North Carolina Preparedness Emergency Response Research Center NCPERRC

- Slides: 45
North Carolina Preparedness & Emergency Response Research Center (NCPERRC) Translating Evidence into Action: Enhancing the Impact of PHEP-Funded Workforce Infrastructure in North Carolina September 20, 2011
North Carolina Preparedness & Emergency Response Research Center (NCPERRC) Jennifer A. Horney, Ph. D, MPH Research Assistant Professor UNC Center for Public Health Preparedness and Department of Epidemiology, Gillings School of Global Public Health, University of North Carolina Lou Turner, Dr. PH, Director Deputy Section Chief, Epidemiology Section, North Carolina Division of Public Health
Presentation Outline • • NC PERRC Background Objectives Methods Results Next Steps Translating Evidence to Action
North Carolina Preparedness and Emergency Response Research Center (NCPERRC) • One of 9 Preparedness and Emergency Response Research Centers (PERRCs) supported by CDC • Studying 4 North Carolina public health systems (accreditation, surveillance, workforce infrastructure, and health alert network) • Partnership with the North Carolina Division of Public Health (NC DPH) and NC Association of Local Health Directors (NCALHD)
Background • NCDPH established several unique preparedness related workforce programs using PHEP funds: – Public Health Regional Surveillance Teams (PHRSTs) – Hospital-based Public Health Epidemiologist (PHEs) Program
Public Health Regional Surveillance Teams (PHRSTs) • NCPDH established the PHRSTs in 2001 – To support local public health capacity to prevent, prepared for, respond to and recover from public health incidents and events • 7 PHRSTs support regions of between 7 and 17 local health departments (LHDs) • Teams originally included 4 members (physician / epidemiologist, nurse / epidemiologist, industrial hygienist and administrative assistant)
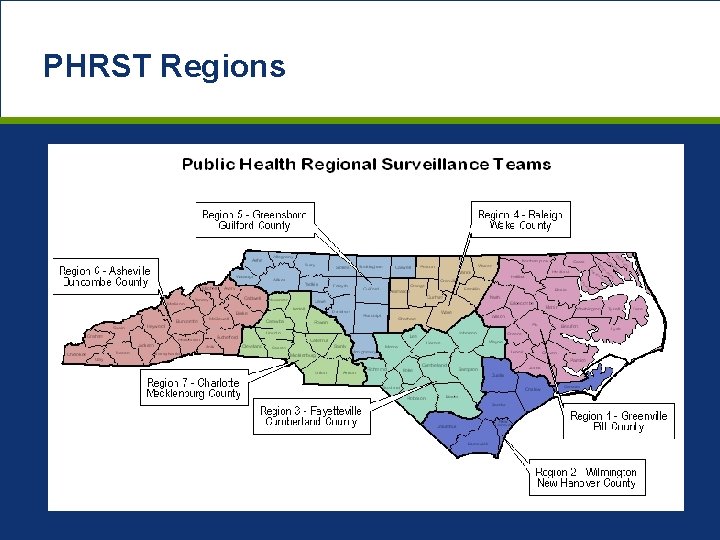
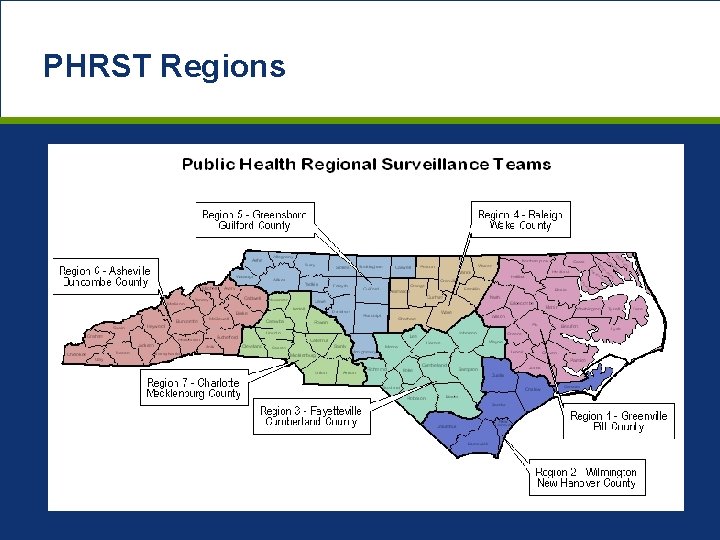
PHRST Regions
Public Health Epidemiologist (PHE) Program • NCDPH established the PHE program in 2003 – To improve communication between hospitals and state and local public health departments • 11 PHEs based in the state’s largest hospitals • Responsibilities include: – surveillance, detection, and monitoring of communityacquired infections and potential bioterrorism events, assisting LHDs with investigations, educating clinicians and enhancing communication
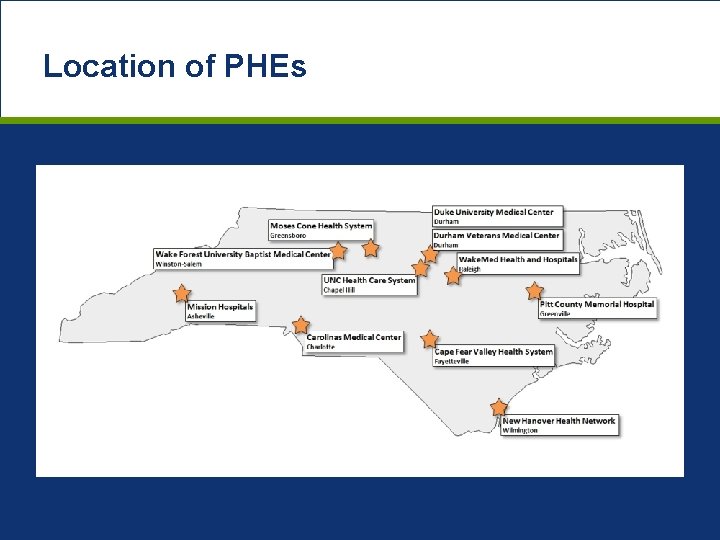
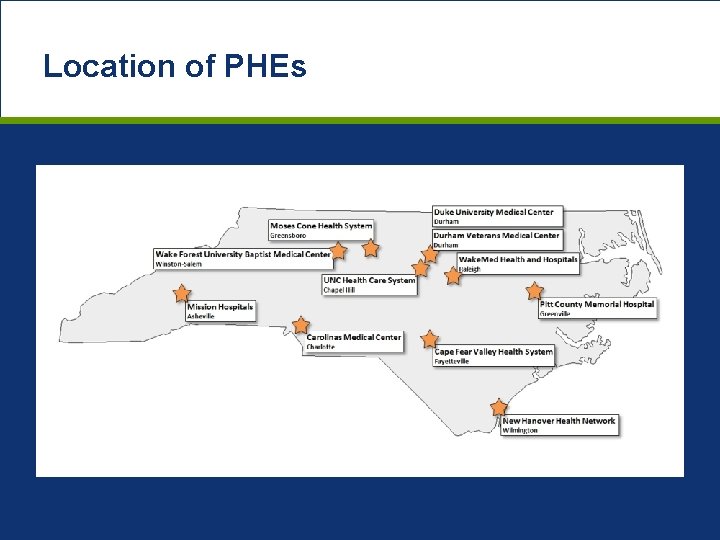
Location of PHEs
Relevance of Studying These Systems • National trend of regionalizing public health preparedness workforce after 2001 has not been well assessed • Programs are a major investment for PHEP funds (as % of grant) • Need to determine if investments are improving core preparedness functions, including response and surveillance
Objective • Analyze the structural capacity of the PHRST and PHE programs and determine impact of support and services provided by these programs on public health preparedness in North Carolina

Methods
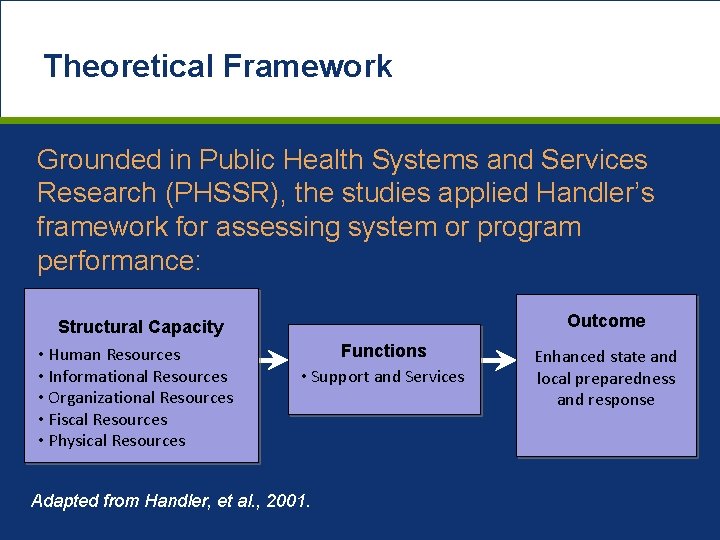
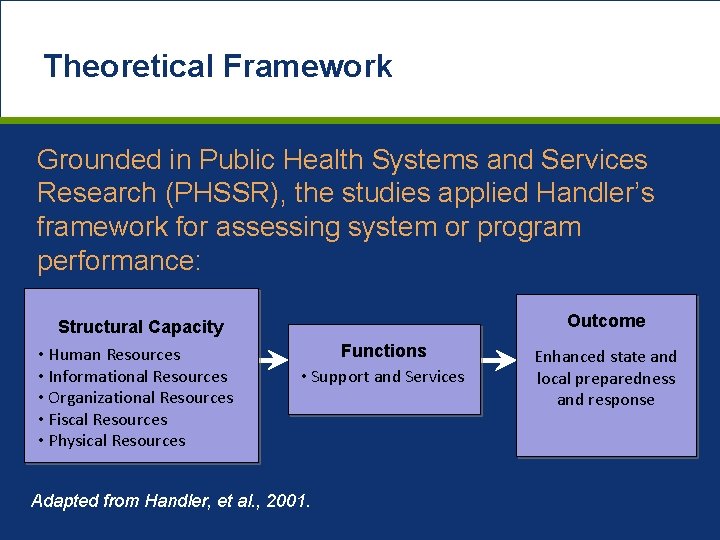
Theoretical Framework Grounded in Public Health Systems and Services Research (PHSSR), the studies applied Handler’s framework for assessing system or program performance: Structural Capacity • Human Resources • Informational Resources • Organizational Resources • Fiscal Resources • Physical Resources Outcome Functions • Support and Services Adapted from Handler, et al. , 2001. Enhanced state and local preparedness and response
Data Collection • Online and paper surveys • Face-to-face interviews • Collection of available secondary data (demographic, funding, and personnel)
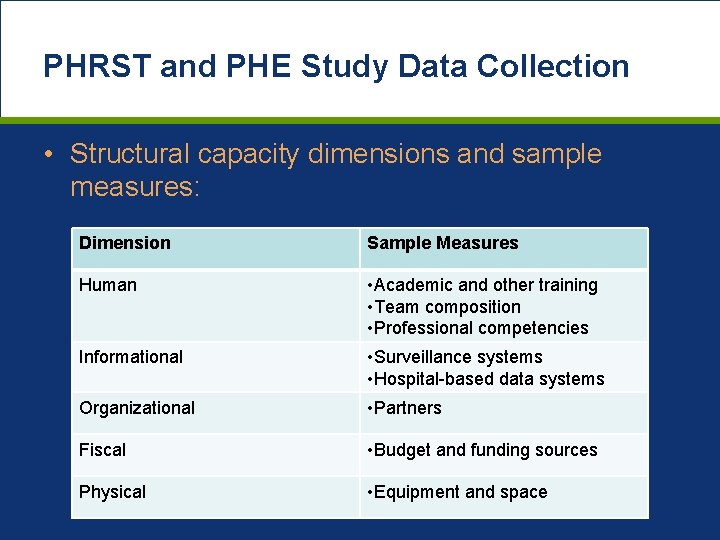
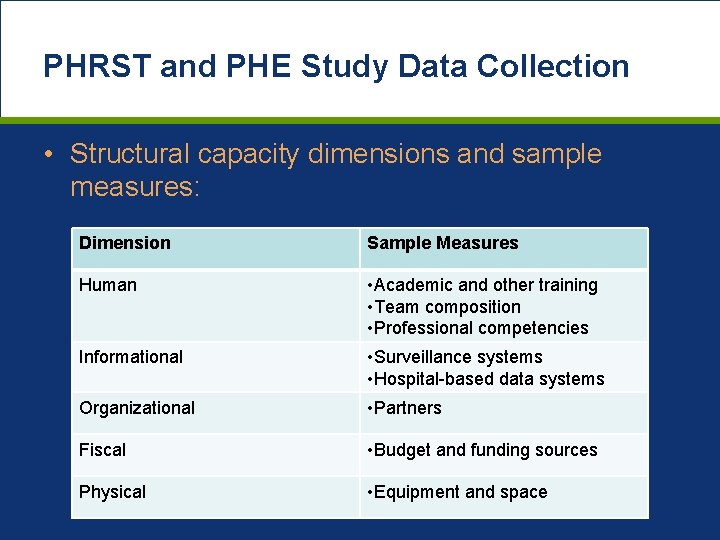
PHRST and PHE Study Data Collection • Structural capacity dimensions and sample measures: Dimension Sample Measures Human • Academic and other training • Team composition • Professional competencies Informational • Surveillance systems • Hospital-based data systems Organizational • Partners Fiscal • Budget and funding sources Physical • Equipment and space
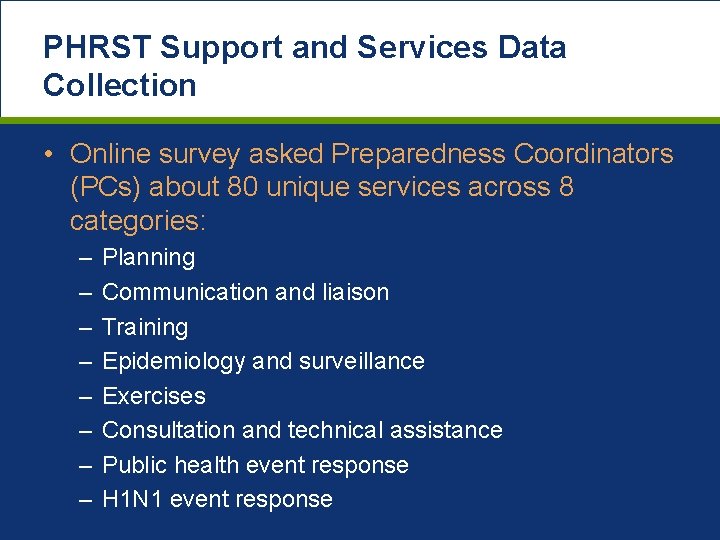
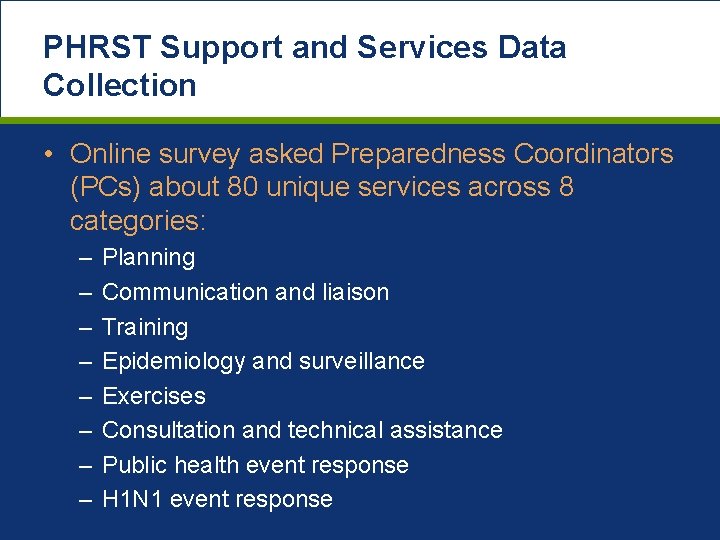
PHRST Support and Services Data Collection • Online survey asked Preparedness Coordinators (PCs) about 80 unique services across 8 categories: – – – – Planning Communication and liaison Training Epidemiology and surveillance Exercises Consultation and technical assistance Public health event response H 1 N 1 event response
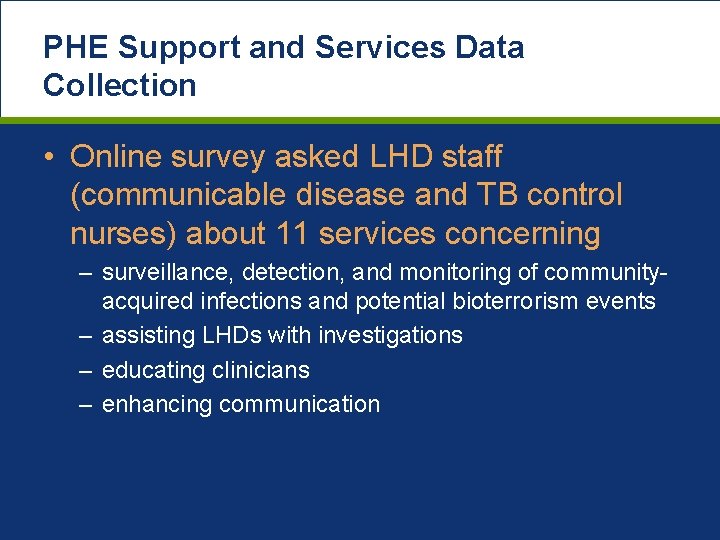
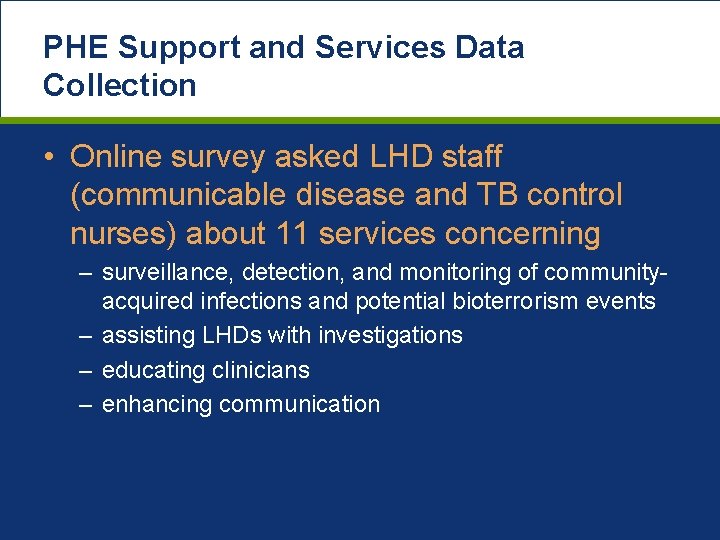
PHE Support and Services Data Collection • Online survey asked LHD staff (communicable disease and TB control nurses) about 11 services concerning – surveillance, detection, and monitoring of communityacquired infections and potential bioterrorism events – assisting LHDs with investigations – educating clinicians – enhancing communication
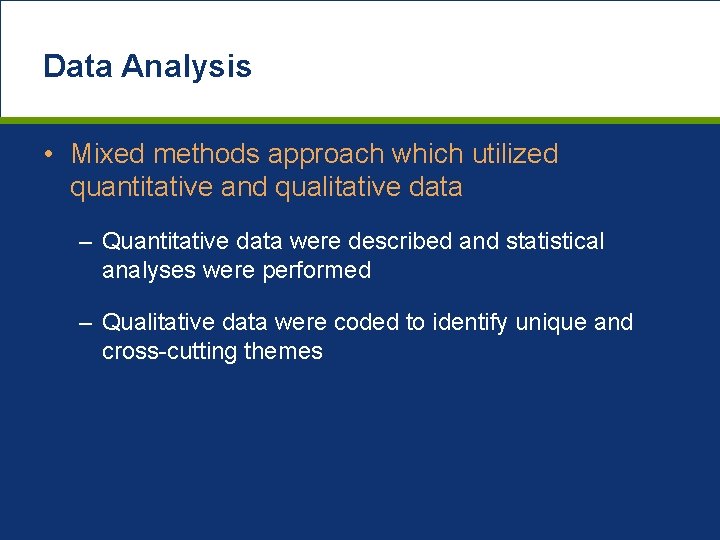
Data Analysis • Mixed methods approach which utilized quantitative and qualitative data – Quantitative data were described and statistical analyses were performed – Qualitative data were coded to identify unique and cross-cutting themes
Results: PHRST Study
PHRST Study Response Rate • Individual and team surveys and semistructured interviews with each PHRST: – 100% response rate • Electronic survey of NC LHD PCs: – 98% response rate
PHRST Support and Services • A core group of 26 (33%) support and services were received by 75% or more LHDs • Significant variation (p<. 05) by PHRST region between the support and services received by LHDs overall and in 3 of the 8 categories: – Communication and liaison – Epidemiology and surveillance – Training • Variation could not be explained by county- or LHD-level variables, which suggests structural capacity effects variation
PHRST Structural Capacity • Most variation was seen in human resources • Variation in team composition was associated with differences in support and services – Teams with MD / DO or epidemiologist had larger budgets and provided more support and services – Teams with pharmacists had more partners – Teams who received directives from more groups (e. g. state and local) provided more assistance in 7 of 8 categories
PHRST Conclusions • Appropriate capacity is essential to achieving the mission of PHRSTs in the NC public health system • Re-evaluate ideal staffing based on what is needed to provide support and services requested by LHDs • Develop a “core package” of 26 types of support and services that were provided to 75% of LHDs
PHRST Conclusions • All PHRSTs reported extensive partner networks – Can they be leveraged to fill identified gaps in PHRST support and services? • More support and services were provided by PHRSTs who received directives from the most groups – Can accountability be clarified to maximize the utility of the PHRSTs to both state and local stakeholders?
Results: PHE Study
PHE Study Response Rates • PHE survey, assessment forms, and interviews – 100% response rate • Semi-structured interviews with PHEs’ hospital supervisors – 100% response rate • Semi-structured interviews with NCDPH respondents – 100% response rate • Online survey of LHD nurses – 83% response rate (74 local health departments)
PHE Services Provided to LHDs • PHEs interacted with an average of 10 LHDs each (range, 2 – 20) • 74% of the CD and TB nurses indicated that they interacted with a PHE in the past year • Of the 88 respondents that interacted with a PHEs, 64% interacted with a single PHE, while 36% interacted with 2 – 5 PHEs
PHE Services Provided to LHDs • Over 85% of LHD respondents reported that the PHE program “greatly” or “somewhat” enhanced: – Communication between hospitals and local public health with regard to communicable disease reporting and investigation – Timeliness and completeness of communicable disease reporting in the community – LHD’s ability to be more efficient in reporting and investigating cases/clusters of communicable disease
PHE Services Provided to NCDPH • Conducting syndromic surveillance of communityacquired infections and potential bioterrorism events • Playing an important role in state flu and respiratory disease surveillance • Providing a communication channel to clinicians and other hospital staff • Providing a bridge between local/state public health • Conducting special studies for NCDPH/CDC
PHE Structural Capacity • Informational Resources – PHEs access/monitor: • North Carolina’s syndromic surveillance system • An average of 4 hospital-based data systems each (e. g. admissions reports, death reports, lab reports, and electronic medical records) – PHEs greatest surveillance challenge: Need to review data from multiple systems to get a complete picture for a single patient
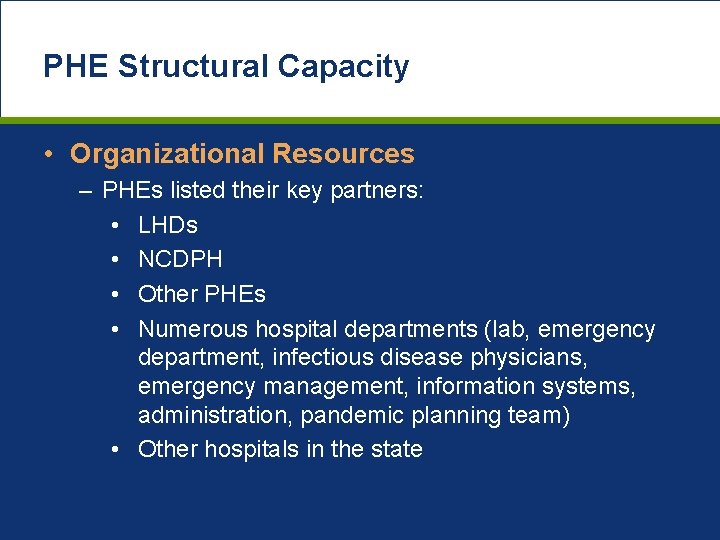
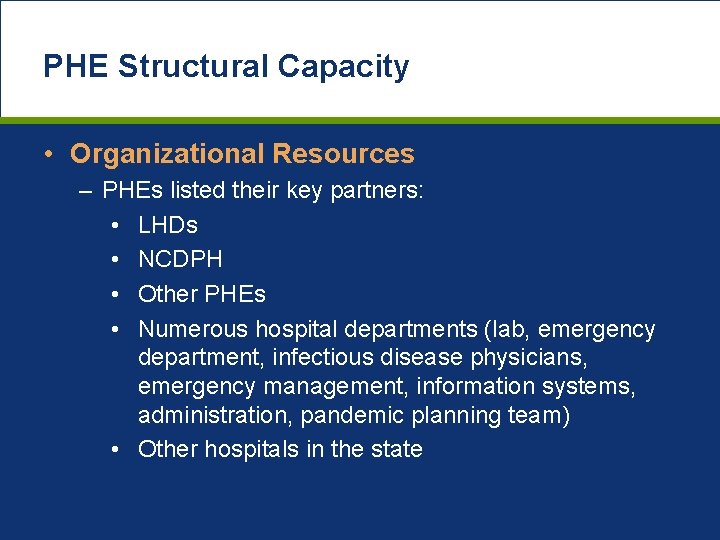
PHE Structural Capacity • Organizational Resources – PHEs listed their key partners: • LHDs • NCDPH • Other PHEs • Numerous hospital departments (lab, emergency department, infectious disease physicians, emergency management, information systems, administration, pandemic planning team) • Other hospitals in the state
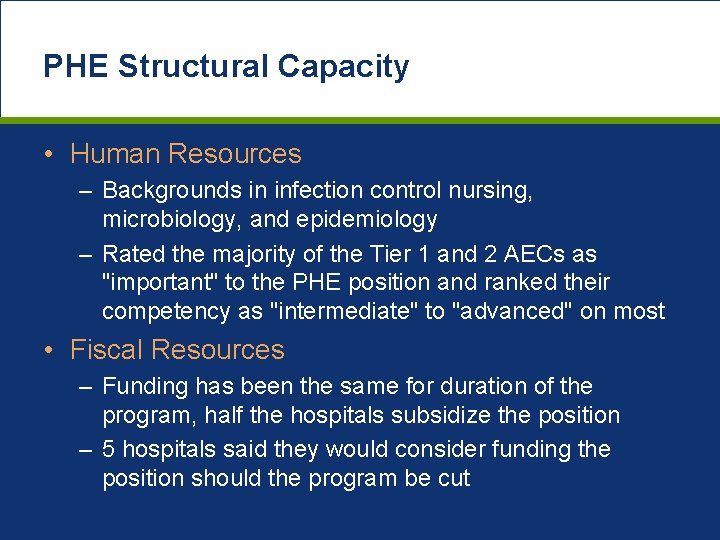
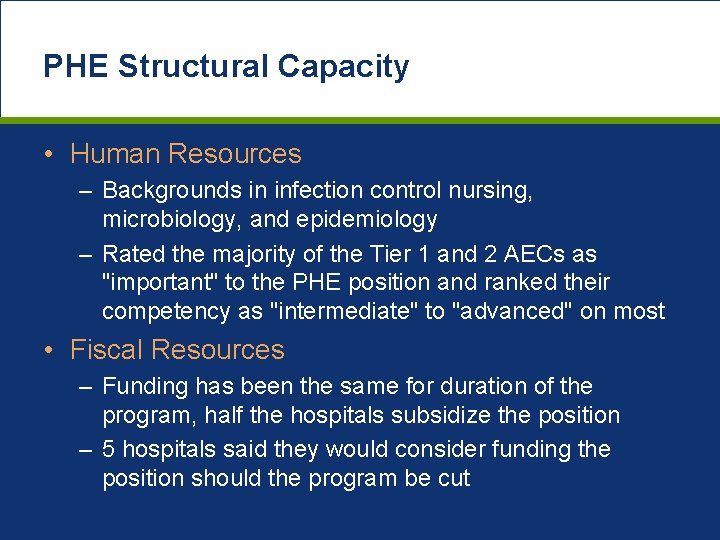
PHE Structural Capacity • Human Resources – Backgrounds in infection control nursing, microbiology, and epidemiology – Rated the majority of the Tier 1 and 2 AECs as "important" to the PHE position and ranked their competency as "intermediate" to "advanced" on most • Fiscal Resources – Funding has been the same for duration of the program, half the hospitals subsidize the position – 5 hospitals said they would consider funding the position should the program be cut
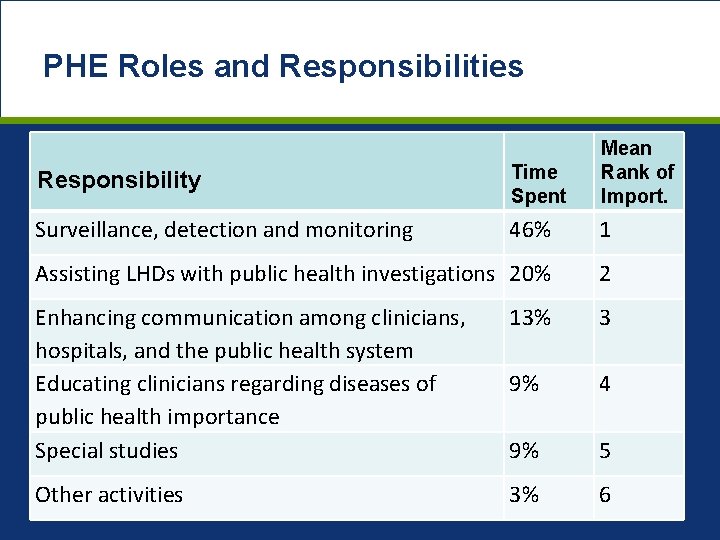
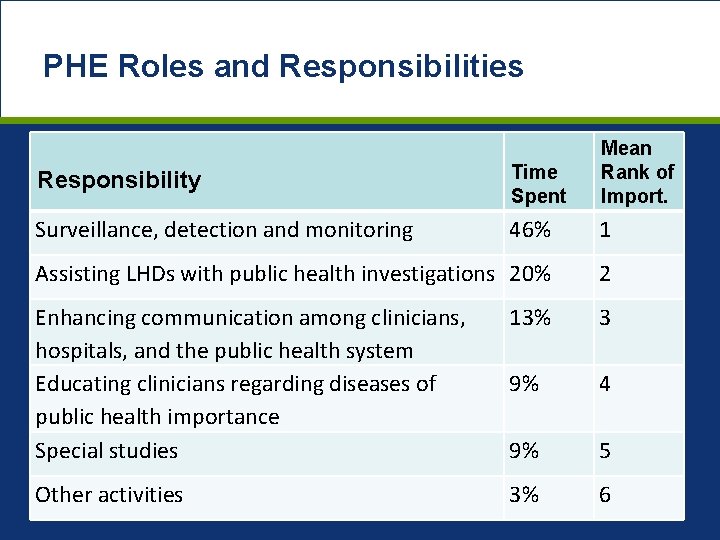
PHE Roles and Responsibilities Responsibility Time Spent Mean Rank of Import. Surveillance, detection and monitoring 46% 1 Assisting LHDs with public health investigations 20% 2 Enhancing communication among clinicians, hospitals, and the public health system Educating clinicians regarding diseases of public health importance Special studies 13% 3 9% 4 9% 5 Other activities 3% 6
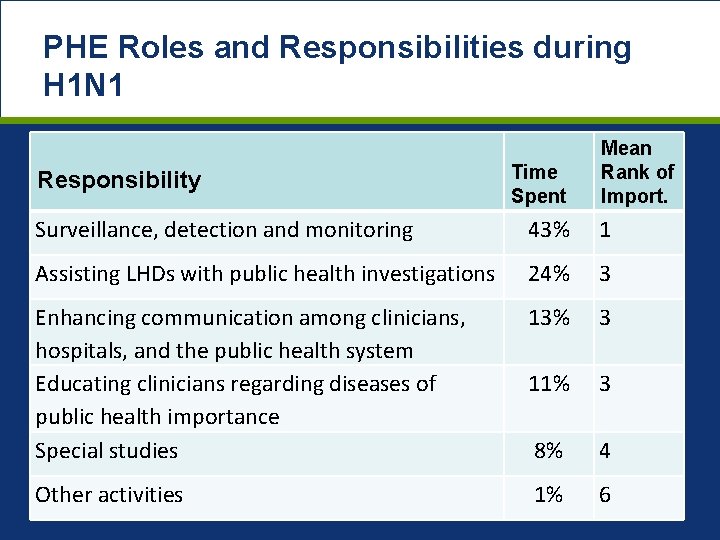
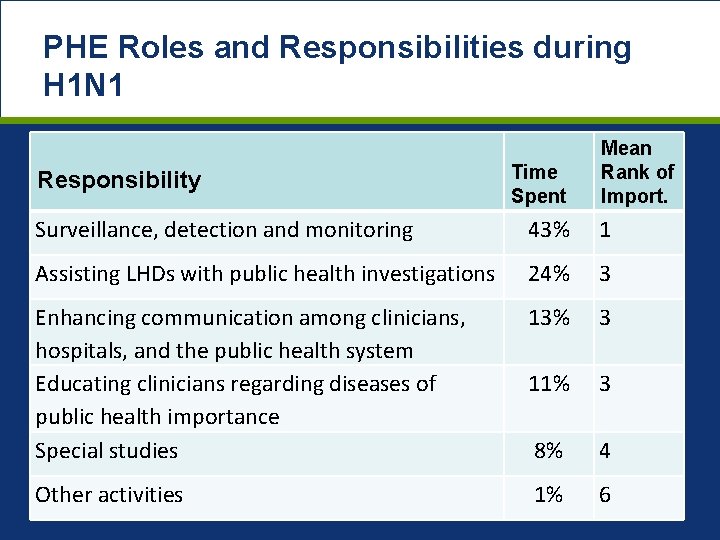
PHE Roles and Responsibilities during H 1 N 1 Responsibility Time Spent Mean Rank of Import. Surveillance, detection and monitoring 43% 1 Assisting LHDs with public health investigations 24% 3 Enhancing communication among clinicians, hospitals, and the public health system Educating clinicians regarding diseases of public health importance Special studies 13% 3 11% 3 8% 4 Other activities 1% 6
Conclusions: PHE Study • PHEs play an important role in identifying and controlling both small and large outbreaks of communicable disease • During H 1 N 1 PHEs: – Provided timely data on status of H 1 N 1 at hospitals to hospital staff, LHDs, and NCDPH – Guided mitigation efforts and policy decisionmaking
Conclusions: PHE Study • Stakeholders (NCDPH, LHDs, hospitals) place a high value on the PHE program • However, not all LHDs are fully aware of the PHE program and services provided by PHEs – Suggests need for more outreach to LHDs about PHE program to increase the program’s impact
Next Steps • NCPERRC staff are working with NCDPH and PHEs on developing a promotional intervention • Continuing to work with NCDPH in strategic planning and other research needs
Next Steps • Using regional preparedness measures from LHDs (e. g. planning, surveillance, training) to further explore variation of support and services – Are the support and services PHRST provide associated with higher LHD preparedness? • Structure of PHRSTs or PHE programs have been modified, opportunity exists for us to study how the change effects support and services and overall LHD preparedness
Limitations • Not a longitudinal study designed to show progress, we did not have a baseline • No performance measurements for PHRSTs • Findings are not generalizable to other states
Translating Evidence to Action: Providing data for decision making • System-wide strategic planning process undertaken in August, 2010 • Results of study used as basis for evaluation of future mission, structure and function of regional support to Local Health Departments • Similar to the use of data from PHRST study, information will inform decisions regarding further development and investment in PHE’s
Translating Evidence to Action: Providing data for decision making • Study results can be used by PHEs and program management to assess if priority services are being provided at desired levels • Suggestions for program improvement from PHEs, NCDPH and hospital supervisors can be considered by program management as they assess the program and plan for its future
Translating Evidence to Action: Providing data for decision making • Findings shared with stakeholders through reports, presentations, and meetings • Presentations at regional and national conferences • Peer reviewed journal publications • NCPERRC staff are participating in NCDPH strategic planning
Translating Evidence to Action: What does it mean for the future? • Inform how we manage operations in the future (constrained budgets, setting priorities) • Integration of the public health capabilities • Document / Measure success of public health responses (hurricanes, H 1 N 1) • Stability of preparedness for the future
Acknowledgements • UNC – – – Pia Mac. Donald Jennifer Hegle Milissa Markiewicz Allison George Christine Bevc Carol Gunther-Mohr • NC Division of Public Health – Julie Casani – Megan Davies – Jeff Engel • NC Association of Local Health Directors – Doug Urland
Contact Information • Jennifer Horney – jen. horney@unc. edu • Lou Turner – lou. turner@dhhs. nc. gov
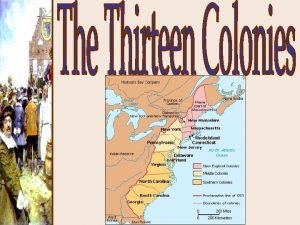
 North carolina marschland
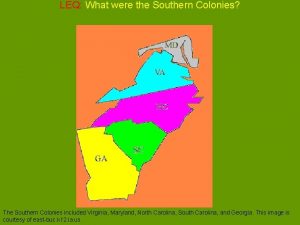
North carolina marschland Map of north carolina and south carolina
Map of north carolina and south carolina Virginia, maryland, north carolina, south carolina, georgia
Virginia, maryland, north carolina, south carolina, georgia Virginia, maryland, north carolina, south carolina, georgia
Virginia, maryland, north carolina, south carolina, georgia Chapter 5 emergency preparedness injury game plan
Chapter 5 emergency preparedness injury game plan Chapter 36 emergency preparedness and protective practices
Chapter 36 emergency preparedness and protective practices Bsa emergency preparedness
Bsa emergency preparedness National radiological emergency preparedness conference
National radiological emergency preparedness conference Chapter 36 emergency preparedness and protective practices
Chapter 36 emergency preparedness and protective practices Stake emergency preparedness plan
Stake emergency preparedness plan Cms emergency preparedness final rule
Cms emergency preparedness final rule Preparedness mitigation response recovery
Preparedness mitigation response recovery West virginia center for threat preparedness
West virginia center for threat preparedness Demand response research center
Demand response research center Nc sunshine law
Nc sunshine law Boston state abbreviation
Boston state abbreviation North carolina victim assistance network
North carolina victim assistance network Packingham v. north carolina
Packingham v. north carolina What is north carolina state bird
What is north carolina state bird Nc presbyterian pilgrimage
Nc presbyterian pilgrimage North carolina toast
North carolina toast Nchsaa transfer rules
Nchsaa transfer rules Nc famous landmarks
Nc famous landmarks What is a face jug
What is a face jug Local sluts lykens pa
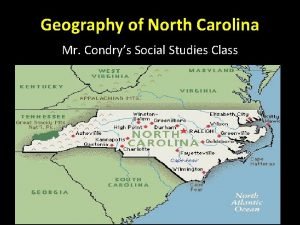
Local sluts lykens pa Geography of north carolina
Geography of north carolina Exploring north carolina
Exploring north carolina University of north carolina hematology oncology fellowship
University of north carolina hematology oncology fellowship Computer science unc chapel hill
Computer science unc chapel hill Nc state bar board of paralegal certification
Nc state bar board of paralegal certification North carolina council on developmental disabilities
North carolina council on developmental disabilities Nc lighthouses map
Nc lighthouses map South carolina geographic regions
South carolina geographic regions Demystifying the cloud
Demystifying the cloud North carolina soccer referee
North carolina soccer referee Family support network of north carolina
Family support network of north carolina South carolina landforms map
South carolina landforms map Discover north carolina's river basins
Discover north carolina's river basins South carolina teacher evaluation system
South carolina teacher evaluation system Nc medical examiner and coroner guidelines
Nc medical examiner and coroner guidelines North carolina land of contrasts
North carolina land of contrasts North carolina state university
North carolina state university Chapter 13: north carolina state government
Chapter 13: north carolina state government Who founded north carolina
Who founded north carolina North carolina referee association
North carolina referee association Residency determination service
Residency determination service