Motion sickness mouth Ulcer Motion sickness is thought






- Slides: 19
Motion sickness & mouth Ulcer
• Motion sickness is thought to be caused by a conflict of messages to the brain, where the vomiting centre receives information from the eyes, the GI tract and the vestibular system in the ear. • Parents commonly seek advice about how to prevent motion sickness in children, in whom the problem is most common. Any form of travel can produce symptoms, including air, sea and road. • Effective prophylactic treatments are available OTC and can be selected to match the patient’s needs.
Motion sickness is common in young children • Babies and very young children up to 2 years seem to only rarely suffer from the problem and therefore do not usually require treatment. • The incidence of motion sickness seems to greatly reduce with age, although some adults still experience symptoms.
Mode of travel/length of journey • Once vomiting starts there is little that can be done, so any medicine recommended by the pharmacist must be taken in good time before the journey if it is to be effective. • The fact that it is important that the symptoms are prevented before they can gain a hold should be emphasised to the parents. • If it is a long journey, it may be necessary to repeat the dose while travelling and the recommended dosage interval should be stressed.
• Children are less likely to feel or be sick if they can see out of the car, so appropriate seats can be used to elevate the seating position of small children. • It allows the child to see relatively still objects outside the car. • Children are less likely to experience symptoms if they are kept occupied by playing games • However, many travel sickness sufferers, reading exacerbates the feeling of nausea.
Management Antihistamines • Antihistamines include cinnarizine, meclozine and promethazine. Anticholinergic effects • All have the potential to cause drowsiness and promethazine appears to be the most sedative. • Meclozine and promethazine have long durations of action and are useful for long journeys since they need to be taken only once daily. • Cinnarizine and promethazine are not recommended for children younger than 5 years, whereas meclozine can be given to those over 2 years.
Anticholinergic agents • The only anticholinergic used widely in the prevention of motion sickness is hyoscine hydrobromide, which can be given to children over 3 years. • Anticholinergic drugs can cause drowsiness, blurred vision, dry mouth, constipation and urinary retention as side-effects, • Hyoscine has a short duration of action (from 1 to 3 h). suitable for shorter journeys and should be given 20 min before the start of the journey. • Anticholinergic drugs and antihistamines with anticholinergic effects are best avoided in patients with prostatic hypertrophy and in glaucoma • intraocular pressure and urinary retention and might be increased
Other remidities • Ginger • Conflicting findings in travel sickness. No mechanism of • action has been identified, but it has been suggested that ginger acts on the GI tract itself rather than on the vomiting centre in the brain or on the vestibular system.

• Acupressure bands are stretchy bands worn around the wrists. They apply pressure to a particular point on the inside of your wrist between the two tendons on your inner arm.
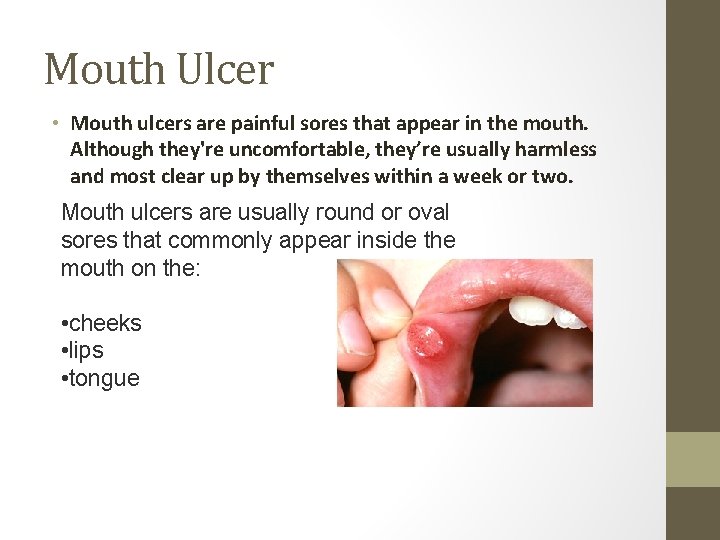
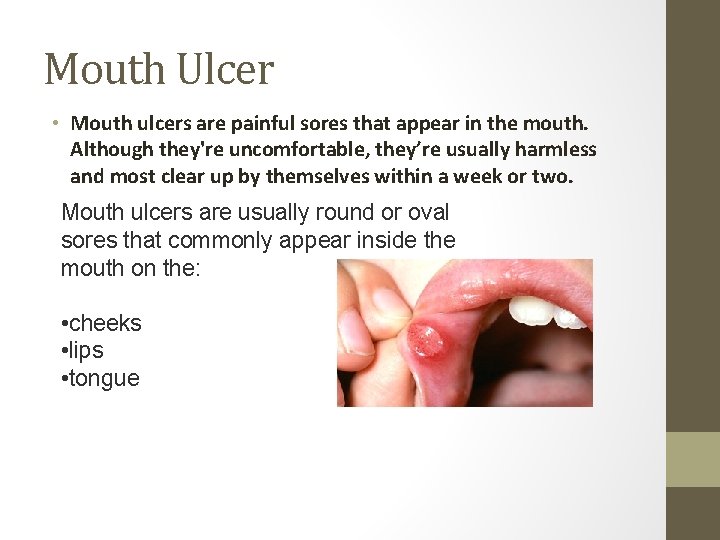
Mouth Ulcer • Mouth ulcers are painful sores that appear in the mouth. Although they're uncomfortable, they’re usually harmless and most clear up by themselves within a week or two. Mouth ulcers are usually round or oval sores that commonly appear inside the mouth on the: • cheeks • lips • tongue

• They can be white, red, yellow or grey in colour and swollen. • It's possible to have more than one mouth ulcer at a time and they may spread or grow. • Mouth ulcers shouldn't be confused with cold sores, which are small blisters that develop on the lips or around the mouth. Cold sores often begin with a tingling, itching or burning sensation around your mouth.

• Mouth ulcers can be painful, which can make it uncomfortable to eat, drink or brush teeth. • Mouth ulcers don’t usually need to be treated, because they tend to clear up by themselves within a week or two. • However, treatment can help to reduce swelling and ease any discomfort.

Causes • Most single mouth ulcers are caused by damage to the lining inside of the mouth. For example: • accidentally biting the inside of your cheek or a sharp tooth • poorly fitting dentures • hard food • a defective filling • Run in families 40%
• It’s not always clear what causes mouth ulcers that keep returning, but triggers are thought to include: • stress and anxiety • hormonal changes – some women develop mouth ulcers during their monthly period • eating certain foods – such as chocolate, spicy foods, coffee, peanuts, almonds, strawberries, cheese, tomatoes and wheat flour • toothpaste containing sodium lauryl sulphate • stopping smoking – when first stop smoking, may develop mouth ulcers

Management • Antimicrobial mouthwash may speed up healing and prevent infection of the ulcer. Children under two shouldn't use this treatment. It also contains chlorexidine gluconate, which may stain teeth – but this may fade once treatment is finished. • Painkillers are available as a mouthwash, lozenge, gel or spray. They can sting on first use and your mouth may feel numb – but this is temporary. Mouthwash can be diluted with water if stinging continues. Children under 12 shouldn’t use mouthwash or gel. Mouthwash shouldn’t be used for more than seven days in a row. • Corticosteroid lozenges may reduce pain and speed up healing. These are best used as soon as the ulcer appears, but shouldn't be used by children under 12.
• In a few cases, a long-lasting mouth ulcer can be a sign of mouth cancer. Ulcers caused by mouth cancer usually appear on or under the tongue, although you can get them in other areas of the mouth. • Risk factors for mouth cancer include: • smoking or using products that contain tobacco • drinking alcohol – smokers who are also heavy drinkers have a much higher risk compared to the population at large

Cold sore (herpes simplex virus) • Cold sores are small blisters that develop on the lips or around the mouth. They're caused by the herpes simplex virus and usually clear up without treatment within 7 to 10 days. • Cold sores often start with a tingling, itching or burning sensation around your mouth. Small fluid-filled sores then appear, usually on the edges of your lower lip. • is highly contagious and can be easily passed from person to person by close direct contact. After someone has contracted the virus, it remains inactive (dormant) most of the time. • However, every so often the virus can be activated by certain triggers, resulting in an outbreak of cold sores. These triggers vary from person to person, but can include sunlight, fatigue, an injury to the affected area, and, in women, their period. • Some people have frequently recurring cold sores around two or three times a year, while others have one cold sore and never have another. Some people never get cold sores at all because the virus never becomes active.
• Treating cold sores • Cold sores usually clear up by themselves without treatment within 7 to 10 days. • However, antiviral creams are available over the counter from pharmacies without a prescription. If used correctly, these can help ease your symptoms and speed up the healing time. • To be effective, these treatments should be applied as soon as the first signs of a cold sore appear – when you feel a tingling, itching or burning sensation around your mouth. Using an antiviral cream after this initial period is unlikely to have much of an effect. • Cold sore patches are also available that contain hydrocolloid gel, which is an effective treatment for skin wounds. The patch is placed over the cold sore while it heals.
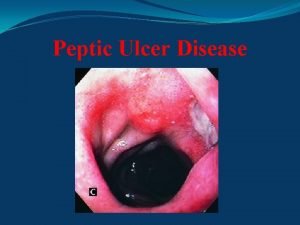
 Gastric ulcer vs duodenal ulcer
Gastric ulcer vs duodenal ulcer Ulcer niche and ulcer notch
Ulcer niche and ulcer notch Niche and notch in gastric ulcer meaning
Niche and notch in gastric ulcer meaning Modified johnson classification
Modified johnson classification Anatomy of ulcer
Anatomy of ulcer Tuberculous ulcer vs typhoid ulcer
Tuberculous ulcer vs typhoid ulcer Complete or incomplete thought
Complete or incomplete thought Lcc outline
Lcc outline Pagwash
Pagwash How does baba view amir’s episodes with car sickness?
How does baba view amir’s episodes with car sickness? What is the irony in how mercutio receives his wound?
What is the irony in how mercutio receives his wound? Nhs sickness
Nhs sickness Serum sickness hypersensitivity type
Serum sickness hypersensitivity type Altitude sickness
Altitude sickness Hezekiah sickness and recovery
Hezekiah sickness and recovery Sewage sickness
Sewage sickness Decompression sickness
Decompression sickness Industry relations meaning
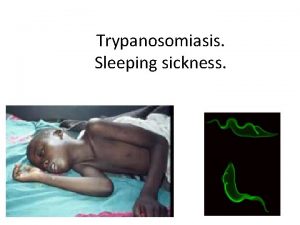
Industry relations meaning Trypanosomiasis
Trypanosomiasis Promastigote
Promastigote