Nutrition Teresa V Hurley MSN RN Factors Affecting




- Slides: 47
Nutrition Teresa V. Hurley. MSN, RN
Factors Affecting Food Habits • Physical — – geographic location, – food technology, – income • Physiologic — – health, – hunger – stage of development • Psychosocial — – – culture, religion, tradition, education

Psycho/Social

Developmental
Human Growth and Development • Infants through School-Age -rapid growth with high protein, vitamin, mineral and energy demand; infant doubles birth weight in 4 -5 months; triples weight at 1 year Breast Feeding encouraged -reduces allergy risks What other factors?
Infants • • Formula Cow’s milk causes GI bleeding Kidney’s unable to handle Research: milk in 1 st and the development of Type I Diabetes later in life • Honey and corn syrup maybe be source of botulism
Introduction of Solid Food • 4 to 6 months of age • Introduce one at a time 4 to 7 days apart to identify allergies
Toddlers • Picky eaters around 18 months of age • 3 meals and 3 snacks • Calcium and phosphorous for bone growth Hot dogs, candy, nuts, grapes, raw veggies, popcorn frequently lead to choking deaths
School Age • Growth slower and steadier • Check for protein, vitamins A and C • High fat, sugar and salt intake lead to childhood obesity compounded by sedentary lifestyle
Adolescents • Energy needs increase to meet the increase metabolic demands of growth • protein. , calcium, iron (females) and muscle growth (males) • Fad dieting, oral contraceptive use, fast foods, skipping meals • Eating disorders anorexia nervosa and bulimia nervosa
Young and Middle-Age • Energy demands less • Fetal development affected by mother’s nutritional status and weight at time of conception; protein, calcium, iron, folic acid • Lactation: protein, calcium, Vitamins A, C, B; avoid caffeine, alcohol and drugs
Older Adults • Lifestyle • Income • Lack of teeth, dentures, thirst sensation less with resultant dehydration (confusion, weakness, hot dry skin, rapid pulse • Nutrient dense foods: peanut butter, cheese, eggs, cream and meat-based soups


Cultural
Alternative Food Patterns • Vegetarian – Ovolactovegetarian (no meat, fish and poultry but will have milk and eggs) – Lactovegetarians (drink milk but no eggs) – Vegans (plant foods) -A Zen vegan eats brown rice, grains, herb teas -Fruitarians eat only fruits, nuts, honey and olive oil
Religious Dietary Restrictions • Islam (no pork, caffeine, ritual slaughter of animals; Ramadan fasting sunrise to sunset for a month) • 7 th day Adventists (no pork, shellfish, alcohol, vegetarianism encouraged) • Hinduism (no meats) • Latter Day Saints (no alcohol, tobacco , caffeine)
Risk Factors for Poor Nutritional Status • Developmental factors • Alcohol abuse • State of health • Medications • Megadoses of nutrient supplements
Anorexia -poor appetite related to ketosis an appetite suppressant Surgical Procedures with resultant pain Diagnostic testing (NPO, bowel evacuations)
Promoting Appetite • Keep environment free of odors • Oral hygiene • Insulin, glucosteriods, thyroid hormones affect metabolism • Antifungals alter taste • Psychotropics affect appetite, nausea, alter taste
Nursing Interventions • Risk for Aspiration – Assess LOC – Decrease or absent gag or cough reflex – Surgical procedures – Neuromuscular impairments – Sensory impairments
Nursing Interventions • • Upright position Food placed stronger side of mouth Thickening agents Rate of eating slower to provide for chewing and swallowing • Use clock as guide to identify food location for visually impaired • Use assistive devices (padded forks, spoons etc)
Nursing Interventions • Client to direct order and preferences of food items to eat
Therapeutic Diets • NPO nothing by mouth • Clear Liquid: broth, bouillon cubes, tea, carbonated beverages, clear fruit juices, popsicles • Full Liquid: add to clear liquid diet smooth textured dairy products as custard, refined cooked cereals, pureed veggies, all fruit juices
Diets Continued • Pureed ( continue to add to the previous) scrambled eggs, pureed meats, veggies, fruits, mashed potatoes and gravy • Mechanical Soft (add to the previous) ground or diced meats, flaked fish, cottage cheese, rice, potaotes, pancakes, light breads, cooked vegetables and fruits, canned fruits, bananas, soups, peanut butter
Diets Continued • Soft Low Residue: add pastas, casseroles, moist tender meats, canned cooked fruits and vegetables, desserts, cakes, cookies without nuts or coconut • High Fiber: add fresh uncooked fruits, steamed veggies, bran, oatmeal, dried fruits • Low Sodium: 4 g (no added salt) 2 gm to 500 mg Na diets require selective choices
Medications • Stimulate appetite – Periactin – Megace – Marinol’
Diets Continued • Low Cholesterol 300 mg/day in accordance with AHA guidelines for serum lipid reduction • Diabetic: Food exchanges with balanced intake of protein, CHO and fats and vary according to energy demands as exercise, pregnancy, illness • Regular NO restrictions
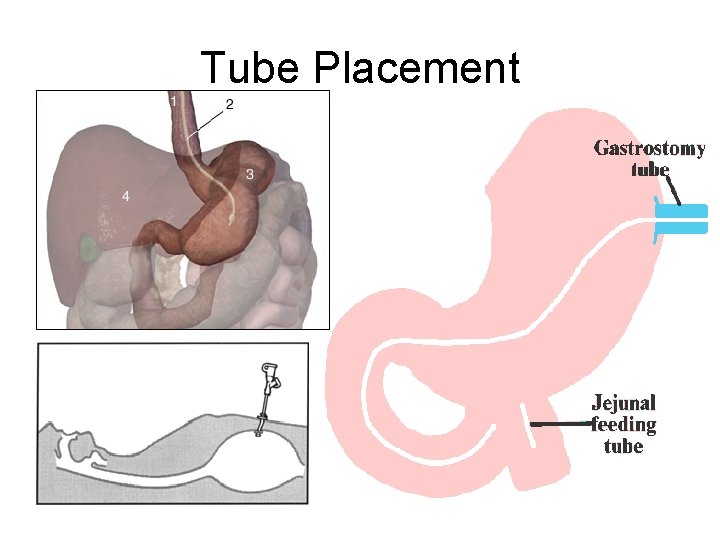
Enteral Nutrition • Short-term nutritional support – Nasogastric – nasointestinal route • Long-term nutritional support – Enterostomal tube created into • stomach (gastrostomy) – Percutaneous endoscopic gastrostomy (PEG) • jejunum (jejunostomy)
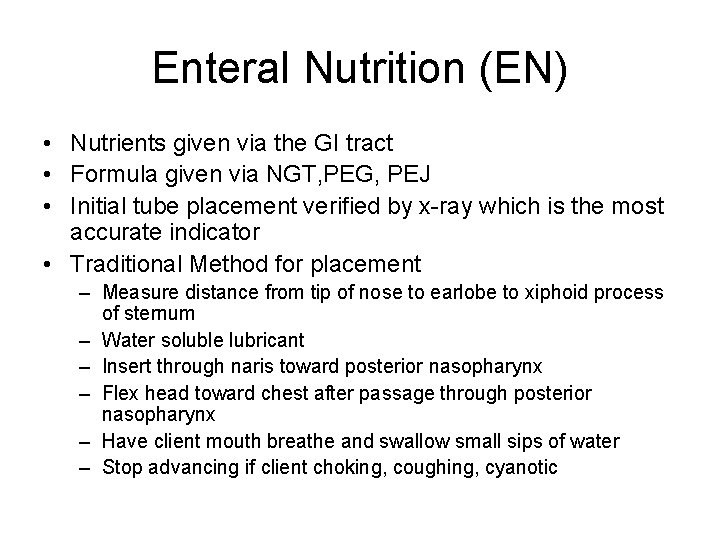
Enteral Nutrition (EN) • Nutrients given via the GI tract • Formula given via NGT, PEG, PEJ • Initial tube placement verified by x-ray which is the most accurate indicator • Traditional Method for placement – Measure distance from tip of nose to earlobe to xiphoid process of sternum – Water soluble lubricant – Insert through naris toward posterior nasopharynx – Flex head toward chest after passage through posterior nasopharynx – Have client mouth breathe and swallow small sips of water – Stop advancing if client choking, coughing, cyanotic
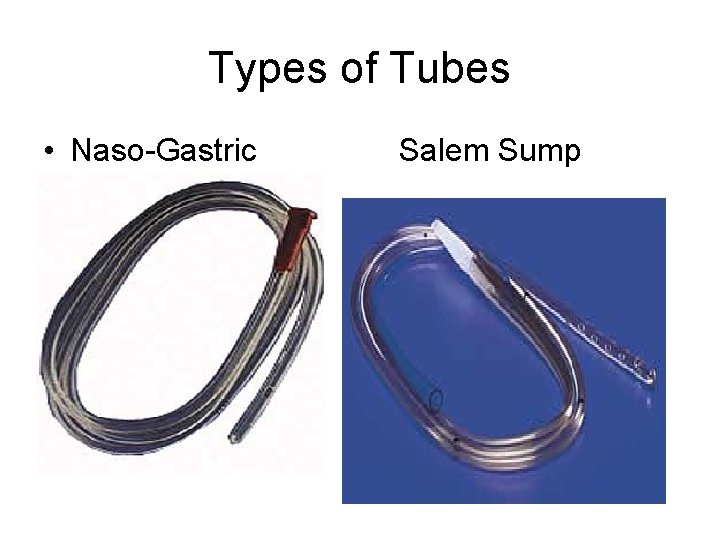
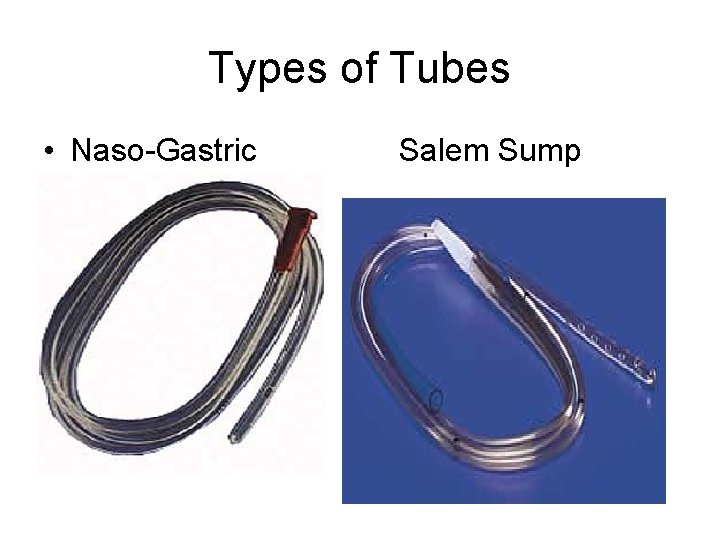
Types of Tubes • Naso-Gastric Salem Sump
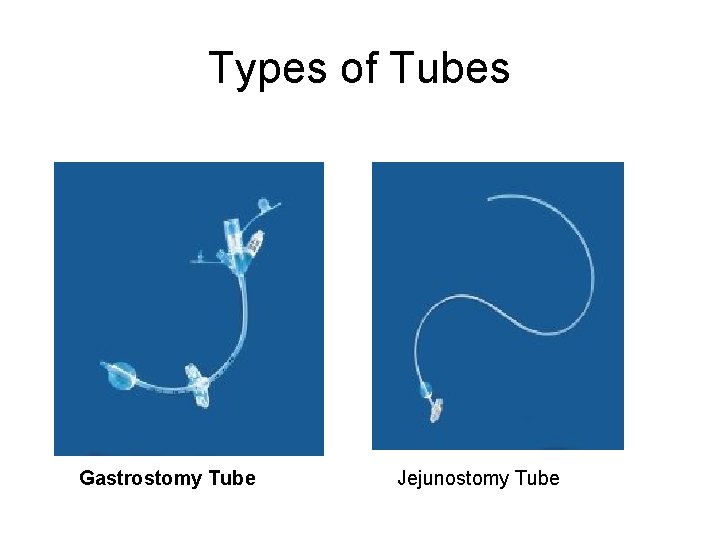
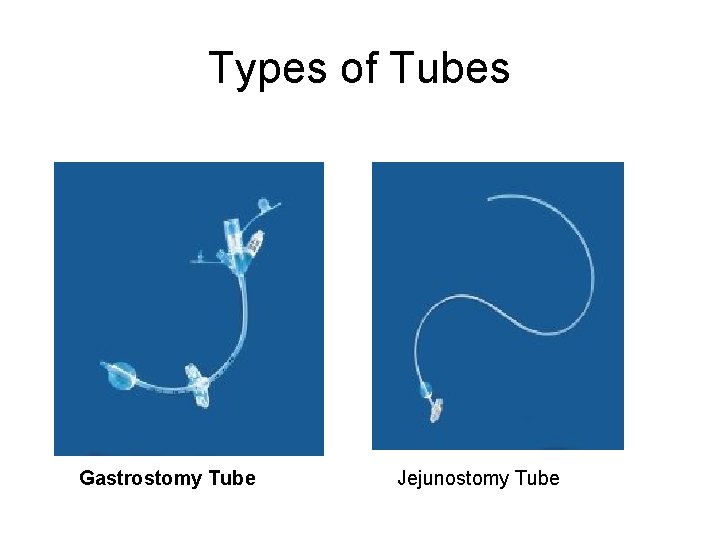
Types of Tubes Gastrostomy Tube Jejunostomy Tube
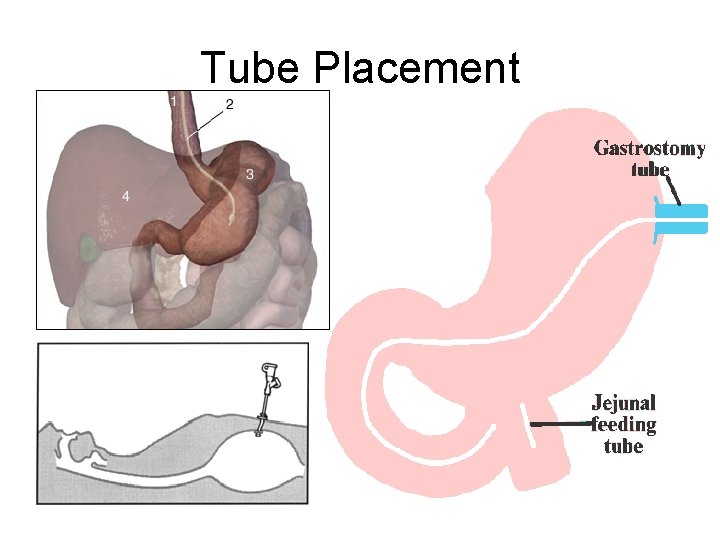
Tube Placement
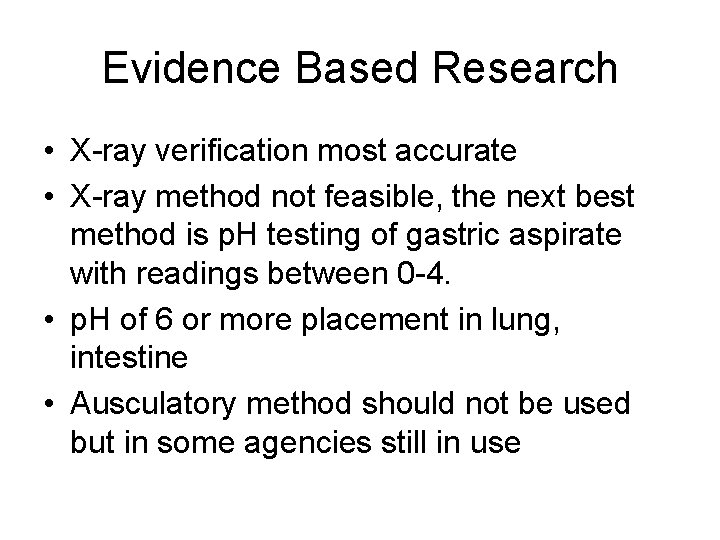
Evidence Based Research • X-ray verification most accurate • X-ray method not feasible, the next best method is p. H testing of gastric aspirate with readings between 0 -4. • p. H of 6 or more placement in lung, intestine • Ausculatory method should not be used but in some agencies still in use
Gastrostomy or Jejunostomy Tube • HOB elevated 45 degrees • Auscultate for bowel sounds • Verify placement by testing p. H of gastric aspirate • Check gastric residual – If over 100 ml notify MD – Would you replace the gastric contents? – Would you stop the feeding?
Some Complications of Feeding • • • Aspiration Tube displacement Cramping from using cold formula Diarrhea Impaired skin integrity Nosocomial infections
Parenteral Nutrition • Total parenteral nutrition (TPN) • Partial parenteral nutrition (PPN)
Total Parenteral Nutrition TPN- Total Parenteral Nutrition • complete form of nutrition – protein – CHO – fat – vitamin – minerals =
Indications for TPN • Inability to eat – Ventilator dependency – Additional surgery – Altered mental status affecting ability to eat • Diminished nutrient intake – Anorexia – Dyspepsia from medications – Gastrointestinal problems including nausea, vomiting, diarrhea, and distention • Increased nutrient requirements – Hyper metabolism – Nitrogen loss caused by surgery and corticosteroid administration – Malabsorption
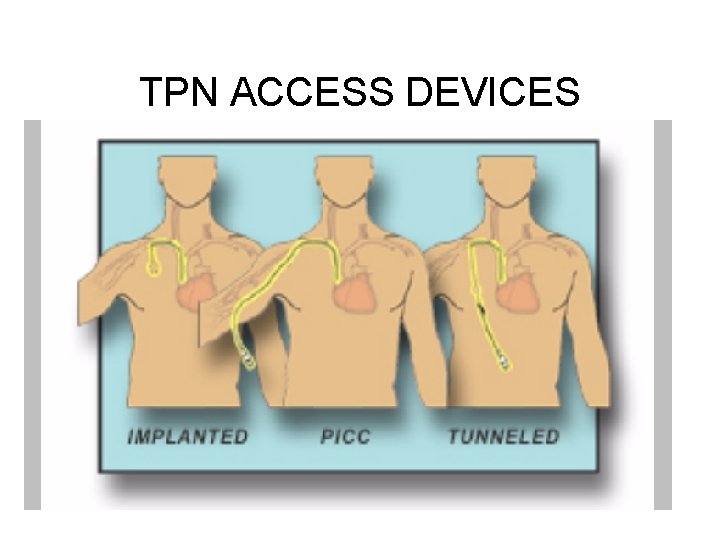
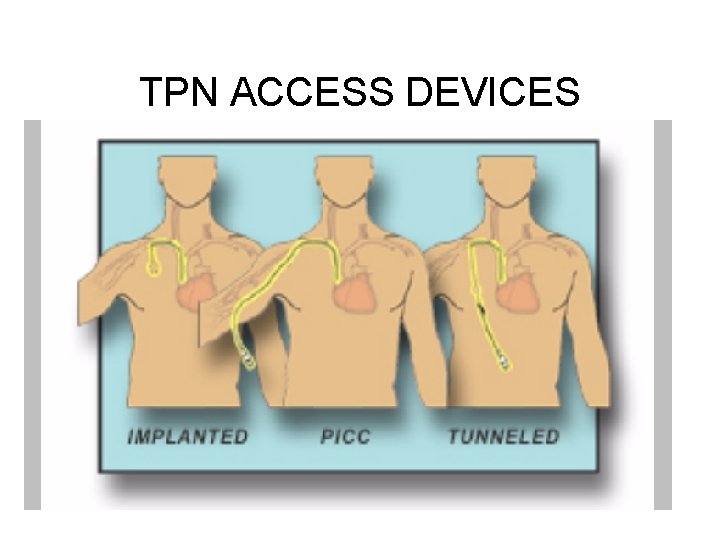
TPN ACCESS DEVICES
Complications of Parenteral Nutrition • Insertion problems • Fluid, electrolyte, and acid-base imbalances • Infection • Phlebitis • Metabolic alterations
PN Complications • Electrolyte and Mineral imbalances: refeeding syndrome -high concentrations of glucose leads to endogeneous insulin production which leads to -cations moving from inter to intracellular (potassium, magnesium and phosphorus) which leads to cardiac dysarrthymias, CHF. Respiratory distress, convulsions, coma, death
Complications of PN • Rapid administration of hypertonic dextrose leads to osmotic diuresis and dehydration – DO NOT SPEED UP IF BEHIND – DO NOT STOP LEADS TO HYPOGLYCEMIA
Glucose Testing • Diabetes is a metabolic disorder – Inadequate insulin production by pancreatic beta cells or – Insulin resistance whereby glucose unable to cross sell membrane • Cellular starvation • Fluid and electrolyte imbalances
Diabetes • Hypoglycemia: pancreas secretes glucagon • Hyperglycemia: pancreas secretes insulin – Polyuria – Polydyspia – Polyphagia – Glycosuria – Ketones
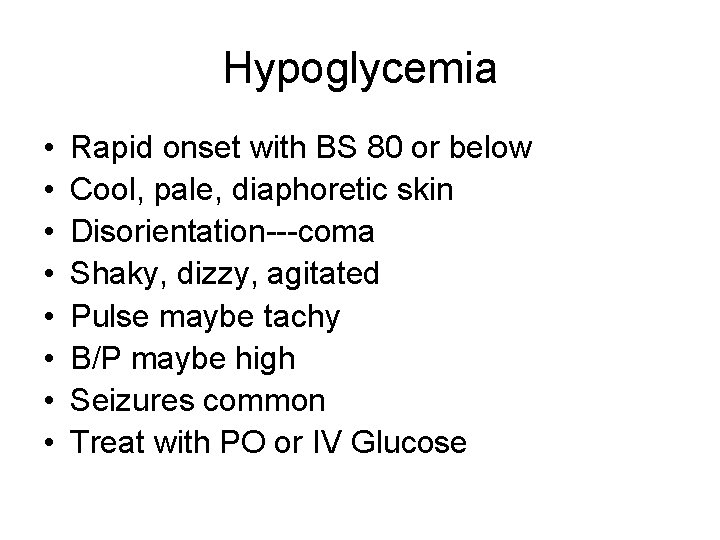
Hypoglycemia • • Rapid onset with BS 80 or below Cool, pale, diaphoretic skin Disorientation---coma Shaky, dizzy, agitated Pulse maybe tachy B/P maybe high Seizures common Treat with PO or IV Glucose
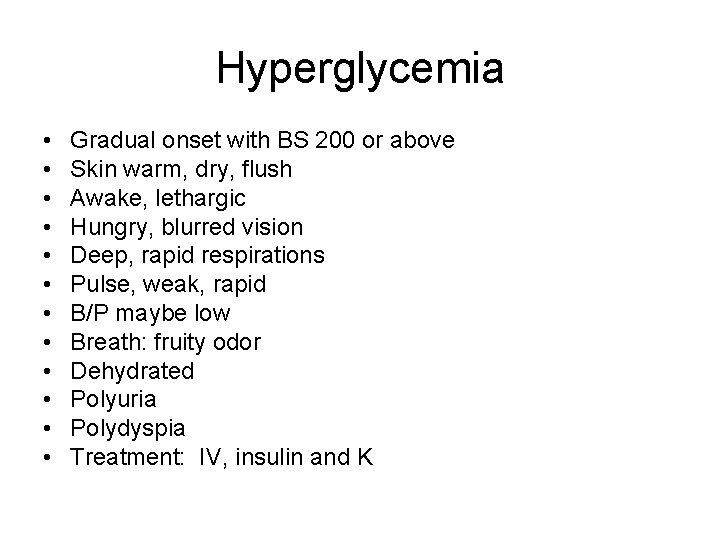
Hyperglycemia • • • Gradual onset with BS 200 or above Skin warm, dry, flush Awake, lethargic Hungry, blurred vision Deep, rapid respirations Pulse, weak, rapid B/P maybe low Breath: fruity odor Dehydrated Polyuria Polydyspia Treatment: IV, insulin and K
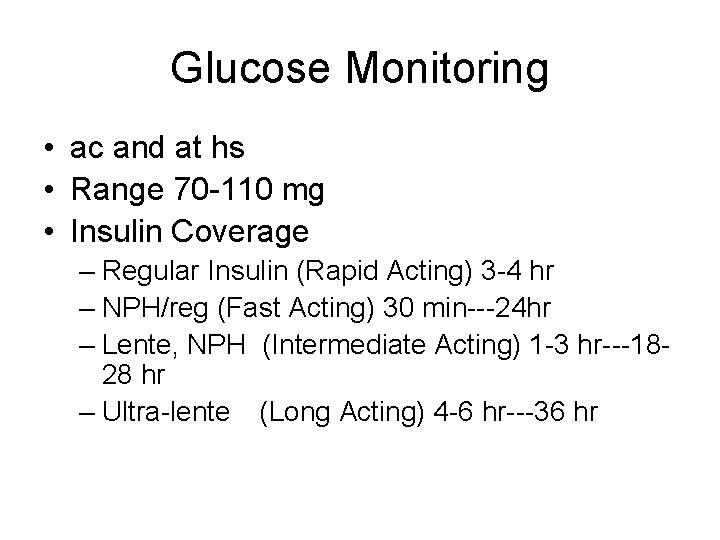
Glucose Monitoring • ac and at hs • Range 70 -110 mg • Insulin Coverage – Regular Insulin (Rapid Acting) 3 -4 hr – NPH/reg (Fast Acting) 30 min---24 hr – Lente, NPH (Intermediate Acting) 1 -3 hr---1828 hr – Ultra-lente (Long Acting) 4 -6 hr---36 hr
 Dene hurley
Dene hurley Lynda hurley
Lynda hurley Siobhan hurley
Siobhan hurley Tape v hurley
Tape v hurley Cubemap generator
Cubemap generator Kirsten hurley
Kirsten hurley Dr. jeffrey hurley
Dr. jeffrey hurley Who made history
Who made history Hurley range
Hurley range Hurley phantom 120
Hurley phantom 120 Bebo messenger
Bebo messenger Msn messenger chat rooms
Msn messenger chat rooms Odev
Odev Msn
Msn Msn 1886
Msn 1886 Chamberlain fnp practicum
Chamberlain fnp practicum Msn yoga
Msn yoga Messenger
Messenger Coreg to metoprolol conversion
Coreg to metoprolol conversion Msn ph
Msn ph Alverno direct entry msn
Alverno direct entry msn Msn msft
Msn msft Msn signs
Msn signs Legal nurse consultant websites
Legal nurse consultant websites Instant messenger msn
Instant messenger msn Bruit msn
Bruit msn Msn fritzbox
Msn fritzbox Msn
Msn Msn dating
Msn dating Msn wetter jakutsk
Msn wetter jakutsk Msn quiz
Msn quiz Msn
Msn Msn
Msn Msn cloud storage
Msn cloud storage Cardiac output and stroke volume
Cardiac output and stroke volume Factors affecting runoff
Factors affecting runoff Ct wimage
Ct wimage Factors affecting drug absorption biopharmaceutics
Factors affecting drug absorption biopharmaceutics Factors affecting learning
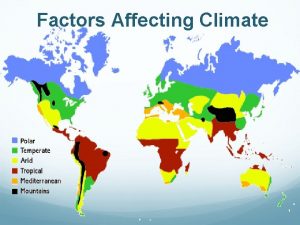
Factors affecting learning What are the factors affecting the climate
What are the factors affecting the climate Erythroid precursors
Erythroid precursors Types of promotion mix
Types of promotion mix Functional strategy and strategic choice
Functional strategy and strategic choice No.of pins attracted
No.of pins attracted Factors influencing human resource management
Factors influencing human resource management Psychological factors affecting sports performance
Psychological factors affecting sports performance Oncotic pressure vs hydrostatic
Oncotic pressure vs hydrostatic Factors affecting media planning
Factors affecting media planning