IN THE NAME GOD Noninvasive Ventilation Noninvasive ventilation



- Slides: 53
IN THE NAME GOD
Noninvasive Ventilation
Noninvasive ventilation (NIV) refers to the administration of ventilatory support without using an invasive artificial airway (endotracheal tube or tracheostomy tube) and noninvasive ventilation has now become an integral tool in the management of both acute and chronic respiratory failure, in both the home setting and in the critical care unit.
Methods of Delivery Noninvasive positive-pressure ventilation Noninvasive negative-pressure ventilation High-flow nasal oxygen
Noninvasive positive-pressure ventilation
Ventilatory support can be achieved through a variety of interfaces (mouth piece or nasal, face, or helmet mask), using a variety of ventilatory modes (eg, volume ventilation, pressure support, bilevel positive airway pressure [Bi. PAP], continuous positive airway pressure [CPAP]) with either ventilators dedicated to noninvasive ventilation (NIV) or those capable of providing support through an endotracheal tube or mask. Older models of noninvasive ventilators required oxygen to be bled into the system, but current models incorporate oxygen blenders for precise delivery of the fraction of inspired oxygen (FIO 2).

Noninvasive negative-pressure ventilation
Negative-pressure ventilators provide ventilatory support using a device that encases the thoracic cage starting from the neck, and devices range from a whole-body tank to a cuirass shell. The general principal is the same with a vacuum device, which lowers the pressure surrounding the thorax, creating subatmospheric pressure and thereby passively expanding the chest wall with diaphragmatic descent, all leading to lung inflation. Exhalation occurs with passive recoil of the chest wall.
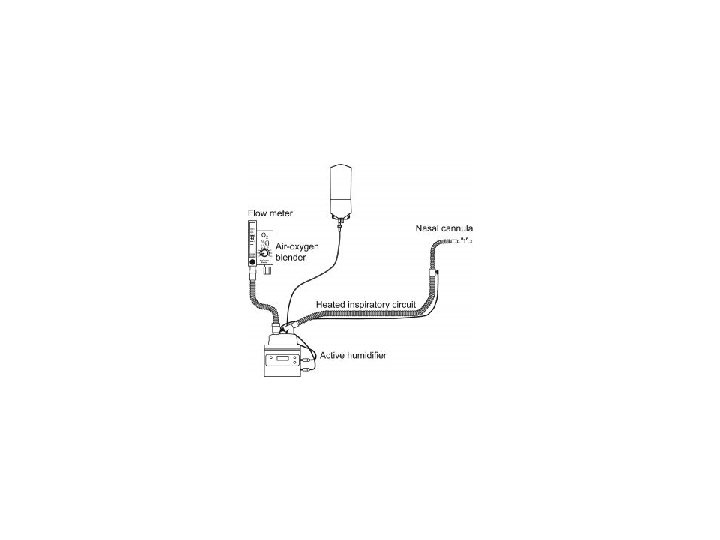
High-flow nasal oxygen
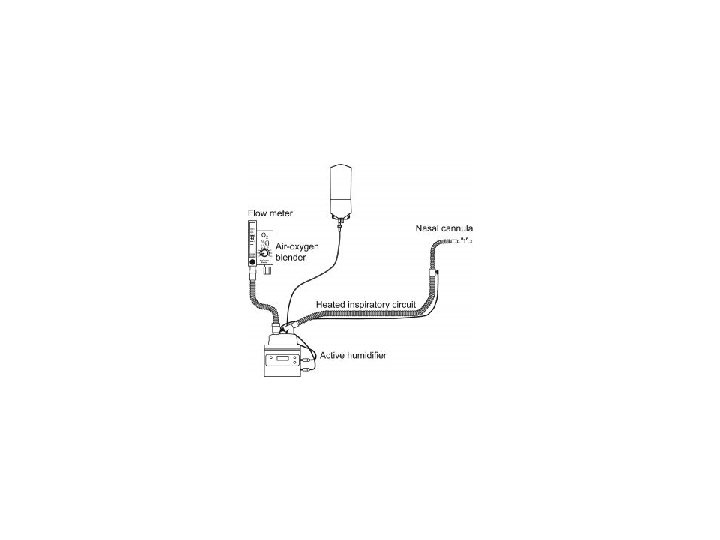
Conventional oxygen therapy is not well tolerated at high flow rates because of problems with unheated and nonhumidified oxygen. The high-flow nasal cannula oxygen systems are able to heat and humidify, improving patient tolerance and comfort. increasing the FIO 2 that can be provided to patients; are able to wash out dead space carbon dioxide, improving the efficiency of oxygen delivery; and the increased flow rate translates into positive end-expiratory pressure (PEEP).
An intact respiratory drive is required with this modality, which means that it is not suited for patients with hypoventilation or a blunted respiratory drive.

Absolute contraindications of noninvasive positivepressure ventilation are as follows: COMA CARDIAC ARREST RESPIRATORY ARREST ANY CONDITION REQUIRING IMMEDIATE INTUBATION
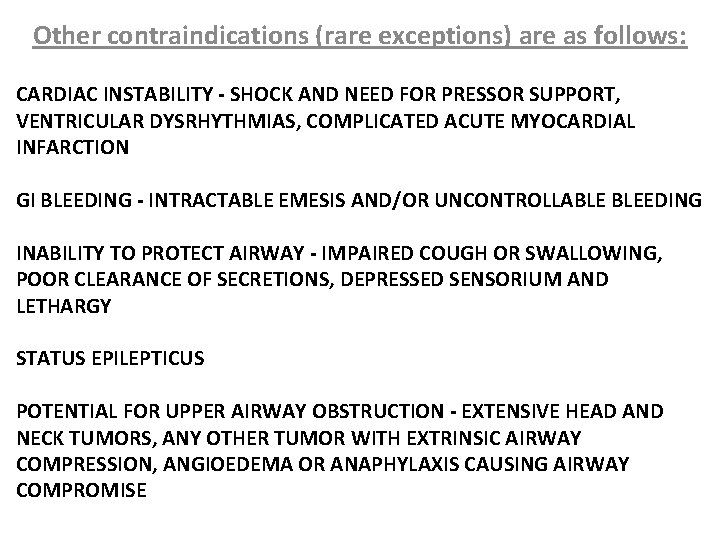
Other contraindications (rare exceptions) are as follows: CARDIAC INSTABILITY - SHOCK AND NEED FOR PRESSOR SUPPORT, VENTRICULAR DYSRHYTHMIAS, COMPLICATED ACUTE MYOCARDIAL INFARCTION GI BLEEDING - INTRACTABLE EMESIS AND/OR UNCONTROLLABLE BLEEDING INABILITY TO PROTECT AIRWAY - IMPAIRED COUGH OR SWALLOWING, POOR CLEARANCE OF SECRETIONS, DEPRESSED SENSORIUM AND LETHARGY STATUS EPILEPTICUS POTENTIAL FOR UPPER AIRWAY OBSTRUCTION - EXTENSIVE HEAD AND NECK TUMORS, ANY OTHER TUMOR WITH EXTRINSIC AIRWAY COMPRESSION, ANGIOEDEMA OR ANAPHYLAXIS CAUSING AIRWAY COMPROMISE
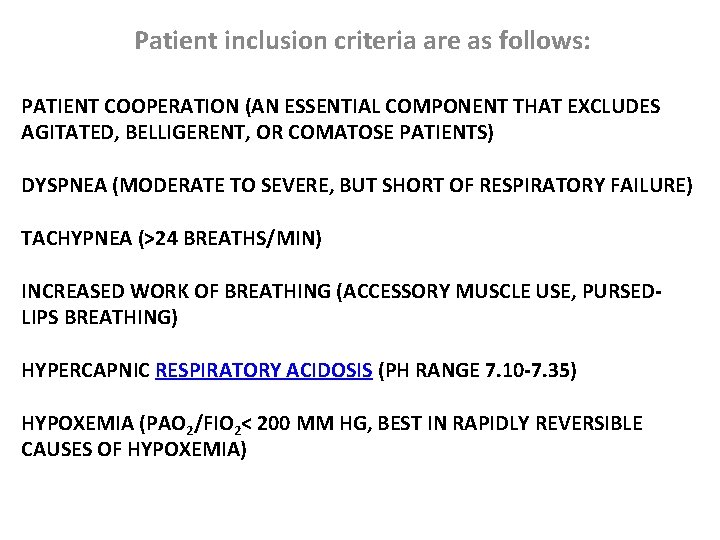
Patient inclusion criteria are as follows: PATIENT COOPERATION (AN ESSENTIAL COMPONENT THAT EXCLUDES AGITATED, BELLIGERENT, OR COMATOSE PATIENTS) DYSPNEA (MODERATE TO SEVERE, BUT SHORT OF RESPIRATORY FAILURE) TACHYPNEA (>24 BREATHS/MIN) INCREASED WORK OF BREATHING (ACCESSORY MUSCLE USE, PURSEDLIPS BREATHING) HYPERCAPNIC RESPIRATORY ACIDOSIS (PH RANGE 7. 10 -7. 35) HYPOXEMIA (PAO 2/FIO 2< 200 MM HG, BEST IN RAPIDLY REVERSIBLE CAUSES OF HYPOXEMIA)
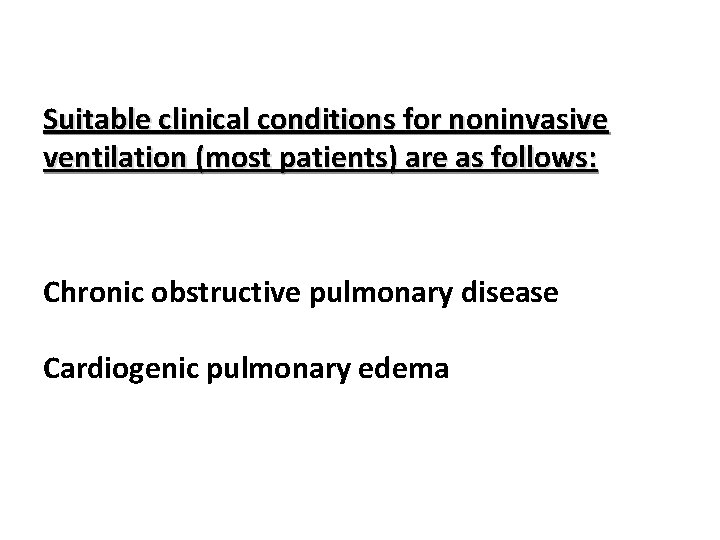
Suitable clinical conditions for noninvasive ventilation (most patients) are as follows: Chronic obstructive pulmonary disease Cardiogenic pulmonary edema
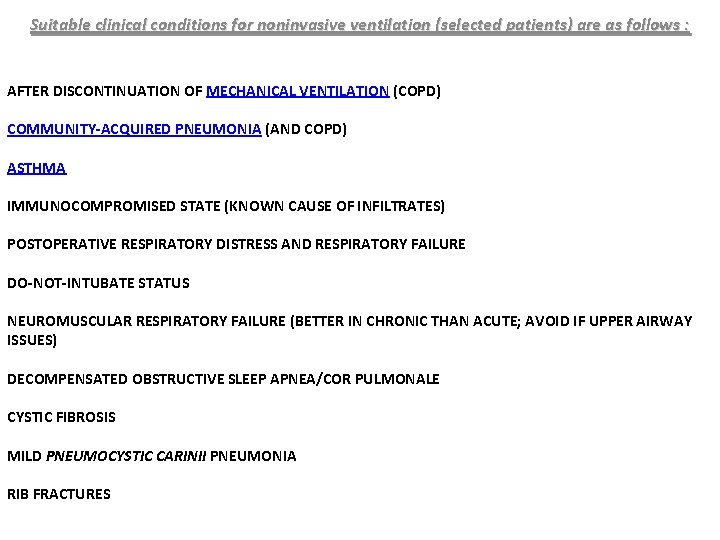
Suitable clinical conditions for noninvasive ventilation (selected patients) are as follows : AFTER DISCONTINUATION OF MECHANICAL VENTILATION (COPD) COMMUNITY-ACQUIRED PNEUMONIA (AND COPD) ASTHMA IMMUNOCOMPROMISED STATE (KNOWN CAUSE OF INFILTRATES) POSTOPERATIVE RESPIRATORY DISTRESS AND RESPIRATORY FAILURE DO-NOT-INTUBATE STATUS NEUROMUSCULAR RESPIRATORY FAILURE (BETTER IN CHRONIC THAN ACUTE; AVOID IF UPPER AIRWAY ISSUES) DECOMPENSATED OBSTRUCTIVE SLEEP APNEA/COR PULMONALE CYSTIC FIBROSIS MILD PNEUMOCYSTIC CARINII PNEUMONIA RIB FRACTURES
Use with caution in the following clinical conditions: IDIOPATHIC PULMONARY FIBROSIS (EXACERBATION) ACUTE RESPIRATORY DISTRESS SYNDROME
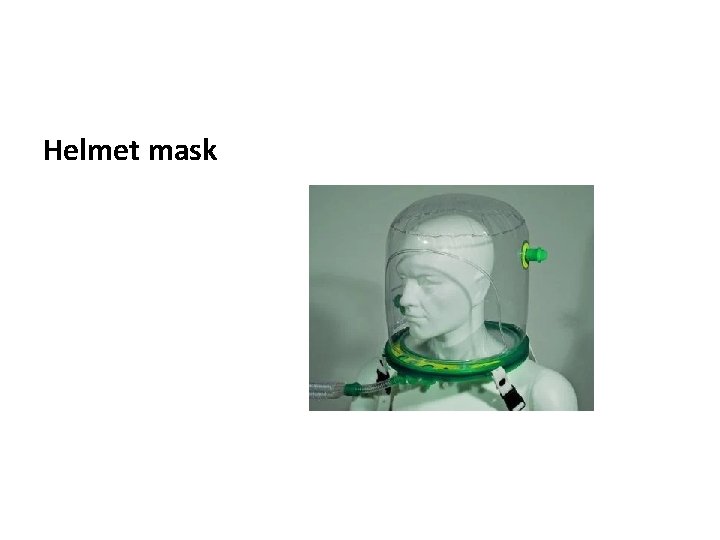
Patient interfaces Nasal masks and orofacial masks were the earliest interfaces, with subsequent development and use of full face masks, mouthpieces, nasal pillows, and helmets. Nasal masks and orofacial masks are still the most commonly used interfaces.
Nasal mask
Full face mask
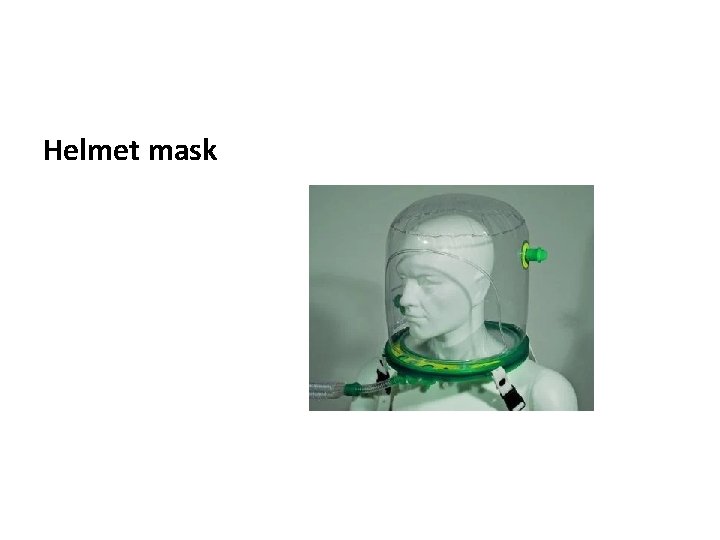
Helmet mask
Modes of ventilation continuous positive airway pressure (CPAP) Bilevel positive airway pressure (Bi. PAP)
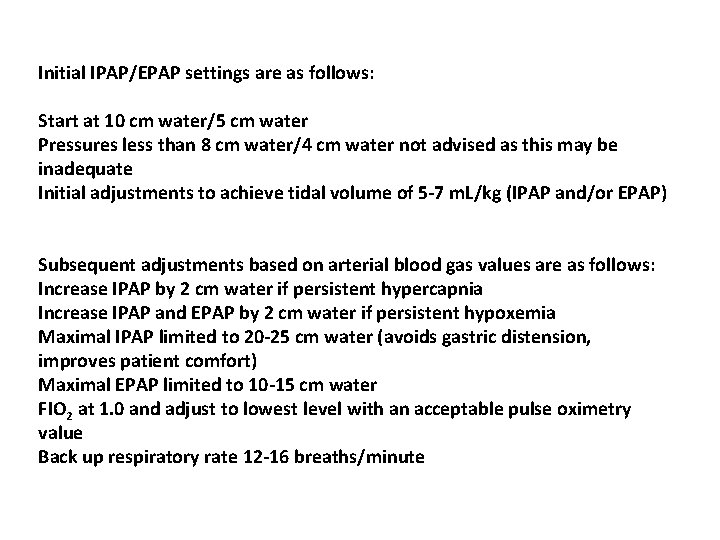
Initial IPAP/EPAP settings are as follows: Start at 10 cm water/5 cm water Pressures less than 8 cm water/4 cm water not advised as this may be inadequate Initial adjustments to achieve tidal volume of 5 -7 m. L/kg (IPAP and/or EPAP) Subsequent adjustments based on arterial blood gas values are as follows: Increase IPAP by 2 cm water if persistent hypercapnia Increase IPAP and EPAP by 2 cm water if persistent hypoxemia Maximal IPAP limited to 20 -25 cm water (avoids gastric distension, improves patient comfort) Maximal EPAP limited to 10 -15 cm water FIO 2 at 1. 0 and adjust to lowest level with an acceptable pulse oximetry value Back up respiratory rate 12 -16 breaths/minute
Predictors of success, with a response to a trial of NIV (1 -2 h), are as follows: Decrease in Pa. CO 2 greater than 8 mm Hg Improvement in p. H greater than 0. 06 Correction of respiratory acidosis
Predictors of failure as follows: SEVERITY OF ILLNESS - ACIDOSIS (PH < 7. 25), HYPERCAPNIA (>80 AND PH < 7. 25), ACUTE PHYSIOLOGY AND CHRONIC HEALTH EVALUATION II (APACHE II) SCORE HIGHER THAN 20 LEVEL OF CONSCIOUSNESS - NEUROLOGIC SCORE (>4 = STUPOROUS, AROUSAL ONLY AFTER VIGOROUS STIMULATION; INCONSISTENTLY FOLLOWS COMMANDS), ENCEPHALOPATHY SCORE (>3 = MAJOR CONFUSION, DAYTIME SLEEPINESS OR AGITATION), GLASGOW COMA SCALE SCORE LOWER THAN 8 FAILURE OF IMPROVEMENT WITH 12 -24 HOURS OF NONINVASIVE VENTILATION
Late admission predictors of failure (>48 h after initiation of noninvasive ventilation) are as follows: LOWER FUNCTIONAL STATUS (ACTIVITY SCORE < 2 = DYSPNEA LIGHT ACTIVITY) INITIAL ACIDOSIS (PH ≤ 7. 22) HOSPITAL COMPLICATIONS (PNEUMONIA, SHOCK, COMA)
Noninvasive Ventilation in COPD Exacerbations increase the work of breathing in these patients and may exceed the patient's ability to adequately ventilate through a variety of mechanisms, including increasing hyperinflation with decreased diaphragmatic excursion and strength, increasing intrinsic positive end-expiratory pressure (PEEP), ineffective or inadequate tidal volume generation, respiratory patterns, and increased respiratory frequency. Noninvasive ventilation effectively unloads the respiratory muscles, increasing tidal volume, decreasing the respiratory rate, and decreasing the diaphragmatic work of breathing, which translates to an improvement in oxygenation, a reduction in hypercapnia, and an improvement in dyspnea.
Noninvasive ventilation reduces the need for intubation, mortality, complications, and length of stay in patients with COPD.
Patients who are not cooperative and have a p. H that approaches 7. 20 must be evaluated with caution because they have a higher risk of failure with noninvasive ventilation and would therefore benefit from earlier intubation (if an option), especially if they do not respond to a short trial of noninvasive ventilation.
Noninvasive ventilation is most effective in patients with moderate-to-severe disease Hypercapnic respiratory acidosis may define the best responders (p. H 7. 20 -7. 30). Noninvasive ventilation is also effective in patients with a p. H of 7. 30 -7. 35, but no added benefit is appreciated if the p. H is greater than 7. 35. Improvement after a 1 - to 2 -hour trial may predict success.
Noninvasive Ventilation in Cardiogenic Pulmonary Edema
Noninvasive ventilation is well suited for patients with cardiogenic pulmonary edema. CPAP and Bi. PAP modalities both are effective, with CPAP possibly being more effective. The greatest benefits are realized in relief of symptoms and dyspnea. A decrease in intubation and mortality rates is not a universal experience. Patients with hypercapnic respiratory acidosis may derive the greatest benefit from noninvasive ventilation. Importantly, adjust to standard therapy, including diuresis. Benefit may be seen with as few as 2 hours of support.
Noninvasive Ventilation in COVID-19
It is suggested to start supplemental oxygen if the peripheral oxygen saturation (SPO 2) is less than 92%. It is recommended to start supplemental oxygen if the SPO 2 is less than 90%. In the event of acute hypoxemic respiratory failure on oxygen, it is recommended that the SPO 2 be maintained at no higher than 96%. In patients with acute hypoxemic respiratory failure despite conventional oxygen therapy, it is suggested that a high-flow nasal cannula be used rather than conventional oxygen therapy.
In patients with acute hypoxemic respiratory failure, it is also suggested that a high-flow nasal cannula be used over noninvasive positive-pressure ventilation. In these patients with acute hypoxemic respiratory failure, in the event a high-flow nasal cannula is not available and the patient has no urgent indication for endotracheal intubation, it is suggested that a trial of noninvasive positive -pressure ventilation be conducted, with close monitoring and short-interval assessment for worsening of respiratory failure. While considered an option, no recommendation was made regarding helmet noninvasive positive-pressure ventilation versus mask noninvasive positive-pressure ventilation.
In patients receiving either noninvasive positive-pressure ventilation or high-flow nasal cannula, it is recommended they be closely monitored for worsening respiratory status; early intubation in a controlled setting is recommended if worsening occurs. In patients with acute respiratory distress syndrome (ARDS) who are on mechanical ventilation, it is recommended to use low-tidal-volume ventilation (4 -8 m. L/kg of predicted body weight) versus higher tidal volumes (>8 m. L/kg). In patients with ARDS who are on mechanical ventilation, it is recommended to target plateau pressures at less than 30 cm water.
In patients with moderate-to-severe ARDS who are on mechanical ventilation, it is suggested to use a higher positive end-expiratory pressure (PEEP) strategy versus a lower PEEP strategy. When using a higher PEEP strategy (ie, PEEP >10 cm water), monitor patients for barotrauma. In patients with ARDS who are on mechanical ventilation, it is suggested to use a conservative fluid strategy versus a liberal fluid strategy. In patients with moderate-to-severe ARDS who are on mechanical ventilation, it is suggested to use prone ventilation for 12 -16 hours versus no prone ventilation.
In patients with moderate-to-severe ARDS who are on mechanical ventilation, it is suggested to use, as needed, intermittent boluses of neuromuscular blocking agents versus a continuous infusion, to facilitate protective lung ventilation. Use of a continuous infusion of neuromuscular blocking agents is suggested in the event of persistent ventilator dyssynchrony, a need for ongoing deep sedation, prone ventilation, or persistently high plateau pressures. In patients with ARDS who are on mechanical ventilation, routine use of inhaled nitric oxide is not recommended.
In mechanically ventilated patients with severe ARDS and hypoxemia despite optimization of ventilation and other rescue strategies, a trial of inhaled pulmonary vasodilator is suggested as rescue therapy; if rapid improvement in oxygenation is not observed, taper off treatment. In mechanically ventilated patients with severe ARDS and hypoxemia despite optimization of ventilation, use of recruitment maneuvers is suggested over not using recruitment maneuvers. If recruitment maneuvers are used, staircase (incremental PEEP) recruitment maneuvers are not recommended.
In those patients on mechanical ventilation who have refractory hypoxemia despite optimization of ventilation and who have undergone rescue therapies and proning, it is suggested to use venous extracorporeal membrane oxygenation (EMCO) if available; alternatively, refer the patient to center that has ECMO. However, because EMCO is resource-intensive and it requires experienced centers/healthcare workers and infrastructure, it should only be considered in carefully selected patients with severe ARDS.
Complications of Noninvasive Ventilation
For facial and nasal pressure injury and sores, note the following: Result of tight mask seals used to attain adequate inspiratory volumes Minimize pressure by intermittent application of noninvasive ventilation Schedule breaks (30 -90 min) to minimize effects of mask pressure Balance strap tension to minimize mask leaks without excessive mask pressures Cover vulnerable areas (erythematous points of contact) with protective dressings
For gastric distension, note the following: Rarely a problem Avoid by limiting peak inspiratory pressures to less than 25 cm water Nasogastric tubes can be placed but can worsen leaks from the mask Nasogastric tube also bypasses the lower esophageal sphincter and permits reflux

For dry mucous membranes and thick secretions, note the following: Seen in patients with extended use of noninvasive ventilation Provide humidification for noninvasive ventilation devices Provide daily oral care
For aspiration of gastric contents, note the following: Especially if emesis during noninvasive ventilation Avoid noninvasive ventilation in patient with ongoing emesis or hematemesis
Complications of both noninvasive and invasive ventilation These include the following: Barotrauma (significantly less risk with noninvasive ventilation) Hypotension related to positive intrathoracic pressure (support with fluids)
Complications avoided by noninvasive ventilation These include the following: Ventilator-associated pneumonia Sinusitis Reduction in need for sedative agents - Sedatives used in less than 15% of noninvasive ventilation patients in one survey
Noninvasive Ventilation in Other Conditions
In asthma patients, note the following: Similar pathophysiology to COPD; limited reported experience with noninvasive ventilation Mostly case series with reported benefit Prospective, randomized studies based on emergency department settings Improvement in spirometry main outcome measure Fewer admissions with noninvasive ventilation; intubation not an outcome measure Hypercapnic asthma patients not represented in randomized trials Noninvasive ventilation probably beneficial, but experience limited
For acute respiratory distress syndrome, note the following: Not recommended as first-line therapy in management Limited experience, but may benefit those who do not require immediate intubation Noninvasive ventilation provided via mask or helmet; able to avoid intubation in approximately half - Ventilator settings in successful noninvasive ventilation are pressure support ventilation of 14 cm water; positive end-expiratory (PEEP) of 7 cm water; successfully treated patients found to have lower severity of illness (Simplified Acute Physiology Score II < 34 or improvement of Pa. O 2/Fi. O 2 ratio >175 after 1 h) High-flow nasal cannula oxygen in a trial compared with high-flow nasal cannula plus noninvasive face mask ventilation with better mortality outcomes than noninvasive ventilation, although no statistical difference in primary outcome of intubation [68] Single-center trial of selected patients with acute respiratory distress syndrome who did not improve with noninvasive ventilation demonstrated benefit with helmet ventilation with decreased intubation rate, more ventilator-free days, and decreased mortality [69] ; higher PEEP delivered and high flow rates (100 -200 L/min) may explain benefit of helmet noninvasive ventilation
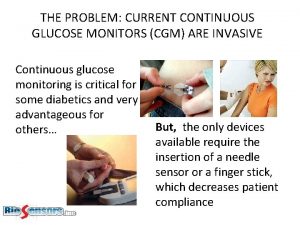
 Noninvasive glucose meter
Noninvasive glucose meter Modes of mechanical ventilation
Modes of mechanical ventilation Name three line segments
Name three line segments God ventilation
God ventilation Hình ảnh bộ gõ cơ thể búng tay
Hình ảnh bộ gõ cơ thể búng tay Ng-html
Ng-html Bổ thể
Bổ thể Tỉ lệ cơ thể trẻ em
Tỉ lệ cơ thể trẻ em Chó sói
Chó sói Tư thế worm breton là gì
Tư thế worm breton là gì Bài hát chúa yêu trần thế alleluia
Bài hát chúa yêu trần thế alleluia Các môn thể thao bắt đầu bằng tiếng nhảy
Các môn thể thao bắt đầu bằng tiếng nhảy Thế nào là hệ số cao nhất
Thế nào là hệ số cao nhất Các châu lục và đại dương trên thế giới
Các châu lục và đại dương trên thế giới Cong thức tính động năng
Cong thức tính động năng Trời xanh đây là của chúng ta thể thơ
Trời xanh đây là của chúng ta thể thơ Mật thư tọa độ 5x5
Mật thư tọa độ 5x5 101012 bằng
101012 bằng độ dài liên kết
độ dài liên kết Các châu lục và đại dương trên thế giới
Các châu lục và đại dương trên thế giới Thể thơ truyền thống
Thể thơ truyền thống Quá trình desamine hóa có thể tạo ra
Quá trình desamine hóa có thể tạo ra Một số thể thơ truyền thống
Một số thể thơ truyền thống Cái miệng nó xinh thế
Cái miệng nó xinh thế Vẽ hình chiếu vuông góc của vật thể sau
Vẽ hình chiếu vuông góc của vật thể sau Biện pháp chống mỏi cơ
Biện pháp chống mỏi cơ đặc điểm cơ thể của người tối cổ
đặc điểm cơ thể của người tối cổ V cc
V cc Vẽ hình chiếu đứng bằng cạnh của vật thể
Vẽ hình chiếu đứng bằng cạnh của vật thể Vẽ hình chiếu vuông góc của vật thể sau
Vẽ hình chiếu vuông góc của vật thể sau Thẻ vin
Thẻ vin đại từ thay thế
đại từ thay thế điện thế nghỉ
điện thế nghỉ Tư thế ngồi viết
Tư thế ngồi viết Diễn thế sinh thái là
Diễn thế sinh thái là Các loại đột biến cấu trúc nhiễm sắc thể
Các loại đột biến cấu trúc nhiễm sắc thể Số nguyên là gì
Số nguyên là gì Tư thế ngồi viết
Tư thế ngồi viết Lời thề hippocrates
Lời thề hippocrates Thiếu nhi thế giới liên hoan
Thiếu nhi thế giới liên hoan ưu thế lai là gì
ưu thế lai là gì Hươu thường đẻ mỗi lứa mấy con
Hươu thường đẻ mỗi lứa mấy con Khi nào hổ con có thể sống độc lập
Khi nào hổ con có thể sống độc lập Sơ đồ cơ thể người
Sơ đồ cơ thể người Từ ngữ thể hiện lòng nhân hậu
Từ ngữ thể hiện lòng nhân hậu Thế nào là mạng điện lắp đặt kiểu nổi
Thế nào là mạng điện lắp đặt kiểu nổi Our god is an awesome god vine
Our god is an awesome god vine My god is an awesome god he reigns
My god is an awesome god he reigns Our god is an awesome god medley
Our god is an awesome god medley God is good god is great speed
God is good god is great speed O god you are my god earnestly i seek you
O god you are my god earnestly i seek you God-given virtues that direct us to our loving, triune god.
God-given virtues that direct us to our loving, triune god. Justice and virtue
Justice and virtue My god's bigger than your god
My god's bigger than your god