Pediatric Nursing Rounds MARIAN GEMENDER Introduction and Overview








- Slides: 25

Pediatric Nursing Rounds MARIAN GEMENDER
Introduction and Overview �Client: 21 -year-old male with cerebral palsy, mental retardation, and developmental delay Admitted for spinal fusion to treat scoliosis �Focus of presentation: Client history and assessment Nursing plan of care Applicable research �Techniques to obtain audience interest: Handout Discussion
Client History �Birth history Full-term birth C-section with Pitocin secondary to non-reassuring heart tones Suffered intracranial hemorrhage at this time �Heath history Quadriplegic with thoracolumbar curve 95 degrees to the right Scoliosis diagnosed 2 -3 years ago Allergies: Chloral hydrate �Past surgical history: G-tube Appendectomy for ruptured appendix
Cultural Considerations �Special needs child �Mother’s relationship with patient

Hospitalization �Chief reason for admission: Spinal fusion �Primary medical diagnosis: Idiopathic scoliosis �Relationship of secondary medical diagnoses: Children with cerebral palsy (CP) are at increased risk for developing scoliosis (Persson-Bunke, Hägglund, Lauge-Pedersen, Ma, & Westbom, 2012)
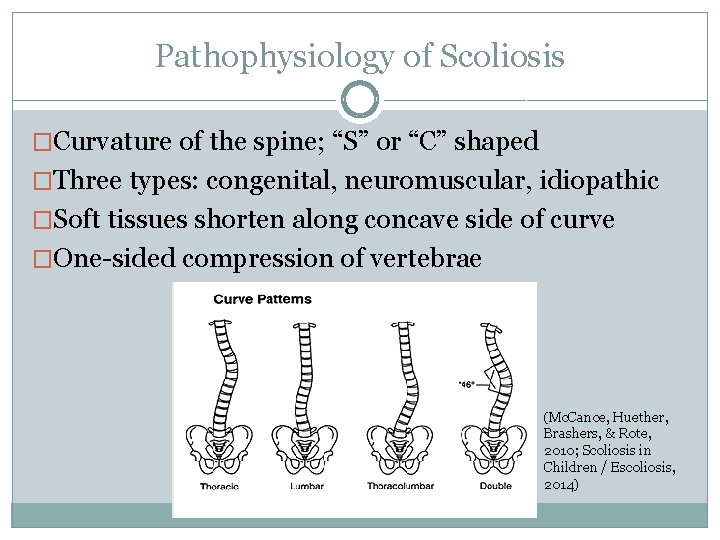
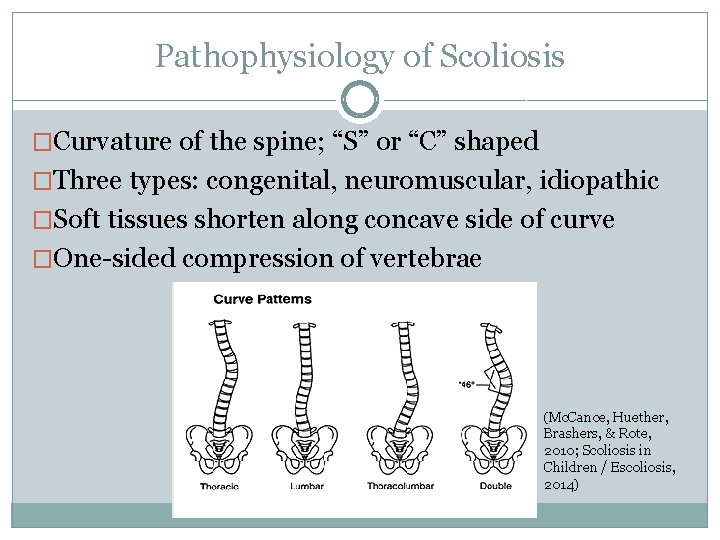
Pathophysiology of Scoliosis �Curvature of the spine; “S” or “C” shaped �Three types: congenital, neuromuscular, idiopathic �Soft tissues shorten along concave side of curve �One-sided compression of vertebrae (Mc. Cance, Huether, Brashers, & Rote, 2010; Scoliosis in Children / Escoliosis, 2014)
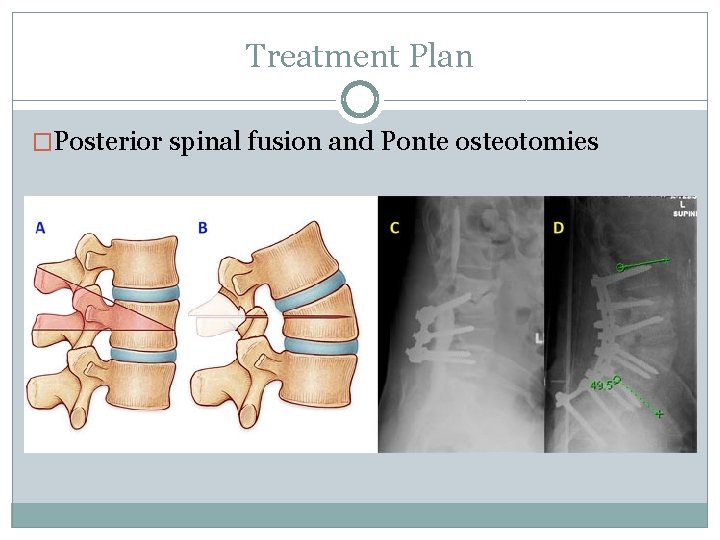
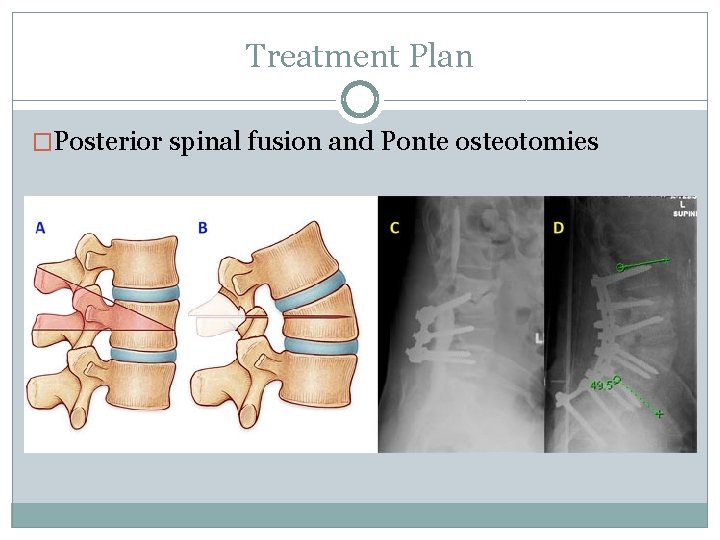
Treatment Plan �Posterior spinal fusion and Ponte osteotomies
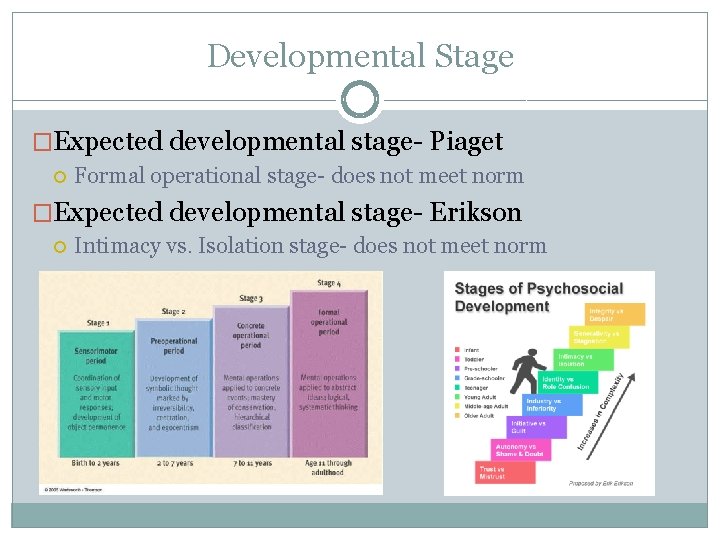
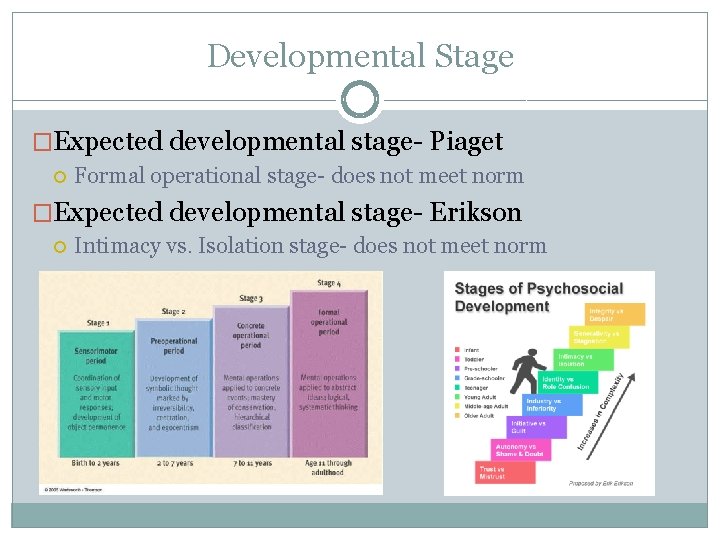
Developmental Stage �Expected developmental stage- Piaget Formal operational stage- does not meet norm �Expected developmental stage- Erikson Intimacy vs. Isolation stage- does not meet norm
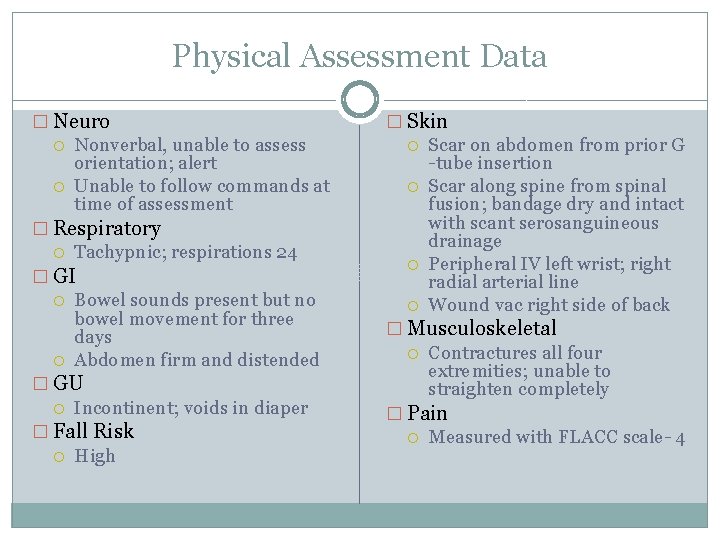
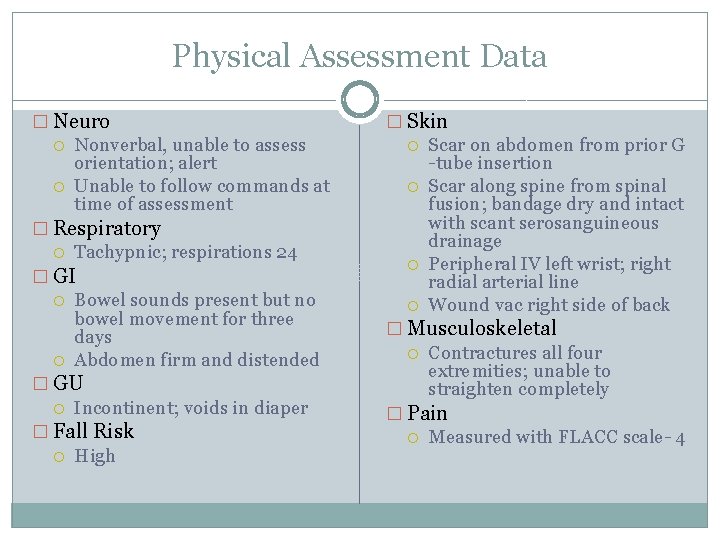
Physical Assessment Data � Neuro Nonverbal, unable to assess orientation; alert Unable to follow commands at time of assessment � Respiratory Tachypnic; respirations 24 � GI Bowel sounds present but no bowel movement for three days Abdomen firm and distended � GU Incontinent; voids in diaper � Fall Risk High � Skin Scar on abdomen from prior G -tube insertion Scar along spine from spinal fusion; bandage dry and intact with scant serosanguineous drainage Peripheral IV left wrist; right radial arterial line Wound vac right side of back � Musculoskeletal Contractures all four extremities; unable to straighten completely � Pain Measured with FLACC scale- 4
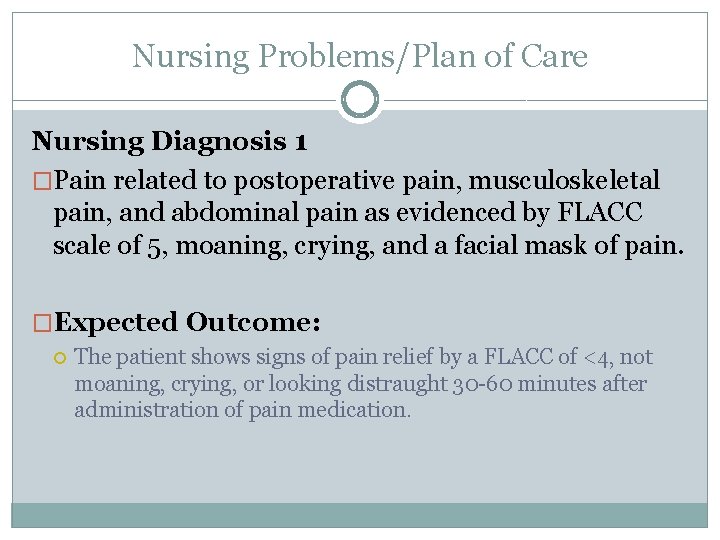
Nursing Problems/Plan of Care Nursing Diagnosis 1 �Pain related to postoperative pain, musculoskeletal pain, and abdominal pain as evidenced by FLACC scale of 5, moaning, crying, and a facial mask of pain. �Expected Outcome: The patient shows signs of pain relief by a FLACC of <4, not moaning, crying, or looking distraught 30 -60 minutes after administration of pain medication.

Nursing Diagnosis 1 �Nursing Interventions: Observe or monitor signs and symptoms associated with pain such as BP, heart rate, temperature, color and moisture of skin, and restlessness q 4 h. Assess for probable cause of pain. Evaluate patient's response to pain using FLACC with medications or therapeutics aimed at abolishing or relieving pain 30 to 60 minutes after administration and q 4 h. Evaluate for decreased moaning and crying. Monitor for changes in general condition that may herald need for change in pain relief method if current medications are not working within 30 to 60 minutes of administration. Anticipate the need for pain relief.
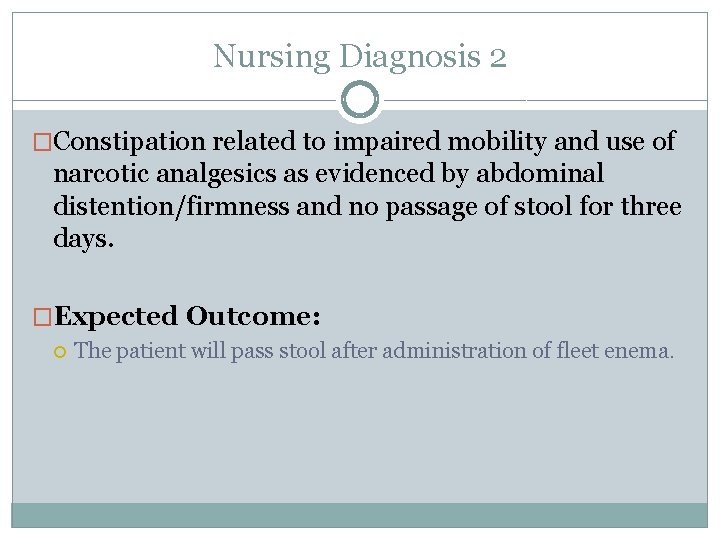
Nursing Diagnosis 2 �Constipation related to impaired mobility and use of narcotic analgesics as evidenced by abdominal distention/firmness and no passage of stool for three days. �Expected Outcome: The patient will pass stool after administration of fleet enema.
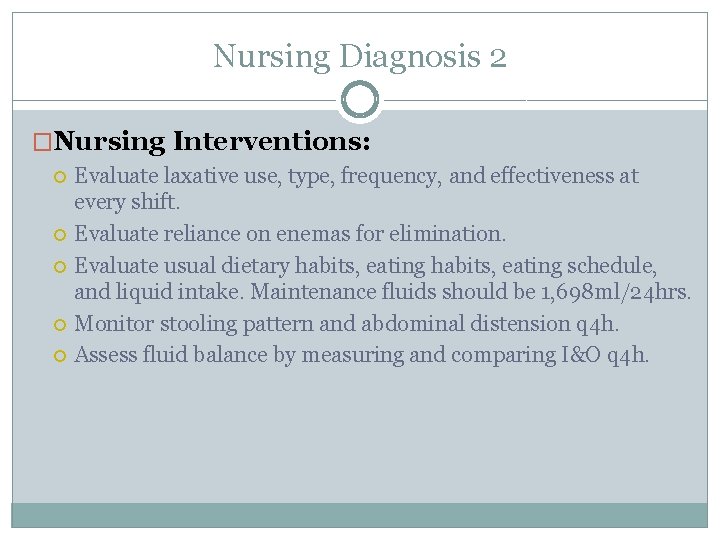
Nursing Diagnosis 2 �Nursing Interventions: Evaluate laxative use, type, frequency, and effectiveness at every shift. Evaluate reliance on enemas for elimination. Evaluate usual dietary habits, eating schedule, and liquid intake. Maintenance fluids should be 1, 698 ml/24 hrs. Monitor stooling pattern and abdominal distension q 4 h. Assess fluid balance by measuring and comparing I&O q 4 h.
Nursing Diagnosis 3 �Risk for infection related to an invasive procedure. �Expected Outcome: Patient remains free of infection throughout hospitalization, as evidenced by temperature between 36. 4 and 37. 4 degrees Celsius and absence of purulent drainage from wounds, incisions, and tubes
Nursing Diagnosis 3 �Nursing Interventions: Monitor for signs of infection q 4 h, including redness, swelling, increased pain, or purulent drainage at surgical site located along his spine. Also monitor temperature to see if it goes above 37. 4 degrees Celsius q 4 h. Maintain asepsis for dressing changes and wound care. Provide maintenance fluids 70. 75 ml/hr. Teach caregiver importance of washing hands often and how to use aseptic technique when caring for surgical site.

Nursing Diagnosis 4 �Risk for impaired skin integrity related to impaired mobility, incontinence, and healing surgical wound located along spine. �Expected Outcome: The patient’s skin remains intact as evidenced by no redness over bony prominences and capillary refill <2 seconds throughout hospitalization.
Nursing Diagnosis 4 �Nursing Interventions: Assess general condition of skin at the beginning of the shift to use as baseline. Specifically assess skin over bony prominences (sacrum, trochanters, scapulae, elbows, heels, inner and outer malleolus, inner and outer knees, back of head). Assess patient's nutritional status, including weight, weight loss, and fluid maintenance. Maintenance fluids should be 70. 75 ml/hr Encourage implementation of a turning schedule, restricting time in one position to 2 hours or less.
Nursing Diagnosis 5 �Parent knowledge deficit related to new procedure as evidenced by questioning members of the health care team. �Expected Outcome: Mother will verbalize that she feels comfortable caring for her child’s needs, including caring for the surgical site and monitoring his daily needs by discharge.

Nursing Diagnosis 5 �Nursing Interventions: Assess ability of mother to learn or perform post-operative care, paying attention to physical and psychological limitations. Question the mother regarding previous experience and health teaching to determine what she already knows. Provide clear instruction for specific topics such as using aseptic technique. Evaluate how much the mother knows after providing her with new information.
Holistic Nursing Care �Traditional Care Nursing assessment Medication administration Turning in bed Communication with family �Collaborative Care Surgical procedure (spinal fusion) Physical therapy �Complimentary/Alternative Care Massage therapy Acupuncture Music therapy

Relationship of Nursing Problems Constipation Pain Risk for impaired skin integrity Risk for infection Parent knowledge deficit

Discharge Planning �Follow up care- medications for pain and constipation �Schedule home health nurse as necessary �Schedule follow up visit �Fluids and nutrition �Teaching directed towards family How to safely transfer patient Teaching for infection prevention around surgical site Teach signs of infection
Nursing Research �Individualized Numeric Rating Scale (INRS) is geared toward nonverbal children with intellectual disability �Aim: at assessing pain in nonverbal children with intellectual disabilities �Population: parents of 50 children with intellectual disabilities going in for surgery �Results: Pain assessment of both bedside nurse and research nurse agreed with parent’s assessment (Solodiuk et al. , 2010) �Correlation: may provide a much more accurate pain assessment and could result in better pain management for patient if used

Summary �Introduction of patient �History and assessment �Developmental Stage �Nursing plan of care �Applicable nursing research
References Mc. Cance, K. L. , Huether, S. E. , Brashers, V. L. , Rote N. S. , (2010). Pathophysiology: The biologic basis for disease in adults and children. Maryland Heights: Mosby Elsevier Persson-Bunke, M. , Hägglund, G. , Lauge-Pedersen, H. , Ma, P. , & Westbom, L. (2012). Scoliosis in a total population of children with cerebral palsy. Spine, 37(12), E 708 -13. doi: 10. 1097/BRS. 0 b 013 e 318246 a 962 Scoliosis in Children / Escoliosis. (2014). Retrieved December 1, 2014, from http: // www. chkd. org/Patients-and-Families/Health-Library/Content. aspx? content. Type. Id=90&content. Id=P 02281 Solodiuk, J. , Scott-Sutherland, J. , Meyers, M. , Myette, B. , Shusterman, C. , Karian, V. , &. . . Curley, M. (2010). Validation of the Individualized Numeric Rating Scale (INRS): a pain assessment tool for nonverbal children with intellectual disability. Pain (03043959), 150(2), 231 -236. doi: 10. 1016/j. pain. 2010. 03. 016
 Nursing grand rounds presentation example
Nursing grand rounds presentation example Tabular dimensioning
Tabular dimensioning Trends in pediatric nursing
Trends in pediatric nursing Modern concepts of child care
Modern concepts of child care Current concept of pediatric nursing
Current concept of pediatric nursing Paediatric nurse
Paediatric nurse Autramatic care
Autramatic care Autramatic care
Autramatic care Perspective of pediatric nursing
Perspective of pediatric nursing Pediatric nursing definition
Pediatric nursing definition Sucking reflex disappear
Sucking reflex disappear What is bioinformatics an introduction and overview
What is bioinformatics an introduction and overview Utmb grand rounds
Utmb grand rounds Round 75
Round 75 Christmas table quiz seomra ranga
Christmas table quiz seomra ranga Layers of neurosis gestalt
Layers of neurosis gestalt A is an odd number which rounds to 100 000
A is an odd number which rounds to 100 000 Maintenance rounds
Maintenance rounds Schwartz rounds facilitator training
Schwartz rounds facilitator training Sam rounds
Sam rounds Quality teaching rounds coding sheet
Quality teaching rounds coding sheet Red white and blue tortilla chips
Red white and blue tortilla chips Readiness rounds
Readiness rounds Breech face gun
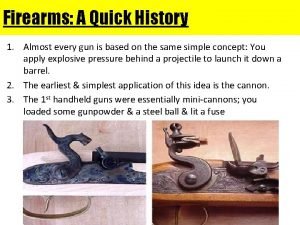
Breech face gun Harvard instructional rounds
Harvard instructional rounds Duke medicine grand rounds
Duke medicine grand rounds