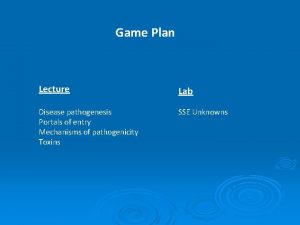
Overview of Pathogenesis the manner in which disease
- Slides: 13
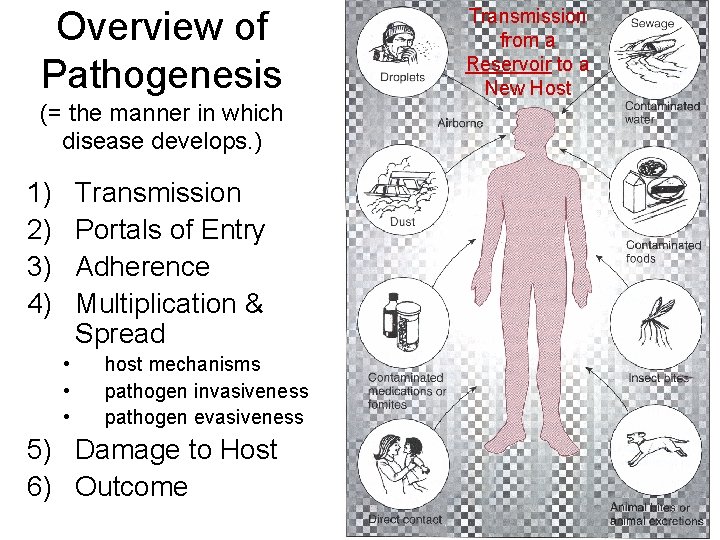
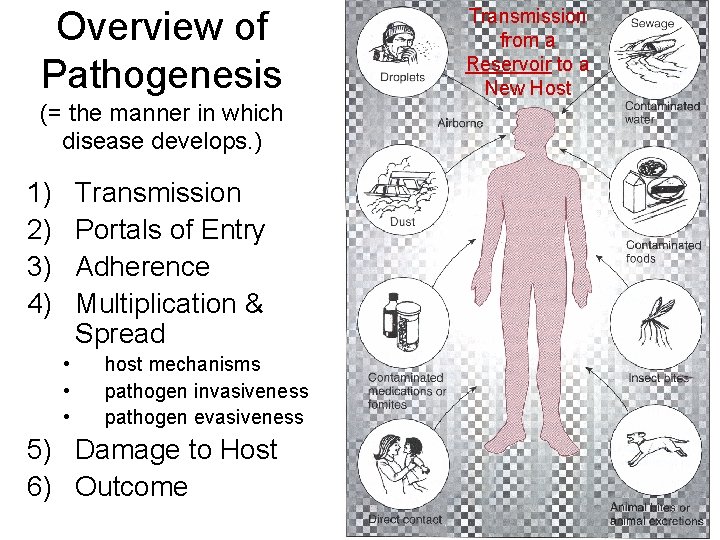
Overview of Pathogenesis (= the manner in which disease develops. ) 1) 2) 3) 4) Transmission Portals of Entry Adherence Multiplication & Spread • • • host mechanisms pathogen invasiveness pathogen evasiveness 5) Damage to Host 6) Outcome Transmission from a Reservoir to a New Host
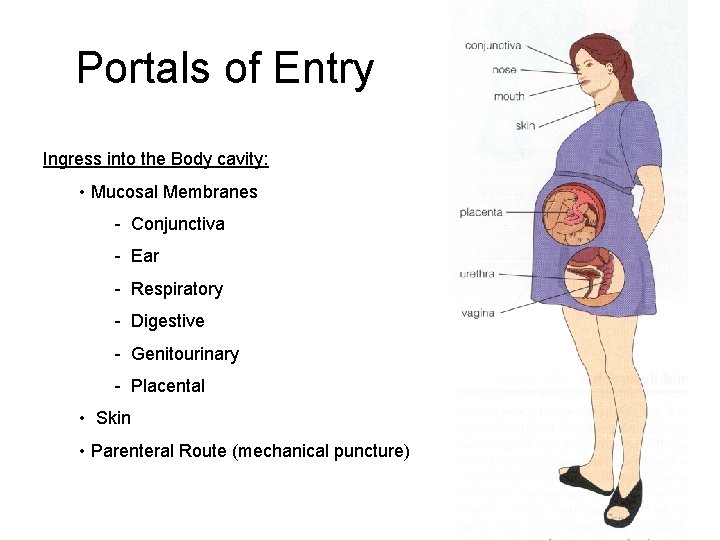
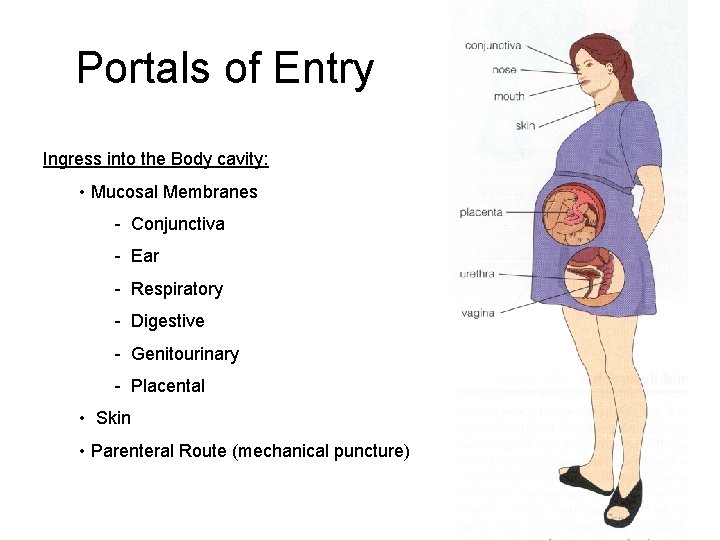
Portals of Entry Ingress into the Body cavity: • Mucosal Membranes - Conjunctiva - Ear - Respiratory - Digestive - Genitourinary - Placental • Skin • Parenteral Route (mechanical puncture)
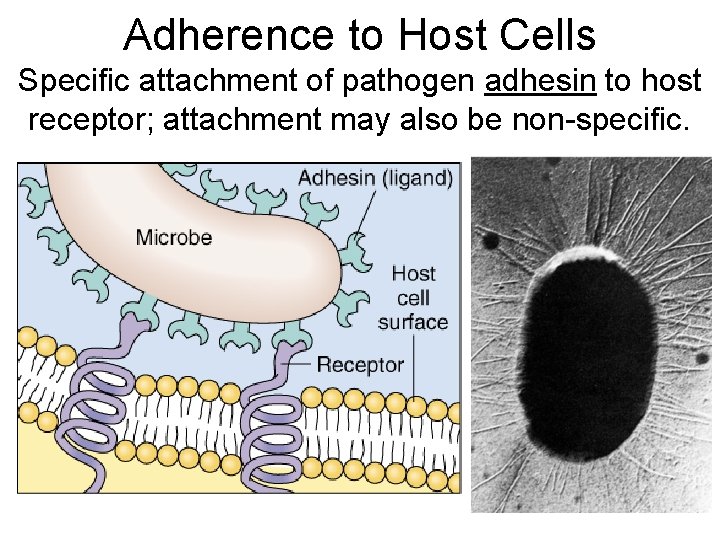
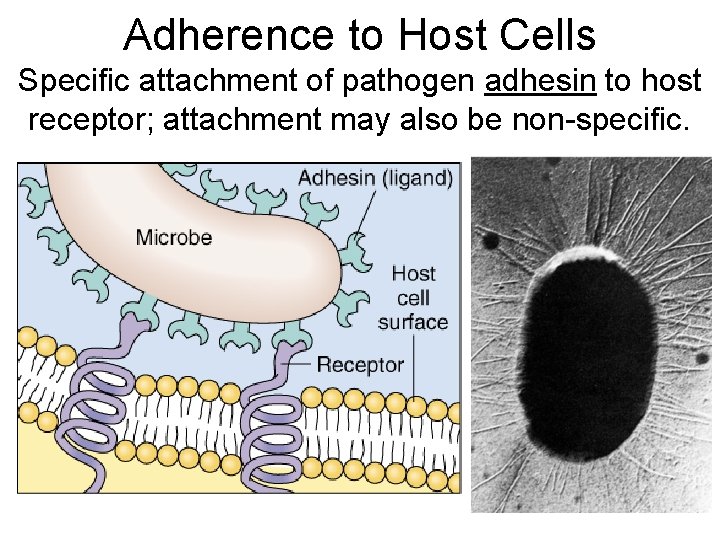
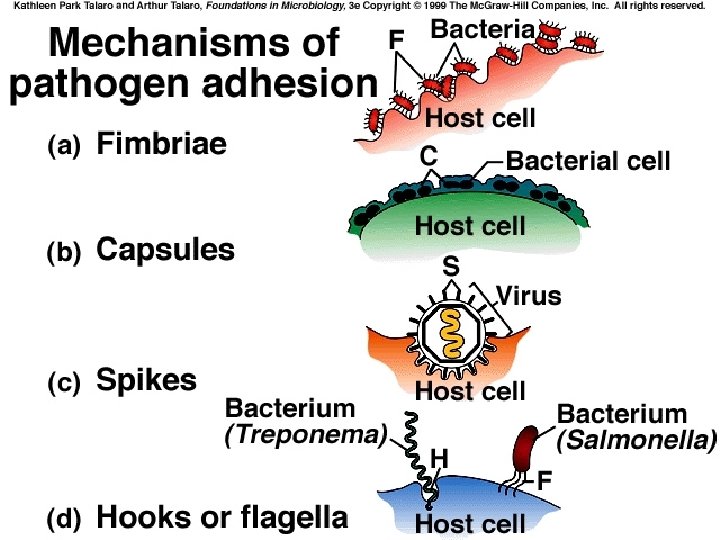
Adherence to Host Cells Specific attachment of pathogen adhesin to host receptor; attachment may also be non-specific.
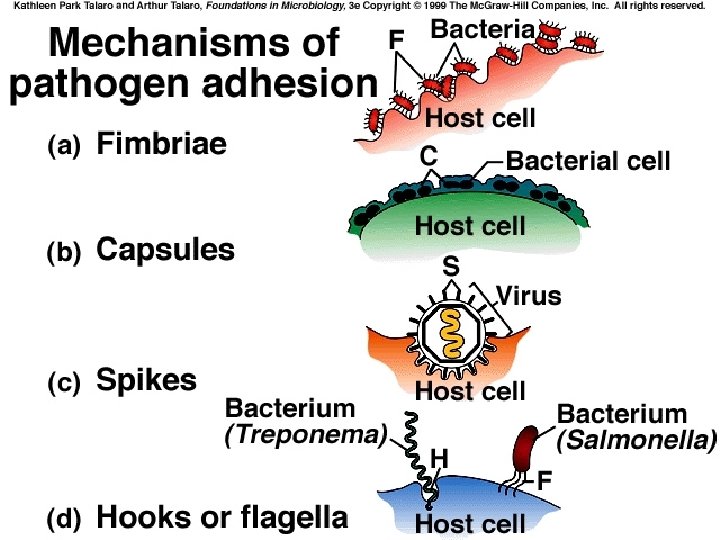
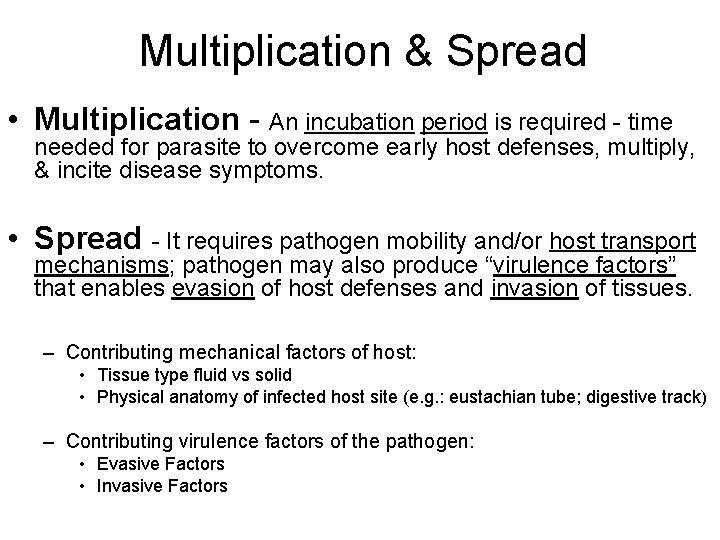
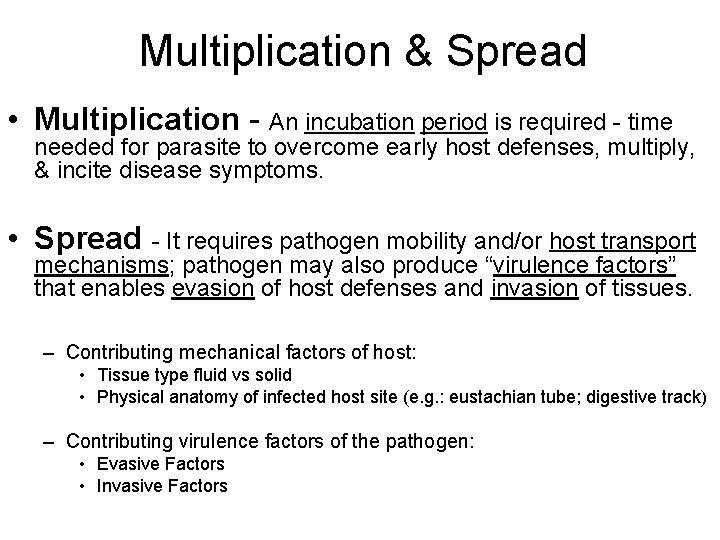
Multiplication & Spread • Multiplication - An incubation period is required - time needed for parasite to overcome early host defenses, multiply, & incite disease symptoms. • Spread - It requires pathogen mobility and/or host transport mechanisms; pathogen may also produce “virulence factors” that enables evasion of host defenses and invasion of tissues. – Contributing mechanical factors of host: • Tissue type fluid vs solid • Physical anatomy of infected host site (e. g. : eustachian tube; digestive track) – Contributing virulence factors of the pathogen: • Evasive Factors • Invasive Factors
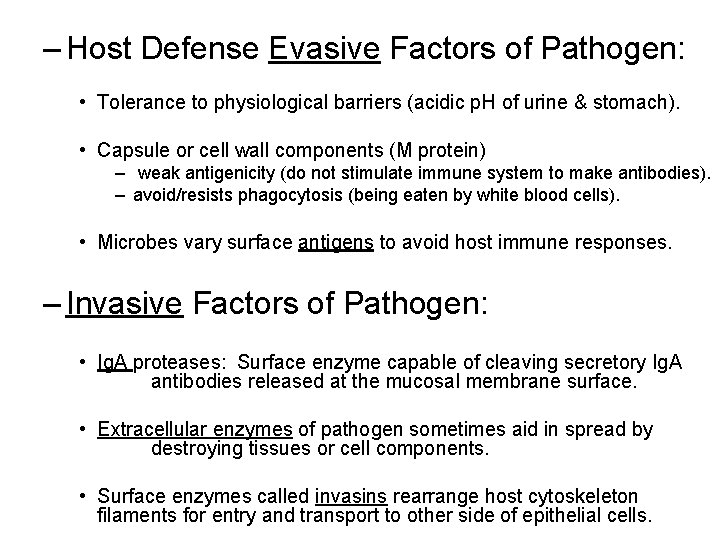
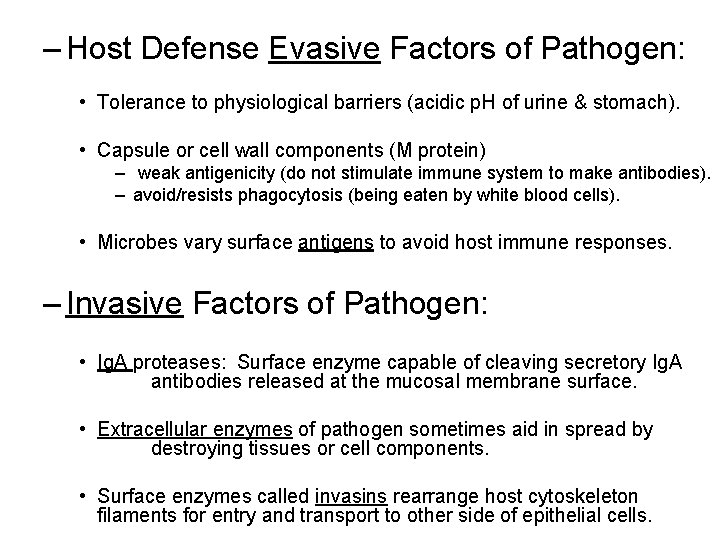
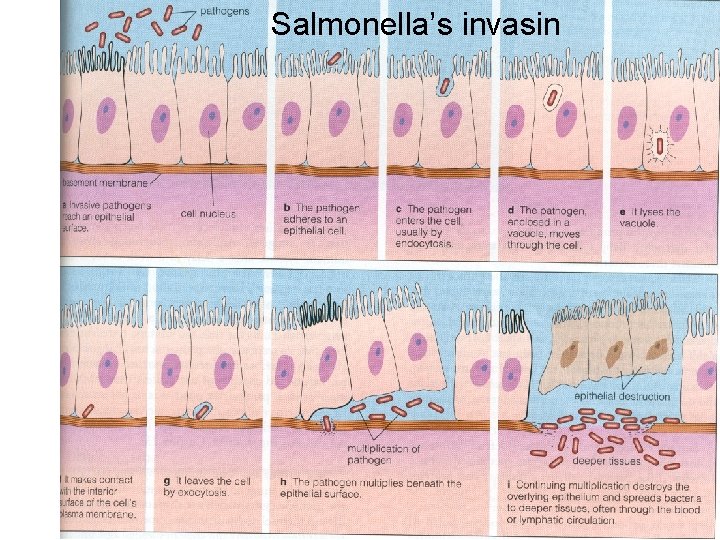
– Host Defense Evasive Factors of Pathogen: • Tolerance to physiological barriers (acidic p. H of urine & stomach). • Capsule or cell wall components (M protein) – weak antigenicity (do not stimulate immune system to make antibodies). – avoid/resists phagocytosis (being eaten by white blood cells). • Microbes vary surface antigens to avoid host immune responses. – Invasive Factors of Pathogen: • Ig. A proteases: Surface enzyme capable of cleaving secretory Ig. A antibodies released at the mucosal membrane surface. • Extracellular enzymes of pathogen sometimes aid in spread by destroying tissues or cell components. • Surface enzymes called invasins rearrange host cytoskeleton filaments for entry and transport to other side of epithelial cells.
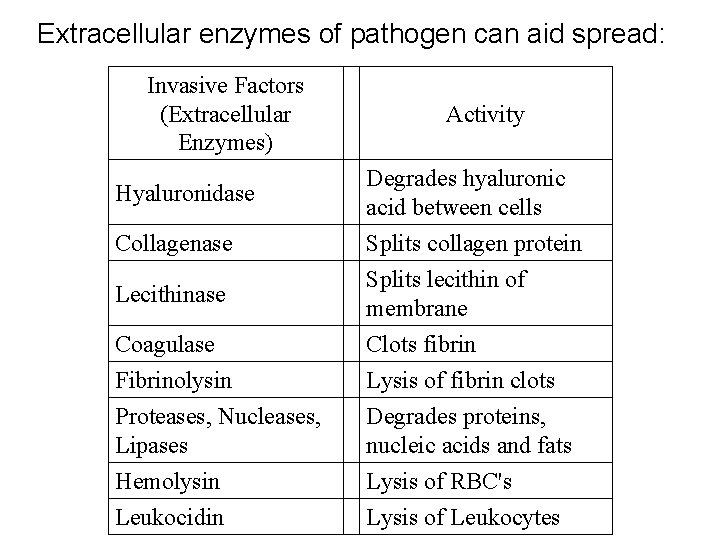
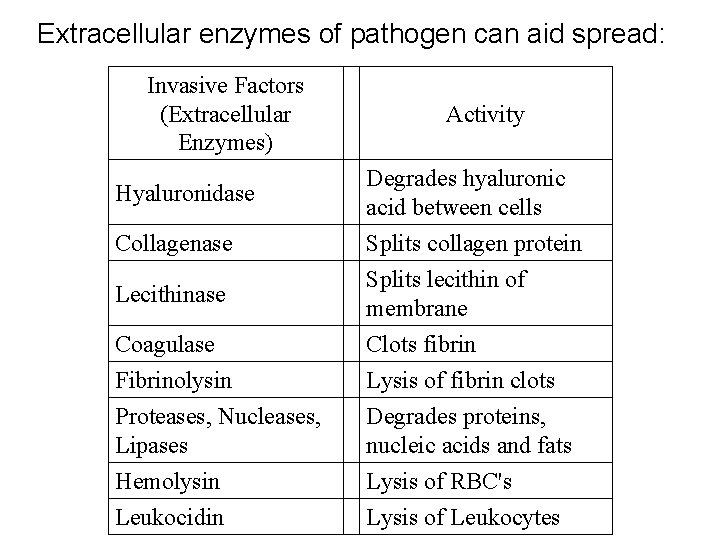
Extracellular enzymes of pathogen can aid spread: Invasive Factors (Extracellular Enzymes) Hyaluronidase Collagenase Lecithinase Coagulase Fibrinolysin Proteases, Nucleases, Lipases Hemolysin Leukocidin Activity Degrades hyaluronic acid between cells Splits collagen protein Splits lecithin of membrane Clots fibrin Lysis of fibrin clots Degrades proteins, nucleic acids and fats Lysis of RBC's Lysis of Leukocytes
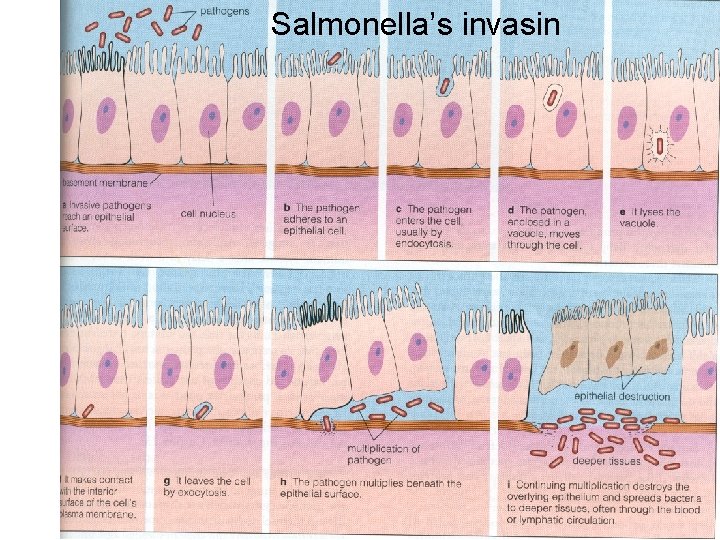
Salmonella’s invasin
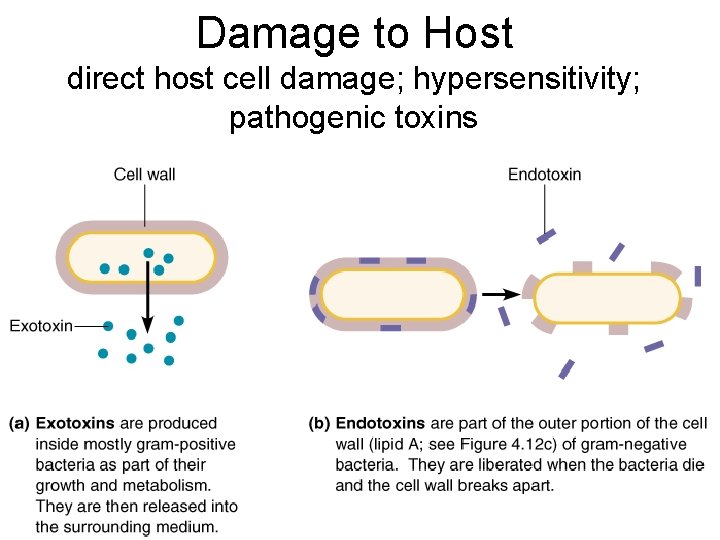
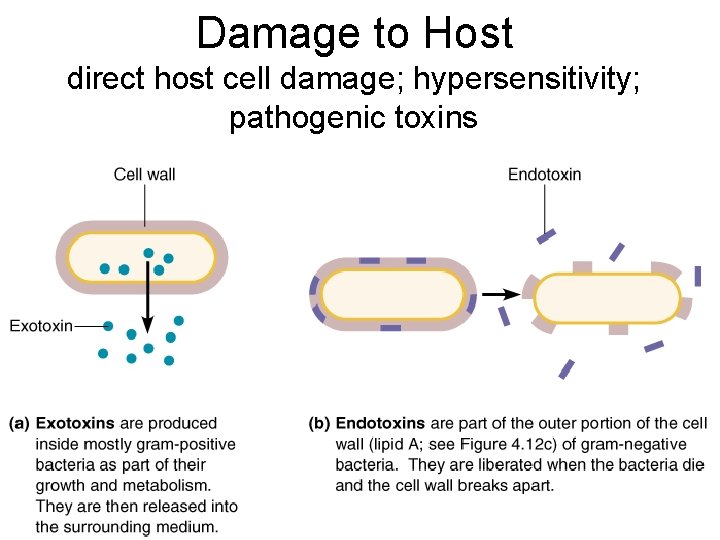
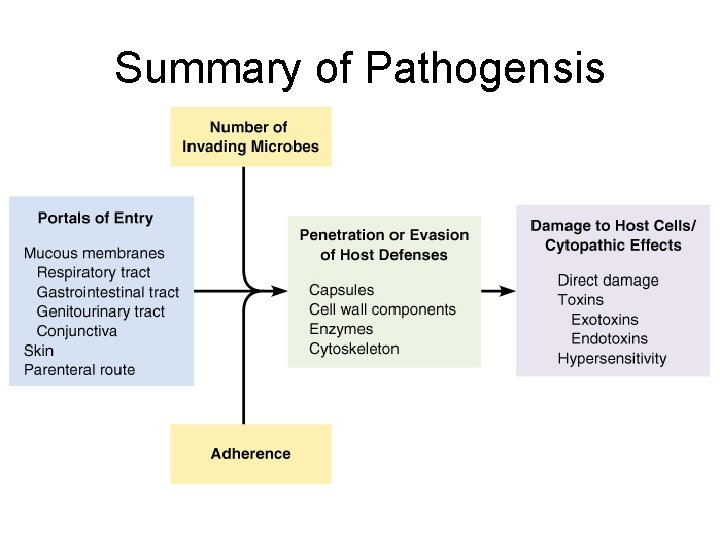
Damage to Host direct host cell damage; hypersensitivity; pathogenic toxins
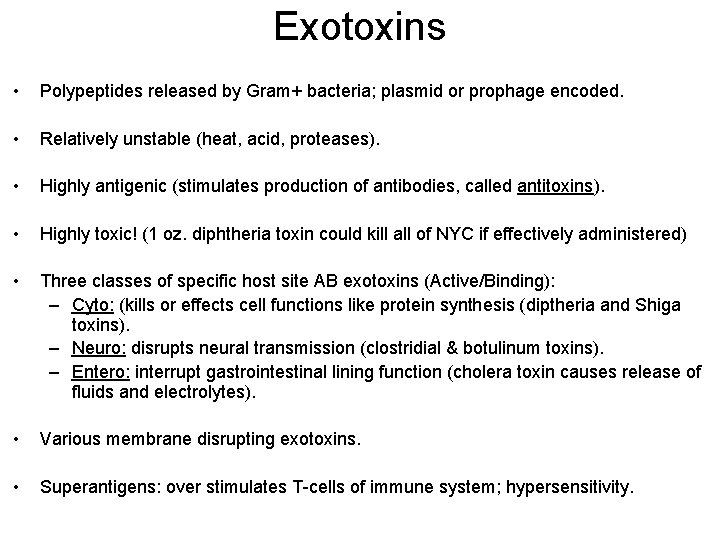
Exotoxins • Polypeptides released by Gram+ bacteria; plasmid or prophage encoded. • Relatively unstable (heat, acid, proteases). • Highly antigenic (stimulates production of antibodies, called antitoxins). • Highly toxic! (1 oz. diphtheria toxin could kill all of NYC if effectively administered) • Three classes of specific host site AB exotoxins (Active/Binding): – Cyto: (kills or effects cell functions like protein synthesis (diptheria and Shiga toxins). – Neuro: disrupts neural transmission (clostridial & botulinum toxins). – Entero: interrupt gastrointestinal lining function (cholera toxin causes release of fluids and electrolytes). • Various membrane disrupting exotoxins. • Superantigens: over stimulates T-cells of immune system; hypersensitivity.
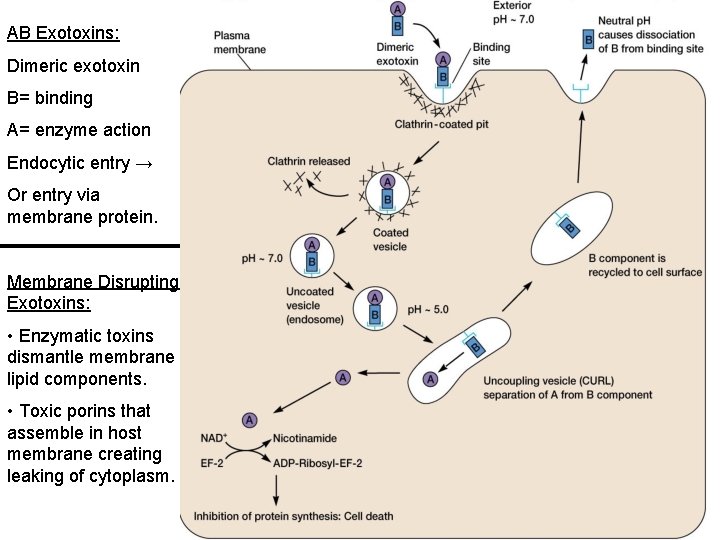
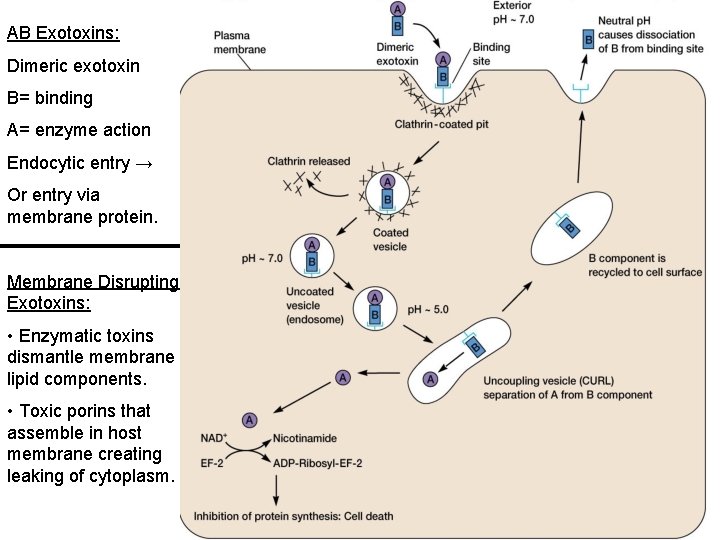
AB Exotoxins: Dimeric exotoxin B= binding A= enzyme action Endocytic entry → Or entry via membrane protein. Membrane Disrupting Exotoxins: • Enzymatic toxins dismantle membrane lipid components. • Toxic porins that assemble in host membrane creating leaking of cytoplasm.
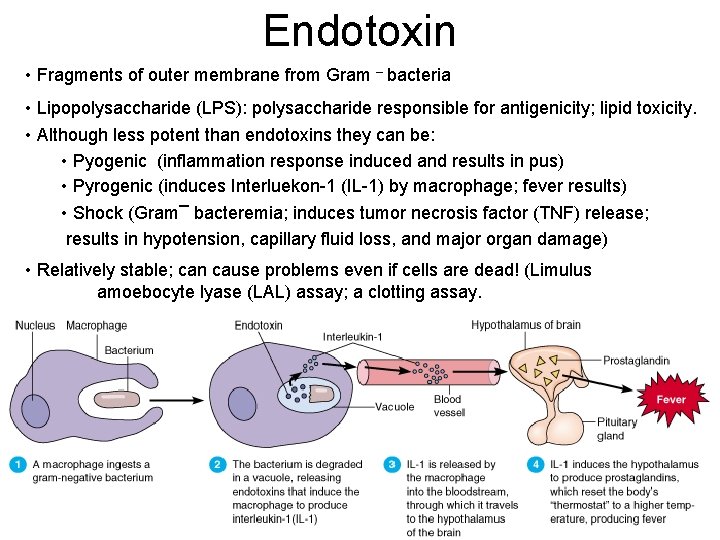
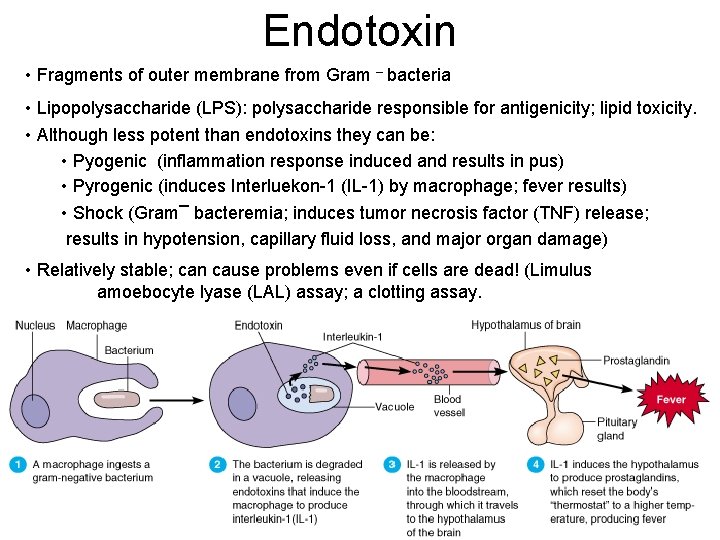
Endotoxin • Fragments of outer membrane from Gram – bacteria • Lipopolysaccharide (LPS): polysaccharide responsible for antigenicity; lipid toxicity. • Although less potent than endotoxins they can be: • Pyogenic (inflammation response induced and results in pus) • Pyrogenic (induces Interluekon-1 (IL-1) by macrophage; fever results) • Shock (Gram– bacteremia; induces tumor necrosis factor (TNF) release; results in hypotension, capillary fluid loss, and major organ damage) • Relatively stable; can cause problems even if cells are dead! (Limulus amoebocyte lyase (LAL) assay; a clotting assay.
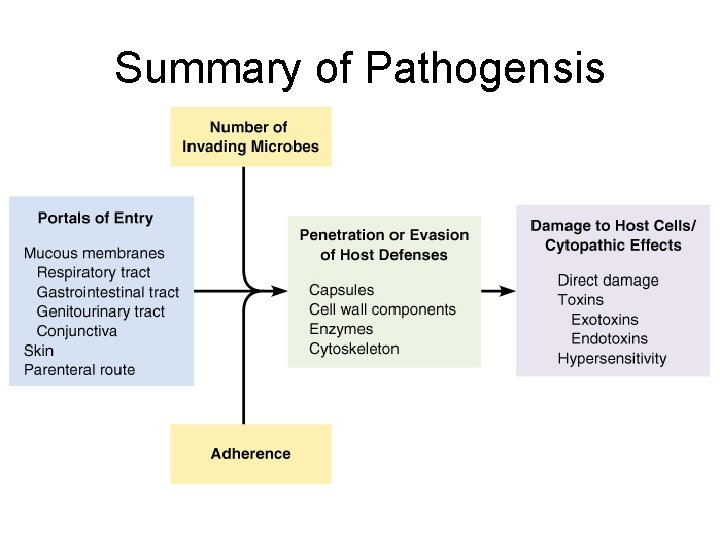
Summary of Pathogensis