Pathology Dentistry Hemodynamic Disorders Dr Tariq Aladily tnaladilyju
- Slides: 40
Pathology – Dentistry Hemodynamic Disorders ﻃﺎﺭﻕ ﺍﻟﻌﺪﻳﻠﻲ. ﺩ Dr. Tariq Aladily tnaladily@ju. edu. jo Office hours: Sunday 12 -1 Hematology Lab, JUH
Hyperemia and congestion Hyperemia: • Increased intravascular blood volume in a tissue • Secondary to arteriolar dialtion (O 2 blood) • Physiologic: exercise • Pathologic: inflammation
Congestion • • Passive process, pathologic Impaired venous blood outflow from tissue Systemic: cardiac failure Localized: local venous obstruction Deoxygenated blood (blue-red) Lead to hypoxia, tissue death, fibrosis (chronic) Also increased intravascular pressure, capillary rupture, tissue edema and hemorrhage (acute)
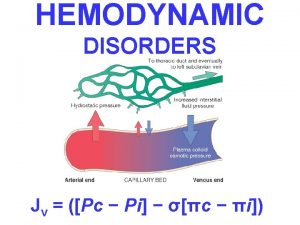
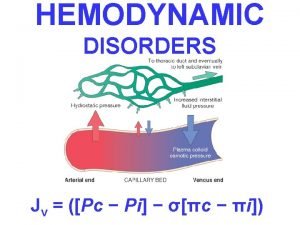
Edema 60% of lean body weight is water Two thirds is intracellular One third is extracellular (interstitial fluid) Only 5% of the body’s water is in blood plasma Edema is an accumulation of interstitial fluid within tissues • Extravascular fluid can also collect in body cavities such as the pleural cavity (hydrothorax), the pericardial cavity (hydropericardium), or the peritoneal cavity (hydroperitoneum, or ascites) • Anasarca is severe, generalized edema marked by profound swelling of subcutaneous tissues and accumulation of fluid in body cavities • • •
Fluid movement Governed by: • Arterioral hydrostatic pressure • Venous osmotic pressure • Small portion stays in interstitium (goes to lymphatic)
Normal circulation in the capillary • Hydrostatic pressure: blood reaches the capillary in a high speed, because of this, and because the capillary is smaller than the arteriole, part of blood plasma exits outside into the tissue carrying nutrients • Osmotic pressure: after the plasma exits, the remaining proteins in the blood become more concentrated as the fluid became less. This creates an increased osmotic pressure inside the capillary and attracts the plasma which already exited. Plasma returns again inside the venule carrying waste and CO 2 • Not all the plasma that exited the arteriole returns back, a small part remains in the tissue. This part exit the tissue into the lymphatic system
Increased hydrostatic pressure • Deep venous thrombosis in lower limbs – localized edema • Congestive heart failure - generalized
Reduced osmotic pressure • Nephrotic syndrome (loss of albumin) • Chronic liver disease (no synthesis of proteins) • Protein malnutrition • In both settings (increased hydrostatic and low osmotic pressures) there is renal hypoperfusion and increased aldosteron level, which worsens edema. • The fluid is called transudate, which has low amount of proteins
Lymphatic obstruction • Localized: • infections (fliaria) • tumors (breast cancer – orange peel skin)
Morphology of edema • Subcutaneous tissue, lung, brain are most common sites • Subcutaneous edema favors farthest sites from the heart (legs, sacrum) called dependant edema • Edema secondary to renal diseases favors loose connective tissue (eyelids) called periorbital edema • Lung edema: weighs 2 -3 times, frothy and bloody • Brain edema: sulci are narrowed, gyri are swollen
Hemorrhage • Extravasation of blood from vessels • Hemorrhagic diathesis: group of diseases in which the patient has a risk of hemorrhage • Chronic congestion leads to capillary bleeding • Large vessel bleeding occur in trauma, atherosclerosis, inflammation and neoplastic erosion
Hematoma • Accumulation of extravascular blood within tissue • Can be trivial (e. g. bruise) • Can be fatal (retroperitoneal hematoma) • Bleeding into body cavities gives bloody fluid, called hemothorax, hemopericardium, hemoperitoneum, hemoarthrosis (into joints) • Patients later develop jaundice, secondary to massive breakdown of hemoglobin in RBCs
Ecchymoses (bruise) • Large subcutaneous hematoma • Extravasated RBCs are phagocytosed by macrophages • Begins as red-blue color • Then blue-green (bilirubin) • Eventually golden-brown (hemosiderin)
Clinical significance of hemorrhage • Rapid loss of small amount (up to 20% of blood volume) or slow loss of larger amount may have little impact in healthy adult • Larger loss leads to hemorrhagic shock secondary to hypovolemia • The site of hemorrhage is important, bleeding in brain can be fatal even if the amount is small • Chronic and recurrent bleeding results in anemia and iron loss
Hemostastis • Definition: Arrest of bleeding • Hemostasis depends on the integrity of: – Blood vessels – Platelets – Coagulation factors – Anticoagulation factors First response after vessel injury: Neurogenic reflex, augmented by local endothelin release, causes arteriolar constriction
Primary hemostasis • Endothelial injury exposes highly thrombogenic subendothelial extracellular matrix (ECM), facilitating platelet adherence, activation, and aggregation. The formation of the initial platelet plug is called primary hemostasis • Endothelial injury also exposes and secrete tissue factor (also known as factor III or thromboplastin), a membrane-bound procoagulant glycoprotein synthesized by endothelial cells. Exposed tissue factor, acting in conjunction with factor VII, is the major in vivo trigger of the coagulation cascade and its activation eventually culminates in the activation of thrombin, which has several roles in regulating coagulation.
• Activated thrombin promotes the formation of an insoluble fibrin clot by cleaving fibrinogen; thrombin also is a potent activator of additional platelets, which serve to reinforce the hemostatic plug. This sequence, termed secondary hemostasis, results in the formation of a stable clot capable of preventing further hemorrhage • As bleeding is controlled, counterregulatory mechanisms (e. g. , factors that produce fibrinolysis, such as tissue-type plasminogen activator) are set into motion to ensure that clot formation is limited to the site of injury
Endothelial function • balance between the anti- and prothrombotic activities • Normal endothelial cells express a variety of anticoagulant factors that inhibit platelet aggregation and coagulation and promote fibrinolysis • After injury or activation, however, this balance shifts, and endothelial cells acquire numerous procoagulant activities • Besides trauma, endothelium can be activated by microbial pathogens, hemodynamic forces, and a number of pro-inflammatory mediators.
Antiplatelet • Nitric oxide (NO) • Prostacyclin (PGI 2) • Adenoside diphosphatase (cleaves ADP)
Anticoagulation • Heparin-like molecules: activates antithrombin III, which inhibits thrombin • Thrombomodulin: binds thrombin and prevents its function it, also activates protein C (anticoagulant) • Protein S: a cofactor for protein C • Protein C inhibits factors V and VIII
Fibrinolysis • Tissue-type plasminogen activator: converts plasminogen into plasmin, which cleaves fibrin
Prothrombotic activities • Always follows endothelial injury
Activation of clotting factors • In response to tumor necrosis factor (TNF), interleukin-1 (IL-1) or bacterial products, endothelium produces tissue factor (TF) and decrease production of thrombomodulin • Direct activation of factors IX and X, which lead to activation of thrombin
Antifibrinolytic effect • Secrete plasminogen activator inhibitor (PAI), which limits fibrinolysis and favor thrombosis
Thrombosis • Occur when: • 1) endothelial damage (smoking, hypertension, hyperlipidemia, infection) • 2) abnormal blood flow (turbulence), mainly in heart and arteries • 3) blood stasis, mainly in veins
Hypercoaguability • Alteration in coagulation pathway that predisposes the person to thrombosis • Mostly venous • Primary (genetic) • Secondary (acquired)
Primary thrombophilia • Factor V (Leiden) mutation: resistant to inhibition by protein C • Prothrombin gene mutation: increased function of prothrombin protein
Secondary thrombophilia • • • Chronic congestion (heart failure) Abnormal turbulence (heart arrhythmia) Pregnancy Advanced cancer Drugs (oral contraceptives)
Morphology of thrombus • focally attached to vascular wall • Tend to propagate toward the heart (arterial thrombus grows retrograde) • Propagating part is loosely attached, tend to detach and move in blood circulation (embolus) • Lines of Zahn: alternation of light (platelets and fibrin) lines with dark ones (RBCs) in thrombi • Post mortum thrombus: loosely attached to vessel wall, contain yellow part (chicken fat), no lines of Zahn
Fate of thrombus • • Probagation Embolization Dissolution Organization and canalization
Embolism • Intravascular solid, liquid or gas mass that is carried by the blood to a distant site • Most commonly arise from a dislodged thrombus (called thromboembolism)
Pulmonary embolism • Arises from deep venous thrombosis (DVT) • Detached thrombus moves into the right side of the heart, then to the lung • If large, will occlude the bifurcation of the pulmonary artery (saddle embolus), causes death • Smaller emboli moves to arterioles, commonly multiple
• 60 -80% of emboli are small and clinically silent • Large embolus causes sudden death • Medium sized embolus causes capillary rupture, pulmonary hemorrhage, pulmonary infarction • Multiple recurrent small emboli will cause pulmonary hypertension and right sided heart failure
Systemic thromboembolism • Mostly arises from intracardiac “mural” thrombi • Less commonly from aortic aneurysm (abnormal large dilation of part of the aorta) • Causes arterial thrombi, can lodge anywhere, most commonly to lower limbs (80%), then CNS (10%)
Fat embolism • Occur in soft tissue crush injury, or long bone fracture • Microscopic fat is released into circulation • Only 10% of cases develop symptoms: 1 -3 days after injury as tachypnea, tachycardia, coma • Causes direct physical occlusion, and platelets aggregation
Amniotic fluid embolism • Uncommon, grave complication of labor • 80% mortality • Amniotic fluid, containing shed squamous cells and hair from the fetus, enters the maternal circulation • Severe dyspnea, cyanosis, hypotensive shock, followed by seizure and coma
Air embolism • Gas bubbles within circulation can coalesce and obstruct vascular flow • During coronary artery or brain surgery • Small venous air emboli are generally not deleterious • Large emboli can arrest the heart and cause sudden death
Infarction • Ischemic necrosis secondary to vascular occlusion • Caused by thrombosis, embolism, vasospasm, tumor, edema • Tissue shows inflammation • Can be infected • Brain infarction show liquifactive necrosis (exception)
Red infarcts • • • Occur in venous occlusion Loose tissue (lung) Organs with dual blood supply (lung, intestine) Previously congested tissue If blood flow is reestablished
White infarcts • Arterial occlusion • Solid organs (heart, spleen, kidneys) • Infarcts appear as wedge shaped
 Nutmeg liver
Nutmeg liver Cerebral infarction
Cerebral infarction Hemodynamic disorders
Hemodynamic disorders Hemodynamic disorders
Hemodynamic disorders Robbins
Robbins Edema lesion
Edema lesion Difference between hyperemia and congestion
Difference between hyperemia and congestion Kalsoom tariq
Kalsoom tariq Imtashal tariq
Imtashal tariq Dr tariq ashraf
Dr tariq ashraf Tariq salameh
Tariq salameh Telle tariq
Telle tariq Diya scholarship
Diya scholarship Dynapulse
Dynapulse Hemodynamic monitoring system
Hemodynamic monitoring system Swan catheter
Swan catheter Proximal lumen
Proximal lumen Pinsky hemodynamic monitoring
Pinsky hemodynamic monitoring Female reproductive system pathology
Female reproductive system pathology Spine pathology
Spine pathology Dohányos tüdő
Dohányos tüdő What pathology
What pathology Pathology visions
Pathology visions Warthin's tumor
Warthin's tumor Benign nephrosclerosis pathology outlines
Benign nephrosclerosis pathology outlines Prostate pathology
Prostate pathology Types of necrosis
Types of necrosis Destructive pathology
Destructive pathology Anatomical pathology definition
Anatomical pathology definition Seed pathology definition
Seed pathology definition Cryptology and pathology
Cryptology and pathology Pathology
Pathology Driven snow appearance
Driven snow appearance Clinical pathology accreditation
Clinical pathology accreditation Dr. heidi shea
Dr. heidi shea Tronsmo plant pathology and plant diseases download
Tronsmo plant pathology and plant diseases download Status asthmaticus pathophysiology
Status asthmaticus pathophysiology Oral pathology
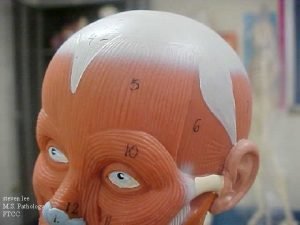
Oral pathology Hysterosalpingoophorectomy
Hysterosalpingoophorectomy Gross pathology
Gross pathology Certificate in pathology collection
Certificate in pathology collection