Opioids in SNF Jonathan M Evans MD MPH

- Slides: 31
Opioids in SNF Jonathan M. Evans MD MPH CMD FACP
Goals of This Session • Support you in your role, setting • Develop practical, actionable strategies to make you and your patients more comfortable • Practice problem solving around familiar scenarios
Needs Assessment: • What questions/concerns/worries do you have? • What challenges confront you?
Opioids In SNF: (Some) Challenges • War on Opioids (and those who prescribe them? ) • Fear • Fragmented care across care settings, practitioners • Isolation of SNF – Limited clinical info, follow-up, referral options for new admissions – Communication challenges, barriers • Limited resources compared to other settings (Pharmacy, nursing, internet, consultations, support, etc) • Access to meds
Opioids In SNF: (Some) Challenges Cont’d • • • Med storage issues /diversion risks Chain of custody for meds, Rxs Vulnerable populations Geriatric issues Regulations (i. e re: Orders, Rxs) compared to hospital • Avoidable emergencies/ problems related to admission/care planning • Many challenges with Rxs, Faxes
Some Advantages/Opportunities • Access to PT/OT for pain relief • Consultant pharmacist/ pharmacist resources
Cases
80 year old Woman s/p ORIF for Hip Fracture • Transferred to SNF 8 pm on Friday PM. Arrives in severe pain. Has not had pain meds since beofre noon. Has a prescription for oxycodone from hospital “ 5 mg 1 -2 tabs q 4 -6 hrs prn” • LTC pharmacy will not fill prescription. .
44 Year-old homeless man with history of substance abuse admitted after staged procedure for prosthetic knee joint infection. • On IV antibiotics x 8 weeks. Morphine sulfate extended release started in hospital BID.
Call from Nursing Facility at 6 pm On New Years: Re: Meds Didn’t Arrive • You wrote six prescriptions for Class 2 drugs for your patients running low on meds. They were faxed at 8 am. None of the meds arrived today from pharmacy. • Pharmacy now closed • Nurse called pharmacist on call. “We never received the faxes. ” • You have fax confirmations for each one
66 year old patient with chronic osteomyelitis associated with sacral wound. Going on leave of absence for three • The Patientwith wants family to take scheduled medsdays. with him, including Dilaudid tabs and diazepam
75 year old woman with metastatic cancer. Takes Morphine XR bid and IR q four hrs PRN • Resident of facility for two months. Now out of narcotics. • You have written multiple prescriptions for 30 day supply of each med. You have repeatedly been told that pharmacist needs a new prescription. A total of six months worth of both meds has been prescribed thus far.
Issues: • • Admission issues/ Acquiring medications Prescription management Managing/monitoring reorders/refills Discharging meds with narcotics
Prescription Management • Communication and documentation are key – Communicate what, to whom? – Document what, where? – Faxes? – Processes
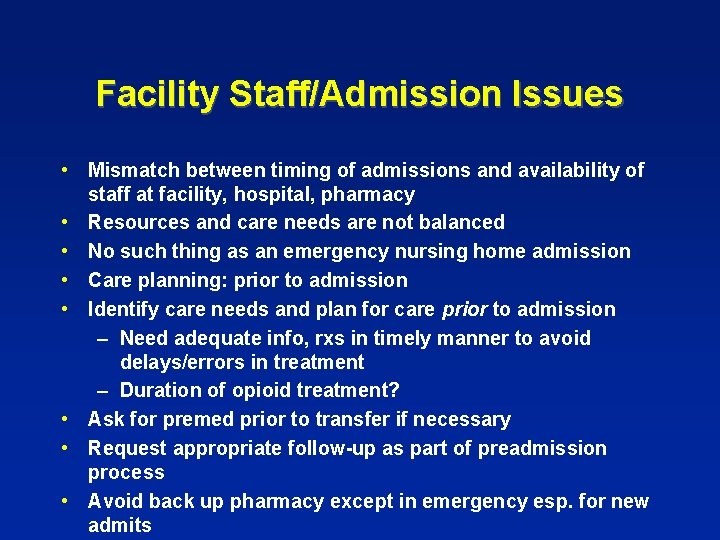
Facility Staff/Admission Issues • Mismatch between timing of admissions and availability of staff at facility, hospital, pharmacy • Resources and care needs are not balanced • No such thing as an emergency nursing home admission • Care planning: prior to admission • Identify care needs and plan for care prior to admission – Need adequate info, rxs in timely manner to avoid delays/errors in treatment – Duration of opioid treatment? • Ask for premed prior to transfer if necessary • Request appropriate follow-up as part of preadmission process • Avoid back up pharmacy except in emergency esp. for new admits
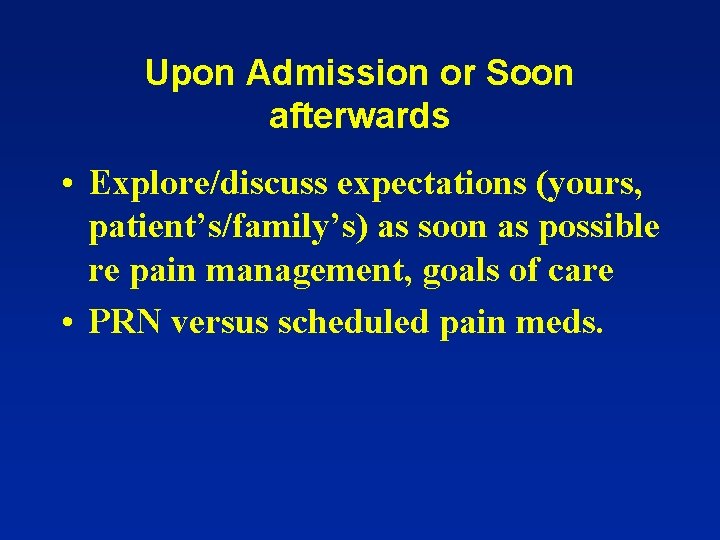
Upon Admission or Soon afterwards • Explore/discuss expectations (yours, patient’s/family’s) as soon as possible re pain management, goals of care • PRN versus scheduled pain meds.
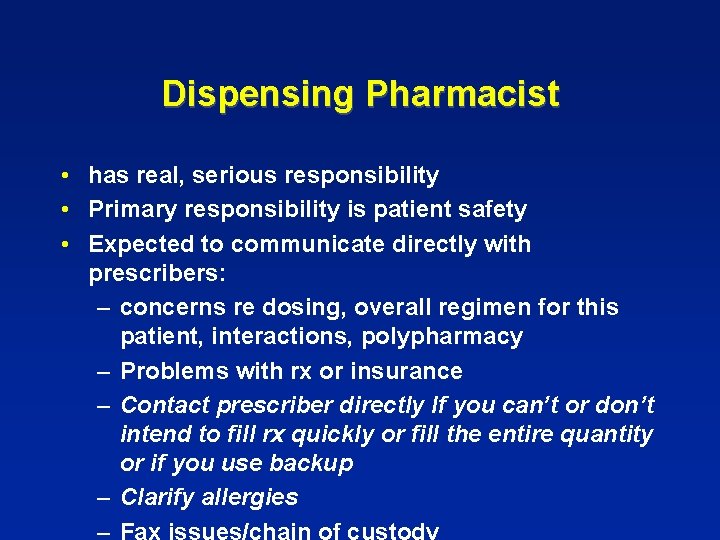
Dispensing Pharmacist • has real, serious responsibility • Primary responsibility is patient safety • Expected to communicate directly with prescribers: – concerns re dosing, overall regimen for this patient, interactions, polypharmacy – Problems with rx or insurance – Contact prescriber directly If you can’t or don’t intend to fill rx quickly or fill the entire quantity or if you use backup – Clarify allergies – Fax issues/chain of custody
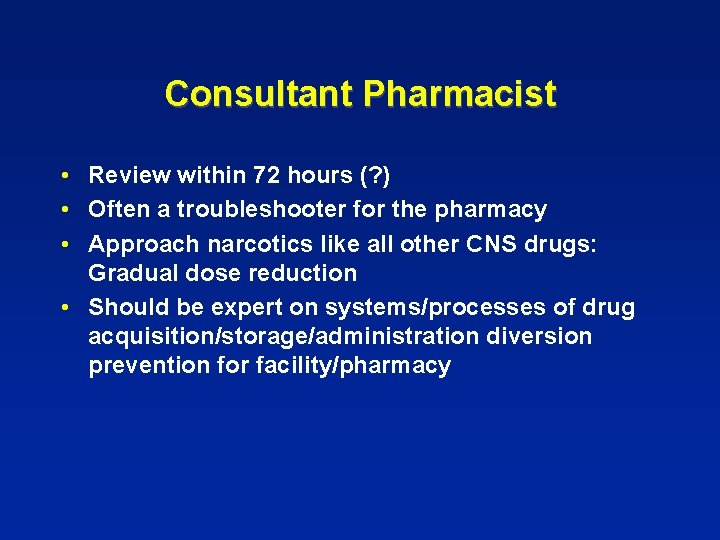
Consultant Pharmacist • Review within 72 hours (? ) • Often a troubleshooter for the pharmacy • Approach narcotics like all other CNS drugs: Gradual dose reduction • Should be expert on systems/processes of drug acquisition/storage/administration diversion prevention for facility/pharmacy
Role of Pharmacists • Changing • Historic task of counting pills has largely been taken over by others/technology incl. packaging • Future of the profession relies entirely upon using/sharing expertise regarding medications with others • Mismatch between pharmacists’ training, abilities, and their jobs today • Greater human interaction is required now and in the future • Retrospective review of meds that have already been dispensed is somewhat problematic.
Med Director • Should meet face to face with consultant pharmacist regularly • Should be involved with pharmacist in developing, overseeing systems and processes re: medication issues including processes to prevent potentially unnecessary or risky drugs prior to drugs being dispensed as well ass to ensure access to necessary meds in a timely manner. • Increased responsibility for GDRs.
Backup pharmacy Issues/ problems • Meds often dispensed in bottles in conflict with facility policies – Increased risk of errors/diversion? • May void the remainder of a prescription, without prescriber’s knowledge resulting in meds running out or concern re: diversion • May undermine efforts/goal of earlier care planning, other proactive measures
Med cart issues – Increased of errors, other problems when too many meds in cart – Issues when patient discharged to hospital – Tension between having too many and too few meds available – Consultant pharmacist should inspect med carts periodically along with nursing supervisors
Diversion prevention • • Chain of custody of meds, prescriptions Keep copy of all Rxs sent and/or faxed Medication cart management Prompt destruction of discontinued meds Organized effort at GDR when appropriate Direct observation of medication administration Crush meds or nonoral meds an issue if patient may be pocketing or hoarding meds
Drug Addicts admitted to SNFs • A very frequent occurrence • Connecting them to resources, followup important but difficult or impossible • History/records often lacking • Care planning, active steps, documentation increasingly important to address this issue • Close followup after discharge important. Limit quantities dispensed at discharge • Ongoing referral for long-term care residents to pain management, psych, etc
Emergency Fill for Narcotics (without a hard RX) • Should be reserved for true medical emergencies, unusual circumstances • Often patient not seen at time of emergency request • Should not be a frequent occurrence • Rate of emergency fills an indicator or poor quality of care and/or poor systems/processes
(Geriatric) Prescribing Issues Re: Pain, Narcotics • Pain meds may have delayed onset, longer duration in older patients • One size doesn’t fit all • Be very cautious in narcotic naïve patients • Sustained release narcs may cause less delirium • Long acting meds, transdermal fentanyl not for acute pain management, esp. in narcotic naive patient • Be wary/ careful with patients admitted from home on big doses of meds • NSAIDs fairly high risk in older patients. Assume all have renal insufficiency • Tramadol less well tolerated in older patients.
Pain Rx by Mechanism of Pain • Different neurotransmitters, neuron types /receptors involved with different mechanisms of pain • Optimal treatment of pain therefore depends upon pain mechanism • (patients may have more than one type of pain)
Neuropathic pain: • Narcotics inefficient. Anticonvulsants, tricyclics (nortriptyline or desiprimine, not amitriptyine) may be preferable • ? Methadone (with caution) among narcotics • Gabapentin vs. pregabalin? • TENS, capsaicin, lidocaine, desensitization massage among other options

Musculoskeletal Pain • Antiinflammatory drugs for acute inflammation ONLY (red/warm/swollen/tender joints or tender soft tissues) • Steroid vs. NSAID • PT/OT first line treatment in SNF • Pt/OT may also cause musculoskeletal pain in (disuse/overuse syndrome) • Acetaminophen is first line drug but may be ineffectve • Opioids may be useful/necessary in some patients for chronic pain • SNF a fairly safe place for long-term opioid use
Visceral Pain • Pain from stretch or blockage of hollow viscus Usually an acute pain issue though may be intermittent, chronic cause (i. e. stone disease) • Narcotics are mainstay • May be a palliative care issue (i. e. advanced cancer)
Opioid Prescribing in the SNF • Teamwork is key • Involve others (pharmacists, pain specialists, psychiartrists etc) depending upon underlying issues If you are uncomfortable • Refer post acute patients for followup from the people that sent you the patient • Arrange followup after discharge • Communication with receiving physician after discharge advisable • Approach to chronic pain meds similar to other CNS drugs