NONINVASIVE POSITIVE PRESSURE VENTILATION NIPPV ADELYN MITCHELL RN
- Slides: 13
NONINVASIVE POSITIVE PRESSURE VENTILATION NIPPV ADELYN MITCHELL, RN, BSN, CEN, BSRC NURS 5303 INFORMATION AND TECHNOLOGY
OBJECTIVES To educate the target audience of nursing students in the advanced respiratory class in regards to: • Definition/Physiology of non-invasive positive pressure ventilation (NIPPV) • Modes of NIPPV • Advantages/Disadvantages of NIPPV • Indications/contraindications of NIPPV • Application/implementation of NIPPV • Evaluation of the effectiveness of NIPPV
DEFINITION OF NIPPV External application of positive pressure ventilation to enhance respiration and ventilation of the patient exhibiting signs of respiratory distress and are: • Spontaneously breathing • Conscious and alert • Poor ventilatory drive
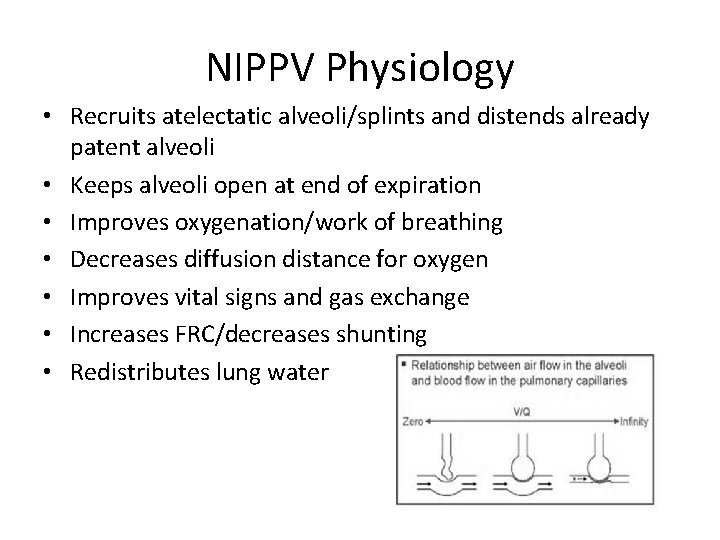
NIPPV Physiology • Recruits atelectatic alveoli/splints and distends already patent alveoli • Keeps alveoli open at end of expiration • Improves oxygenation/work of breathing • Decreases diffusion distance for oxygen • Improves vital signs and gas exchange • Increases FRC/decreases shunting • Redistributes lung water
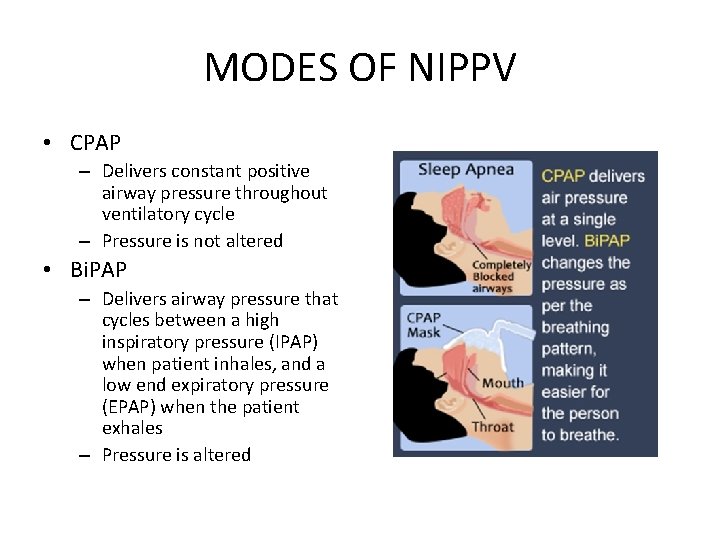
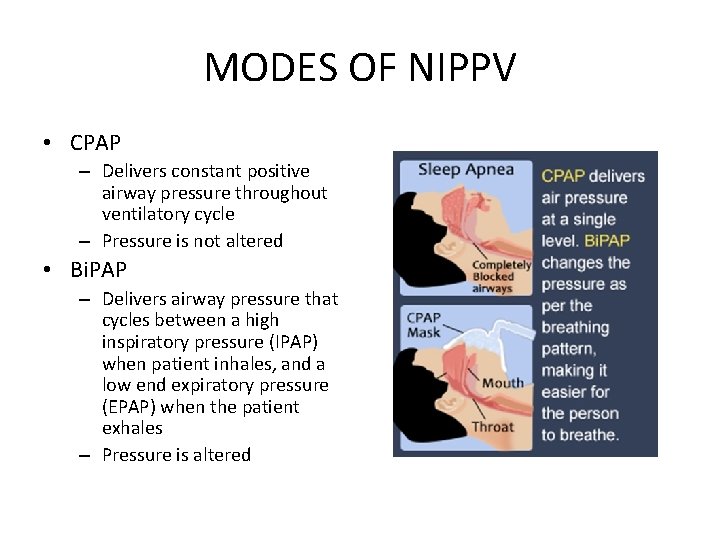
MODES OF NIPPV • CPAP – Delivers constant positive airway pressure throughout ventilatory cycle – Pressure is not altered • Bi. PAP – Delivers airway pressure that cycles between a high inspiratory pressure (IPAP) when patient inhales, and a low end expiratory pressure (EPAP) when the patient exhales – Pressure is altered
Advantages of NIPPV • Keeps airway open while you sleep. • Preservation of speech, swallowing, and physiological airway defense mechanisms • Reduced risk of airway injury • Reduced risk of nosocomial infections • Reduced length of stay in the intensive care unit • Offers short-term (typically 1 -4 days) ventilatory support • Decreases sense of dyspnea and need for endotracheal intubation
Disadvantages of NIPPV • • Gastric distention, vomiting, aspiration Drying of secretions, mucus plugging Hypotension Pneumothorax Corneal drying Anxiety Facial skin breakdown
INDICATIONS CPAP vs BIPAP Respiratory distress/hypoxemia secondary to CHF, acute pulmonary edema, pneumonia, asthma, COPD, sleep apnea • CPAP = patients without respiratory failure • Bi. PAP = patients with impending or existing respiratory failure
BIPAP
CONTRAINDICATIONS NIPPV • Pneumothorax • Respiratory arrest • Decreased level of consciousness • Hypovolemic shock • Chest trauma • Persistent nausea/vomiting • Facial anomalies/trauma/CVA • Active GI bleeding or recent surgery
IMPLEMENTATION NIPPV • Apply mask and ensure good fit with minimal leak • CPAP – Initiate CPAP at 5 -7. 5 cm. H 20 – Titrate to patient comfort and vital signs • Bi. PAP – Start with 8 -12 cm. H 20 IPAP and 4 -6 cm. H 20 EPAP – Titrate to patient comfort and vital signs
EVALUATION NIPPV • Assess breath sounds for adequate ventilation • Assess pulse oximetry for adequate oxygenation • Assess patient comfort and anxiety – Consider Ativan • Document – IPAP, EPAP, or CPAP levels – Patient response to treatment • Consider intubation
BIBLIOGRAPHY • http: //www. differencebetween. net/object/dif ference-between-cpap-and-bipap/ • http: //emedicine. medscape. com/article/3042 35 -overview • http: //www. nhlbi. nih. gov/healthtopics/cpap/