ORAL SURGERY IN PATIENTS ON ANTICOAGULANT THERAPY Presented




- Slides: 32
ORAL SURGERY IN PATIENTS ON ANTICOAGULANT THERAPY Presented by. Dr. Varun Mittal, PG Dept of Maxillofacial Surgery SRM DENTAL COLLEGE, CHENNAI, INDIA

Which all patients? Mostly cardiac or vascular disorders: � Atrial fibrillation � Ischemic cardiac disease � Cardiac valvular disease � Prosthetic cardiac valves � Post myocardial infarction � Deep venous thrombosis � Pulmonary embolism � Cerebrovascular accident
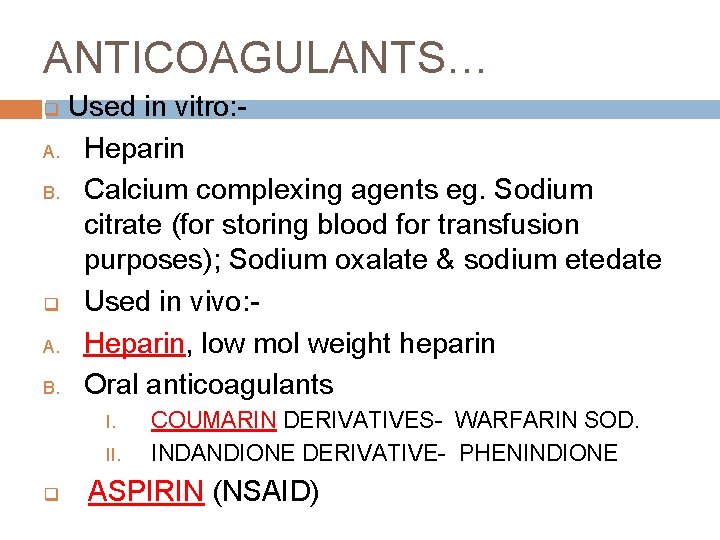
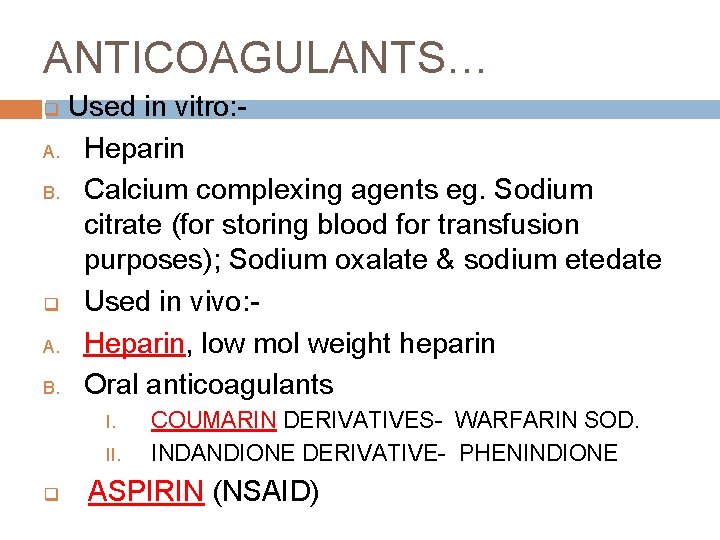
ANTICOAGULANTS… Used in vitro: A. Heparin B. Calcium complexing agents eg. Sodium citrate (for storing blood for transfusion purposes); Sodium oxalate & sodium etedate q Used in vivo: A. Heparin, low mol weight heparin B. Oral anticoagulants q I. II. q COUMARIN DERIVATIVES- WARFARIN SOD. INDANDIONE DERIVATIVE- PHENINDIONE ASPIRIN (NSAID)
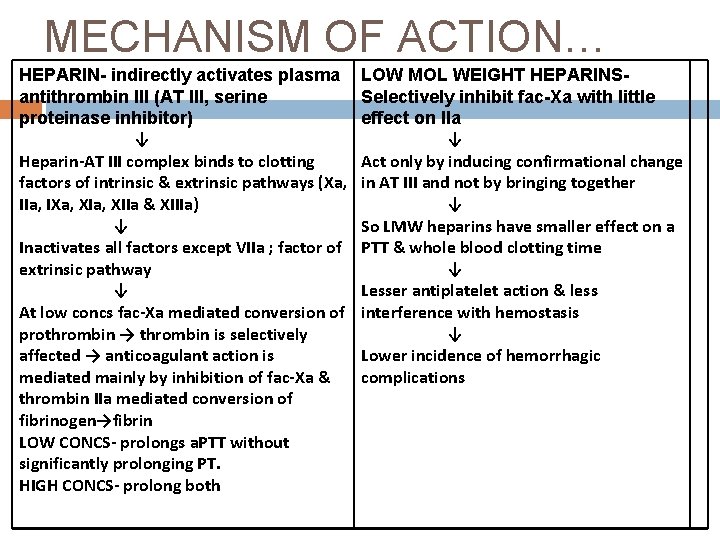
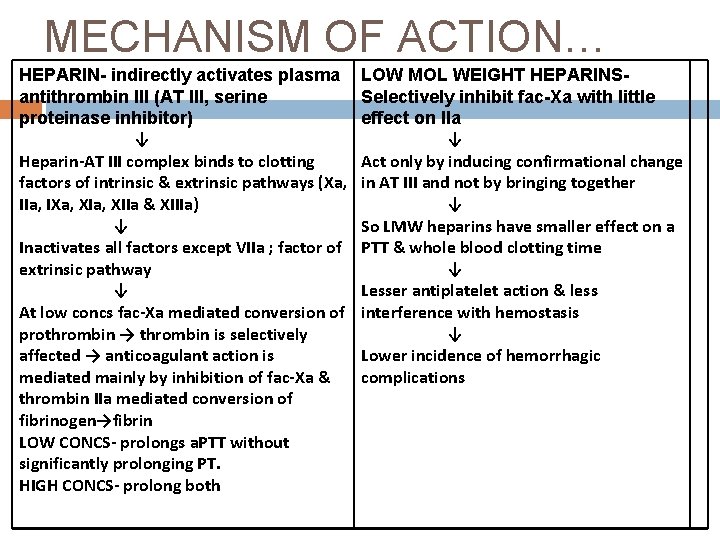
MECHANISM OF ACTION… HEPARIN- indirectly activates plasma antithrombin III (AT III, serine proteinase inhibitor) ↓ Heparin-AT III complex binds to clotting factors of intrinsic & extrinsic pathways (Xa, IIa, IXa, XIIa & XIIIa) ↓ Inactivates all factors except VIIa ; factor of extrinsic pathway ↓ At low concs fac-Xa mediated conversion of prothrombin → thrombin is selectively affected → anticoagulant action is mediated mainly by inhibition of fac-Xa & thrombin IIa mediated conversion of fibrinogen→fibrin LOW CONCS- prolongs a. PTT without significantly prolonging PT. HIGH CONCS- prolong both LOW MOL WEIGHT HEPARINSSelectively inhibit fac-Xa with little effect on IIa ↓ Act only by inducing confirmational change in AT III and not by bringing together ↓ So LMW heparins have smaller effect on a PTT & whole blood clotting time ↓ Lesser antiplatelet action & less interference with hemostasis ↓ Lower incidence of hemorrhagic complications
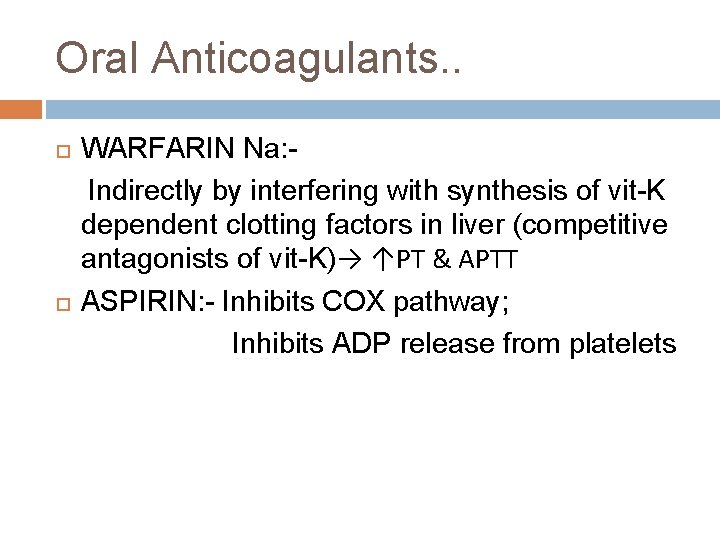
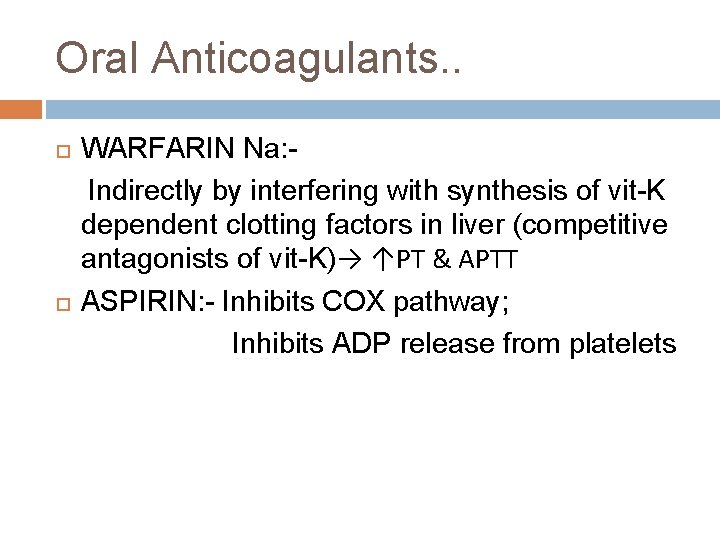
Oral Anticoagulants. . WARFARIN Na: Indirectly by interfering with synthesis of vit-K dependent clotting factors in liver (competitive antagonists of vit-K)→ ↑PT & APTT ASPIRIN: - Inhibits COX pathway; Inhibits ADP release from platelets
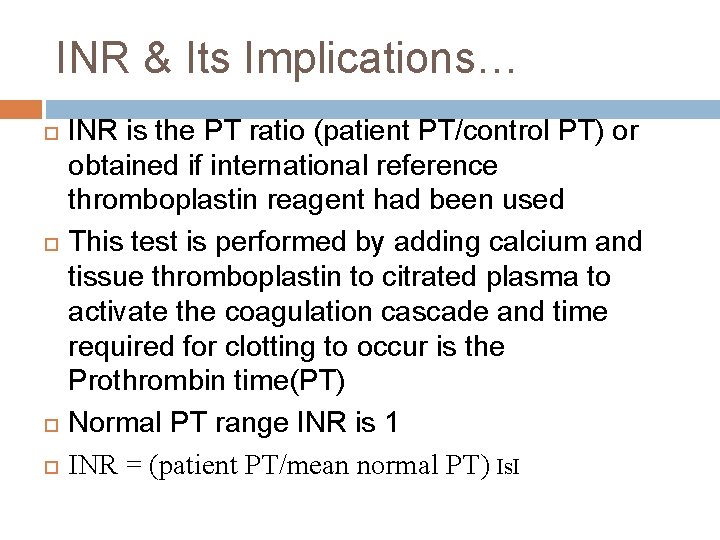
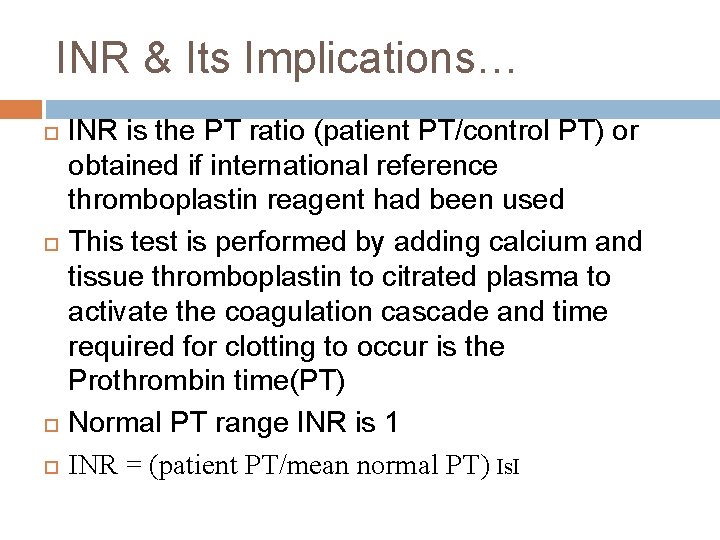
INR & Its Implications… INR is the PT ratio (patient PT/control PT) or obtained if international reference thromboplastin reagent had been used This test is performed by adding calcium and tissue thromboplastin to citrated plasma to activate the coagulation cascade and time required for clotting to occur is the Prothrombin time(PT) Normal PT range INR is 1 INR = (patient PT/mean normal PT) Is. I
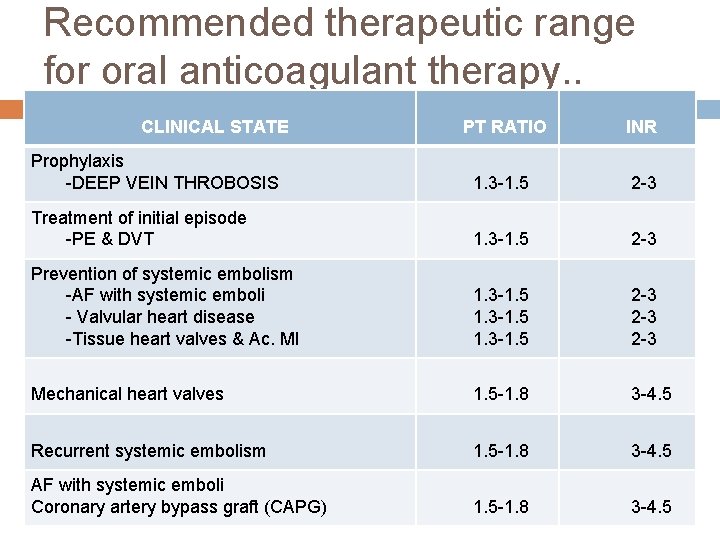
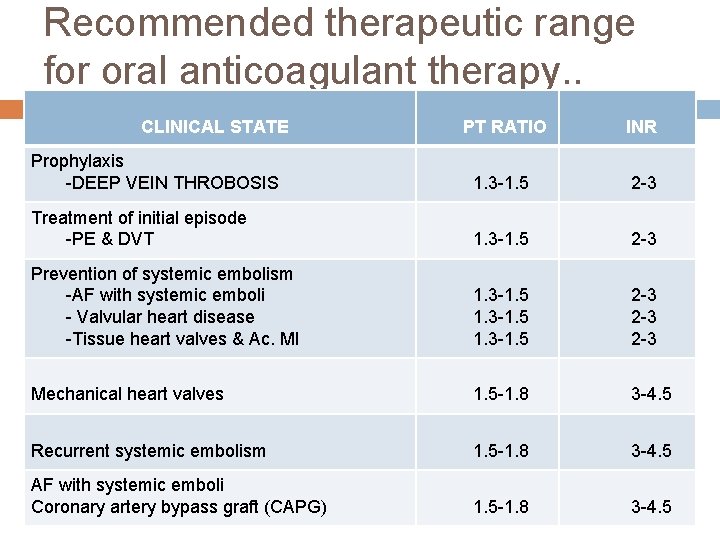
Recommended therapeutic range for oral anticoagulant therapy. . CLINICAL STATE PT RATIO INR Prophylaxis -DEEP VEIN THROBOSIS 1. 3 -1. 5 2 -3 Treatment of initial episode -PE & DVT 1. 3 -1. 5 2 -3 Prevention of systemic embolism -AF with systemic emboli - Valvular heart disease -Tissue heart valves & Ac. MI 1. 3 -1. 5 2 -3 2 -3 Mechanical heart valves 1. 5 -1. 8 3 -4. 5 Recurrent systemic embolism 1. 5 -1. 8 3 -4. 5 AF with systemic emboli Coronary artery bypass graft (CAPG) 1. 5 -1. 8 3 -4. 5
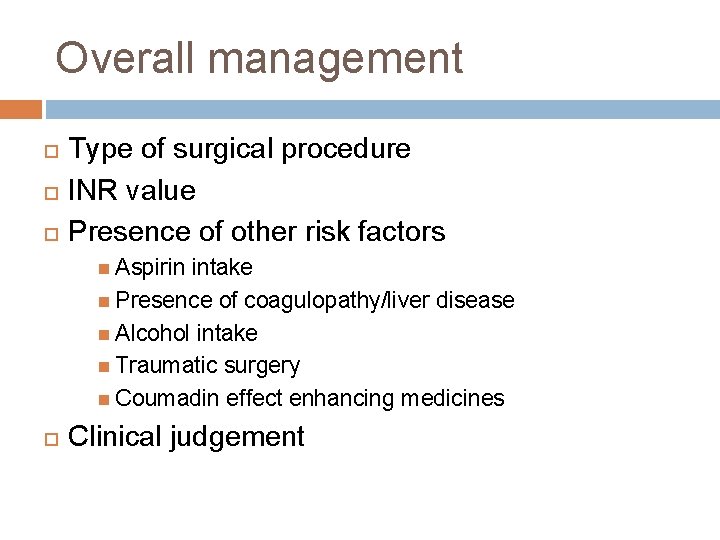
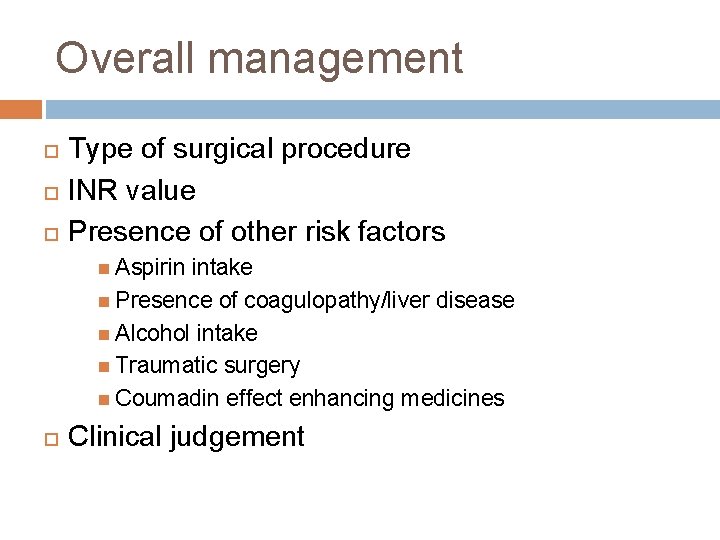
Overall management Type of surgical procedure INR value Presence of other risk factors Aspirin intake Presence of coagulopathy/liver disease Alcohol intake Traumatic surgery Coumadin effect enhancing medicines Clinical judgement
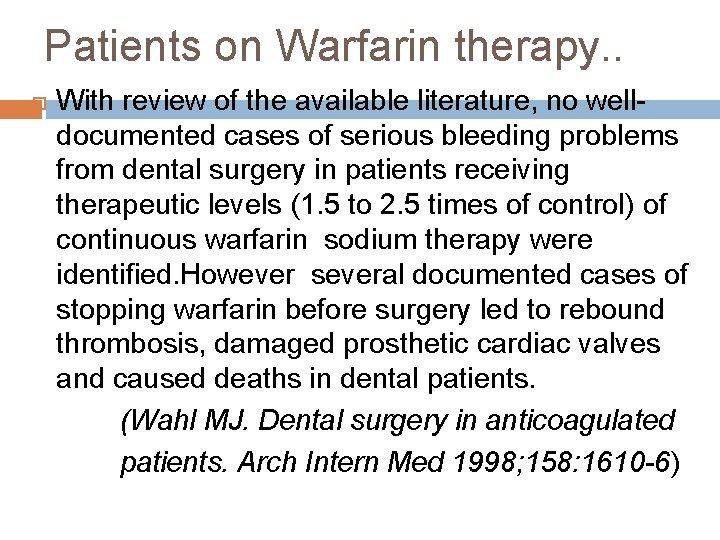
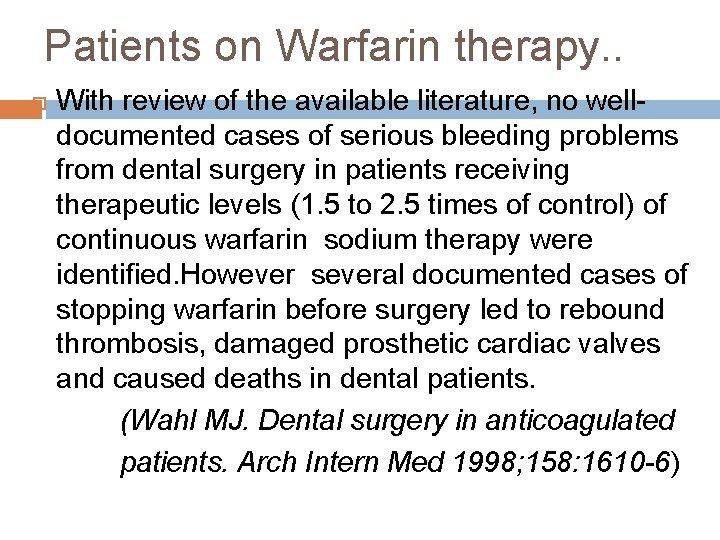
Patients on Warfarin therapy. . With review of the available literature, no welldocumented cases of serious bleeding problems from dental surgery in patients receiving therapeutic levels (1. 5 to 2. 5 times of control) of continuous warfarin sodium therapy were identified. However several documented cases of stopping warfarin before surgery led to rebound thrombosis, damaged prosthetic cardiac valves and caused deaths in dental patients. (Wahl MJ. Dental surgery in anticoagulated patients. Arch Intern Med 1998; 158: 1610 -6)
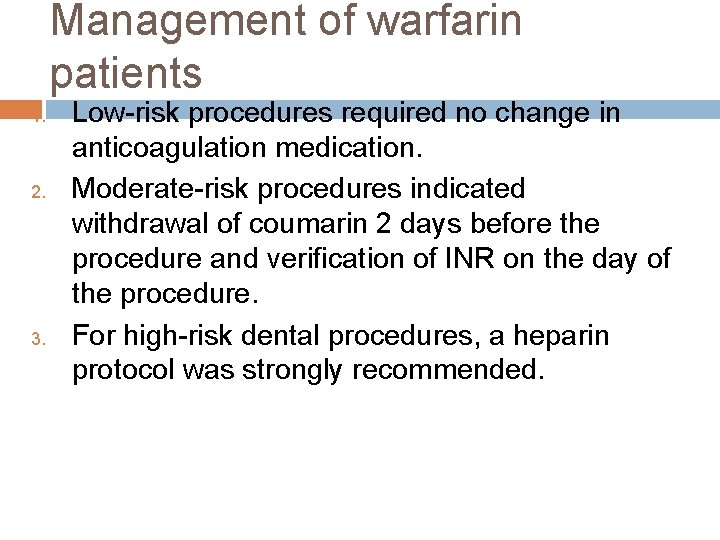
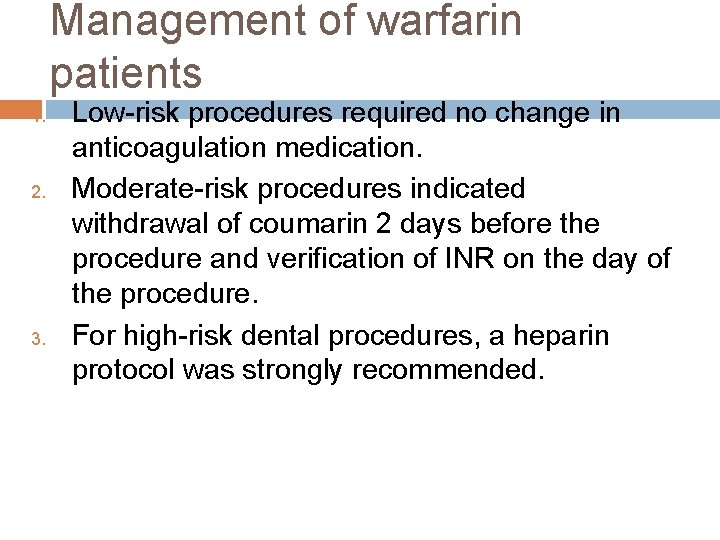
Management of warfarin patients 1. 2. 3. Low-risk procedures required no change in anticoagulation medication. Moderate-risk procedures indicated withdrawal of coumarin 2 days before the procedure and verification of INR on the day of the procedure. For high-risk dental procedures, a heparin protocol was strongly recommended.
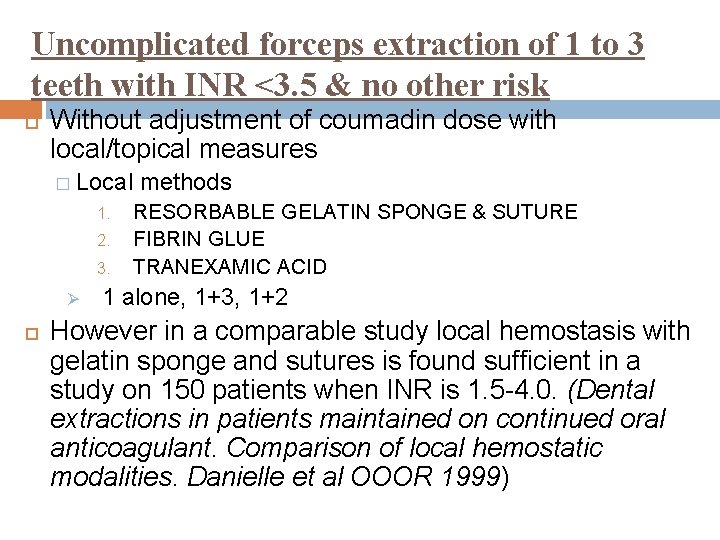
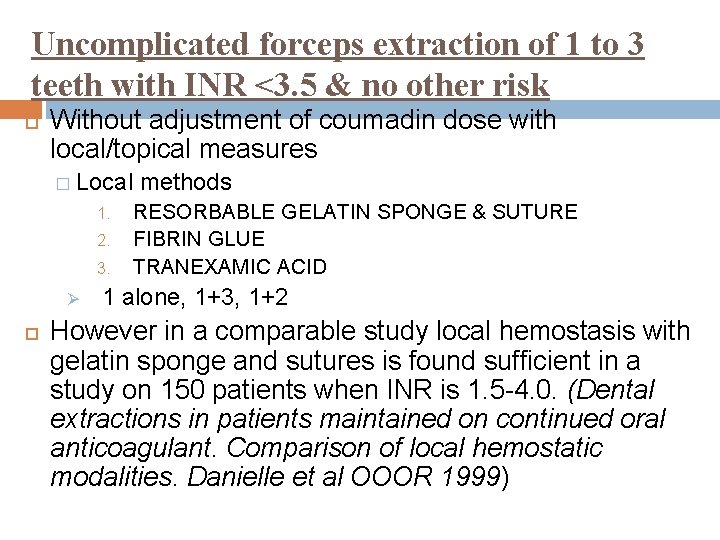
Uncomplicated forceps extraction of 1 to 3 teeth with INR <3. 5 & no other risk Without adjustment of coumadin dose with local/topical measures � Local 1. 2. 3. Ø methods RESORBABLE GELATIN SPONGE & SUTURE FIBRIN GLUE TRANEXAMIC ACID 1 alone, 1+3, 1+2 However in a comparable study local hemostasis with gelatin sponge and sutures is found sufficient in a study on 150 patients when INR is 1. 5 -4. 0. (Dental extractions in patients maintained on continued oral anticoagulant. Comparison of local hemostatic modalities. Danielle et al OOOR 1999)
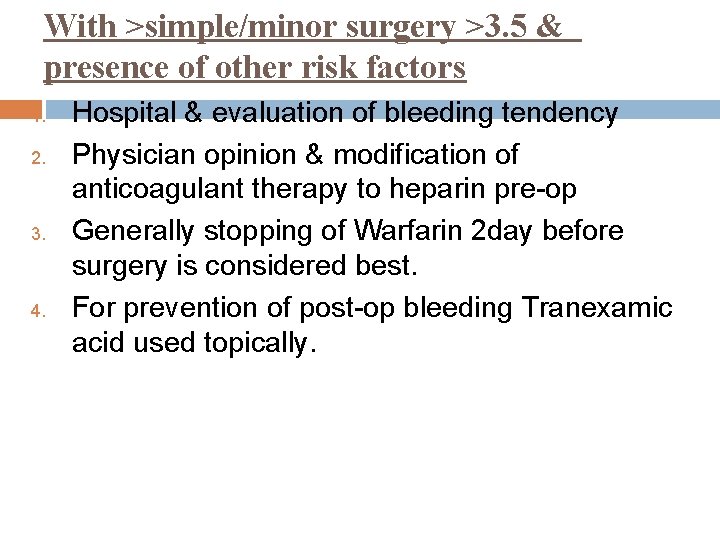
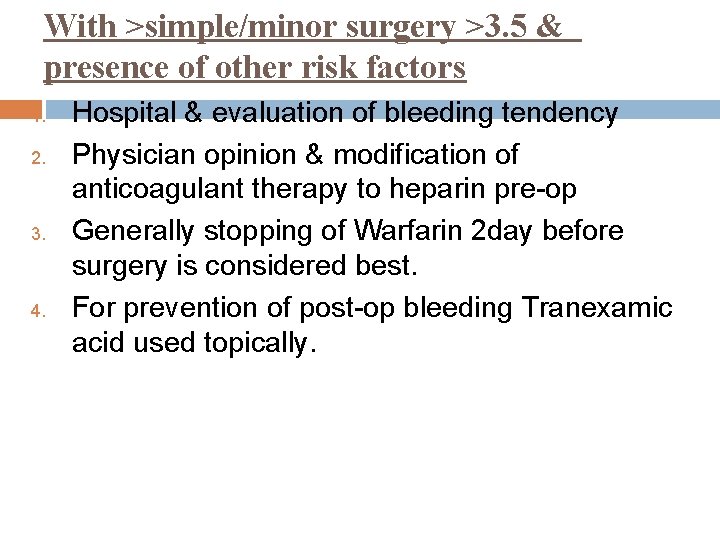
With >simple/minor surgery >3. 5 & presence of other risk factors 1. 2. 3. 4. Hospital & evaluation of bleeding tendency Physician opinion & modification of anticoagulant therapy to heparin pre-op Generally stopping of Warfarin 2 day before surgery is considered best. For prevention of post-op bleeding Tranexamic acid used topically.
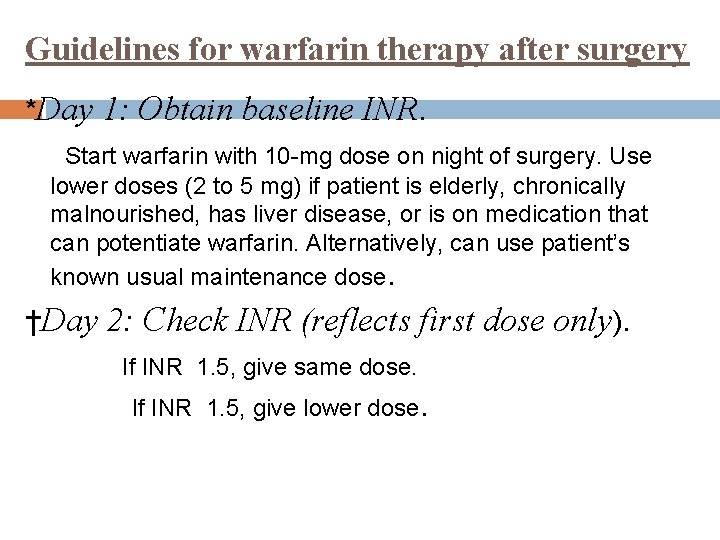
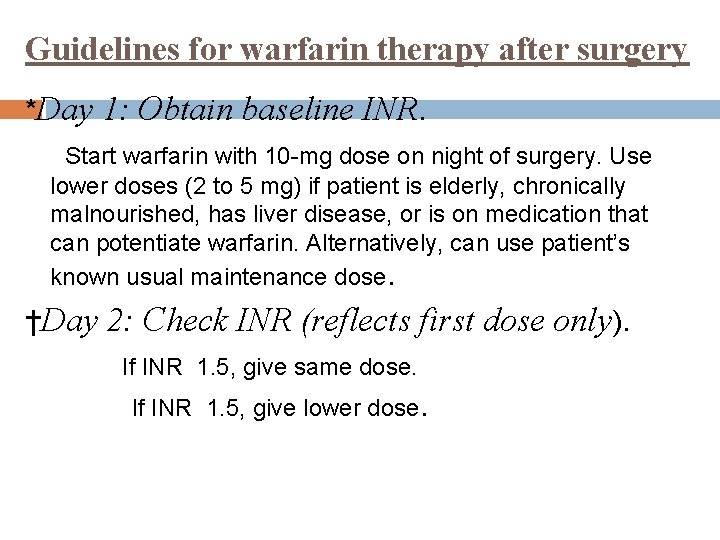
Guidelines for warfarin therapy after surgery *Day 1: Obtain baseline INR. Start warfarin with 10 -mg dose on night of surgery. Use lower doses (2 to 5 mg) if patient is elderly, chronically malnourished, has liver disease, or is on medication that can potentiate warfarin. Alternatively, can use patient’s known usual maintenance dose. †Day 2: Check INR (reflects first dose only). If INR 1. 5, give same dose. If INR 1. 5, give lower dose.
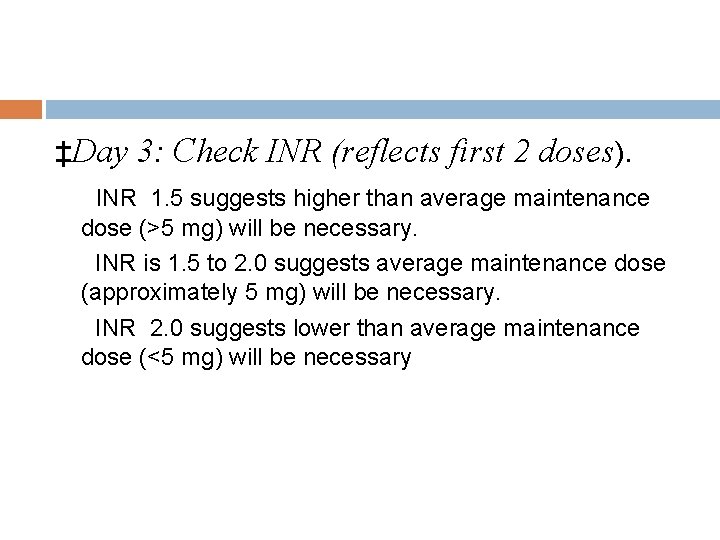
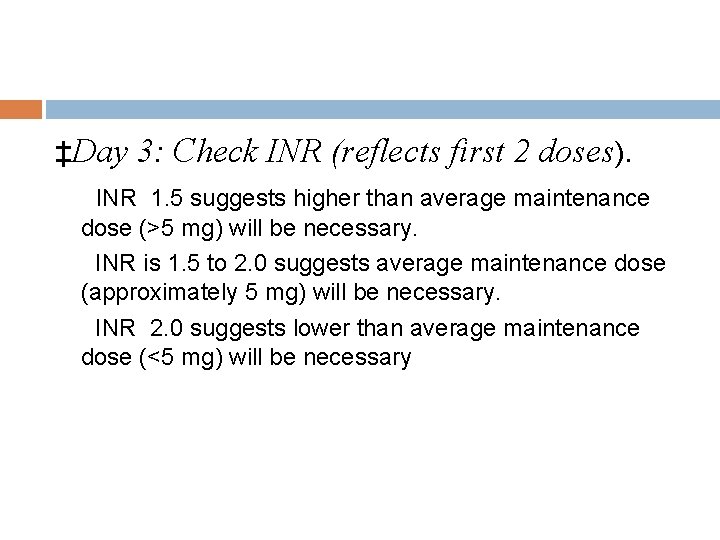
‡Day 3: Check INR (reflects first 2 doses). INR 1. 5 suggests higher than average maintenance dose (>5 mg) will be necessary. INR is 1. 5 to 2. 0 suggests average maintenance dose (approximately 5 mg) will be necessary. INR 2. 0 suggests lower than average maintenance dose (<5 mg) will be necessary
Post-op care… Antifibrinolytics � Tranexamic acid topical mouthwash � EACA(250 mg/ml)25% syrup 5 to 10 ml Oral penicillins V 250 to 500 mg qid for 7 days Paracetamol choice drug for short term use as no affect on platelets OR Codeine is also effective Diet cool liquid and minced solids for several days
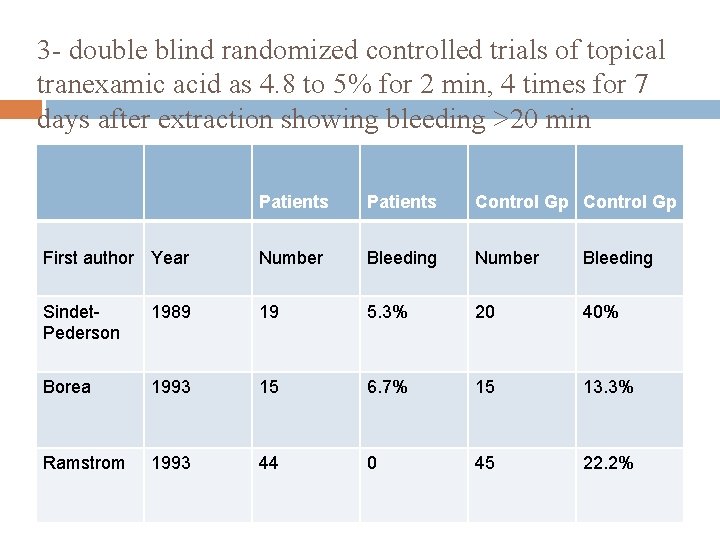
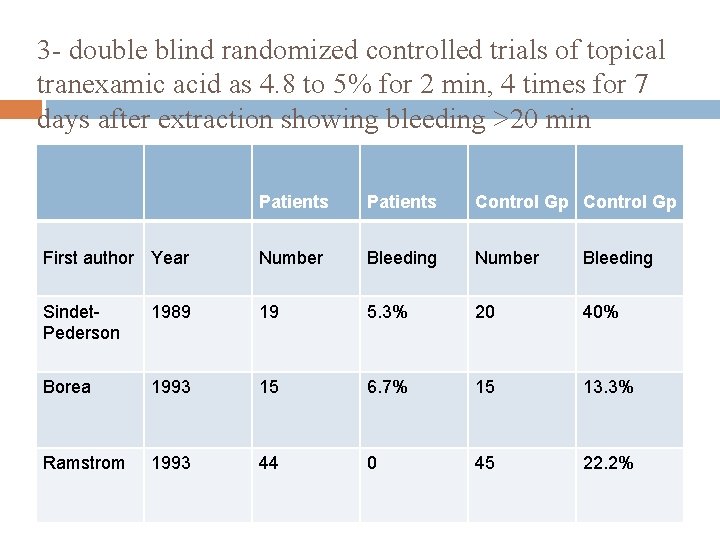
3 - double blind randomized controlled trials of topical tranexamic acid as 4. 8 to 5% for 2 min, 4 times for 7 days after extraction showing bleeding >20 min Patients Control Gp First author Year Number Bleeding Sindet. Pederson 1989 19 5. 3% 20 40% Borea 1993 15 6. 7% 15 13. 3% Ramstrom 1993 44 0 45 22. 2%
Post-op prolonged bleeding Biting on a gauze pad soaked in Tranexamic acid or a moist tea bag for 30 min, firmly Need for infusion should be assessed Desmopressin acetate synthetic analogue of vasopressin initiates release of fac VIIIC, v. W fac & t-PA from storage site of endothelium Given as intranasal spray (1. 5 mg/m. L with each 0. 1 m. L pump spray delivering 100 - to 150 - μg)
Management of patients on heparin anticoagulation therapy Heparin has an immediate effect on blood clotting but acts for only 4 to 6 hours. The effect of heparin is best assessed by the APTT. For uncomplicated forceps extraction of 1 to 3 teeth, there is usually no need to interfere with anticoagulant treatment involving heparin or LMW heparins or antiplatelet drugs. Medical consultation should be sought before more advanced surgery in a patient with heparin treatment

Initiation and modification of heparin therapy 1. One to 2 days before hospitalization, discontinue coumadin. 2. Check baseline APTT, INR, complete blood cell/platelet count. 3. Give bolus of heparin at dose of 80 U/kg intravenously. 4. Start drip infusion of heparin at 18 U/kg/h intravenously. 5. Check APTT 6 hours after initial bolus of heparin. 6. Adjust dose of heparin as per sliding scale: APTT <35 seconds 80 U/kg bolus; ↑ drip by 4 U/kg/h APTT 35 -45 seconds 40 U/kg bolus; ↑ drip by 2 U/kg/h APTT 46 -70 seconds. No change because level is therapeutic
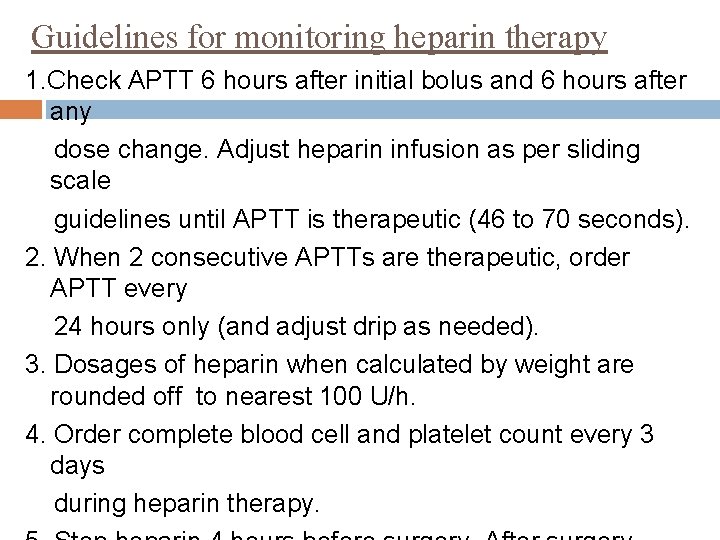
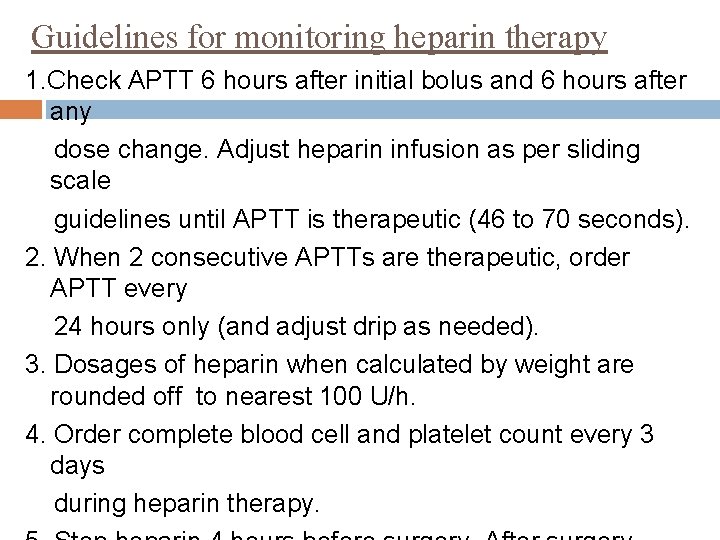
Guidelines for monitoring heparin therapy 1. Check APTT 6 hours after initial bolus and 6 hours after any dose change. Adjust heparin infusion as per sliding scale guidelines until APTT is therapeutic (46 to 70 seconds). 2. When 2 consecutive APTTs are therapeutic, order APTT every 24 hours only (and adjust drip as needed). 3. Dosages of heparin when calculated by weight are rounded off to nearest 100 U/h. 4. Order complete blood cell and platelet count every 3 days during heparin therapy.
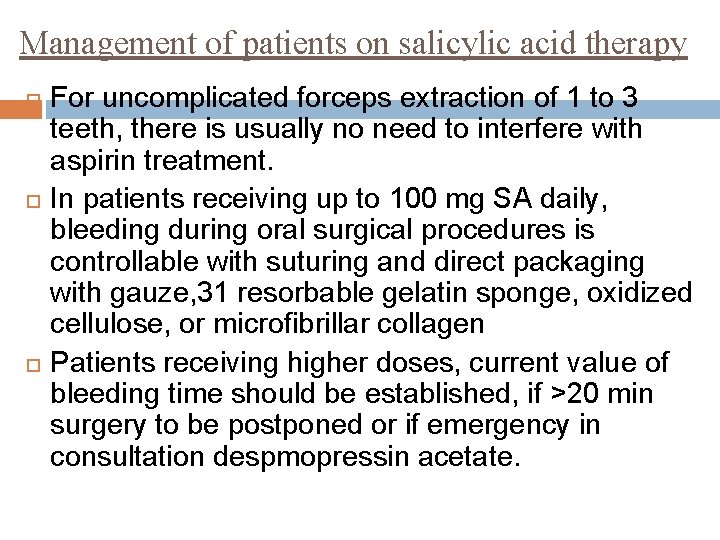
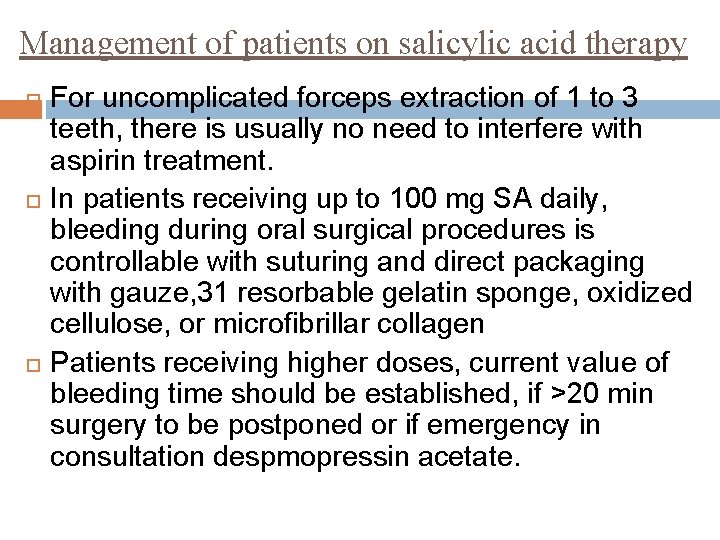
Management of patients on salicylic acid therapy For uncomplicated forceps extraction of 1 to 3 teeth, there is usually no need to interfere with aspirin treatment. In patients receiving up to 100 mg SA daily, bleeding during oral surgical procedures is controllable with suturing and direct packaging with gauze, 31 resorbable gelatin sponge, oxidized cellulose, or microfibrillar collagen Patients receiving higher doses, current value of bleeding time should be established, if >20 min surgery to be postponed or if emergency in consultation despmopressin acetate.
Patients on Aspirin with hemophilia or uremia medical advice & to discontinue aspirin for 7 days before the procedure.
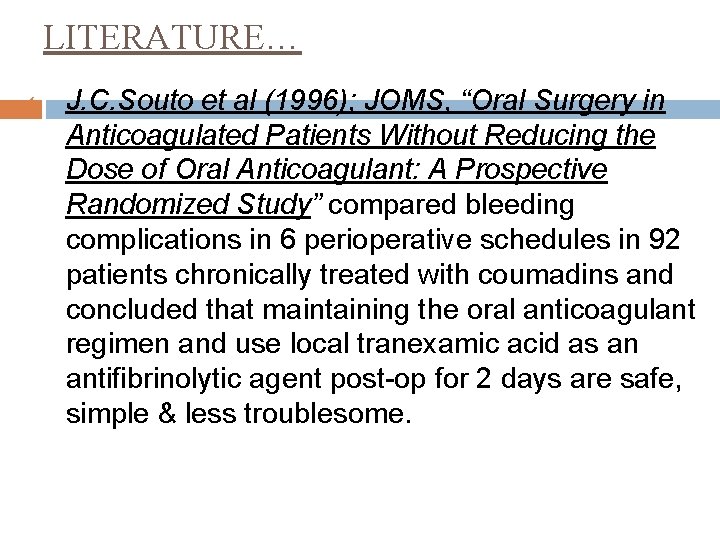
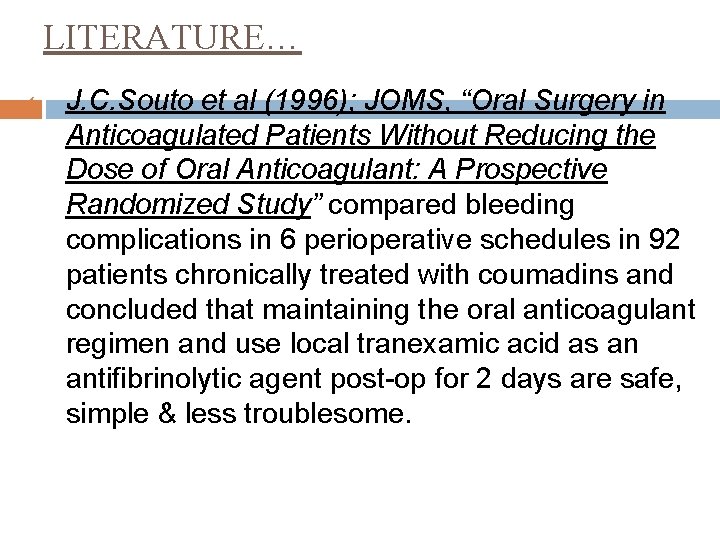
LITERATURE… 1. J. C. Souto et al (1996); JOMS, “Oral Surgery in Anticoagulated Patients Without Reducing the Dose of Oral Anticoagulant: A Prospective Randomized Study” compared bleeding complications in 6 perioperative schedules in 92 patients chronically treated with coumadins and concluded that maintaining the oral anticoagulant regimen and use local tranexamic acid as an antifibrinolytic agent post-op for 2 days are safe, simple & less troublesome.
2. P. Devani et al (1998); BJOMS, “Dental extractions in patients on warfarin: is alteration of anticoagulant regime necessary? ” studied a controlled group of 32 and experimental group of 33 patients on warfarin under local anesthesia on an outpatient basis and proposed that provided the INR is within therapeutic range of 2. 0 to 4. 0 and local measures are used to control postoperative bleeding, there is no justification in altering warfarin treatment prior to dental extractions in these patients, and thereby exposing them to the risk of thromboembolism.
3. G. Carter et al (2003); IJOMS, “Tranexamic acid mouthwash— A prospective randomized study of a 2 -day regimen vs 5 -day regimen to prevent postoperative bleeding in anticoagulated patients requiring dental extractions, ” conducted a prospective randomized study analysing the use of 4. 8% tranexamic acid post-op mouthwash over 2 days vs 5 days to prevent bleeding. 85 patients (21 -86 years). Gp-A for 2 days Gp-B for 5 days by same surgeon on ambulatory basis, assessed 1, 3 & 7 th day for bleeding and proposed that 2 day course was equally effective.
4. K. Webster et al (2000); BJOMFS, “Management of anticoagulation in patients with prosthetic heart valves undergoing oral & maxillofacial operations” gives guidelines for minor surgical procedures asthe anticoagulation regimen does not require alteration if INR <4. 0, if INR >4. 0 warfarin should be discontinued & surgery to be done when INR is therapeutic range. Use of LA with vasoconstrictor and local hemostatic methods is recommended, & operative field should be irrigated with 4. 8% tranexamic acid. Sockets and mucoperiosteal flaps should then be sutured & oxidized cellulose gauze(Surgicel) placed in socket. Oral rinsing 4. 8% TA sol 10 ml for 2 min qid for 7 days
For Major surgery(parotidectomy or neck dissection) Discontinue warfarin on 3 evenings before addmission, & admitted on day before surgery. Inj. LMWH in prophylactic dose if INR<2. 0 On day of surgery INR checked to ensure the PT is within normal limits(INR <1. 3) & prophylactic dose of LMWH 2 hr pre-op given If INR =not normal range vit-K 1 mg i. v. which brings INR in accepted range in 2 -3 hrs. Warfarin is started at night of surgery at a double dose. INR should be checked daily & dose adjusted.

Emergency surgery… If can be postponed for few hours-oral anticoagulation can be partially reversed by vitk 1 mg i. v. If immediate surgery is required, fresh frozen plasma or prothrombin complex conc should be given to correct anticoagulation & hematologist’s advice is invaluable.

SUMMARY & CONCLUSION. . Surgery is the main oral healthcare hazard to the patient with a bleeding tendency, which is mostly caused by the use of anticoagulants The traditional management entails the interruption of anticoagulant therapy for dental surgery to prevent hemorrhage. However, this practice may increase the risk of a potentially life-threatening thromboembolism.
The management of oral surgery procedures on patients treated with anticoagulants should be influenced by several factors: � extent and urgency of surgery, � laboratory values, � treating physician’s recommendation, � available facilities, � dentist expertise, and � patient’s oral, medical, and general condition.
References. . Medical Problems in Dentistry-Cawson & scully K. D. Tripathi-Pharmacology Reference Articles � Clinics of North America � IJOMS � BJOMS � OOOR
Thankyou. .
 Streptokinase mechanism of action
Streptokinase mechanism of action Anticoagulant
Anticoagulant Kathryn connors md
Kathryn connors md Blood red color code
Blood red color code Anticoagulant
Anticoagulant Thrombolytic vs anticoagulant
Thrombolytic vs anticoagulant Anticoagulant drugs
Anticoagulant drugs Anticoagulant examples
Anticoagulant examples Anticoagulant
Anticoagulant Rocking chair therapy for dementia patients
Rocking chair therapy for dementia patients Periodontal therapy in female patients
Periodontal therapy in female patients Ch 56 oral and maxillofacial surgery
Ch 56 oral and maxillofacial surgery Chapter 26 oral and maxillofacial surgery
Chapter 26 oral and maxillofacial surgery Chapter 56 oral and maxillofacial surgery
Chapter 56 oral and maxillofacial surgery Oral placement therapy for speech clarity and feeding
Oral placement therapy for speech clarity and feeding Psychoanalytic vs humanistic
Psychoanalytic vs humanistic Bioness integrated therapy system price
Bioness integrated therapy system price Psychoanalytic therapy is to as humanistic therapy is to
Psychoanalytic therapy is to as humanistic therapy is to Professionally presented
Professionally presented Proudly presented by
Proudly presented by Comparing kamikaze and the prelude
Comparing kamikaze and the prelude Procedure text how to charge handphone battery
Procedure text how to charge handphone battery Which idea is presented in both passages?
Which idea is presented in both passages? Plant assets natural resources and intangible assets中文
Plant assets natural resources and intangible assets中文 Presented below
Presented below Young and dyslexic poem
Young and dyslexic poem Cause and effect text structure clue words
Cause and effect text structure clue words How is mr hyde presented as a frightening outsider
How is mr hyde presented as a frightening outsider Name presentation
Name presentation Family feud presented by
Family feud presented by Macbeth act 5 scene 5
Macbeth act 5 scene 5 Conic sections
Conic sections Presenters name
Presenters name