsley, 1863
Family and Patient-centered
Family and Patient-centered • • • Leukemia patient and laying on of hands Home nasogastric feedings Continuous nasogastric feedings Pain medication for seizure patient Home extubation
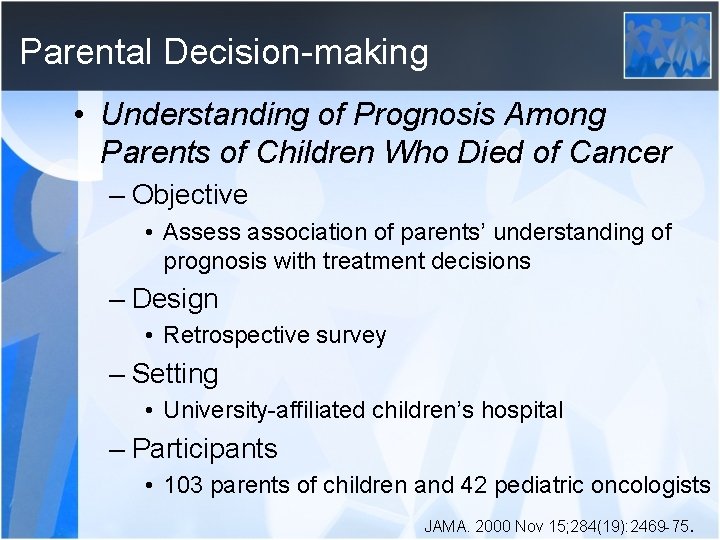
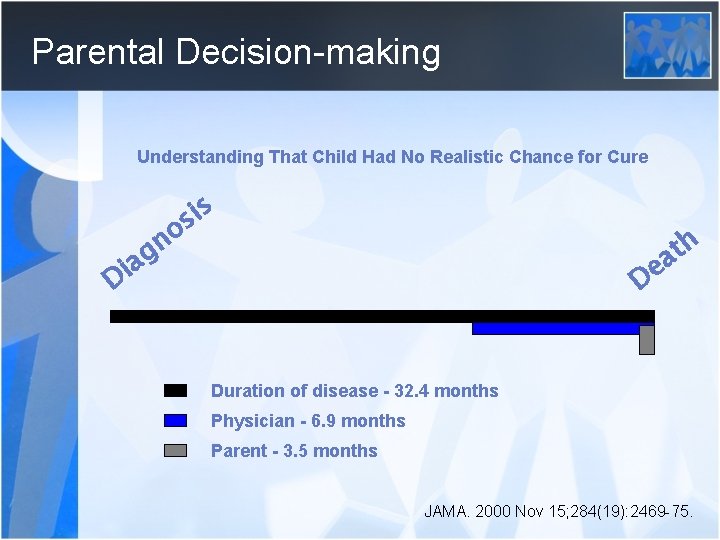
Parental Decision-making • Understanding of Prognosis Among Parents of Children Who Died of Cancer – Objective • Assess association of parents’ understanding of prognosis with treatment decisions – Design • Retrospective survey – Setting • University-affiliated children’s hospital – Participants • 103 parents of children and 42 pediatric oncologists JAMA. 2000 Nov 15; 284(19): 2469 -75.
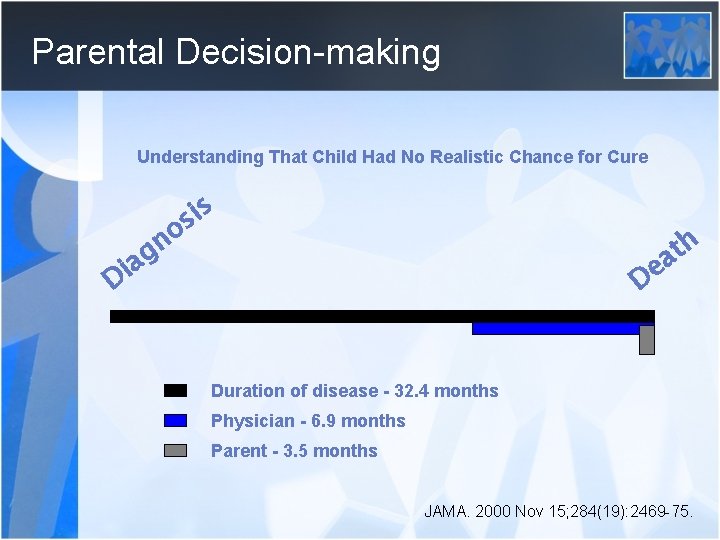
Parental Decision-making Understanding That Child Had No Realistic Chance for Cure i s no s h t a Di ag De Duration of disease - 32. 4 months Physician - 6. 9 months Parent - 3. 5 months JAMA. 2000 Nov 15; 284(19): 2469 -75.
Parental Decision-making • Understanding of Prognosis Among Parents of Children Who Died of Cancer – Results • Earlier recognition of prognosis – Earlier hospice discussion – Better quality of home care – Earlier DNR – Less cancer directed therapy in last month – Higher likelihood of goal to diminish suffering JAMA. 2000 Nov 15; 284(19): 2469 -75.
Parental Decision-making • Study cont. – Conclusion • Delay in parents’ recognition of prognosis • Earlier recognition emphasizes decreased suffering • Earlier recognition leads to integration of palliative care JAMA. 2000 Nov 15; 284(19): 2469 -75.
POST-Pediatrics
Practical Approaches • Develop relationship – Discard personal or medical team agenda • “Tell me what you have heard? ” • “Tell me what questions you have? ” • “What worries you most right now? – Family-centered and patient-centered • Always acknowledge child • Engage in discussion of what the child likes, brings joy, child’s meaning in the family – Communication • Always sit
Potential Pitfalls • Communication • Unacknowledged prognostic uncertainty – Dogmatic predictions • POST and hospital DNR • Unrecognized consequences • Parental guilt – Child’s experience – Child’s preference
Potential Pitfalls • Communication • Unacknowledged prognostic uncertainty – Dogmatic predictions • POST and hospital DNR • Unrecognized consequences • Parental guilt – Child’s experience – Child’s preference
Communication: The Power of Words http: //www. inmycommunity. com
Communication: The Power of Words The Great Mokusatsu Mistake Was This the Deadliest Error of Our Time? William J. Coughlin March 1953, p. 31 -40

Communication Training How did you learn to care for dying children? *Trial and error 92% From colleagues in clinical practice 82% From role models during residency and fellowship 65% Formal courses 10% * Reported by physicians to be most useful Hilden et al JCO 2001
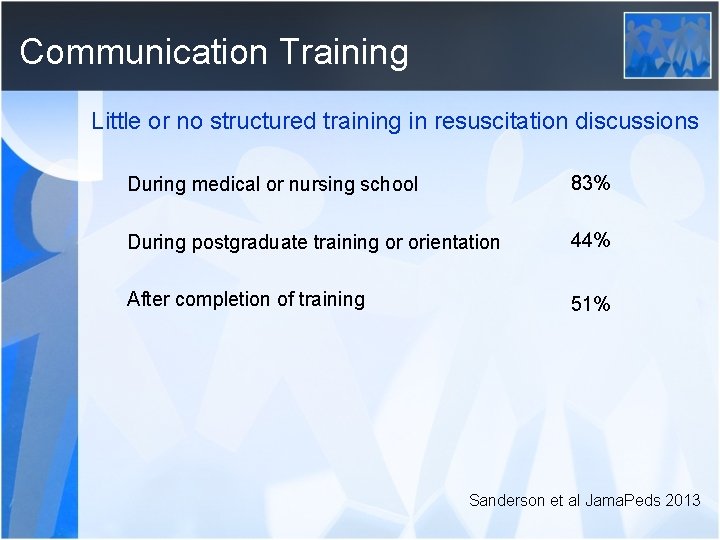
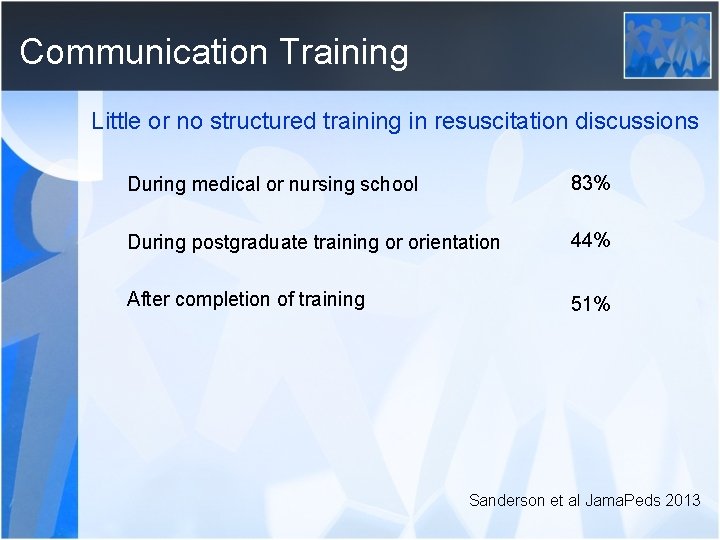
Communication Training Little or no structured training in resuscitation discussions During medical or nursing school 83% During postgraduate training or orientation 44% After completion of training 51% Sanderson et al Jama. Peds 2013
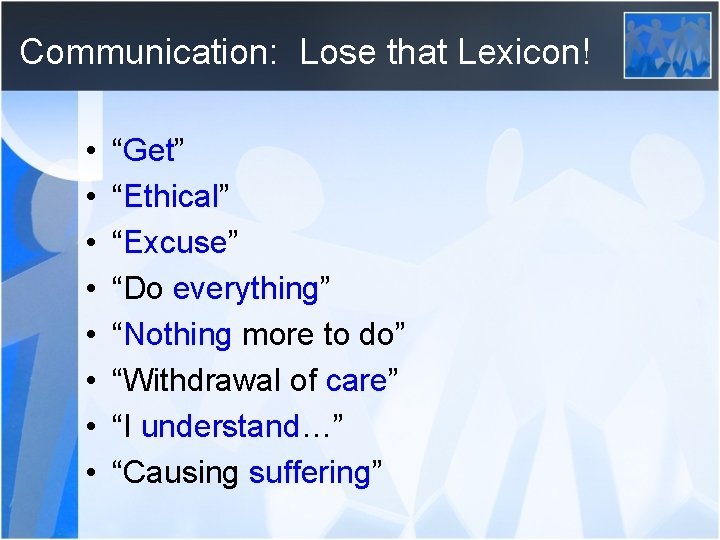
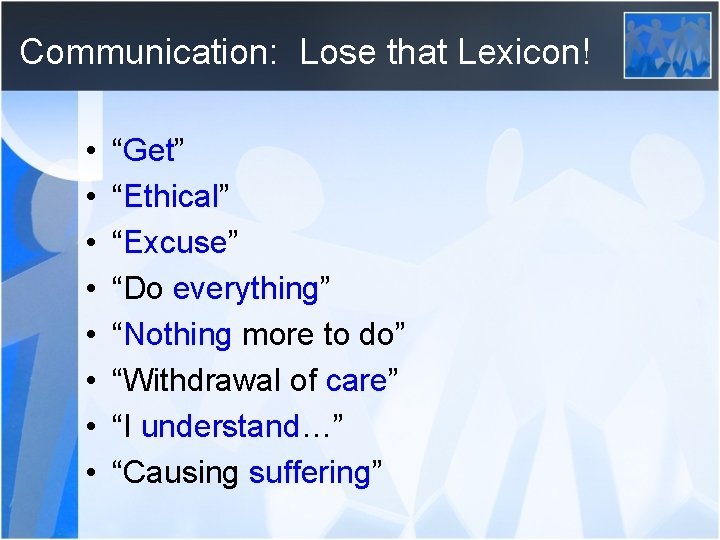
Communication: Lose that Lexicon! • • “Get” “Ethical” “Excuse” “Do everything” “Nothing more to do” “Withdrawal of care” “I understand…” “Causing suffering”
Listening “I assure you that you can pick up more information when you are listening than when you are talking. ” -The Trumpet of the Swan, E. B. White, 1970
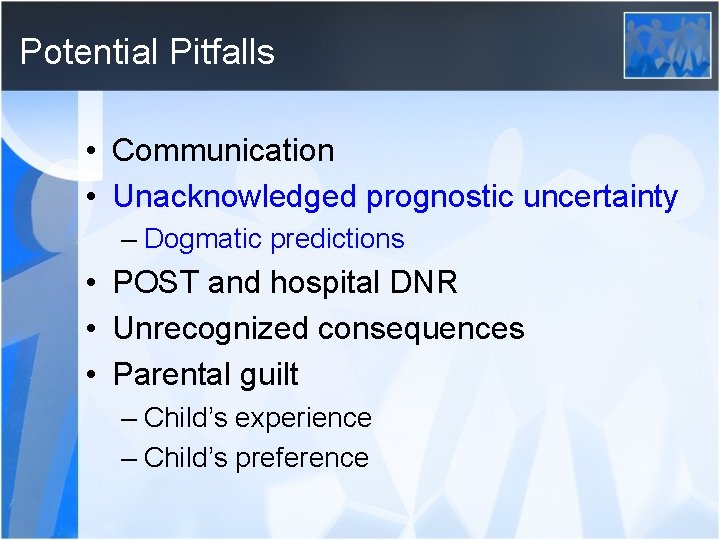
Potential Pitfalls • Communication • Unacknowledged prognostic uncertainty – Dogmatic predictions • POST and hospital DNR • Unrecognized consequences • Parental guilt – Child’s experience – Child’s preference
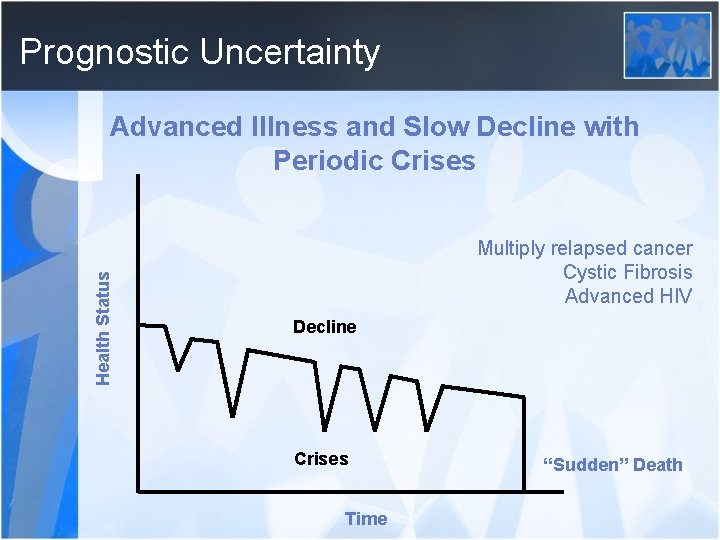
Prognostic Uncertainty Health Status Advanced Illness and Slow Decline with Periodic Crises Multiply relapsed cancer Cystic Fibrosis Advanced HIV Decline Crises Time “Sudden” Death
Prognostic Uncertainty and “Happys” • “We are not in charge. ” – 3 year old and motor vehicle accident – 10 year old and near-drowning episode – 17 year old with cerebral palsy and severe developmental delay and Holidays
Potential Pitfalls • Communication • Unacknowledged prognostic uncertainty – Dogmatic predictions • POST and hospital DNR • Unrecognized consequences • Parental guilt – Child’s experience – Child’s preference
POST and Hospital DNR Orders • • POST vs. Inpatient DNR order Documented discussion Computer order entry Parent signature
Potential Pitfalls • Communication • Unacknowledged prognostic uncertainty – Dogmatic predictions • POST and hospital DNR • Unrecognized consequences • Parental guilt – Child’s experience – Child’s preference
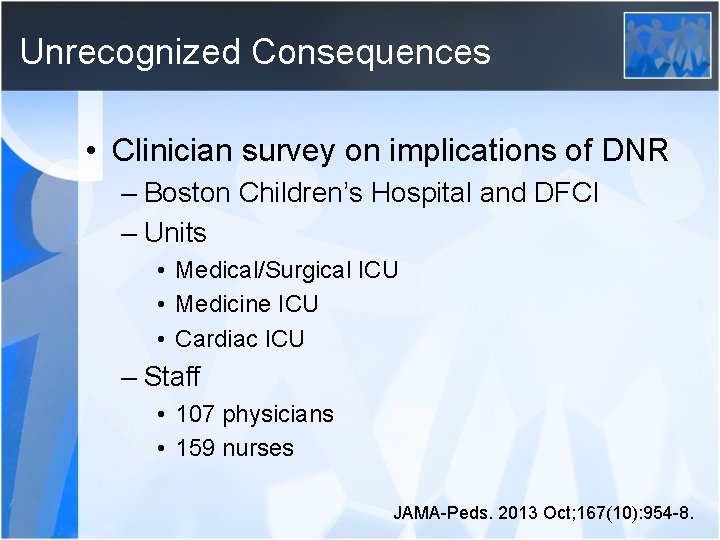
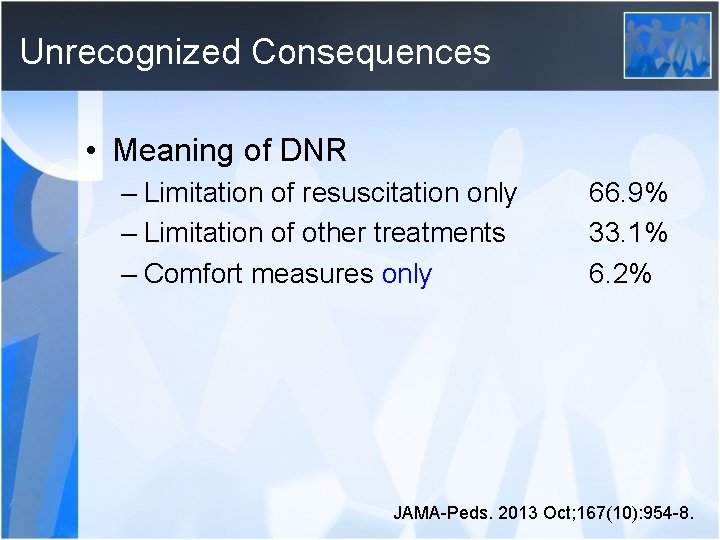
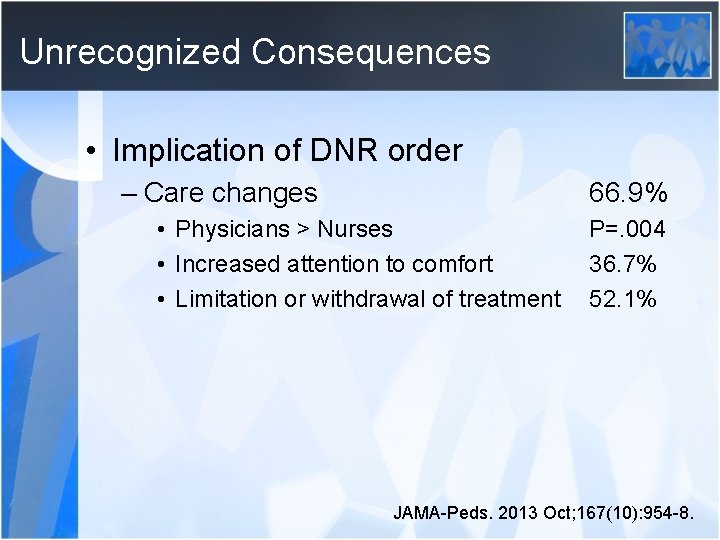
Unrecognized Consequences • Clinician survey on implications of DNR – Boston Children’s Hospital and DFCI – Units • Medical/Surgical ICU • Medicine ICU • Cardiac ICU – Staff • 107 physicians • 159 nurses JAMA-Peds. 2013 Oct; 167(10): 954 -8.
Unrecognized Consequences • When a child has a DRN order in place, what does this mean to you? • In your experience, how much does the care of a patient change once a DNR order is written? • In what way does care change? JAMA-Peds. 2013 Oct; 167(10): 954 -8.
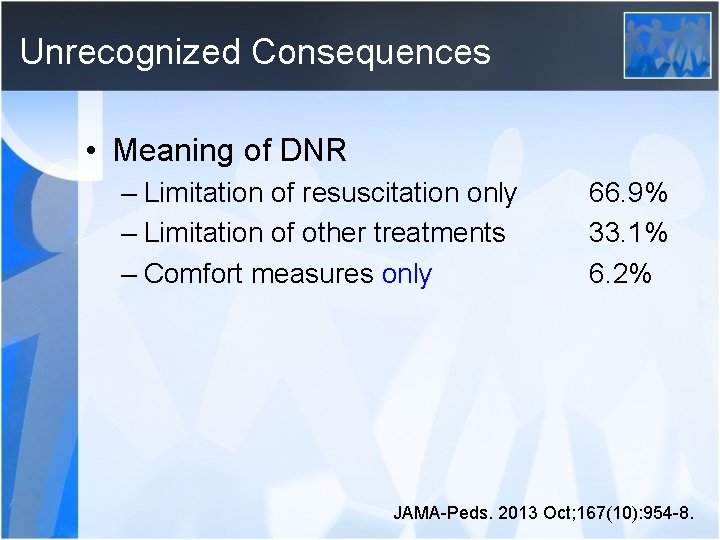
Unrecognized Consequences • Meaning of DNR – Limitation of resuscitation only – Limitation of other treatments – Comfort measures only 66. 9% 33. 1% 6. 2% JAMA-Peds. 2013 Oct; 167(10): 954 -8.
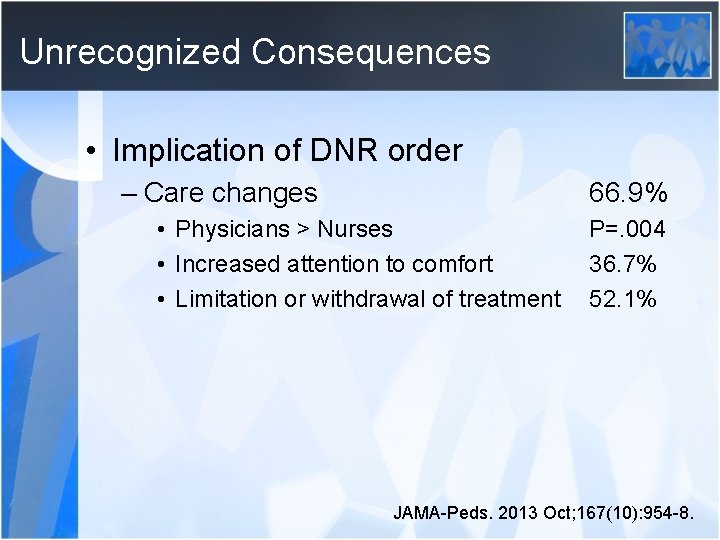
Unrecognized Consequences • Implication of DNR order – Care changes 66. 9% • Physicians > Nurses • Increased attention to comfort • Limitation or withdrawal of treatment P=. 004 36. 7% 52. 1% JAMA-Peds. 2013 Oct; 167(10): 954 -8.
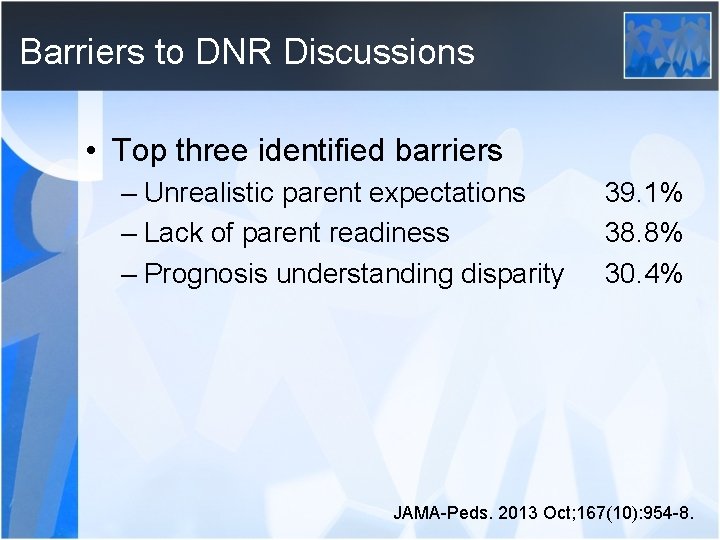
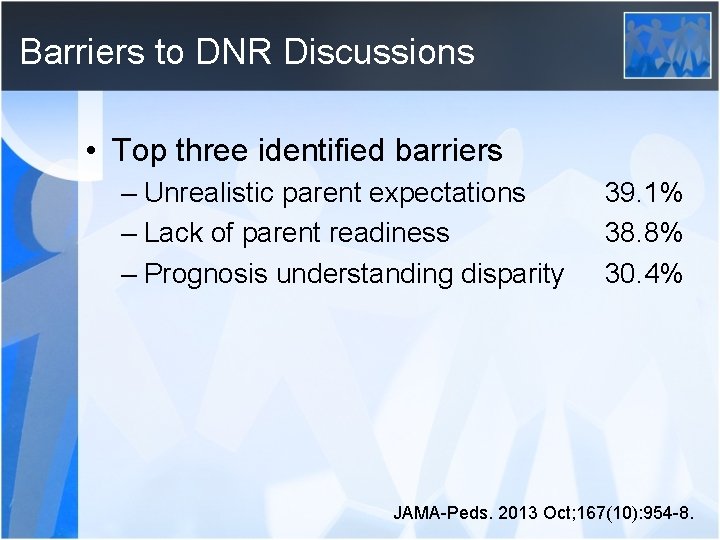
Barriers to DNR Discussions • Top three identified barriers – Unrealistic parent expectations – Lack of parent readiness – Prognosis understanding disparity 39. 1% 38. 8% 30. 4% JAMA-Peds. 2013 Oct; 167(10): 954 -8.
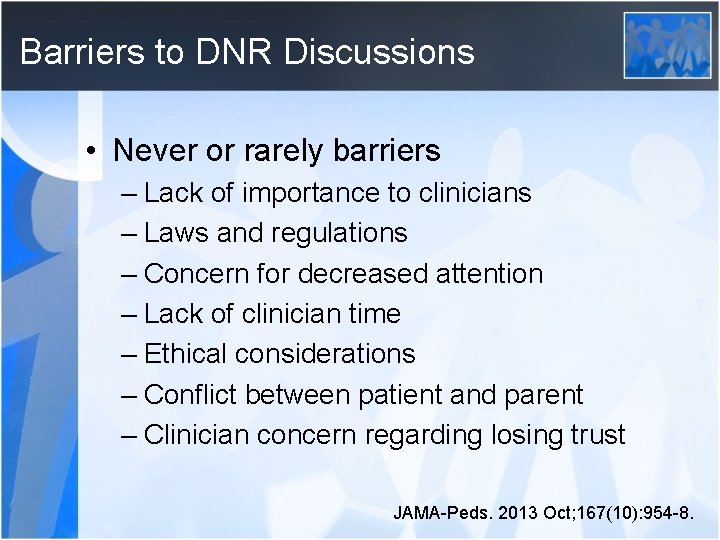
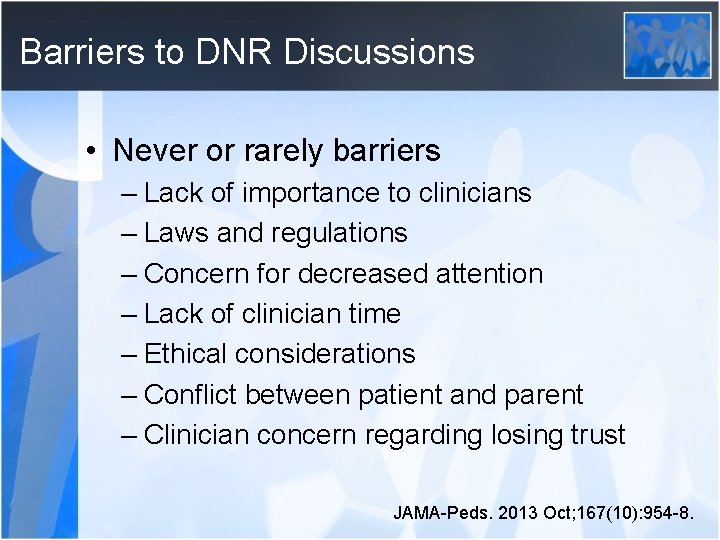
Barriers to DNR Discussions • Never or rarely barriers – Lack of importance to clinicians – Laws and regulations – Concern for decreased attention – Lack of clinician time – Ethical considerations – Conflict between patient and parent – Clinician concern regarding losing trust JAMA-Peds. 2013 Oct; 167(10): 954 -8.
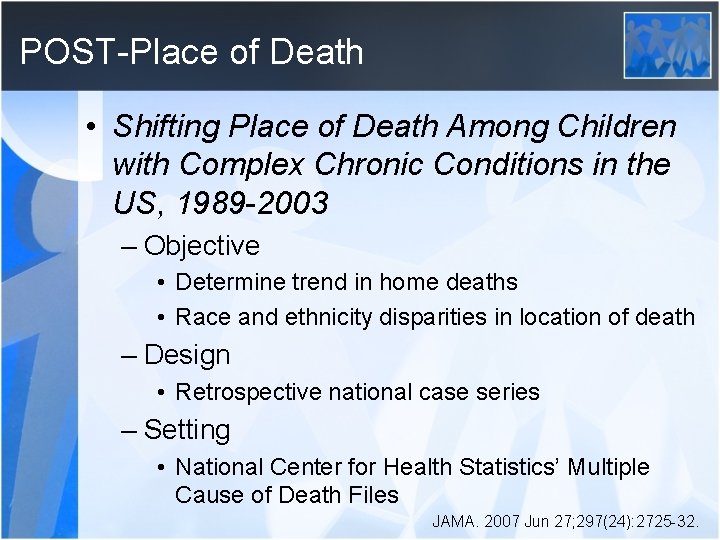
POST-Place of Death • Shifting Place of Death Among Children with Complex Chronic Conditions in the US, 1989 -2003 – Objective • Determine trend in home deaths • Race and ethnicity disparities in location of death – Design • Retrospective national case series – Setting • National Center for Health Statistics’ Multiple Cause of Death Files JAMA. 2007 Jun 27; 297(24): 2725 -32.
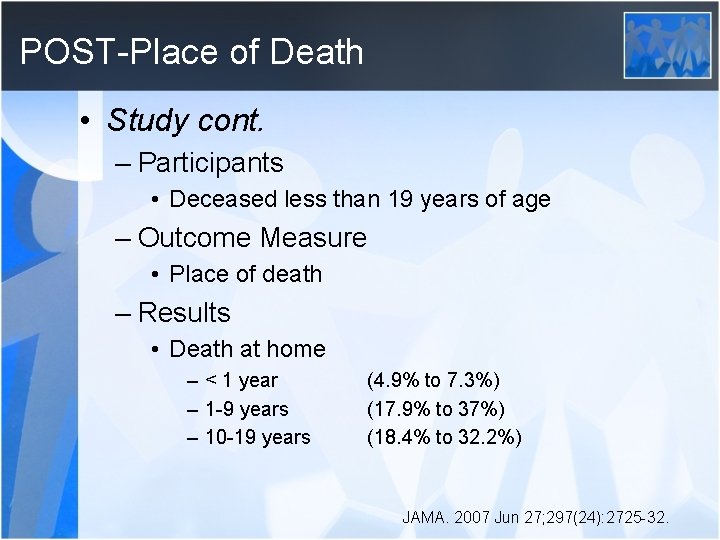
POST-Place of Death • Study cont. – Participants • Deceased less than 19 years of age – Outcome Measure • Place of death – Results • Death at home – < 1 year – 1 -9 years – 10 -19 years (4. 9% to 7. 3%) (17. 9% to 37%) (18. 4% to 32. 2%) JAMA. 2007 Jun 27; 297(24): 2725 -32.
POST-Place of Death • Study cont. – Results cont. • Death at home by ethnicity – Black (OR 0. 50) – Hispanic (OR 0. 52) – Conclusions • Children with complex, chronic medical conditions are increasingly dying at home • Racial and ethnic disparities exist • Opportunities for improvement exist JAMA. 2007 Jun 27; 297(24): 2725 -32.
Poignant Moments

Poignant Moments
Poignant Moments “It is sometimes the mystery of death that brings us to a consciousness of the still greater mystery of life. ” -Rebecca of Sunnybrook Farm, Kate Douglas Wiggin, 1903
Bereavement care • An essential component of pediatric palliative care • Most effective when provided by a team who has known the child and family • Aids family in transition through grief process
Bereavement Care “Tears may be the beginning, but they should not be the end of things. ” “The Goldfish, ” The Little Bookroom, Eleanor Farjeon, 1956


