Corinne Mayer Nursing 421 Pediatric Grand Rounds Presentation



- Slides: 27
Corinne Mayer Nursing 421 Pediatric Grand Rounds Presentation Old Dominion University
“Tiny Tim” 2 Months Old TOF with severe right outflow tract obstruction status post BT shunt
Patient Health History “Tiny Tim” 2 Month old Trisomy 21 Gastroesophageal reflux Chronic lung disease Anemia of prematurity Congenital hypothyroidism Immature retinae 33 week gestation infant Hospitalized since birth
Psychosocial History and Cultural Considerations Adopted One other Trisomy 21 child with TOF 4 other children Culture of being adopted Culture of NICU and PICU Culture of Trisomy 21
Trisomy 21 “Down Syndrome” Most common chromosomal abnormality of a generalized syndrome, occurs in 1 out of 733 live births. Extra chromosome 21 Cause unknown Genetic predisposition Exposure to radiation before conception Immunologic problems Infection Age=women over the age of 35 are at greater risk
Clinical Manifestations Intelligence—varies from severe CI to low-average intelligence Social development 2 -3 years beyond mental age “Easy Child” temperament Sensory problems—ocular problems and hearing loss Growth--delayed Congenital abnormalities— 40 -45% have congenital heart disease. TOF
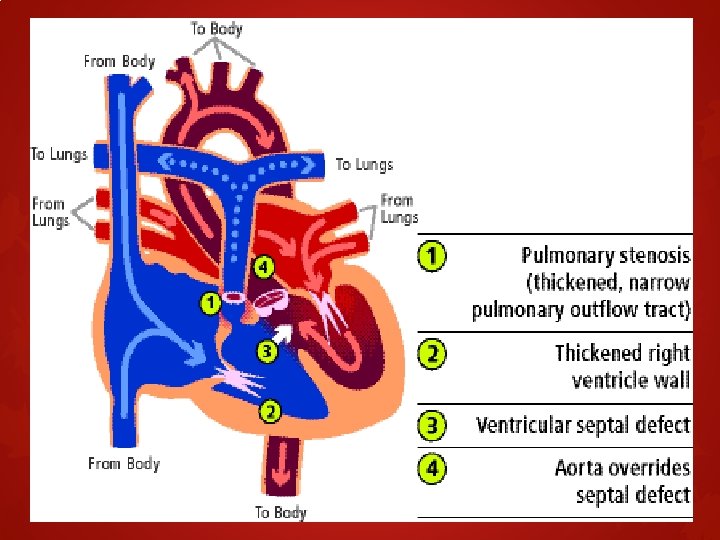
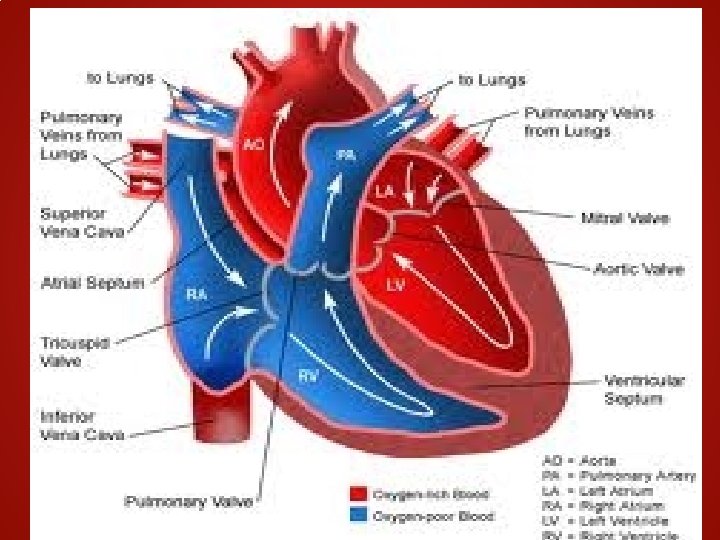
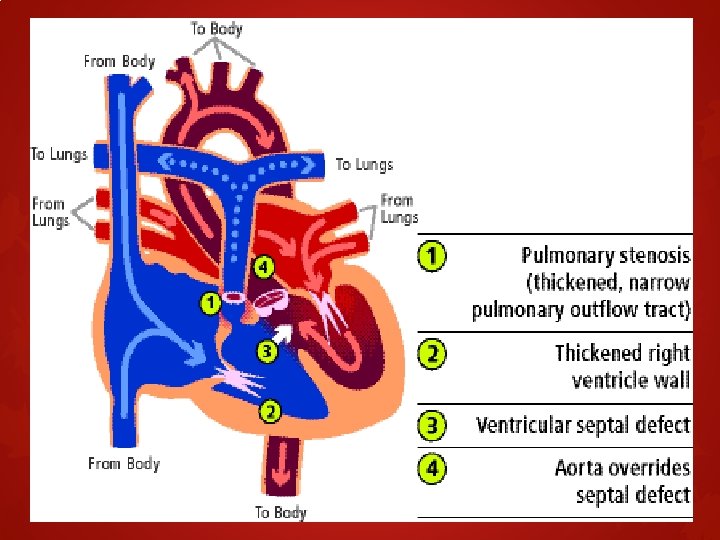
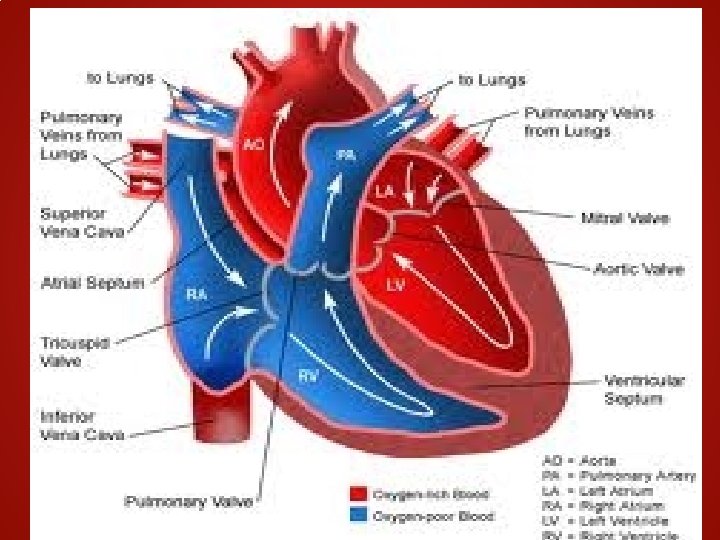
Tetrology of Fallot Four heart defects of the heart Ventricular septal defect Narrowing of the pulmonary outflow tract Overriding aorta shifted over the right ventricle and ventricular septal defect instead of just the left ventricle Right ventricular hypertrophy
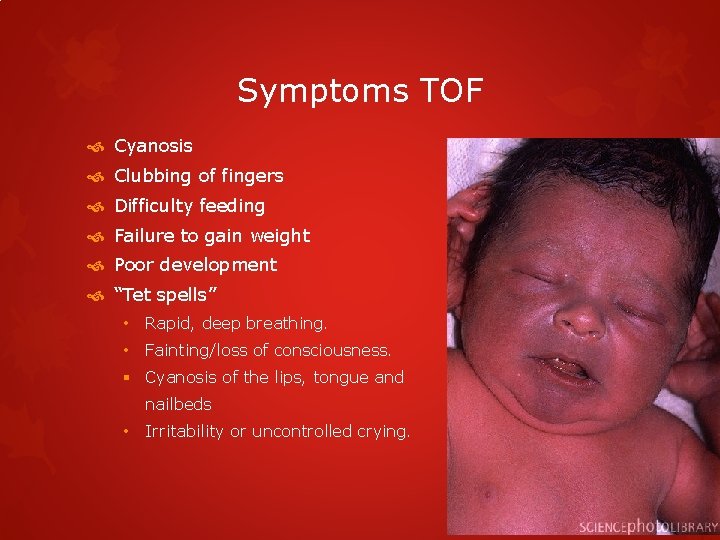
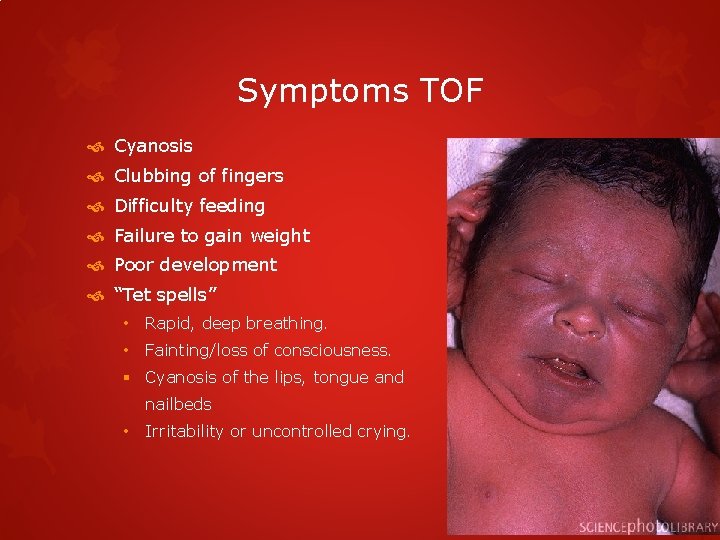
Symptoms TOF Cyanosis Clubbing of fingers Difficulty feeding Failure to gain weight Poor development “Tet spells” • Rapid, deep breathing. • Fainting/loss of consciousness. § Cyanosis of the lips, tongue and nailbeds • Irritability or uncontrolled crying.
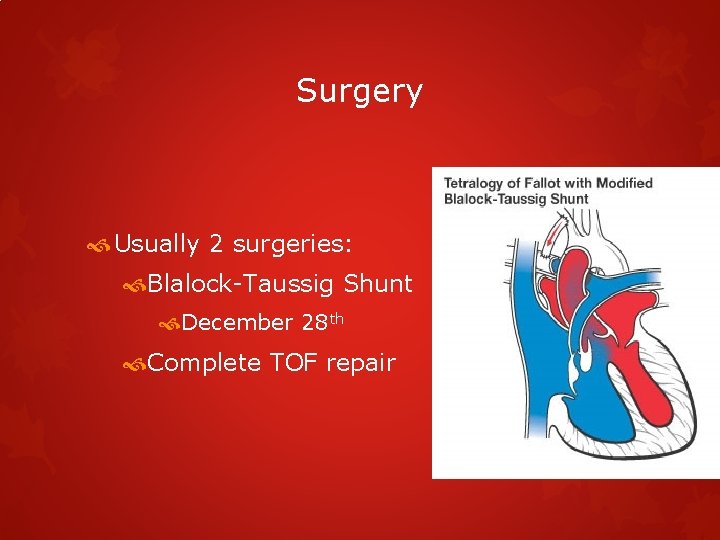
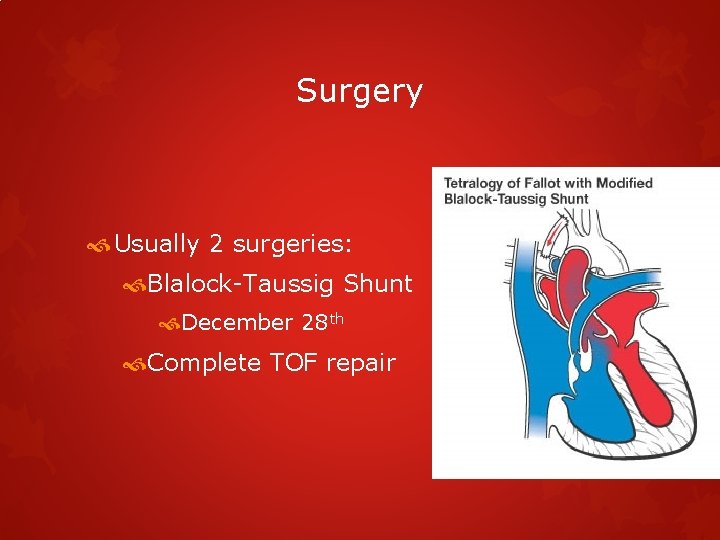
Surgery Usually 2 surgeries: Blalock-Taussig Shunt December 28 th Complete TOF repair
Hospitalization at CHKD Reason for admission: Possible shunt stenting due to Multiple oxygen saturations in the 60’s% Serial echocardiograms at NMCP were concerning Plan of care: Surgery to correct narrowing shunt Possible complete repair of TOF Maintenance care until surgery
Developmental Stage Personal and social Begins to recognize caregivers Smiles spontaneously Speech and Language Cries to express displeasure Make comforting sounds during feeding Fine Motor Hands predominantly closed Clenches hands around rattle Gross Motor Can turn head from side to side when prone Assumes flexed position with pelvis high but knees under abdomen when prone

Developmental Stage Developmentally delayed Does not: Recognize or smile at caregivers Hold head up unassisted Swallowing reflex delayed Make “cooing” sounds or comfort sounds when feeding Does not follow objects with eyes G rasp toys or rattles
Developmental Theory Erikson’s Theory of Psychosocial Development Trust vs Mistrust Can I trust caregivers? Care Comfort when crying or agitated Change diapers promptly Holding Talking
Physical Assessment Respiratory: Maintaining expected oxygen saturation between 75 -85 2 L High Flow Nasal Canula Cardiovascular TOF: at risk for “Tet spells” Systolic murmur Endocrine Hypothyroidism GI Failed swallow screen so patient is on NJ tube with continuous feeding
Physical Assessment Neuro Fontanel soft and slightly distended Patient failed swallow screen, so NJ tube is in place Musculoskeletal moves all extremities well, brings hand to mouth Pain No s/s of pain or agitation Psychosocial Parents not at bedside Vital signs: Temp- 36. 0, HR- 135, RR- 30, BP- 96/42, O 2 - 77%
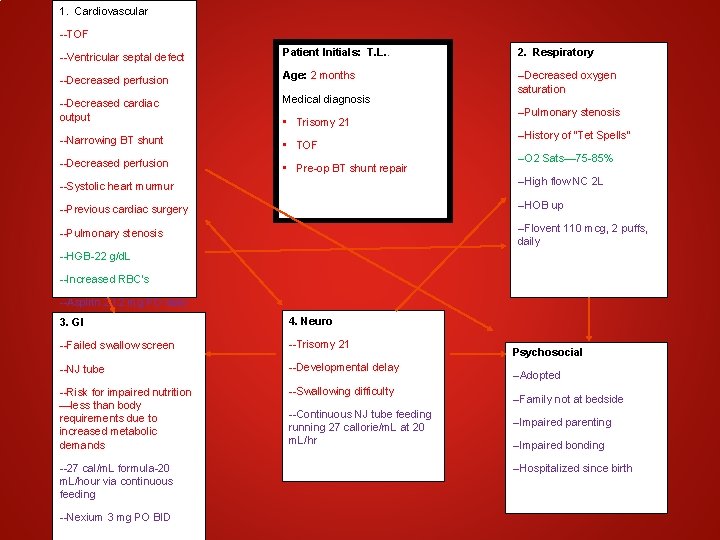
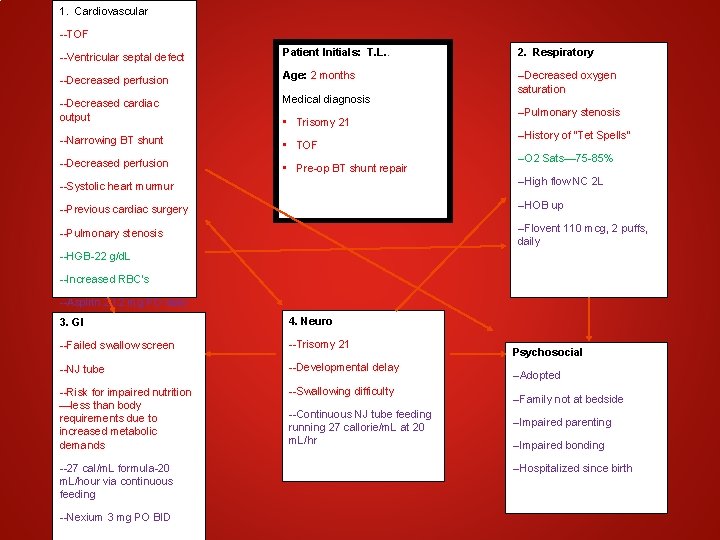
1. Cardiovascular. V --TOF --Ventricular septal defect Patient Initials: T. L. . 2. Respiratory 2. Resp --Decreased perfusion Age: 2 months --Decreased cardiac output Medical diagnosis. Diagnoses: --Decreased oxygen saturation --Narrowing BT shunt • TOF --Decreased perfusion • Pre-op BT shunt repair • Trisomy 21 --Pulmonary stenosis --History of “Tet Spells” --O 2 Sats— 75 -85% --Systolic heart murmur --High flow NC 2 L --Previous cardiac surgery --HOB up --Pulmonary stenosis --Flovent 110 mcg, 2 puffs, daily --HGB-22 g/d. L --Increased RBC’s --Aspirin 20. 2 mg PO daily 3. GI 4. Neuro --Failed swallow screen --Trisomy 21 --NJ tube --Developmental delay --Risk for impaired nutrition —less than body requirements due to increased metabolic demands --Swallowing difficulty --27 cal/m. L formula-20 m. L/hour via continuous feeding --Nexium 3 mg PO BID --Continuous NJ tube feeding running 27 callorie/m. L at 20 m. L/hr Psychosocial --Adopted --Family not at bedside --Impaired parenting --Impaired bonding --Hospitalized since birth
Expected Outcomes Cardiovascular Patient will remain free of tet spells by the end of shift. Respiratory Patient respiration rate will remain between 30 -60 breaths per minute and oxygen saturation will remain between 75 -85% GI Patient will receive and tolerate 100% of continuous feedings throughout the shift
Expected Outcomes Neuro Patient will remain free from choking spells by end of the shift. Patient will pass a swallow screen by discharge Psycosocial Patient’s parents will assist staff with patient care and comfort pre and post operatively
Patient Care Traditional Interventions Monitor intake and output Monitor vital signs every hour per PICU protocol Monitor respiratory status Monitor and administer continuous NJ feeding Perform physical assessment and report any changes Provide hygiene including diaper changes Monitor weight Provide a safe environment Elevate HOB 30 degrees to encourage gas exchange and cardiac output Assess skin for breakdown Administer medications

Complementary Provide comfort measures such as swaddling and pacifier Provide a quiet environment Provide distraction by turning on mobile or playing music Massage patient during times of anxiety Provide support to family Collaborative Communicating changes with healthcare team during rounds. Collaborating care among social work if needed. Assist in coordinating any at home care if needed.
Teaching Developmental delays of Trisomy 21 Post-operative care Importance of bonding in the hospital Characteristics of decreased cardiac output Characteristics of pain Discharge Planning Support groups Continuity of care Home health care? Where to find or assist in coordingating developmental programs in the area such as Parent to Parent of Virginia
High Flow Nasal Cannula What is it? Ordinary nasal cannula that delivers a higher flow of 100% oxygen. Delivers positive airway pressure Thermally controlled Delivers > 95% relative humidity Benefit Less restricting than oxygen mask Better patient tolerance Minimizes the risk of needing invasive ventilation Decreases airway inflammation Hydrates thickened secretions
Research “Skin Integrity in Critically Ill and Injured Children” Determine the incidence of skin breakdown in critically ill and injured children 401 stays in the PICU at the Children’s Hospital of Wisconsin Skin breakdown in 8. 5% Redness in 6. 2% Breakdown and redness in 3. 2% Overall incidence— 18% Younger age and longer stay in the PICU was associated with increased risk. Also more likely to more at risk to have respiratory illness and require mechanical ventilatory support
Questions? ?

References Hockenberry, M. J. , & Wilson, D. (2011). Nursing care of infants and (9 th ed. ). St. Louis, Missouri: Elsevier Mosby. Davis, D. , & Clifton, A. (1995). Psychosocial theory: Erikson. Retrieved http: //www. haverford. edu/psych/ddavis/p 109 g/erikson. stages. html children. from Leaderstorf, M. , Pastore, J. , Wagner, S. , & Kramer, B. (2010, December 10). High flow nasal cannula; history of usage at wchob. Retrieved from http: //www. wchob. org/grandrounds/pdfs/grand_Rounds_121010. pdf Nasal Cannula. (n. d. ). High flow nasal cannula. Retrieved from http: //nasalcannula. net/high-flow-nasal-cannula/ Parent to Parent of Virginia. (n. d. ). Resources. Retrieved from http: //www. ptpofva. com/4 -resources. html Schindler, C. A. , Mikhailov, T. A. , Fischer, K. , Lukasiewicz, G. , Kuhn, E. M. , & Duncan, L. (2007). Skin integrity in critically ill and injured children. American Journal of Critical Care, 16(6), 568 -574. Texas Children's Hospital. (2011). Pediatric heart surgery; congenital heart defects: tetralogy of fallot. Retrieved from http: //www. texaschildrens. org/carecenters/heart/surgery/tetralogy of fallot. aspx