NNAP 2018 results presentation template This slide deck
![[NAME OF NEONATAL UNIT] National Neonatal Audit Programme (NNAP) 2018 results [NAME OF NEONATAL UNIT] National Neonatal Audit Programme (NNAP) 2018 results](https://slidetodoc.com/presentation_image_h/0dc9f9162acf0617a86e7ed3e39f1463/image-3.jpg)
- Slides: 43
NNAP 2018 results presentation template • This slide deck has been designed to be amended by neonatal teams to: • communicate the main national and unit level findings from the audit • facilitate interpretation of results • develop awareness of the functionality of NNAP Online • use the data to stimulate quality improvement activity • All unit level graphs displayed are placeholders, and there are instructions for the generation of bespoke graphs for your unit on the slides displaying these place holders. • For the first measure, Antenatal Steroids, the slide is repeated to show you an example, using Bradford Royal Infirmary’s results for 2017 data. • You may choose to use a selection of the slides and focussing your quality improvement activity; however we recommend that you make the team aware of all measure areas included in the audit. • To compare your validated 2018 results against your provisional 2019 results, use your NNAP quarterly reports.
NNAP 2018 results presentation template: Resources to support your presentation • NNAP Online • National Neonatal Audit Programme 2019 report on 2018 data • Unit poster generator • NNAP parent and carer report, Your baby’s care • Recommendations tracking checklist • How to insert a screenshot or screen clipping into a presentation
![NAME OF NEONATAL UNIT National Neonatal Audit Programme NNAP 2018 results [NAME OF NEONATAL UNIT] National Neonatal Audit Programme (NNAP) 2018 results](https://slidetodoc.com/presentation_image_h/0dc9f9162acf0617a86e7ed3e39f1463/image-3.jpg)
[NAME OF NEONATAL UNIT] National Neonatal Audit Programme (NNAP) 2018 results
Background • The NNAP is a national clinical audit of NHS-funded care, establish in 2006, for babies admitted to neonatal services in England, Scotland, Wales and the Isle of Man. It is managed by the Royal College of Paediatrics and Child Health (RCPCH), commissioned by the Healthcare Quality Improvement Partnership (HQIP) and funded by NHS England, the Welsh and Scottish Governments. • This report relates to the care provided to 104, 577 babies discharged from neonatal care during the calendar year 1 January 2018 to 31 December 2018 in the 181 participating neonatal units. The audit’s aims are to: • assess whether babies admitted to neonatal units receive consistent high-quality care in relation to the NNAP audit measures that are aligned to a set of professionally agreed guidelines and standards • identify areas for quality improvement in neonatal units in relation to the delivery and outcomes of care.
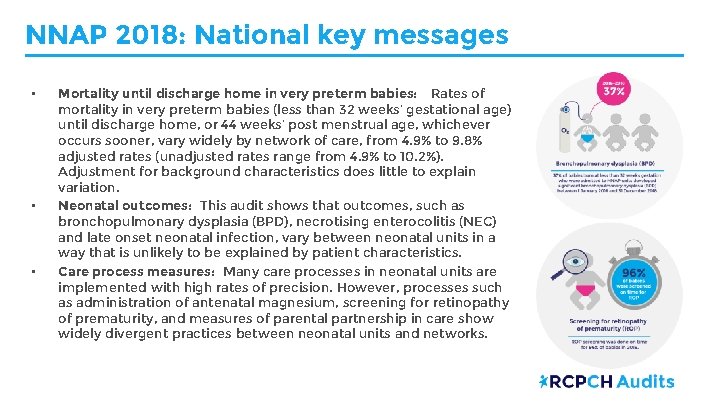
NNAP 2018: National key messages • • • Mortality until discharge home in very preterm babies: Rates of mortality in very preterm babies (less than 32 weeks’ gestational age) until discharge home, or 44 weeks’ post menstrual age, whichever occurs sooner, vary widely by network of care, from 4. 9% to 9. 8% adjusted rates (unadjusted rates range from 4. 9% to 10. 2%). Adjustment for background characteristics does little to explain variation. Neonatal outcomes: This audit shows that outcomes, such as bronchopulmonary dysplasia (BPD), necrotising enterocolitis (NEC) and late onset neonatal infection, vary between neonatal units in a way that is unlikely to be explained by patient characteristics. Care process measures: Many care processes in neonatal units are implemented with high rates of precision. However, processes such as administration of antenatal magnesium, screening for retinopathy of prematurity, and measures of parental partnership in care show widely divergent practices between neonatal units and networks.
NNAP 2018: National key messages • Birth in a centre with a NICU: There is evidence that outcomes for very preterm babies are better when they are cared for in a NICU from birth. 74. 3% of babies born at less than 27 weeks’ gestational age were delivered in a hospital with a NICU on site; no notable change since 2017 when the rate was 73. 9%. 3 of the 15 networks are achieving the standard of 85% which may reflect network structure as much as clinical practice. • Neonatal nurse staffing levels: Nurse staffing levels on neonatal units are below national recommendations. Overall, 64% of shifts (80, 642 of 126, 240) are numerically staffed according to national guidelines. 44% (37, 985 of 86, 139) of shifts have sufficient staff qualified in specialty. Only 21 of 53 NICUs had half or more of their shifts with sufficient staff qualified in specialty.
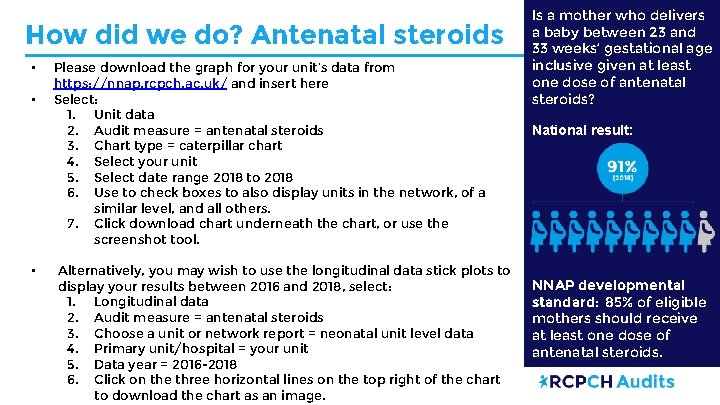
How did we do? Antenatal steroids • • • Please download the graph for your unit’s data from https: //nnap. rcpch. ac. uk/ and insert here Select: 1. Unit data 2. Audit measure = antenatal steroids 3. Chart type = caterpillar chart 4. Select your unit 5. Select date range 2018 to 2018 6. Use to check boxes to also display units in the network, of a similar level, and all others. 7. Click download chart underneath the chart, or use the screenshot tool. Alternatively, you may wish to use the longitudinal data stick plots to display your results between 2016 and 2018, select: 1. Longitudinal data 2. Audit measure = antenatal steroids 3. Choose a unit or network report = neonatal unit level data 4. Primary unit/hospital = your unit 5. Data year = 2016 -2018 6. Click on the three horizontal lines on the top right of the chart to download the chart as an image. Is a mother who delivers a baby between 23 and 33 weeks’ gestational age inclusive given at least one dose of antenatal steroids? National result: NNAP developmental standard: 85% of eligible mothers should receive at least one dose of antenatal steroids.
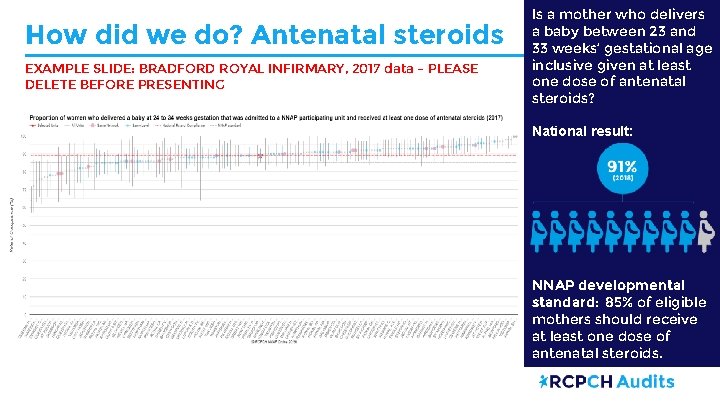
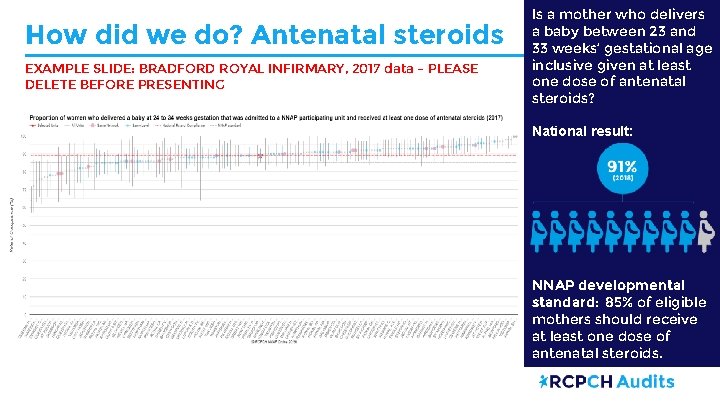
How did we do? Antenatal steroids EXAMPLE SLIDE: BRADFORD ROYAL INFIRMARY, 2017 data – PLEASE DELETE BEFORE PRESENTING Is a mother who delivers a baby between 23 and 33 weeks’ gestational age inclusive given at least one dose of antenatal steroids? National result: NNAP developmental standard: 85% of eligible mothers should receive at least one dose of antenatal steroids.
How did we do? Magnesium sulphate • • • Please download the graph for your unit’s data from https: //nnap. rcpch. ac. uk/ and insert here Select: 1. Unit data 2. Audit measure = magnesium sulphate 3. Chart type = caterpillar chart 4. Select your unit 5. Select date range 2018 to 2018 6. Use to check boxes to also display units in the network, of a similar level, and all others. 7. Click download chart underneath the chart, or use the screenshot tool. Alternatively, you may wish to use the longitudinal data stick plots to display your results between 2016 and 2018, select: 1. Longitudinal data 2. Audit measure = magnesium sulphate 3. Choose a unit or network report = neonatal unit level data 4. Primary unit/hospital = your unit 5. Data year = 2016 -2018 6. Click on the three horizontal lines on the top right of the chart to download the chart as an image. Is a mother who delivers a baby below 30 weeks gestational age given magnesium sulphate in the 24 hours prior to delivery? National result: NNAP developmental standard: 85% of eligible mothers should receive antenatal magnesium sulphate.
How did we do? Birth in a centre with a NICU • • Please download the graph for your network’s result from https: //nnap. rcpch. ac. uk/ and insert here Select: 1. Network data 2. Audit measure = Birth in a centre with a NICU 3. Chart type = caterpillar plot 4. Select your network 5. Select date range 2018 to 2018 6. Click download chart underneath the chart, or use the snipping tool. Is an admitted baby born at less than 27 weeks gestational age delivered in a maternity service on the same site as a designated NICU? National result: NNAP developmental standard: 85% of babies born at less than 27 weeks GA should be delivered in a maternity service on the same site as a NICU.
What next? Birth in a centre with a NICU, Antenatal steroids and magnesium sulphate Recommendation: To optimise preterm perinatal wellbeing, base local quality improvement activity on reviews of cases: • where evidence-based strategies were not used in patient care • where shared learning from networks is available. Use the following methodologies to guide improvement: • The Prevention of Cerebral Palsy in Pre. Term Labour (PRe. Ce. PT) programme, • The Maternity and Neonatal Health Safety Collaborative and • The Scottish Patient Safety Programme. Action: Perinatal teams, neonatal networks and maternity systems
What next? Birth in a centre with a NICU, Antenatal steroids and magnesium sulphate Further information and resources: • The PRe. Ce. PT programme • Maternity and Children Quality Improvement Collaborative (MCQIC), Scottish Patient Safety Programme quality improvement resources • Maternal and neonatal health safety collaborative, NHS Improvement quality and safety resources • Case study: Improving the rate of babies born at less than 27 weeks gestation in a maternity unit with a NICU on site. East of England ODN.
How did we do? Temperature on admission • • • Please download the graph for your unit’s result from https: //nnap. rcpch. ac. uk/ and insert here Select: 1. Unit data 2. Audit measure = Temperature 3. Chart type = caterpillar plot 4. Select your unit 5. Select date range 2018 to 2018 6. Use to check boxes to also display units in the network, of a similar level, and all others. 7. Click download chart underneath the chart, or use the screenshot tool. Alternatively, you may wish to use the longitudinal data stick plots to display your results between 2016 and 2018, select: 1. Longitudinal data 2. Audit measure = Temperature on admission 3. Choose a unit or network report = neonatal unit level data 4. Primary unit/hospital = your unit 5. Data year = 2016 -2018 6. Click on the three horizontal lines on the top right of the chart to download the chart as an image. Does an admitted baby born at less than 32 weeks gestational age have a first temperature on admission which is both between 36. 5– 37. 5°C and measured within one hour of birth? National result: NNAP developmental standard: At least 90% of babies should have a temperature taken within an hour of birth and measuring within the normal range.
What next? Temperature on admission Recommendation: Review local thermoregulation data to drive quality improvement goals. Use the British Association of Perinatal Medicine Quality Improvement toolkit for Improving Normothermia in Very Preterm Infants to support action in response. Action: Neonatal units Further information and resources: • BAPM Quality Improvement Toolkit for Improving Normothermia in Very Preterm Infants • Maternity and Children Quality Improvement Collaborative (MCQIC), Scottish Patient Safety Programme quality improvement resources • Maternal and neonatal health safety collaborative, NHS Improvement quality and safety resources
How did we do? Consultation with parents • • • Please download the graph for your unit’s result from https: //nnap. rcpch. ac. uk/ and insert here Select: 1. Unit data 2. Audit measure = Consultation with parents 3. Chart type = caterpillar plot 4. Select your unit 5. Select date range 2018 to 2018 6. Use the check boxes to also display units in the network, of a similar level, and all others. 7. Click download chart underneath the chart, or use the screenshot tool. Alternatively, you may wish to use the longitudinal data stick plots to display your results between 2016 and 2018, select: 1. Longitudinal data 2. Audit measure = Consultation with parents 3. Choose a unit or network report = neonatal unit level data 4. Primary unit/hospital = your unit 5. Data year = 2016 -2018 6. Click on the three horizontal lines on the top right of the chart to download the chart as an image. Is there a documented consultation with parents by a senior member of the neonatal team within 24 hours of a baby’s first admission? National result: NNAP developmental standard: A consultation should take place with 24 hours of first admission for every baby.
What next? Consultation with parents Recommendation: Review practice and documentation processes where rates of parental consultation and parental presence on the ward round need to be increased. Use the Bliss Baby Charter for guidance on improving parental partnership in care. Action: Neonatal units Further information and resources: • The Bliss Baby Charter is a practical framework that neonatal units can use to ensure families are at the centre of their baby’s care.
How did we do? Parents on ward rounds • • Please download the graph for your unit’s result from https: //nnap. rcpch. ac. uk/ and insert here. Select: 1. Unit data 2. Audit measure = parents on ward rounds 3. Chart type = bar chart 4. Select your unit 5. Select date range 2018 to 2018 6. Use the check boxes to also display units in the network, of a similar level, and all others. 7. Click download chart underneath the chart, or use the screenshot tool. For a baby admitted for more than 24 hours, did at least one parent attend a consultant ward round at any point during the baby’s admission? National result:
What next? Parents on ward rounds Recommendations: • Further information and resources: • The Bliss Baby Charter is a practical framework that neonatal units can use to ensure families are at the centre of their baby’s care. • Case study: Integrated Family Delivered Neonatal Care: From Quality Improvement Project to Standard of Care. Review practice and documentation processes where rates of parental consultation and parental presence on the ward round need to be increased. Use the Bliss Baby Charter for guidance on improving parental partnership in care. Action: Neonatal units • Ensure that staff: o o understand the importance of welcoming parents to the neonatal unit communicate to parents the value of their presence on the ward round involve them directly in the ward round record their presence. Action: Neonatal units Imperial College Healthcare NHS Trust.
How did we do? On time ROP screening • • • Please download the graph for your unit’s result from https: //nnap. rcpch. ac. uk/ and insert here Select: 1. Unit data 2. Audit measure = ROP screening 3. Chart type = caterpillar plot 4. Select your unit 5. Select date range 2018 to 2018 6. Use the check boxes to also display units in the network, of a similar level, and all others. 7. Click download chart underneath the chart, or use the screenshot tool. Alternatively, you may wish to use the longitudinal data stick plots to display your results between 2016 and 2018, select: 1. Longitudinal data 2. Audit measure = ROP screening 3. Choose a unit or network report = neonatal unit level data 4. Primary unit/hospital = your unit 5. Data year = 2016 -2018 6. Click on the three horizontal lines on the top right of the chart to download the chart as an image. Does an admitted baby born weighing less than 1501 g, or at gestational age of less than 32 weeks, undergo the first retinopathy of prematurity (ROP) screening in accordance with the NNAP interpretation of the current guideline recommendations? National result: NNAP developmental standard: All eligible babies should be screened ‘on time’.
How did we do? Encephalopathy • Encephalopathy rates are reported by trust or health board on year in arrears, due to the availability of live birth denominator data. • To look up your trust/health board’s encephalopathy rate: 1. Go to https: //nnap. rcpch. ac. uk/ 2. Select Encephalopathy from the menu 3. Choose data year = 2017 4. Primary trust = your trust/health board 5. Export the table using one of the export options at the bottom left of the table. What next? Further information and resources: • • Each Baby Counts , run by the Royal College of Obstetricians and Gynaecology (RCOG) , is a national quality improvement programme to reduce the number of babies who die or have a serious brain injury because of incidents that occur during term labour. The Avoiding Term Admissions to Neonatal Units (ATAIN) programme , run by NHS Improvement , focussed on perinatal hypoxia–ischaemia as one of four clinical areas. Access the ATAIN e-learning package at: https: //www. e-lfh. org. uk/programmes/avoiding-term-admissions-into -neonatal-units/ Does an admitted baby born at 35 weeks gestational age or above have an encephalopathy within the first three full calendar days after birth? National result (births between 2015 and 2017): 1. 58 cases per 1000 live births (95% confidence interval: 1. 64 -1. 53)
How did we do? Measuring infection • To look up your unit’s results for Bloodstream infection and CLABSI (QISD), go to the annual reports section of NNAP Online: https: //nnap. rcpch. ac. uk/annual-reports. aspx 1. From ‘Choose data year’, select ‘ 2018’. 2. From ‘Choose a unit or network report, select ‘Neonatal Unit level data’ 3. From ‘Choose specific unit/network’, select your unit. 4. Choose ‘Bloodstream infection’ or QISD CLABSI’ from the tabs to view your unit’s results table. 5. Note whether your unit was able to ensure that all positive blood cultures were entered. 6. To view a list of all units, and to filter by just those who were able to validate their data entry, select ‘List all units’ from ‘Choose specific unit/network’ and check the box ‘Display units with validated positive blood culture reporting only’. Does an admitted baby have one or more episodes of bloodstream infection, characterised by one or more positive blood cultures taken, after 72 hours of age? National result: 1. 6% of babies have a growth of any clearly pathogenic organism. How many babies have a positive blood culture (any species) with a central line present, after the first 72 hours of life, per 1000 central line days? National result: 5. 13 babies with a central line associated bloodstream infection per 1000 central line days
What next? Measuring infection Recommendations: Use evidence-based strategies to lower rates of infection or necrotising enterocolitis (NEC). Consider comparing practice with units with ‘complete’ data who have lower rates of infection or NEC to drive improvement in local rates. Action: Neonatal units • Further information and resources: • Develop processes to ensure that NEC and blood culture data • are complete using NNAP quarterly reports to provide assurance. Action: Neonatal units with incomplete NEC and blood culture data • Neonatal networks should work with units that do not validate their NEC or Bloodstream infection NNAP data in order to ensure full participation in the audit, and maximise compliance with the NHS neonatal service specification in England other appropriate structures within the devolved administrations and crown dependencies. Action: Neonatal networks • Infection in Critical Care Quality Improvement Programme (ICCQIP) Maternity and Children Quality Improvement Collaborative (MCQIC )
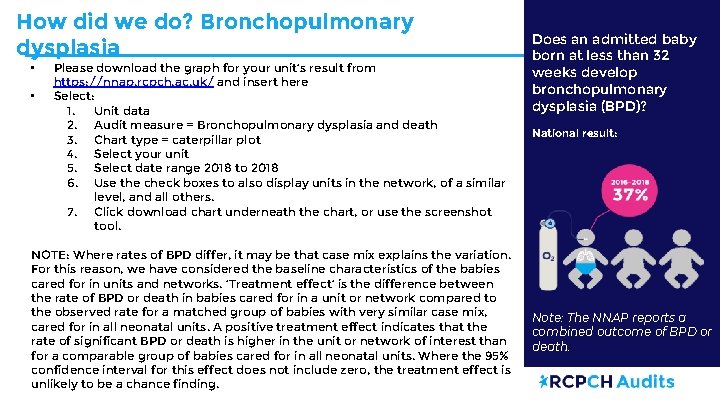
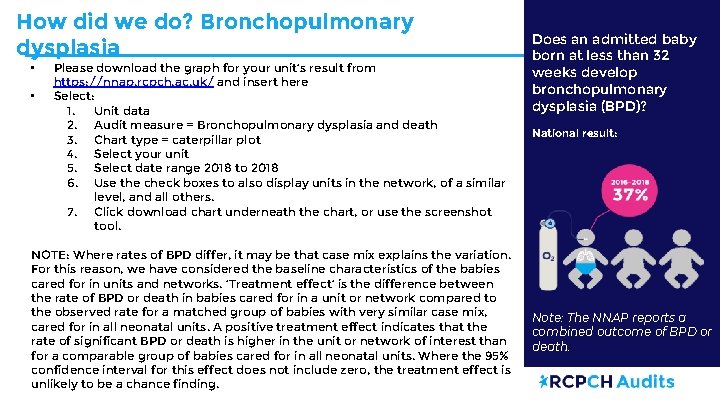
How did we do? Bronchopulmonary dysplasia • • Please download the graph for your unit’s result from https: //nnap. rcpch. ac. uk/ and insert here Select: 1. Unit data 2. Audit measure = Bronchopulmonary dysplasia and death 3. Chart type = caterpillar plot 4. Select your unit 5. Select date range 2018 to 2018 6. Use the check boxes to also display units in the network, of a similar level, and all others. 7. Click download chart underneath the chart, or use the screenshot tool. NOTE: Where rates of BPD differ, it may be that case mix explains the variation. For this reason, we have considered the baseline characteristics of the babies cared for in units and networks. ‘Treatment effect’ is the difference between the rate of BPD or death in babies cared for in a unit or network compared to the observed rate for a matched group of babies with very similar case mix, cared for in all neonatal units. A positive treatment effect indicates that the rate of significant BPD or death is higher in the unit or network of interest than for a comparable group of babies cared for in all neonatal units. Where the 95% confidence interval for this effect does not include zero, the treatment effect is unlikely to be a chance finding. Does an admitted baby born at less than 32 weeks develop bronchopulmonary dysplasia (BPD)? National result: Note: The NNAP reports a combined outcome of BPD or death.
What next? Bronchopulmonary dysplasia Recommendations: Further information and resources: Assess practice for the treatment of bronchopulmonary dysplasia (BPD) against • NICE guideline; NICE guidelines for respiratory care for Specialist preterm babies. Consider comparing neonatal practice with units with a lower rate of BPD respiratory care to identify quality improvement for babies born opportunities. preterm Action: Neonatal networks and units with a ‘positive’ treatment effect for BPD where the 95% confidence interval excludes zero.
How did we do? Necrotising enterocolitis • • Please download the graph for your unit’s result from https: //nnap. rcpch. ac. uk/ and insert here. Select: 1. Unit data 2. Audit measure = parents on ward rounds 3. Chart type = bar chart 4. Select your unit 5. Select date range 2018 to 2018 6. Use the check boxes to also display units in the network, of a similar level, and all others. 7. Click download chart underneath the chart, or use the screenshot tool. Does an admitted baby born at less than 32 weeks gestational age meet the NNAP surveillance definition for necrotising enterocolitis (NEC) on one or more occasion? National result:
What next? Necrotising enterocolitis Recommendations: Use evidence-based strategies to lower rates of infection or necrotising enterocolitis (NEC). Consider comparing practice with units with ‘complete’ data who have lower rates of infection or NEC to drive improvement in local rates. Action: Neonatal units • Further information and resources: • • Develop processes to ensure that NEC and blood culture data are complete using NNAP quarterly reports to provide assurance. Action: Neonatal units with incomplete NEC and blood culture data • Neonatal networks should work with units that do not validate their NEC or Bloodstream infection NNAP data in order to ensure full participation in the audit, and maximise compliance with the NHS neonatal service specification in England other appropriate structures within the devolved administrations and crown dependencies. Action: Neonatal networks • Special Interest Group in Necrotising Enterocolitis Case study: Reducing necrotising enterocolitis (NEC): A quality improvement initiative, West Hertfordshire NHS Trust.
How did we do? Minimising separation of mother and baby (term) • • Please download the graph for your unit’s result from https: //nnap. rcpch. ac. uk/ and insert here. Select: 1. Unit data 2. Audit measure = minimising separation - term 3. Chart type = bar chart 4. Select your unit 5. Select date range 2018 to 2018 6. Use the check boxes to also display units in the network, of a similar level, and all others. 7. Click download chart underneath the chart, or use the screenshot tool. For a baby born at gestational age greater than or equal to 37 weeks, who did not have any surgery or a transfer during any admission, how many special care or normal care days were provided when oxygen was not administered? National result: National average: 3 days
How did we do? Minimising separation of mother and baby (late preterm) • • Please download the graph for your unit’s result from https: //nnap. rcpch. ac. uk/ and insert here. Select: 1. Unit data 2. Audit measure = minimising separation – late preterm 3. Chart type = bar chart 4. Select your unit 5. Select date range 2018 to 2018 6. Use the check boxes to also display units in the network, of a similar level, and all others. 7. Click download chart underneath the chart, or use the screenshot tool. For a baby born at 34 -36 weeks gestational age, who did not have any surgery or a transfer during any admission, how many special care or normal care days were provided when oxygen was not administered? National result: National average: 6. 6 days
What next? Minimising separation of mother and baby (term and late preterm) Further information and resources: • Avoiding Term Admissions to Neonatal Units (ATAIN) programme • British Association for Perinatal Medicine (BAPM) Neonatal Transitional Care Framework for Practice • National Maternity and Perinatal Audit (NMPA) Organisational Report • Case study: Destination TC! Reducing Mother/Infant Separation in Hospital. West Recommendation: Use local knowledge of the rates of admission of term and near-term babies, case review (as used in the ATAIN programme), process mapping and Pareto charts to identify and action modifiable factors to address prolonged mother infant separation. Action: Neonatal units Hertfordshire Hospitals NHS Trust. • Case study: Establishing a transitional care service across three units. Betsi Cadwaladr University Health Board
How did we do? Breastmilk feeding at discharge home • • • Please download the graph for your unit’s result from https: //nnap. rcpch. ac. uk/ and insert here Select: 1. Unit data 2. Audit measure = Mother’s milk at discharge 3. Chart type = caterpillar plot 4. Select your unit 5. Select date range 2018 to 2018 6. Use to check boxes to also display units in the network, of a similar level, and all others. 7. Click download chart underneath the chart, or use the screenshot tool. Alternatively, you may wish to use the longitudinal data stick plots to display your results between 2016 and 2018, select: 1. Longitudinal data 2. Audit measure = Breastmilk feeding at discharge 3. Choose a unit or network report = neonatal unit level data 4. Primary unit/hospital = your unit 5. Data year = 2016 -2018 6. Click on the three horizontal lines on the top right of the chart to download the chart as an image. Does a baby born at less than 33 weeks gestational age receive any of their own mother’s milk at discharge to home from a neonatal unit? National result:
Further What next? Breastmilk feeding at discharge home information and resources: Recommendation: Identify barriers to breastfeeding across the patient pathways using: • parent feedback • a review of breastmilk feeding rate at discharge • the early breastmilk feeding measure in the NNAP quarterly reports. Use tools such as the UNICEF Neonatal Unit Baby Friendly Initiative and Bliss Baby Charter to overcome barriers identified and to drive improvement. Action: Neonatal units • UNICEF Baby Friendly Initiative • Bliss Baby Charter • Case study: Project to review the use of Expressed Breast Milk (EBM) in neonatal units across Yorkshire and the Humber ODN.
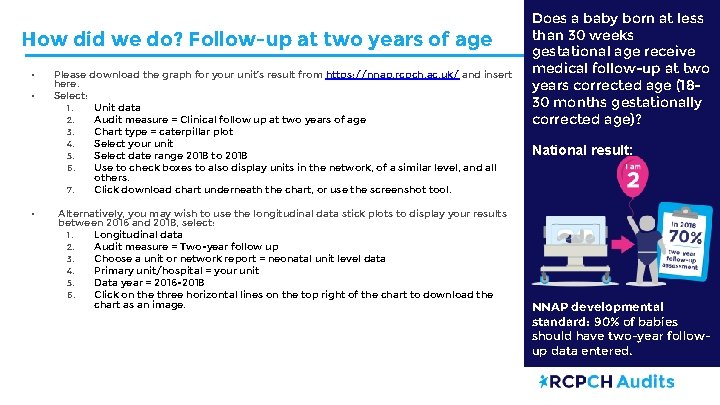
How did we do? Follow-up at two years of age • • • Please download the graph for your unit’s result from https: //nnap. rcpch. ac. uk/ and insert here. Select: 1. Unit data 2. Audit measure = Clinical follow up at two years of age 3. Chart type = caterpillar plot 4. Select your unit 5. Select date range 2018 to 2018 6. Use to check boxes to also display units in the network, of a similar level, and all others. 7. Click download chart underneath the chart, or use the screenshot tool. Alternatively, you may wish to use the longitudinal data stick plots to display your results between 2016 and 2018, select: 1. Longitudinal data 2. Audit measure = Two-year follow up 3. Choose a unit or network report = neonatal unit level data 4. Primary unit/hospital = your unit 5. Data year = 2016 -2018 6. Click on the three horizontal lines on the top right of the chart to download the chart as an image. Does a baby born at less than 30 weeks gestational age receive medical follow-up at two years corrected age (1830 months gestationally corrected age)? National result: NNAP developmental standard: 90% of babies should have two-year followup data entered.
What next? Follow-up at two years of age Further information and resources: • NICE guideline: Developmental follow-up of children and young people born preterm. • Case study: Neurodevelopmental follow-up: Multidisciplinary team working to standardise the delivery, uptake and recording of twoyear neurodevelopmental assessments. Royal Recommendation: Produce detailed plans to provide or organise follow up of care for babies in accordance with NICE guidance: Developmental follow-up of children and young people born preterm. Consider arrangements for: • • • communicating with families about follow up at discharge families who live far from the hospital of care families who do not attend appointments families who move to different areas completing and documenting assessments made. Action: Neonatal units Hospital for Children, Glasgow
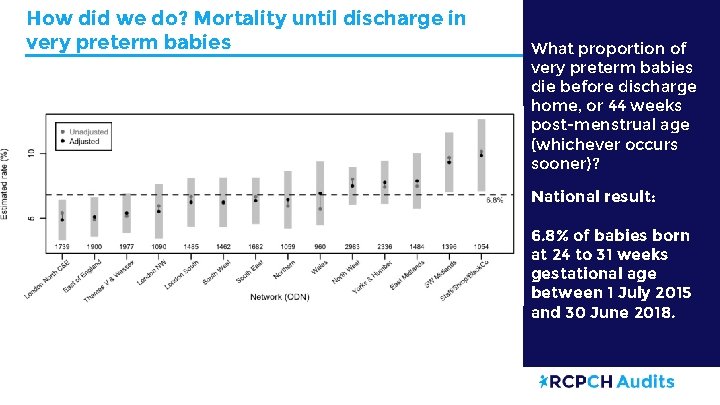
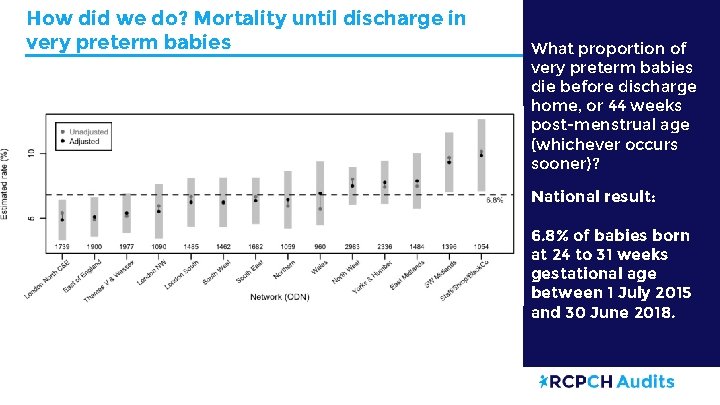
How did we do? Mortality until discharge in very preterm babies What proportion of very preterm babies die before discharge home, or 44 weeks post-menstrual age (whichever occurs sooner)? National result: 6. 8% of babies born at 24 to 31 weeks gestational age between 1 July 2015 and 30 June 2018.
What next? Mortality until discharge in very preterm babies Recommendations: To reduce mortality, neonatal networks should, following a review of local mortality results, take action to: o consider whether a review of network structure, clinical flows, guidelines and staffing may be helpful in responding to local mortality rates o consider the extent of the implementation of evidence-based strategies in the following areas to reduce mortality: — antenatal steroids — deferred cord clamping — avoidance of hypothermia — management of respiratory disease. o ensure that shared learning from multi-disciplinary reviews of deaths (including data from the local use of the Perinatal Mortality Review Tool) informs: — network governance — unit level clinical practice. Action: Neonatal networks Further information and resources: • Use NNAP quarterly reports to ensure that a mortality outcome is clearly recorded for every baby admitted. For babies discharged to a non NNAP unit before 44 weeks’ post menstrual age, units should capture outcome using the ‘final neonatal outcome’ field. Action: Neonatal units and networks • • Each Baby Counts, Royal College of Obstetricians and Gynaecology • MBRRACE-UK • Perinatal Mortality Review Tool • National Child Mortality Database
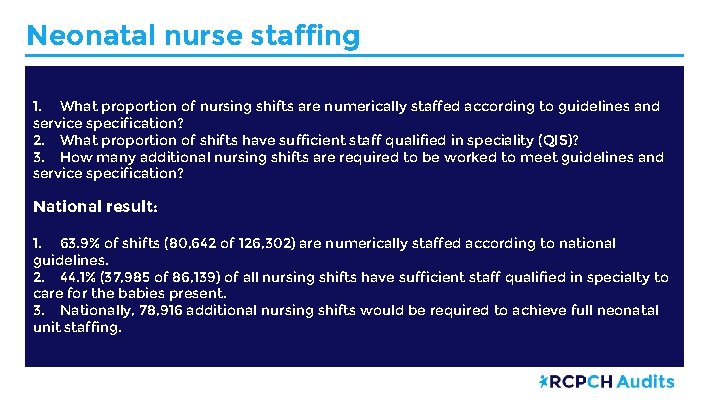
Neonatal nurse staffing 1. What proportion of nursing shifts are numerically staffed according to guidelines and service specification? 2. What proportion of shifts have sufficient staff qualified in speciality (QIS)? 3. How many additional nursing shifts are required to be worked to meet guidelines and service specification? National result: 1. 63. 9% of shifts (80, 642 of 126, 302) are numerically staffed according to national guidelines. 2. 44. 1% (37, 985 of 86, 139) of all nursing shifts have sufficient staff qualified in specialty to care for the babies present. 3. Nationally, 78, 916 additional nursing shifts would be required to achieve full neonatal unit staffing.
How did we do? Neonatal nurse staffing • To look up your unit’s results for Neonatal nurse staffing, go to the annual reports section of NNAP Online: https: //nnap. rcpch. ac. uk/annual-reports. aspx 1. From ‘Choose data year’, select ‘ 2018’. 2. From ‘Choose a unit or network report, select ‘Neonatal Unit level data’ 3. From ‘Choose specific unit/network’, select your unit. 4. Choose ‘Nurse staffing’ from the tabs to view your unit’s results table.
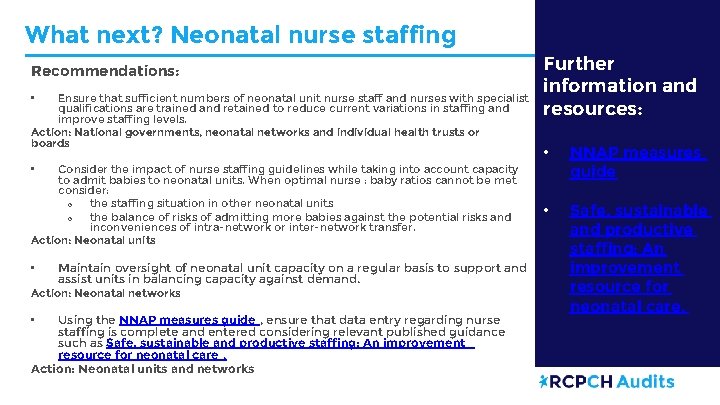
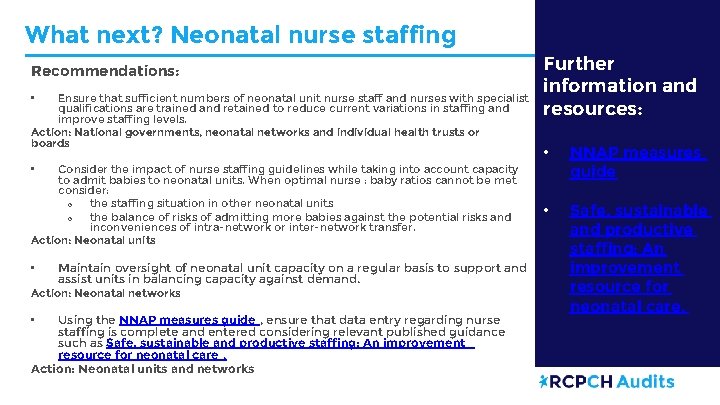
What next? Neonatal nurse staffing Recommendations: Ensure that sufficient numbers of neonatal unit nurse staff and nurses with specialist qualifications are trained and retained to reduce current variations in staffing and improve staffing levels. Action: National governments, neonatal networks and individual health trusts or boards • Consider the impact of nurse staffing guidelines while taking into account capacity to admit babies to neonatal units. When optimal nurse : baby ratios cannot be met consider: o the staffing situation in other neonatal units o the balance of risks of admitting more babies against the potential risks and inconveniences of intra-network or inter-network transfer. Action: Neonatal units Further information and resources: • NNAP measures guide • Safe, sustainable and productive staffing: An improvement resource for neonatal care. • • Maintain oversight of neonatal unit capacity on a regular basis to support and assist units in balancing capacity against demand. Action: Neonatal networks Using the NNAP measures guide , ensure that data entry regarding nurse staffing is complete and entered considering relevant published guidance such as Safe, sustainable and productive staffing: An improvement resource for neonatal care. Action: Neonatal units and networks •
Developing an action plan • With the multidisciplinary team, set goals and develop action plans where your unit results require improvement and your unit is not meeting the audit recommendations. • Use the recommendations checklist to track your unit, trust/health board or network’s status. • Monitor your unit’s performance through the year using NNAP quarterly reports and real time data. • Continue to revisit the recommendations checklist and your unit’s action plan throughout the year.
Planning your improvement goals: Questions for discussion You may consider using the following questions to trigger discussion as a team: • Which areas do we need to focus on for improvement? o Agree as a team which area or areas you will target • What are the four primary drivers (topics or areas) that you will need to work on, in order to achieve your aim? • Are there any secondary drivers that need to be in place to positively influence the primary drivers? • What changes will we make to positively influence the drivers and achieve our aim? Questions are based on the driver diagram model which can be used to plan quality improvement project activities: https: //improvement. nhs. uk/resources/driver-diagrams-tree-diagrams/
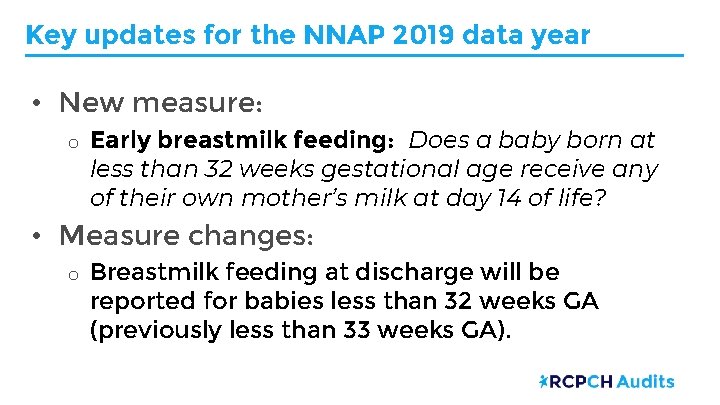
Key updates for the NNAP 2019 data year • New measure: o Early breastmilk feeding: Does a baby born at less than 32 weeks gestational age receive any of their own mother’s milk at day 14 of life? • Measure changes: o Breastmilk feeding at discharge will be reported for babies less than 32 weeks GA (previously less than 33 weeks GA).
Key updates for the 2020 data year • New measure: o Deferred cord clamping: Does a baby born at less than 32 weeks gestational age have their cord clamped at or after one minute? • Measure changes: o Parental consultation within 24 hours: This measure will consider every admission to a neonatal unit for each baby, not just first admission.
Useful links NNAP 2019 annual report on 2018 data Your baby’s care – parent and carer guide to NNAP Online https: //nnap. rcpch. ac. uk/ NNAP measures guides: https: //www. rcpch. ac. uk/workwe-do/quality-improvement-patient-safety/nationalneonatal-audit-programme-nnap/about#about • RCPCH QI Central – case studies: www. qicentral. org. uk • Contact the NNAP team: nnap@rcpch. ac. uk • •