PEDIATRIC NURSING GRAND ROUNDS Natalie Eyer 10813 The








- Slides: 26

PEDIATRIC NURSING GRAND ROUNDS Natalie Eyer 10/8/13

The Patient KL 15 months old African American female Cystic Fibrosis, no enzyme deficiency Pneumonia

Client History: Past Term SVD “Abnormal” newborn screening Diagnosed with Cystic Fibrosis at 13 months old (2 months ago) with positive sweat test
Client History: Hospitalization PCP appointment: Parent report cough, more wet than normal Parent report occasional vomiting Rhinorrhea No fever CXR: left lower lobe pneumonia
Client History: Pathophysiology Chronic, autoimmune, genetic disorder , CTFR gene Characterized by a increased viscosity of mucous secretions, elevation of sweat electrolytes, an increase in enzymes of the saliva, an abnormalities of the nervous system Primary factor responsible for complications with the disease is the viscous mucous secretions Secretions cause impaired gas exchange as a result of bronchial obstruction Thick mucus will also make the victim more susceptible to infection Overtime the destruction of lung tissue leads to fibrotic changes, making the lung much less compliant (Hockenberyy & Wilson, 2011)
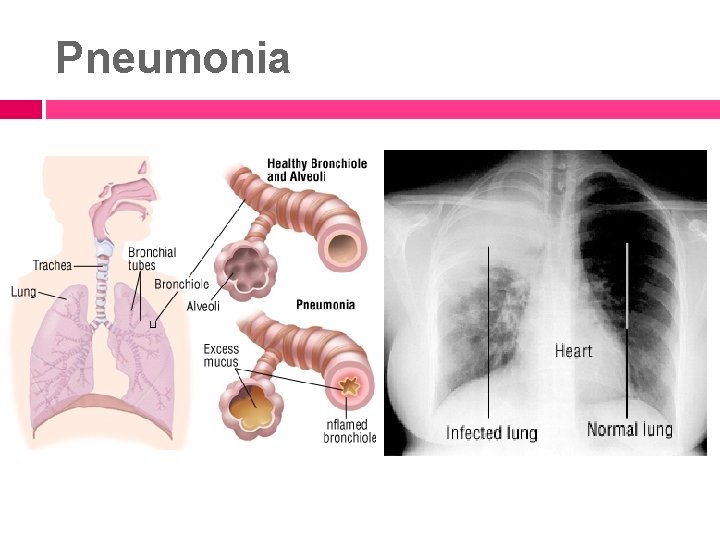
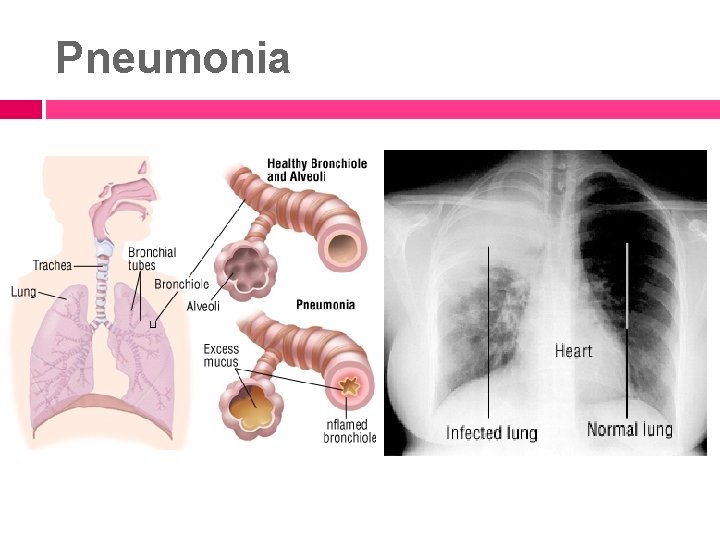
Pneumonia
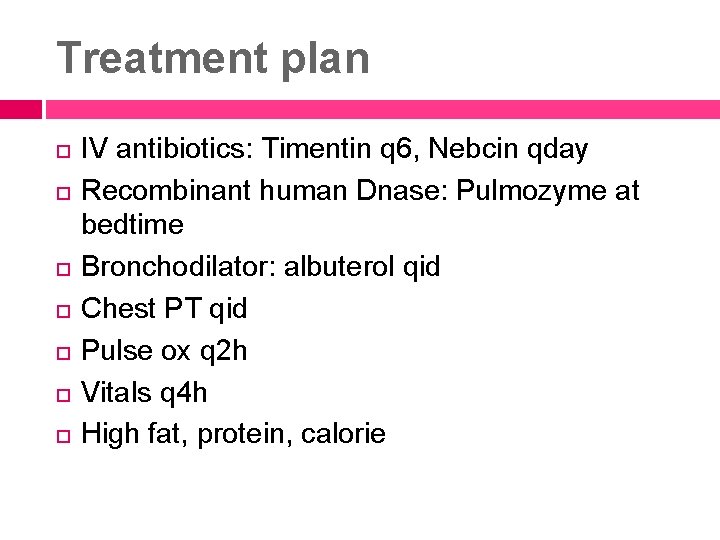
Treatment plan IV antibiotics: Timentin q 6, Nebcin qday Recombinant human Dnase: Pulmozyme at bedtime Bronchodilator: albuterol qid Chest PT qid Pulse ox q 2 h Vitals q 4 h High fat, protein, calorie
Client Assessment: Culture/Psychosocial/Family Heavy family involvement Always at least three members (usually more) in the room at all times Great grandmother, parents, aunt, older sister Family worked with the healthcare team during treatments to calm patient/provide valuable information about patient Financial issues? 4 other children, time off work
Client Assessment: Developmental Stage Erikson’s developmental theory “autonomy vs. shame and doubt” Toddler “gains independence with the family’s encouragement and learns to cooperate with others” (Craven & Hirnle, 2009, p. 248) Learns self control and independence by learning tasks such as potting training, choosing food preferences, choosing toy preferences Nurse must understand this stage of development to encourage the independence of the child so that they can master this stage and prevent “shame and doubt. ”

Client Assessment: Developmental Norms Tolerates some separation from parent Asks for objects by pointing Shakes head for “no” Uses cup well Walks without help Constantly casts objects to floor (Hockenberry & Wilson, 2011)

Client Assessment: Physical Neuro: alert and oriented Resp: clear sounds bilaterally, occasional wet cough, RR= 26, regular rhythm, unlabored. O 2 sat= 99% RA CV: HR= 87, regular rhythm, no murmurs/extra heart sounds noted, 2 second cap refill, palpable pulses +2 bilaterally. PICC L upper arm- dry &intact GI: Bowel sounds X 4, reducible umbilical hernia Gu: Diapered Skin: warm, no breakdown noted, moist mucous membranes Musc/skel: moves extremities X 4, anterior fontanelle open, soft Pain: 0

Identification of Nursing Problems: Concept Map 1. Risk for impaired gas exchange CF Pneumonia Wet cough Worsening cough/WOB 1 week prior to admission Rhinorrhea Albuterol Dornase Timentin Tobramycin
Identification of Nursing Problems: Concept Map 2. Imbalanced nutrition Higher metabolic demands from CF, pneumonia Stress from new environment Unavailability of child’s preferred soy milk Apple juice frequently Knowledge deficit of parents Weight between 5 th and 10 th percentile Duo. Cal
Identification of Nursing Problems: Concept Map 3. Risk for fluid imbalance On 9/7 an intake of 480 ml On 9/8 an intake of 660 ml CF; higher metabolic demands Pneumonia; higher metabolic demands Frequent apple juice: causes faster loss of stool/urine
Identification of Nursing Problems: Concept Map 4. Risk for infection PICC line Hospital setting Multiple specialists coming in and out of the room Multiple family members coming in and out of the room
Identification of Nursing Problems: Concept Map 5. Anxiety (of parents) Child’s recent diagnoses of CF Child’s hospitalization Child’s recent diagnoses of pneumonia
Plan of Care: Interventions/Expected Outcomes 1. Expected Outcome: Patient will maintain O 2 sats greater than or equal to 92% consistently prior to discharge. Assess O 2 sat q 2 hrs and prn Focused respiratory assessment q 4 hrs and before/after albuterol & CPT treatments: auscultate breath sounds, monitor for retractions and flaring. Obtain RR. Monitor effort of breathing. Teach parents about normal/abnormal respiratory findings, what to report immediately

Plan of Care: Interventions/Expected Outcomes 2. Expected Outcome: Patient will maintain or gain weight throughout hospitalization. Assess parent’s knowledge of nutrition Provide diet teaching to parents: a diet that is high in calories, fat & protein. Use of Duo. Cal in soymilk for added calories and nutrients. Monitor daily weights
Plan of Care: Interventions/Expected Outcomes 3. Expected Outcome: Patient will exhibit appropriate fluid balance consistently before discharge as evidenced by: capillary refill ≤ 2 sec, good skin turgor, clear-yellow colored urine, moist mucous membranes and blood pressure 67 -106/37 -63. Monitor I&O continually Encourage parents to promote healthy fluid intake Keep drink within reach of the child at all times Assess hydration q 4 h: color of urine, skin turgor, blood pressure, intake and output, assess mucous membranes, anterior fontanel, LOC, capillary refill.
Plan of Care: Interventions/Expected Outcomes 4. Expected Outcome: Patient will remain free from secondary infections during entire hospitalization as evidenced by a healthy PICC line site; free from drainage, redness, pain, and swelling. Assess PICC line site q 4 hrs and prn Monitor the child for signs of infection: restlessness, irritability, change in vital signs, increased work of breathing, fatigue, weight loss Monitor all vital signs q 4 h and prn
Plan of Care: Interventions/Expected Outcomes 5. Expected Outcome: Patient’s parents will demonstrate a decrease in anxiety as evidenced by: reporting decreased anxiety, being active with care of patient, and by acknowledging option of support group. Assess parent’s level of anxiety Provide teaching about patient’s disease process, status, and changes of status as much as possible Involve parents in care of the child, such as help with bathing, holding child while administering medications, etc Refer parents to CF support groups
Plan of Care: Discharge Planning Parent education: Nutrition teaching Monitoring weight Chest PT Signs and symptoms to report Routine immunizations Medication teaching
Research “The impact of behavioral intervention on family interactions at mealtime in pediatric cystic fibrosis” Aim: evaluate whether participation in “Be In Charge!”, a behavioral intervention designed to improve caloric intake and weight gain in children with CF, also results in improved family functioning during mealtimes Methods: 45 families of CF children 4 -12 Intervention group: “Be In Charge”: nutrition education and child behavioral management strategies Control group: “Nutrition Education”: nutrition education without behavioral management strategies

Research Data collection: Mealtime Family Interaction Coding System (MICS), Behavioral Pediatrics Feeding Assessment Scale (BPFAS), child’s weight. Mealtimes videotaped Results: Behavioral intervention: more positive responders (moving from unhealthy at baseline to healthy), significant improvement in affect management, positive impact on caloric intake Implications: importance of incorporating entire family when implementing dietary interventions, importance of incorporating praise/withdrawal of attention during meal times (Janicke, Mitchell, Quittner, Piazza-Waggoner, & Stark, 2008)
References Craven, R. , & Hirnle, C. (2009). Fundamentals of nursing. (6 th ed. ). Philadelphia, PA: Wolters Kluwer Health. Hocekenberry, J. M. , & Wilson, W. (2011). Wong’s Nursing Care of Infants and Children. (9 th ed. ). St. Louis, MO: Elsevier. Janicke, M. D. , Mitchell, M. J, Quittner, A. L. , Piazza. Waggoner, C. , & Stark, L. J. (2008). The impact of behavioral intervention on family interactions at mealtime in pediatric cystic fibrosis. Children’s Healthcare, 37(1) 49 -66.
Questions?
 Nursing grand rounds presentation example
Nursing grand rounds presentation example Utmb grand rounds
Utmb grand rounds Duke medicine grand rounds
Duke medicine grand rounds What is atraumatic care
What is atraumatic care Modern concept of pediatrics
Modern concept of pediatrics Perspective of pediatric nursing
Perspective of pediatric nursing Roles of a pediatric nurse
Roles of a pediatric nurse Pediatric nursing definition
Pediatric nursing definition Trends in pediatric nursing 2020
Trends in pediatric nursing 2020 What is atraumatic care
What is atraumatic care Sucking reflex disappear
Sucking reflex disappear Concepts of child care
Concepts of child care Quality teaching rounds coding sheet
Quality teaching rounds coding sheet Round of 75 to the nearest ten
Round of 75 to the nearest ten Harvard instructional rounds
Harvard instructional rounds Maintenance rounds
Maintenance rounds Red, white & blue bite size rounds tortilla chips
Red, white & blue bite size rounds tortilla chips What do you call a stubborn angle
What do you call a stubborn angle Schwartz rounds facilitator training
Schwartz rounds facilitator training Readiness rounds
Readiness rounds 5 layers of neurosis gestalt
5 layers of neurosis gestalt Rounds and fillets are usually dimensioned using
Rounds and fillets are usually dimensioned using Sam rounds
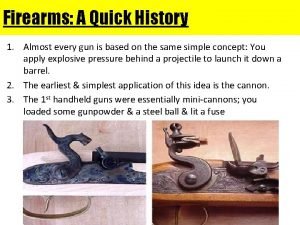
Sam rounds Bullet anatomy
Bullet anatomy A is an odd number which rounds to 100 000
A is an odd number which rounds to 100 000 Natalie maitre
Natalie maitre Natalie ertl
Natalie ertl