PARTURITION The physical effort of expulsion of the



- Slides: 22
PARTURITION
• The physical effort of expulsion of the fetus and the placenta from the uterus. • Labor: The strong, rhythmic contractions of the uterus that result in birth. • The total gestation period from fertilization to birth is about 38 weeks (birth usually occurring 40 weeks after the last menstrual period). • The end of the third trimester, estrogen causes receptors on the uterine wall to develop and bind the hormone oxytocin.
• The baby reorients, facing forward and down with the back or crown of the head engaging the cervix (uterine opening). • This causes the cervix to stretch, sending nerve impulses to the hypothalamus, which signals for the release of oxytocin from the posterior pituitary. • The oxytocin causes the smooth muscle in the uterine wall to contract. • The placenta releases prostaglandins into the uterus, increasing the contractions.

COMMON SIGNS OF LABOUR • Common signs of labour, • Lightening describes the baby moving down from the rib cage with the head of the baby engaging deep in the pelvis. • The pregnant woman may then find breathing easier since her lungs have more room for expansion. • Pressure on bladder may cause more frequent need to void (urinate).
• Some women also experience an increase in vaginal discharge several days before labour begins when the "mucus plug", a thick plug of mucus that blocks the opening to the uterus, is pushed out into the vagina. • Amniotic sac Shortly before, at the beginning of, or during labor the sac ruptures. Once the sac ruptures, termed "the water breaks", the baby is at risk for infection and the mother's medical team will assess the need to induce labor if it has not started within the time they believe to be not safe for the infant.
Dilation • The first stage of parturition starts with the onset of labor It continues until the cervix is fully dilated. This dilation is divided into two phases: • Latent phase. The cervix is 0 to 4 centimeters (cm) dilated. • Active phase. The cervix is 4 to 10 cm dilated. • The latent phase takes about six hours for a woman who’s giving birth for the first time. It takes around five hours for a woman who’s given birth previously. For some women, the latent phase may last 8 to 12 hours. • During the active phase, it’s expected that the cervix will dilate at a rate of about 1 cm per hour for a woman who’s giving birth for the first time. For a woman who’s previously had a vaginal delivery the rate is typically about 2 cm per hour.
• Engagement of the foetal head in the transverse position. The baby's head is facing across the pelvis at one or other of the mother's hips • Descent and flexion of the foetal head. • Internal rotation. The foetal head rotates 90 degrees to the anterior position so that the baby's face is towards the mother's rectum • Delivery by extension. The foetal head is bowed, chin on chest, so that the back or crown of its head leads the way through the birth canal, until the back of its neck presses against the pubic bone and its chin leaves its chest, extending the neck—as if to look up, and the rest of its head passes out of the birth canal. • Restitution. The foetal head turns through 45 degrees to restore its normal relationship with the shoulders, which are still at an angle. • External rotation. The shoulders repeat the corkscrew movements of the head, which can be seen in the final movements of the foetal head.

Expulsion • The second stage of parturition starts at full dilation and continues until birth. This stage also has two phases: • Passive phase. The baby’s head moves down through the vagina. • Active phase. The mother feels a need to push, or contract the abdominal muscles in time with uterine contractions. • The active phase lasts about 45 minutes for a woman who’s having her first baby. For women who’ve had a vaginal delivery, the active phase lasts about 30 minutes. • Stage 2 ends with the birth of the baby. • At this point, the umbilical cord is clamped, and breastfeeding is often encouraged to help with stage 3.
Placental • The third stage of parturition starts after birth and ends with the delivery of the afterbirth (placenta and membranes). • If the doctor takes an active role — including gently pulling on the placenta — stage 3 typically takes around five minutes. If the placenta is delivered without assistance, stage 3 can last around 30 minutes.
• With the expulsion of the child, the cavity of the uterus is greatly diminished. • As a consequence, the site of placental attachment becomes markedly reduced in size, with the result that the placenta (afterbirth) is separated in many places from the membrane lining the uterus. • Within a few minutes subsequent uterine contractions complete the separation and force the placenta into the vagina, from which it is expelled by a bearing-down effort. • Occasionally, the separation may be delayed and accompanied by bleeding, in which case surgical removal of the placenta is necessary.
Complications during childbirth Fetal distress typically refers to a slowdown in the baby’s heart rate. A doctor usually addresses this by using a vacuum extractor or forceps to speed up the birth. If that’s unsuccessful, a caesarean delivery might be called for. This is a surgery to deliver the baby. Nuchal cord This is when the umbilical cord wraps around the baby’s neck. Although a nuchal cord doesn’t mean danger for the baby, it could become a problem if the mother can’t push the baby out and a vacuum extractor or forceps are unsuccessful. A caesarean delivery might be the best treatment for this situation. Breech Human babies should be delivered with their head down. A breech pregnancy is when the baby is positioned feet down, bottom down, or sideways. Sometimes a doctor can reposition the baby manually. Sometimes the solution is a caesarean delivery.
Lacerations • Vaginal lacerations usually manifest as profuse bleeding after delivery of the baby. • A large tear in the vaginal wall may not be discovered until the health care provider inspects the vagina after the placenta is delivered. Rupture of the uterus • Rupture of the uterus may occur spontaneously; it may be caused by trauma, or it may occur when a cesarean-section scar gives way. • The classical signs of spontaneous rupture are gradually increasing, constant, severe pain in the lower part of the abdomen, restlessness, a rising temperature, an increasing pulse rate, and a tense, tender uterus that does not relax between strong contractions. • Immediate abdominal surgery follows the diagnosis of uterine rupture. • Bleeding from the torn uterine walls must be stopped as promptly as possible. (Hysterectomy) • Antibiotics are given, because infection is, or may be, present.

• Uterine prolapse, or a sliding of the uterus from its normal position in the pelvic cavity, may result from injuries to the pelvic supporting ligaments and muscles that occur during labour. • Usually the diagnosis is made months or even years later, when the patient complains of something protruding from the vagina, involuntary loss of urine while coughing or laughing, a sensation of heaviness or discomfort in the pelvic cavity, and difficulty in emptying the lower bowel. • Uterine prolapse may be so severe that the uterus lies completely outside the vagina, and the vagina is turned inside out. Treatment depends on the severity of the symptoms.
• Inversion of the uterus • Another complication that may occur during labour is inversion of the uterus. The uterus turns inside out and upside down so that its inner surface lies outside and against the wall of the vagina. Inversion causes sudden hypotension and shock, and there may be severe bleeding. The diagnosis is made by noting the uterus, covered by a dark red, bleeding surface, filling or protruding outside the vagina. The placenta may be attached to the uterus.
• Embolisms • An embolism is a blockage of a blood vessel as by a blood clot or bubble of air. • Amniotic fluid embolism causes sudden, severe respiratory distress, signs of shock, cyanosis (blueing of the skin), heart collapse, and circulatory failure. If the diagnosis is made promptly, oxygen, blood transfusion and the injection of fibrinogen, a clotting factor, into a vein may be lifesaving. • Air embolism causes the patient to become suddenly short of breath and cyanotic. She may have heart pain and show signs of shock. The heart beats irregularly. • Death follows quickly unless the diagnosis is made at once. Treatment consists of drawing the air from the heart with a needle and syringe.
• Placenta praevia is the implantation of the placenta low in the uterus so that the placenta is close to or partially or completely covering the opening into the cervix. • It is suspected if there is painless bleeding during the last three months of pregnancy. • Untreated, the condition may result in early labour, delivery of a premature or stillborn child, and danger of death to the mother from bleeding. • Treatment includes control of bleeding and replacement of lost blood by transfusion. • Delivery of the infant by cesarean section may be necessary if the mother or the child will be endangered by vaginal delivery. • In cases of suspected placenta praevia, the placenta can be located with considerable accuracy by a careful abdominal examination and ultrasonography. • In some cases, magnetic resonance imaging (MRI) may be used to confirm diagnosis.
• Placenta accreta • Abnormal adherence of the placenta to the uterus, a condition called placenta accreta, is suspected when the placenta cannot be expelled. • If placenta accreta arises on the site of a scar from a previous cesarean section, the uterus may rupture during labour. • Otherwise, depending on the firmness with which the placenta is anchored, it may be removed surgically after the baby is delivered. • If such a removal is unsuccessful, immediate removal of the uterus (hysterectomy) is usually indicated.
• Abruptio placentae is the premature separation of the placenta from its normal implantation site in the uterus. • The separation of the placenta causes bleeding, and replacement of the lost blood by transfusion is necessary. • In instances of complete abruptio placentae, the infant dies unless delivered immediately. • In partial separation the mother is given oxygen, and the infant is delivered by cesarean section as soon as it is safe to do so. • The cause of abruptio placentae is not known, but it is more common in women who have hypertension.
• Umbilical cord complications • A complication of the umbilical cord is suspected when there is marked irregularity in the fetal heart rate and particularly when the irregularity is accentuated by uterine contractions. • A prolapsed cord—that is, a cord lying below the head—can be felt through the membranes on vaginal examination. • The fetus is delivered by cesarean section.
• Puerperium • Within six to eight weeks after childbirth, most of the structures of the maternal organism that underwent change during pregnancy return more or less to their prepregnancy state. • The enlarged uterus, which at the end of gestation weighs about 1, 000 grams (35 ounces), shrinks to a weight of about 60 grams (2 ounces). • Along with this process of uterine involution, the lining membrane of the uterus is almost completely shed and replaced by a new lining, which is then (six to eight weeks after delivery) ready for the reception of another fertilized ovum (egg). • The greatly dilated neck of the uterus and lower birth passage likewise undergo marked and rapid involution, but they seldom return exactly to their prepregnancy condition.
 Phase 2 parturition
Phase 2 parturition Parturition
Parturition Figure 16-1 is a sagittal view of the male reproductive
Figure 16-1 is a sagittal view of the male reproductive Parturition
Parturition Uterotrophins
Uterotrophins Matthew duncan placental separation
Matthew duncan placental separation Equine
Equine Expulsion de los judios de españa
Expulsion de los judios de españa Expulsion from paradise masaccio
Expulsion from paradise masaccio Preschool to prison pipeline
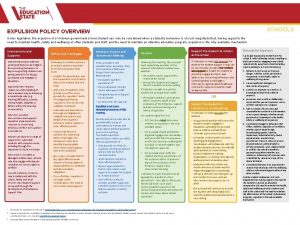
Preschool to prison pipeline Expulsion
Expulsion No second thought expulsion order
No second thought expulsion order Expulsion of the acadians timeline
Expulsion of the acadians timeline Lausd suspension matrix
Lausd suspension matrix Expulsión de los jesuitas reformas borbónicas
Expulsión de los jesuitas reformas borbónicas Expulsion
Expulsion Expulsion
Expulsion Direct and indirect lightning
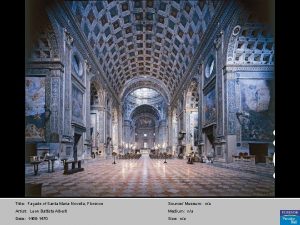
Direct and indirect lightning Expulsion from paradise masaccio
Expulsion from paradise masaccio Pricing tripod in service marketing
Pricing tripod in service marketing Physical fitness components and tests grade 9
Physical fitness components and tests grade 9 Bảng số nguyên tố
Bảng số nguyên tố đặc điểm cơ thể của người tối cổ
đặc điểm cơ thể của người tối cổ