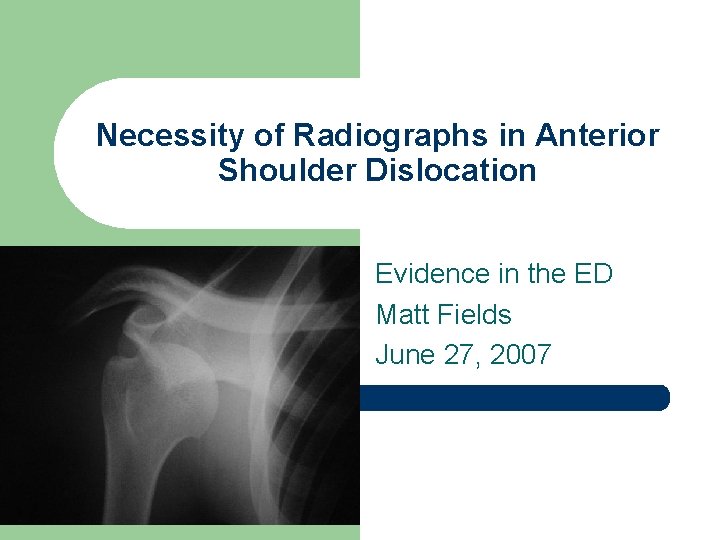
Necessity of Radiographs in Anterior Shoulder Dislocation Evidence


- Slides: 16
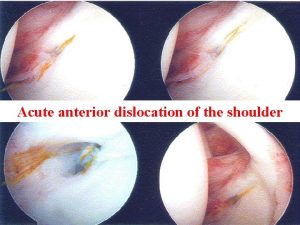
Necessity of Radiographs in Anterior Shoulder Dislocation Evidence in the ED Matt Fields June 27, 2007
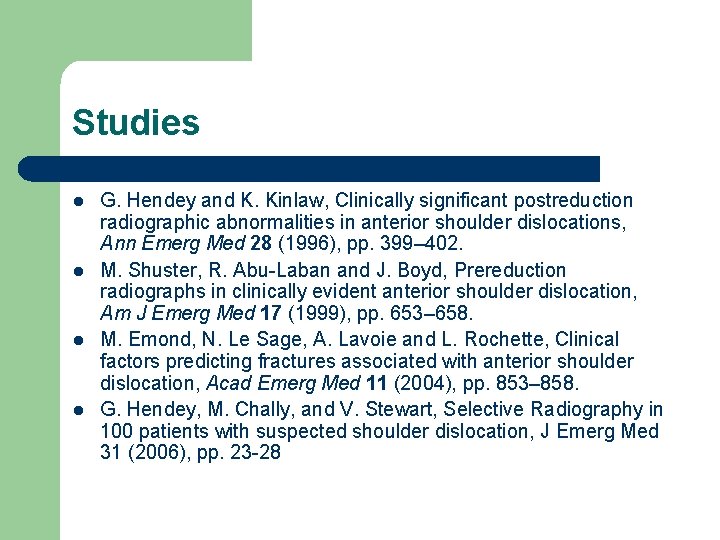
Studies l l G. Hendey and K. Kinlaw, Clinically significant postreduction radiographic abnormalities in anterior shoulder dislocations, Ann Emerg Med 28 (1996), pp. 399– 402. M. Shuster, R. Abu-Laban and J. Boyd, Prereduction radiographs in clinically evident anterior shoulder dislocation, Am J Emerg Med 17 (1999), pp. 653– 658. M. Emond, N. Le Sage, A. Lavoie and L. Rochette, Clinical factors predicting fractures associated with anterior shoulder dislocation, Acad Emerg Med 11 (2004), pp. 853– 858. G. Hendey, M. Chally, and V. Stewart, Selective Radiography in 100 patients with suspected shoulder dislocation, J Emerg Med 31 (2006), pp. 23 -28
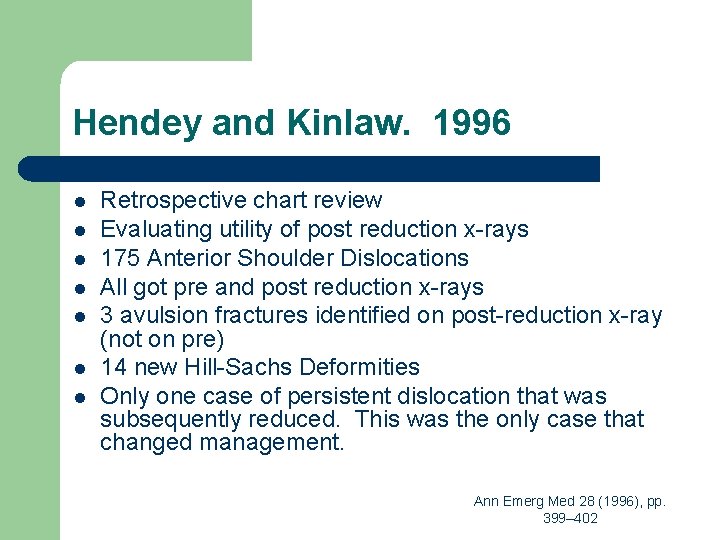
Hendey and Kinlaw. 1996 l l l l Retrospective chart review Evaluating utility of post reduction x-rays 175 Anterior Shoulder Dislocations All got pre and post reduction x-rays 3 avulsion fractures identified on post-reduction x-ray (not on pre) 14 new Hill-Sachs Deformities Only one case of persistent dislocation that was subsequently reduced. This was the only case that changed management. Ann Emerg Med 28 (1996), pp. 399– 402
Hendey and Kinlaw. 1996 l Conclusion – Postreduction radiographs rarely reveal any clinically significant abnormality after an anterior shoulder dislocation has been reduced. Ann Emerg Med 28 (1996), pp. 399– 402
Shuster et al. 1999 l l l Prospective, evaluating utility of pre-reduction x-rays 97 patients presenting to 2 ski-hill clinics and a rural ED (Banff, Colorado) with possible dislocation as assessed by triage staff. At the rural ED, physician certain of dislocation in 40/59 cases on history and physical. All 40 confirmed to have dislocation by x-ray. 36 cases at ski-hill clinic all reduced without x-ray. Prereduction radiograph (when performed) did not change management and added 29. 6 +/- 12. 68 minutes to treatment. Am J Emerg Med 17 (1999), pp. 653– 658.
Shuster et al. 1999 l Conclusion – – Experienced physicians are accurate at diagnosing anterior shoulder dislocation from history and physical. Prereduction x-rays do not alter management and delay treatment. Am J Emerg Med 17 (1999), pp. 653– 658.
Shuster et al. 1999 l This paper also notes that post-reduction films did not change acute management. However the authors believe that postreduction x-rays are good because they reveal fractures, and thus to identify the need for additional treatment or changes to the rehabilitation program. Am J Emerg Med 17 (1999), pp. 653– 658.

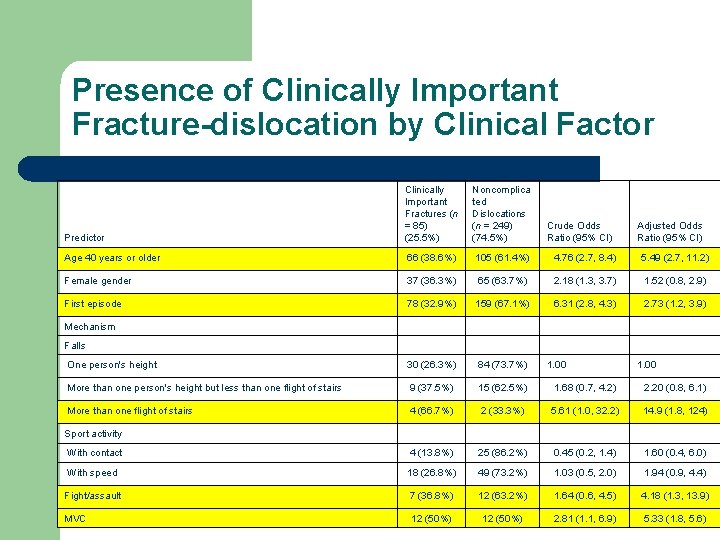
Emond et al. 2004 l l Retrospective Study over 5 years period to compare profiles of those having a clinically important fracture with their shoulder dislocation and those sustaining a noncomplicated shoulder dislocation. 334 patients included: 85 (25. 5%) had a clinically important fracture-dislocation, 249 (74. 5%) had a non-complicated dislocation. Acad Emerg Med 11 (2004), pp. 853– 858.
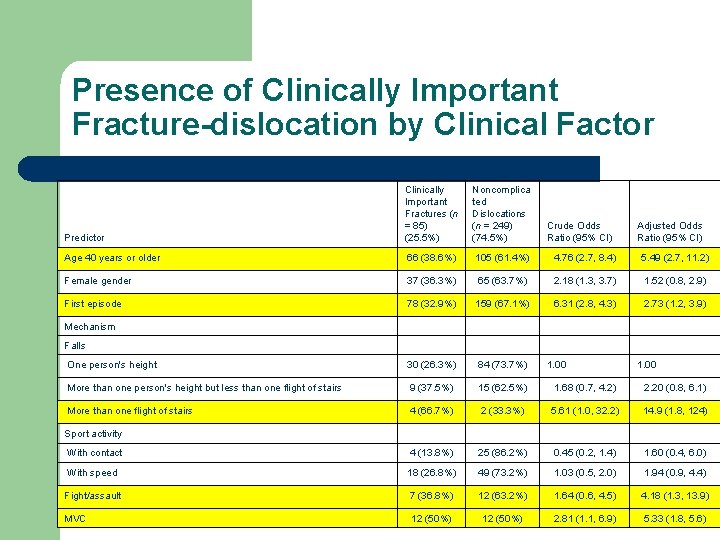
Presence of Clinically Important Fracture-dislocation by Clinical Factor Predictor Clinically Important Fractures (n = 85) (25. 5%) Noncomplica ted Dislocations (n = 249) (74. 5%) Crude Odds Ratio (95% CI) Age 40 years or older 66 (38. 6%) 105 (61. 4%) 4. 76 (2. 7, 8. 4) 5. 49 (2. 7, 11. 2) Female gender 37 (36. 3%) 65 (63. 7%) 2. 18 (1. 3, 3. 7) 1. 52 (0. 8, 2. 9) First episode 78 (32. 9%) 159 (67. 1%) 6. 31 (2. 8, 4. 3) 2. 73 (1. 2, 3. 9) One person's height 30 (26. 3%) 84 (73. 7%) More than one person's height but less than one flight of stairs 9 (37. 5%) 15 (62. 5%) 1. 68 (0. 7, 4. 2) 2. 20 (0. 8, 6. 1) More than one flight of stairs 4 (66. 7%) 2 (33. 3%) 5. 61 (1. 0, 32. 2) 14. 9 (1. 8, 124) With contact 4 (13. 8%) 25 (86. 2%) 0. 45 (0. 2, 1. 4) 1. 60 (0. 4, 6. 0) With speed 18 (26. 8%) 49 (73. 2%) 1. 03 (0. 5, 2. 0) 1. 94 (0. 9, 4. 4) Fight/assault 7 (36. 8%) 12 (63. 2%) 1. 64 (0. 6, 4. 5) 4. 18 (1. 3, 13. 9) MVC 12 (50%) 2. 81 (1. 1, 6. 9) 5. 33 (1. 8, 5. 6) Adjusted Odds Ratio (95% CI) Mechanism Falls 1. 00 Sport activity
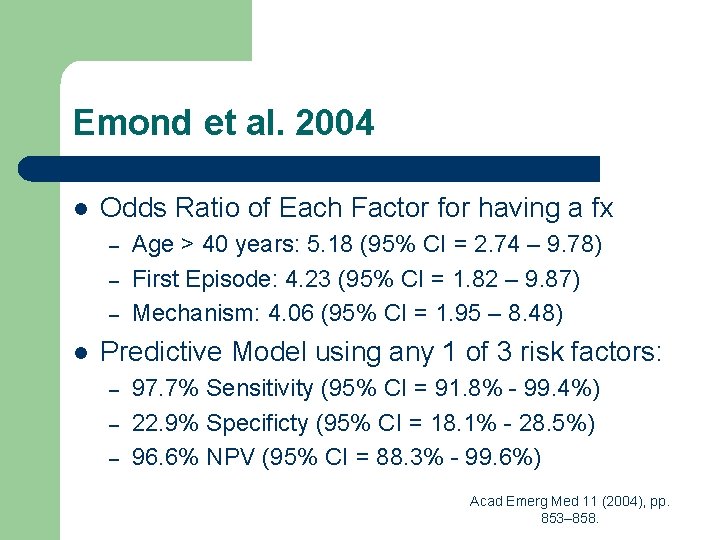
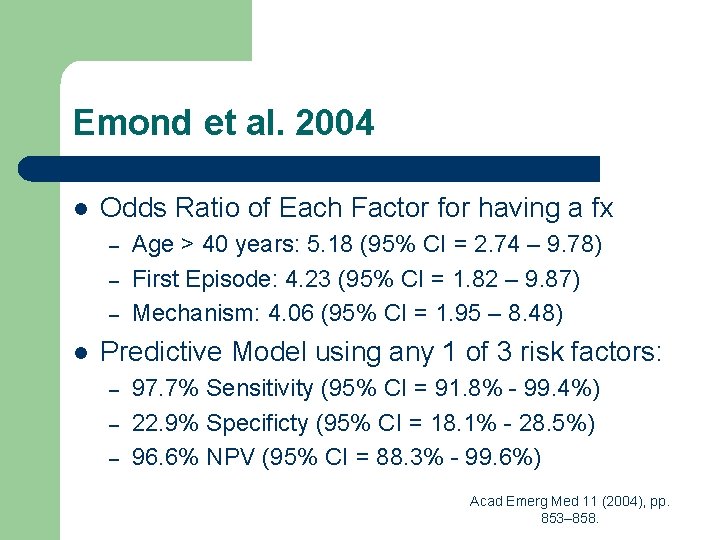
Emond et al. 2004 l Odds Ratio of Each Factor for having a fx – – – l Age > 40 years: 5. 18 (95% CI = 2. 74 – 9. 78) First Episode: 4. 23 (95% CI = 1. 82 – 9. 87) Mechanism: 4. 06 (95% CI = 1. 95 – 8. 48) Predictive Model using any 1 of 3 risk factors: – – – 97. 7% Sensitivity (95% CI = 91. 8% - 99. 4%) 22. 9% Specificty (95% CI = 18. 1% - 28. 5%) 96. 6% NPV (95% CI = 88. 3% - 99. 6%) Acad Emerg Med 11 (2004), pp. 853– 858.
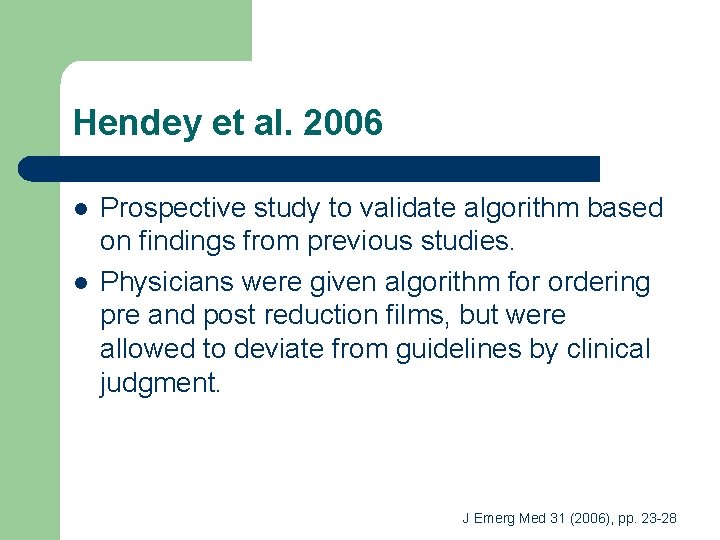
Hendey et al. 2006 l l Prospective study to validate algorithm based on findings from previous studies. Physicians were given algorithm for ordering pre and post reduction films, but were allowed to deviate from guidelines by clinical judgment. J Emerg Med 31 (2006), pp. 23 -28
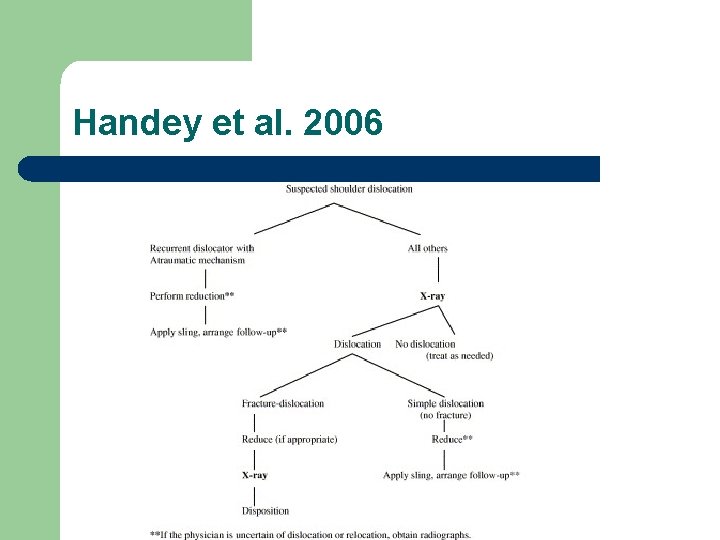
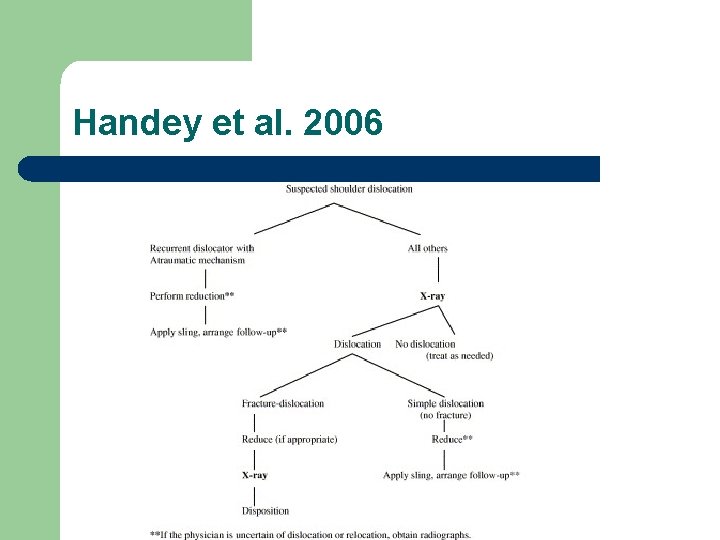
Handey et al. 2006
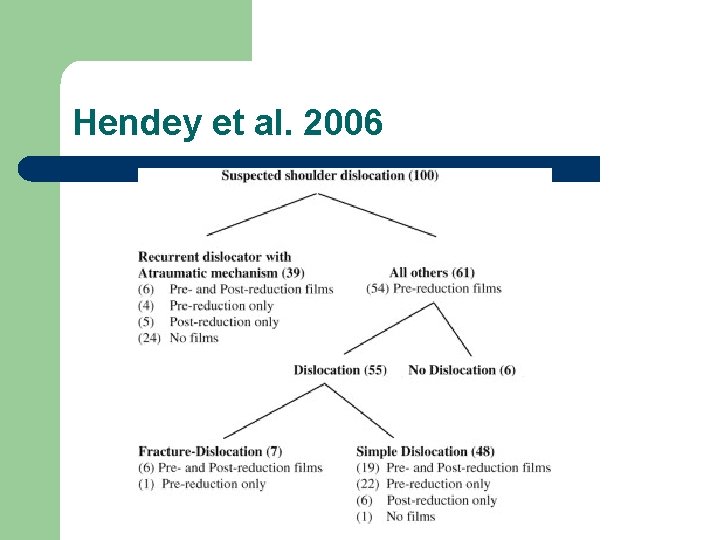
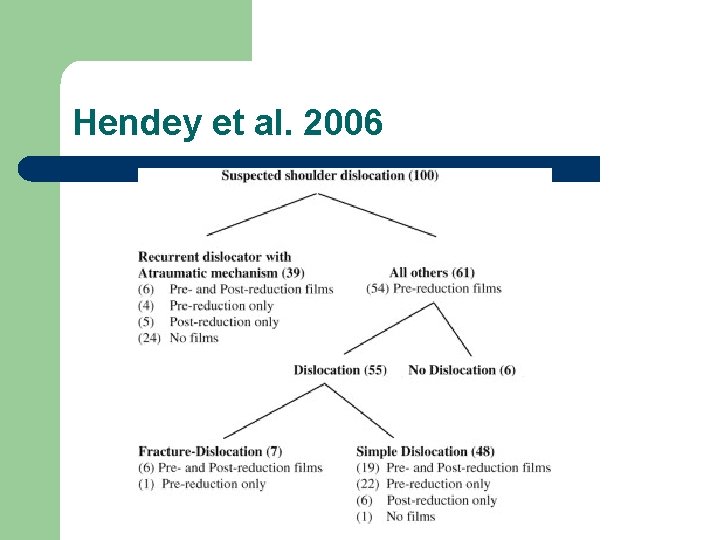
Hendey et al. 2006
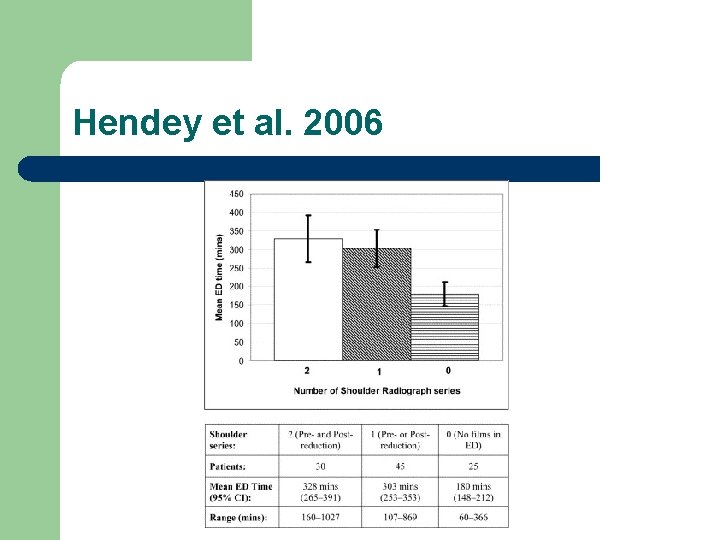
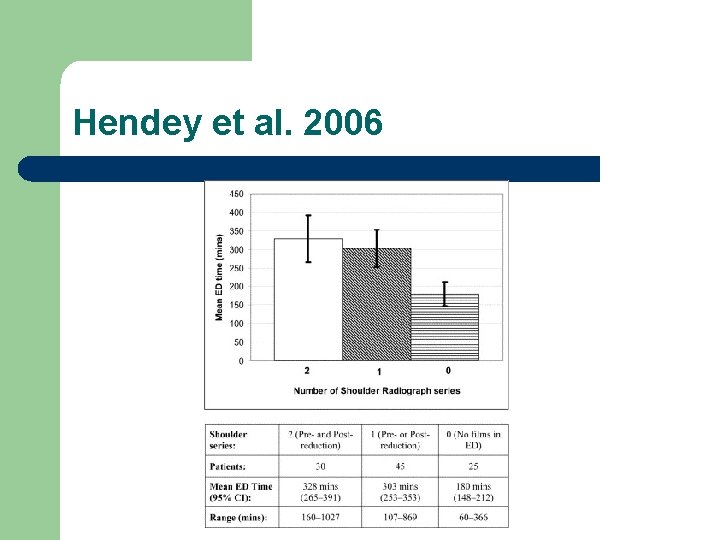
Hendey et al. 2006

Hendey et al. 2006 l Performed phone contact at 1 and 30 days and chart review at 30 days. – – Able to contact 76% at day 1 and 61% at both days. 18 of 25 patients who received no radiographs were reached with no missed fractures. 75 of 76 patients reached satisfied with ED care. 40% of all patients followed up in ortho clinic. l l l 11/30 who had pre and post films. 3 had repeat films. 27/64 who had one or no film. 9 got shoulder films in clinic. No missed fractures or persistent dislocations. J Emerg Med 31 (2006), pp. 23 -28
HUPism l l In patients under 40 with non-traumatic recurrent anterior shoulder dislocation x-rays are not necessary. In all other cases a pre-reduction x-ray should be obtained, but if no clinically significant fracture is seen then a postreduction x-ray is not necessary.
 Thalassemia
Thalassemia Dislocation glide vs climb
Dislocation glide vs climb Abbot saunders test
Abbot saunders test Stimson technique shoulder dislocation
Stimson technique shoulder dislocation Shoulder dislocation strapping
Shoulder dislocation strapping Dr shane barclay
Dr shane barclay Bodybuilding serratus anterior
Bodybuilding serratus anterior Painful arc test
Painful arc test Bitewing periapical
Bitewing periapical Chapter 39 digital imaging film and radiographs
Chapter 39 digital imaging film and radiographs What are the five basic sizes of intraoral dental film?
What are the five basic sizes of intraoral dental film? Lower 90 degree occlusal
Lower 90 degree occlusal Chapter 39 digital imaging film and radiographs
Chapter 39 digital imaging film and radiographs Explain how class evidence may be useful.
Explain how class evidence may be useful. Jobs vancouver
Jobs vancouver Class vs individual evidence
Class vs individual evidence What is a primary source
What is a primary source