Meet the Consultant Infectious Diseases Shana Gleeson MD




- Slides: 40
Meet the Consultant: Infectious Diseases Shana Gleeson, MD Infectious Diseases Fellow October 30, 2018 SLIDE
DISCLOSURE & ACCREDITATION I have no disclosures or conflicts of interest SLIDE 1
Overview • • Nuts and Bolts of the ID Consult Service Posing a consult question When to definitely consult ID Cover some key aspects of common ID problems SLIDE 2
Infectious Diseases Consult Service • York Street Campus – – – 3 fellows staffing 3 separate services General Immunosuppressed Smilow Patients are triaged according to phenotype and numbers of new consults • St Raphael’s Campus – 1 Consult service staffed by 1 fellow – There is also a private ID service at SRC (Dr. Alfirii), and those patients are not seen by fellows. • VA Medical Center – 1 Consult services staffed by 1 fellow SLIDE 3
Some Nuts and Bolts of the ID Consult Service • Work Flow – Follow ups are seen first thing in the morning. – New consults are seen as soon as follow ups are finished. – Rounds start after the fellow sees the new consults (usually early to mid afternoon). – New consult recommendations are finalized on rounds. • Outpatient Follow up – Need for follow up is determined by the ID consult team – Follow up is scheduled by the ID fellow • OPAT (Outpatient Parental Antibiotic Therapy) – – – Instructions are entered into the W 10 by the ID fellow W 10 serves as orders for the SNF or home infusion company Discharging team writes the antibiotic prescription Doses are not included in the W 10 instructions. Many IV antibiotics can be delivered in CADD Pumps SLIDE 4
Basic Principles of Consulting Infectious Diseases • • • Things to Do: Place consults early in the day. Have a clear consult question or problem you need help with. Know about your patient when you call. Tell your patient ID will be coming to see them. • • Things Not to Do: Place non-urgent consults late in the afternoon. Place a consult on the day of discharge. Place a new Epic Consult order on a patient already being followed by ID. • Pan-culture a patient indiscriminately SLIDE 5
Consult Questions • High quality consult questions are: – – Clear Focused Include relevant data Succinct SLIDE 6
Consult Questions • • Antibiotic treatment and duration Antibiotic coverage Infectious Disease work up Need IV antibiotics to go home when ready to be discharged Persistent fevers on antibiotics Pre-Post Septal Cellulitis Infection History of post laminectomy meningitis Curbside– pt with history DDKT on tac p/w Proteus UTI and bacteremia – any duration of IV antibiotics or can we narrow to PO antibiotics based on sensitivities (received 48 hours of zosyn)? SLIDE 7
Consult Questions • 81 year old woman with DLBCL admitted with ESBL bacteremia s/p 7 day course antibiotics, now with same bacteremia growing in urine and c/f septic R knee joint. Does not need to be seen tonight, can see tomorrow. • Neutropenic fever; Citrobacter Braakii bacteremia, pt has cellulitis/derm consulted. Regards antibiotic choice and duration of therapy because of the rare organism • 65 yo with AML s/p BMT on tacro who received platelet transfusion and subsequently has GNR bacteremia. Acinetobacter baumannii complex and GPC in pair. ? antibiotic choice and duration • Gram positive rods in CSF in patient with brain mets, lumbar drain, and concern for leptomeningeal disease • Advancing renal dysfunction on Genvoya – looking for new HIV regimen safe for use in CKD • Strep mitis bacteremia in neutropenic patient • MRSA bacterial endocarditis SLIDE 8
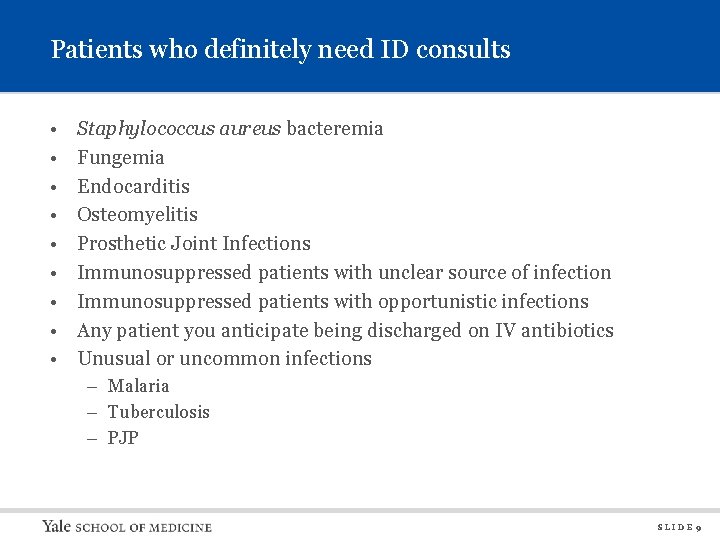
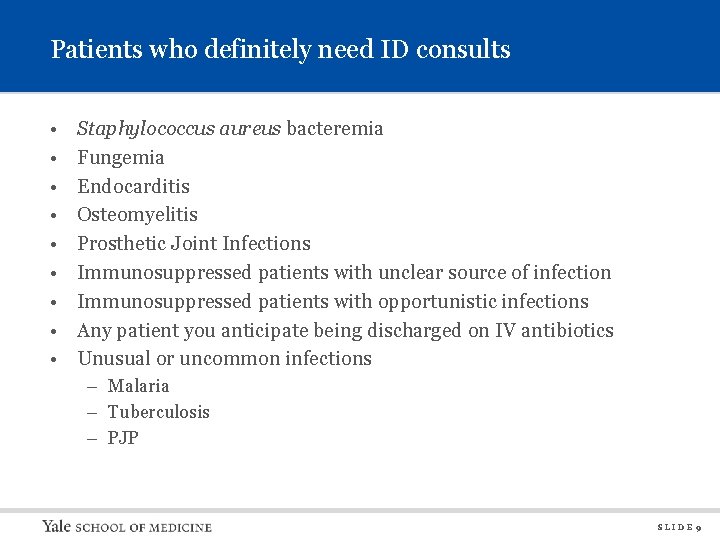
Patients who definitely need ID consults • • • Staphylococcus aureus bacteremia Fungemia Endocarditis Osteomyelitis Prosthetic Joint Infections Immunosuppressed patients with unclear source of infection Immunosuppressed patients with opportunistic infections Any patient you anticipate being discharged on IV antibiotics Unusual or uncommon infections – Malaria – Tuberculosis – PJP SLIDE 9
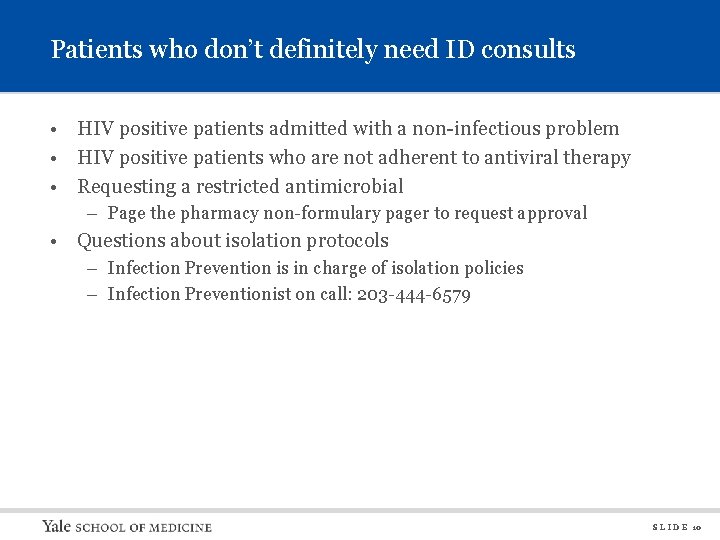
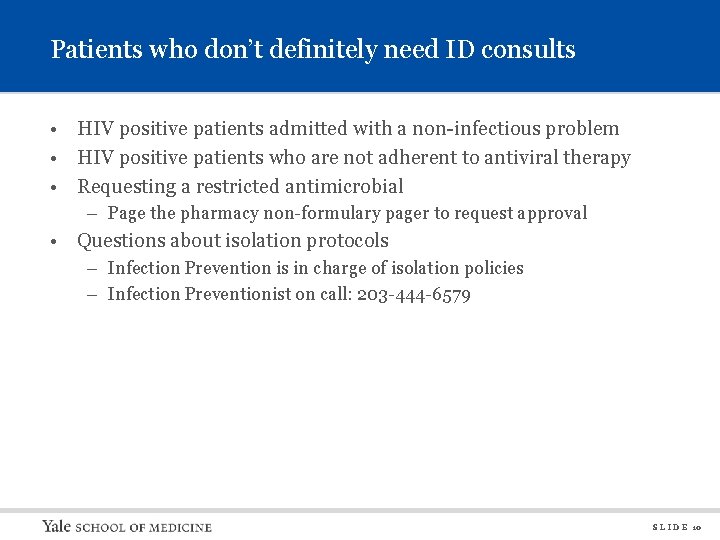
Patients who don’t definitely need ID consults • HIV positive patients admitted with a non-infectious problem • HIV positive patients who are not adherent to antiviral therapy • Requesting a restricted antimicrobial – Page the pharmacy non-formulary pager to request approval • Questions about isolation protocols – Infection Prevention is in charge of isolation policies – Infection Preventionist on call: 203 -444 -6579 S L I D E 10
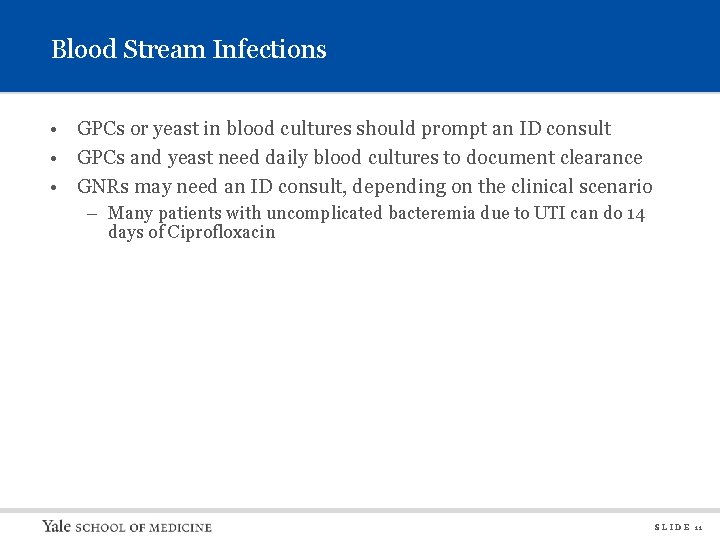
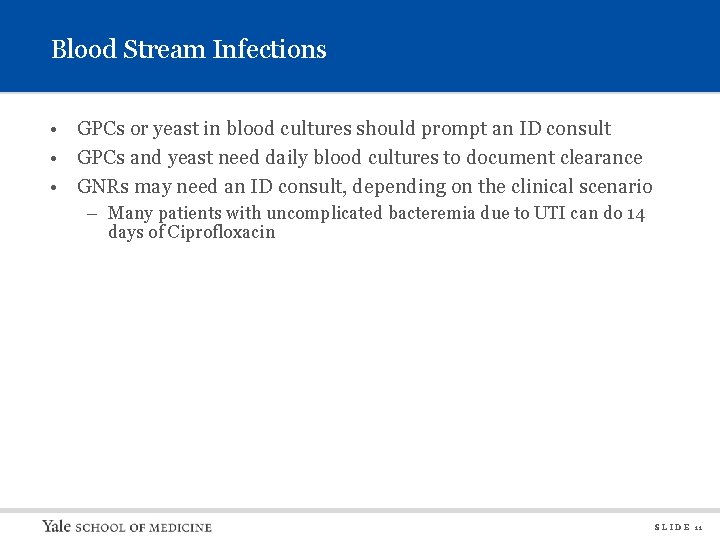
Blood Stream Infections • GPCs or yeast in blood cultures should prompt an ID consult • GPCs and yeast need daily blood cultures to document clearance • GNRs may need an ID consult, depending on the clinical scenario – Many patients with uncomplicated bacteremia due to UTI can do 14 days of Ciprofloxacin S L I D E 11
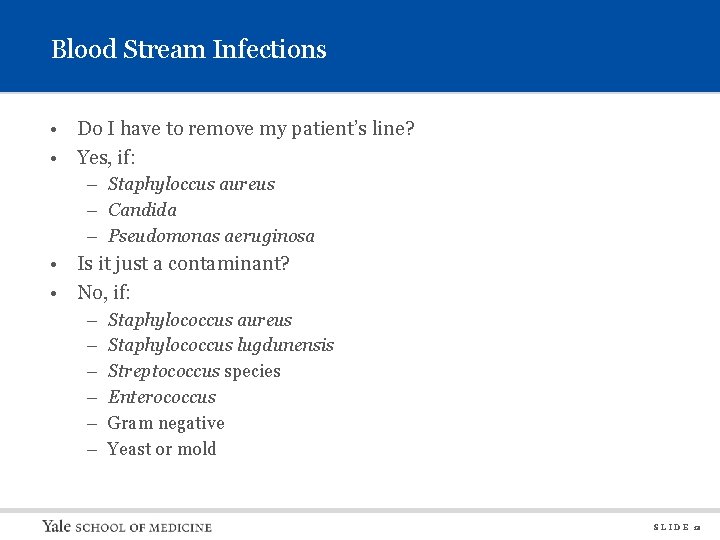
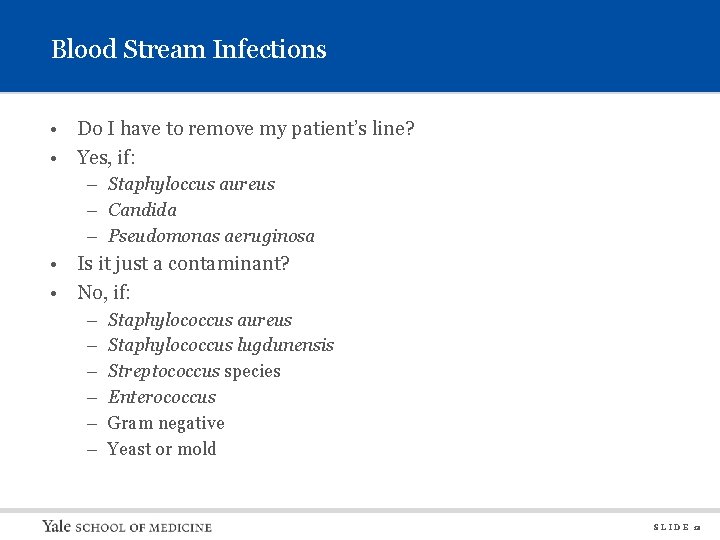
Blood Stream Infections • Do I have to remove my patient’s line? • Yes, if: – Staphyloccus aureus – Candida – Pseudomonas aeruginosa • Is it just a contaminant? • No, if: – – – Staphylococcus aureus Staphylococcus lugdunensis Streptococcus species Enterococcus Gram negative Yeast or mold S L I D E 12
Blood Stream Infections – Staph aureus bacteremia • • • MRSA and MSSA are both highly virulent Rapid PCR test helps rule Staph aureus in or out Patients with MSSA should be on oxacillin or cefazolin Do not treat with PO antibiotics Always consider metastatic sites of infection – Endocarditis – Septic joints – Vertebral osteomyelitis or epidural abscess • Consult ID! S L I D E 13
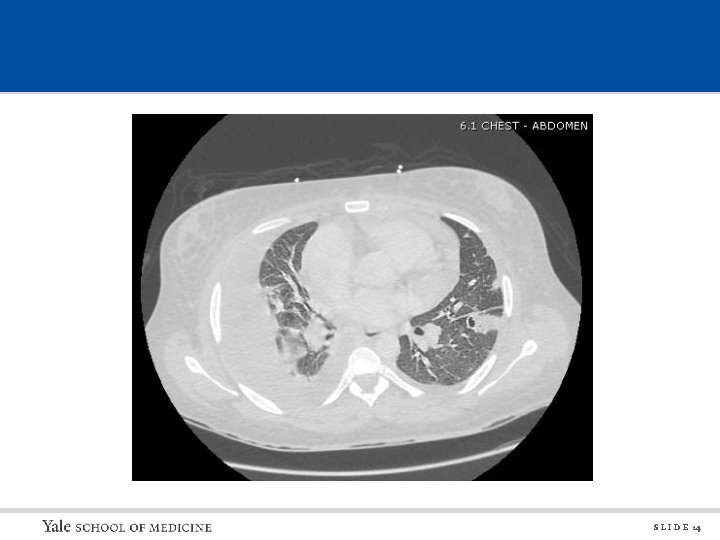
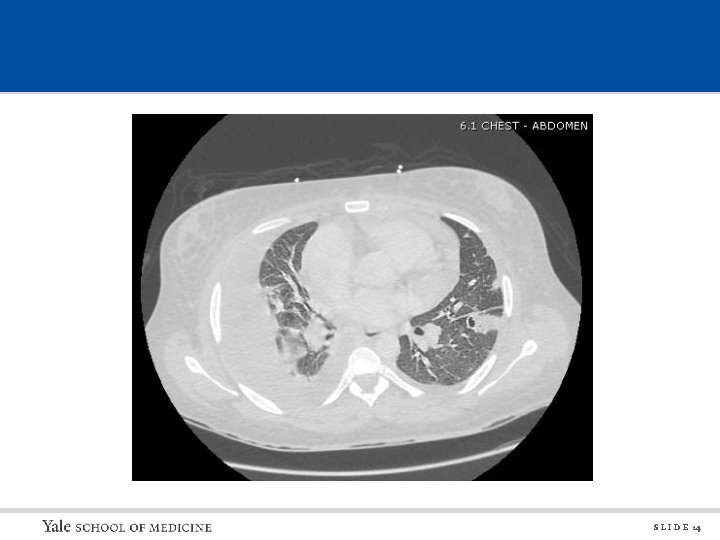
S L I D E 14

S L I D E 15
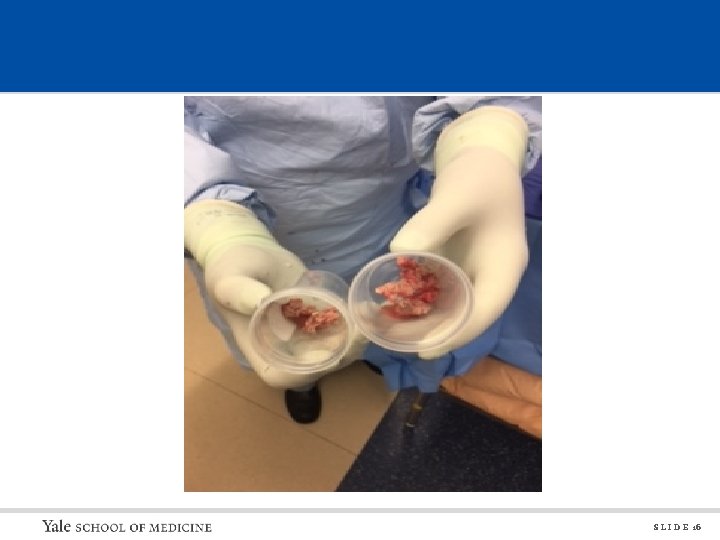
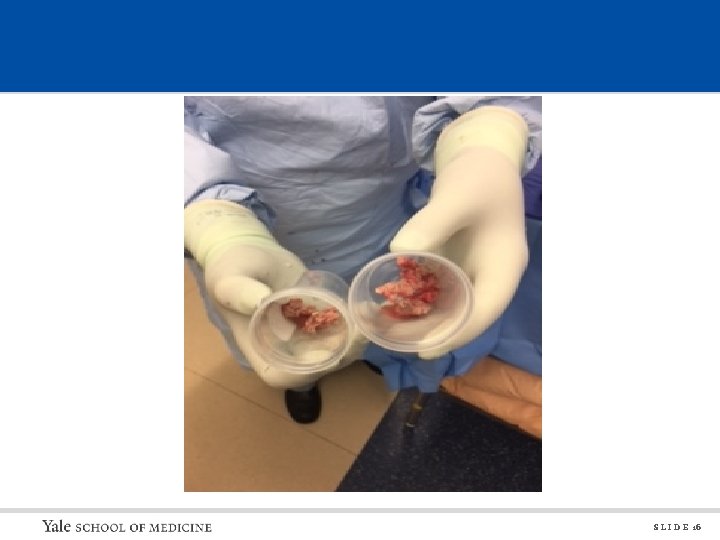
S L I D E 16

Osteomyelitis • Can be caused by hematogenous seeding of bone or direct inoculation – Vertebral osteomyelitis – usually hematogenous spread – Foot osteomyelitis – usually direct inoculation or tracking from wound – Sacral osteomyelitis – usually direct inoculation from stool • Whenever possible, we like to get a microbiologic diagnosis via bone biopsy • MRI is usually the best diagnostic study • Exposed bone is usually synonymous with chronic osteomyelitis • Initial treatment depends on patient’s clinical condition and physical exam S L I D E 17
Osteomyelitis • Does my patient need empiric antibiotics right away? • Often times patient can wait until bone biopsy to start treatment – Chronic wounds – Imaging finding of osteomyelitis without other signs/symptoms – Defer antibiotics whenever possible, so we get a better diagnosis • Yes, if: • Patient has signs of sepsis (fever, leukocytosis) • Patient has signs of skin/soft tissue infection or wound superinfection (redness, erythema, purulent drainage) • Patient has an abscess • Patient has positive blood cultures S L I D E 18
Osteomyelitis • What does a patient need to achieve a cure? • Adequate blood flow • Wound closure – Exposed bone will continue to be inoculated with bacteria • Appropriate surgical debridement – Devitalized or chronically infected bone will not heal well • Appropriate antibiotics – Typically 6 weeks of treatment – IV vs PO depends on whether we can use a highly bioavailable drug • Sometimes surgical resection is the most effective and definitive course of action S L I D E 19

S L I D E 20

S L I D E 21
Osteomyelitis – Take Away Points • If patient has no signs of soft tissue infection, abscess, or sepsis, then wait until cultures are obtained to start empiric antibiotics • Exposed bone almost always means osteomyelitis, but immediate antibiotics are not usually the answer • Consult ID! • Make sure other consultants are involved as needed – Podiatry – Surgery – Vascular Surgery or Peripheral Vascular Team S L I D E 22
Tick-Borne Diseases • Lyme Disease • Babesiosis • Anaplasmosis/Ehrlichiosis S L I D E 23
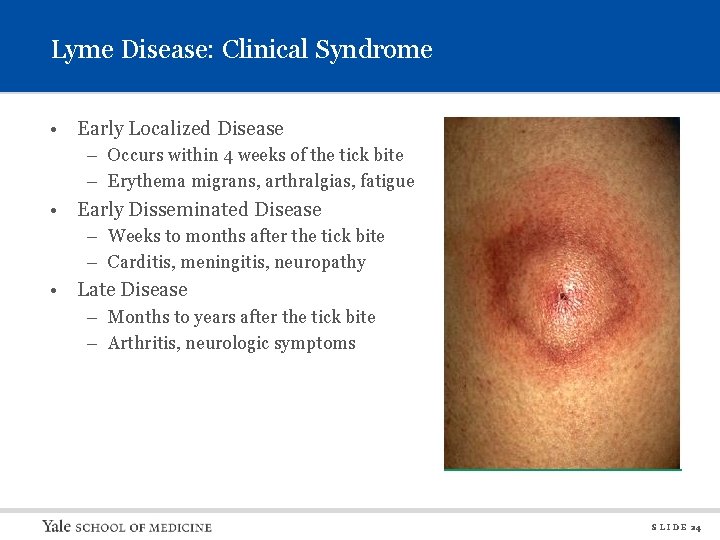
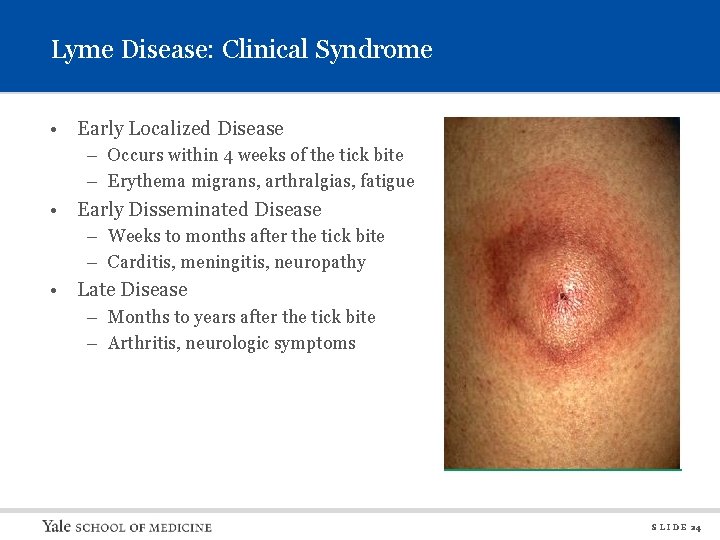
Lyme Disease: Clinical Syndrome • Early Localized Disease – Occurs within 4 weeks of the tick bite – Erythema migrans, arthralgias, fatigue • Early Disseminated Disease – Weeks to months after the tick bite – Carditis, meningitis, neuropathy • Late Disease – Months to years after the tick bite – Arthritis, neurologic symptoms S L I D E 24
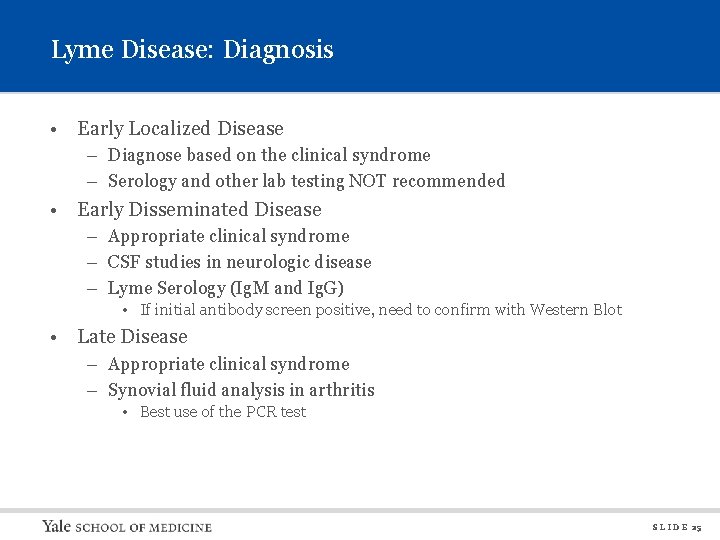
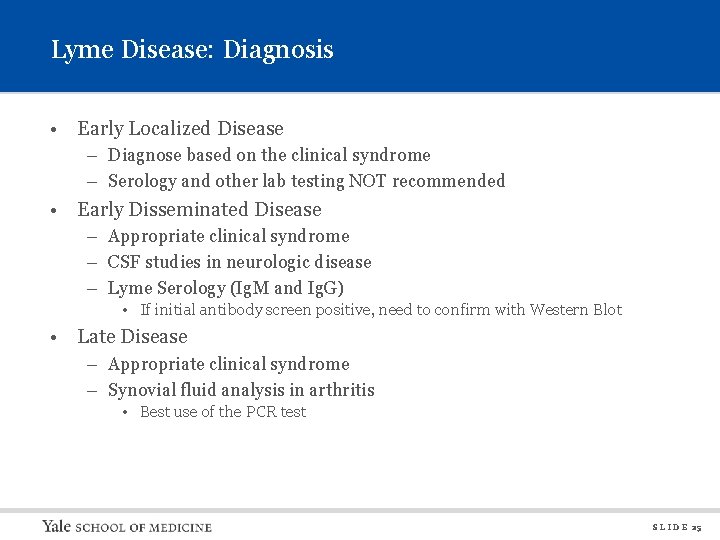
Lyme Disease: Diagnosis • Early Localized Disease – Diagnose based on the clinical syndrome – Serology and other lab testing NOT recommended • Early Disseminated Disease – Appropriate clinical syndrome – CSF studies in neurologic disease – Lyme Serology (Ig. M and Ig. G) • If initial antibody screen positive, need to confirm with Western Blot • Late Disease – Appropriate clinical syndrome – Synovial fluid analysis in arthritis • Best use of the PCR test S L I D E 25
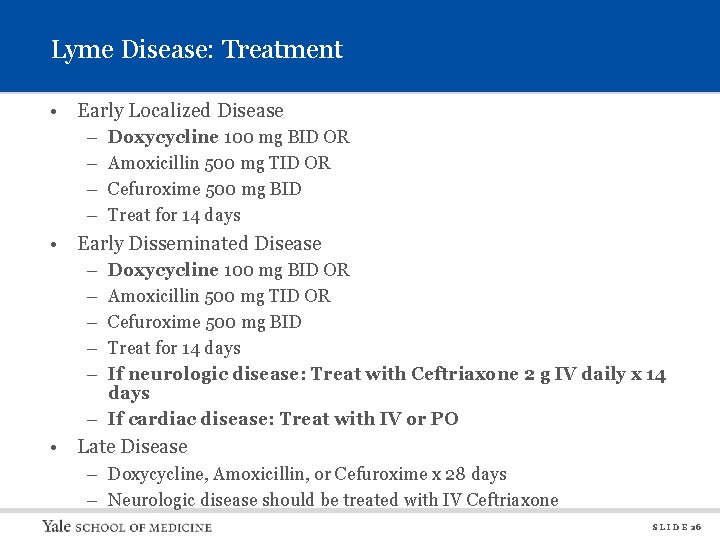
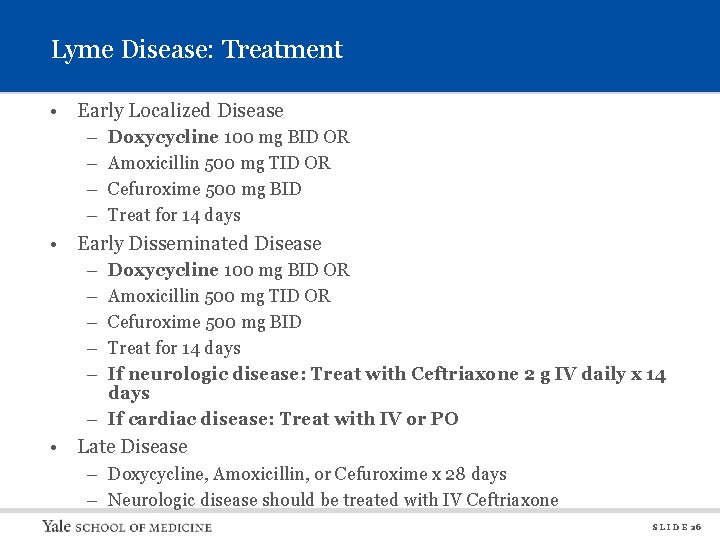
Lyme Disease: Treatment • Early Localized Disease – – Doxycycline 100 mg BID OR Amoxicillin 500 mg TID OR Cefuroxime 500 mg BID Treat for 14 days • Early Disseminated Disease – – – Doxycycline 100 mg BID OR Amoxicillin 500 mg TID OR Cefuroxime 500 mg BID Treat for 14 days If neurologic disease: Treat with Ceftriaxone 2 g IV daily x 14 days – If cardiac disease: Treat with IV or PO • Late Disease – Doxycycline, Amoxicillin, or Cefuroxime x 28 days – Neurologic disease should be treated with IV Ceftriaxone S L I D E 26
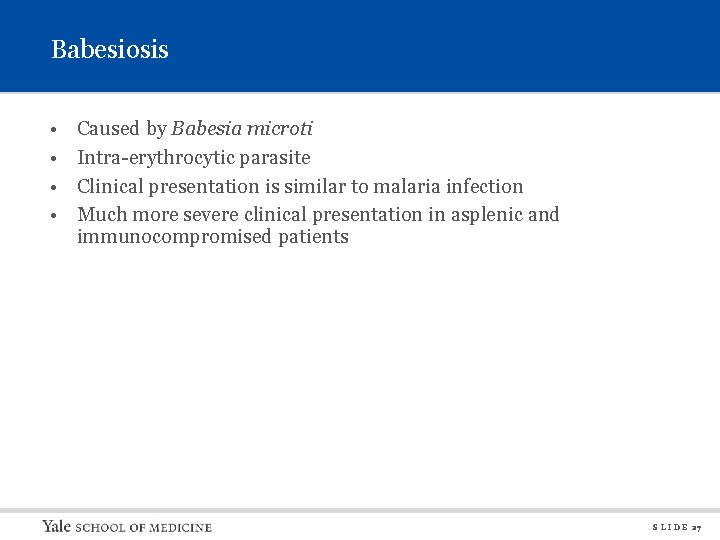
Babesiosis • • Caused by Babesia microti Intra-erythrocytic parasite Clinical presentation is similar to malaria infection Much more severe clinical presentation in asplenic and immunocompromised patients S L I D E 27
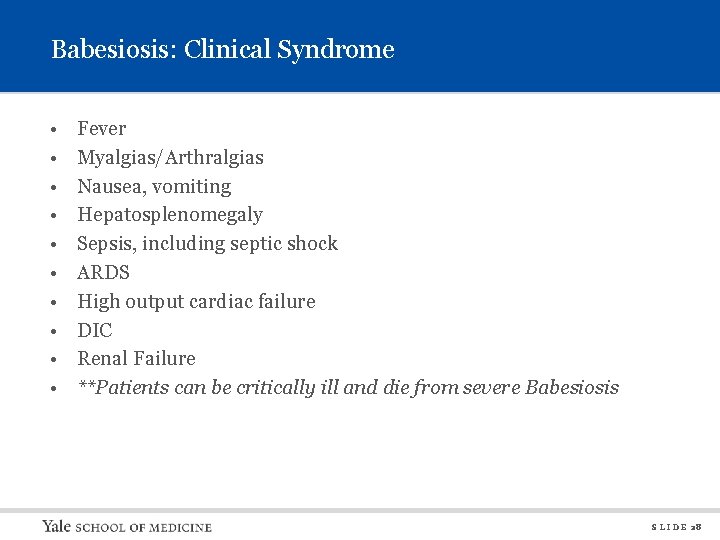
Babesiosis: Clinical Syndrome • • • Fever Myalgias/Arthralgias Nausea, vomiting Hepatosplenomegaly Sepsis, including septic shock ARDS High output cardiac failure DIC Renal Failure **Patients can be critically ill and die from severe Babesiosis S L I D E 28
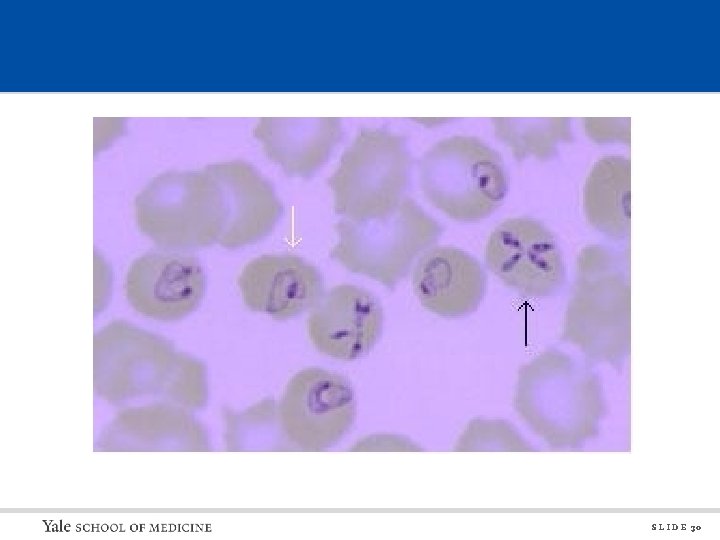
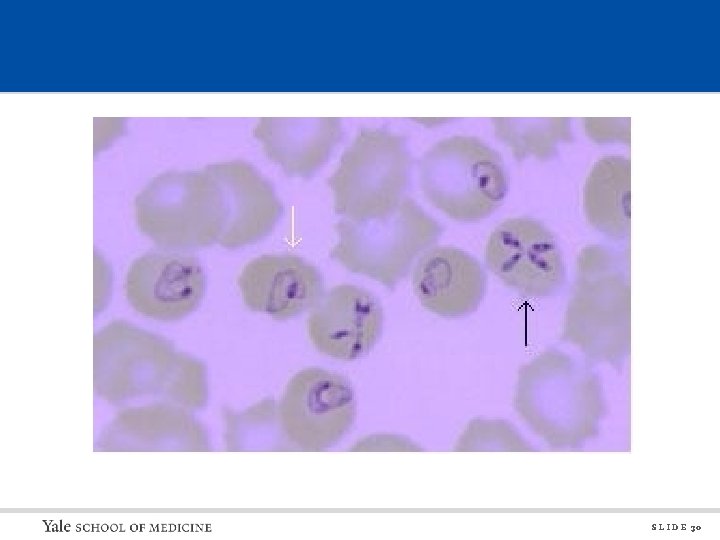
Babesia: Diagnosis • Intraerythrocytic Parasite – Hemolytic anemia – Jaundice • Thrombocytopenia • Hepatitis • Diagnosis is generally made by Babesia smear – Also gives a % parasitemia • Serology available but is less helpful • PCR testing is available but only slightly more sensitive than the smear S L I D E 29
S L I D E 30
Babesia: Treatment • Mild to Moderate Disease – Azithromycin and Atovaquone • Severe Disease – Clindamycin and Quinine • Duration of therapy is generally 7 -10 days • Exchange Transfusion – Done if % parasitemia is > 10% – Done if significant end organ compromise S L I D E 31
Anaplasmosis and Ehrlichiosis • Two different organisms with almost identical clinical syndromes • Anaplasma phagocytophilium – Causes Human Granulocytic Anaplasmosis – Transmitted by Ixodes scapularis (deer tick) • Ehrlichia chaffeensis – Causes Human Monocytic Ehrlichiosis – Transmitted by Amblyomma americanum (Lone Star Tick) • Anaplasma is the organism mainly seen in our geographic region S L I D E 32
Anaplasmosis: Clinical Syndrome • • • Fever and Chills Myalgias/Arthralgias Headache Nausea/Vomiting Rash – Rare – Macular, papular, petechial • Neurologic Manifestations – Rare – Altered mental status – Meningitis • Severity can range from mild febrile illness to severe illness with sepsis and multi-organ failure S L I D E 33
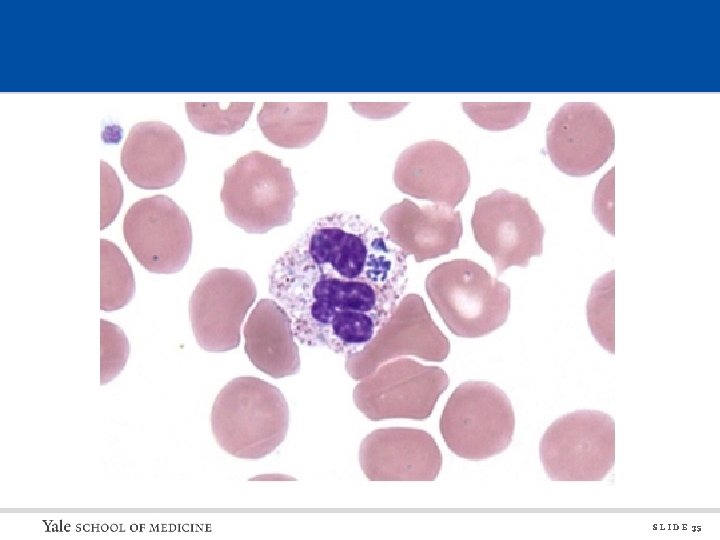
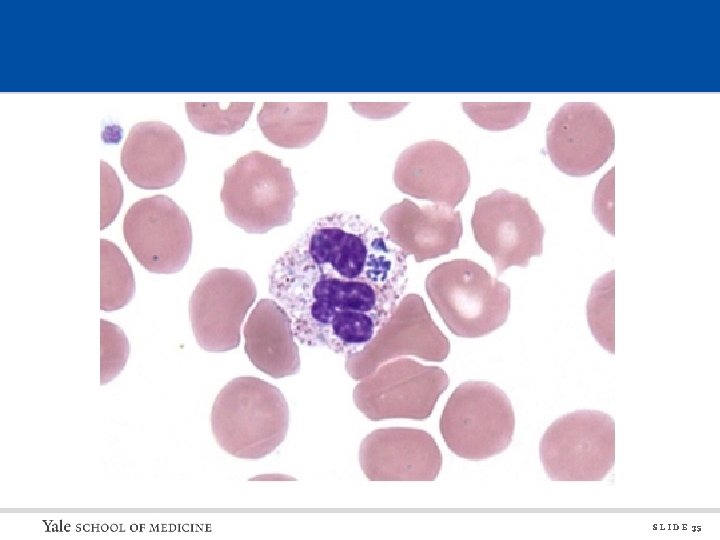
Anaplasmosis: Diagnosis • Intra-leukocytic organism • Laboratory Findings: – Leukopenia – Thrombocytopenia – Elevated transaminases (usually mild) • Smear is helpful only if positive, because it has very poor sensitivity • Serology is sensitive but has to be timed appropriately – Clinically can have limited utility • PCR is highly sensitive – If sent prior to treatment S L I D E 34
S L I D E 35
Anaplasmosis: Treatment • Doxycycline 100 mg BID x 10 days • Patients rapidly respond to treatment, and this is often helpful diagnostically (while waiting for lab tests). – Should defervesce within 24 -48 hours of starting doxycycline – If fail to improve within a couple of days, need to consider alternative diagnoses S L I D E 36
Tick Borne Diseases Take Home Points • Patients often do not recall having been bitten by a tick. • Patients can be co-infected with 2 or 3 of these diseases simultaneously. • If the patient is febrile/septic, think Anaplasma or Babesia before thinking about Lyme. • Best Diagnostic Tests Are: – Lyme: Serology (Antibody testing) – Babesia: Babesia smear (detection and quantitation) – Anaplasma/Ehrlichia: PCR testing • Doxycycline will cover all of these except for Babesia. S L I D E 37
Infectious Diseases Take Away Points • • Call consults early in the day! Please clearly delineate the question/reason for the consult Please consult for the “must see ID” diagnoses Pharmacy approves restricted antimicrobials Infection Prevention makes isolation policies If you’re not sure if your patient needs an ID consult, ask us Come rotate with us to learn how we approach infectious disease questions! S L I D E 38
Thank You! S L I D E 39
 Emerging infectious diseases
Emerging infectious diseases Certain infectious and parasitic diseases
Certain infectious and parasitic diseases Cvs to bvs
Cvs to bvs Shanna hayes
Shanna hayes Shana ross bayhealth
Shana ross bayhealth Till we meet till we meet at jesus feet
Till we meet till we meet at jesus feet Infectious canine hepatitis in dogs
Infectious canine hepatitis in dogs Lead poisoning
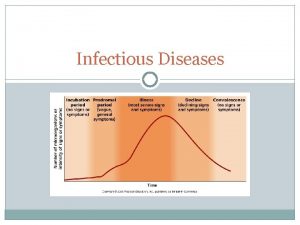
Lead poisoning Stages of infection
Stages of infection Hpps logo
Hpps logo Infectious disease board review
Infectious disease board review Infectious disease
Infectious disease Chapter 26 infectious disease prevention and control
Chapter 26 infectious disease prevention and control Noncellular infectious protein particles are called
Noncellular infectious protein particles are called Smallest infectious agent
Smallest infectious agent Infectious waste definition
Infectious waste definition Ebv
Ebv Stages of infectious disease
Stages of infectious disease Infectious stunting syndrome
Infectious stunting syndrome Infectious nucleic acid
Infectious nucleic acid Infectious canine hepatitis in dogs
Infectious canine hepatitis in dogs Infectious disease quality controls
Infectious disease quality controls Hennepin county infectious disease manual
Hennepin county infectious disease manual Chinchilla business consultant
Chinchilla business consultant Epicor configurator
Epicor configurator Consultant radiographer
Consultant radiographer Ph consultant
Ph consultant Jojy mathew
Jojy mathew Consultant contract 2003
Consultant contract 2003 Partner technical consultant
Partner technical consultant Rodan and fields tax write offs
Rodan and fields tax write offs Internet marketing consultant job description
Internet marketing consultant job description Nous hospital consultant
Nous hospital consultant Pgmdt
Pgmdt Knowledge management consultant
Knowledge management consultant New consultant training
New consultant training Behavioral genetics consultant
Behavioral genetics consultant Engineers pi is 3
Engineers pi is 3 Smita had been working as an assistant manager
Smita had been working as an assistant manager Stuart minty camden planning consultant
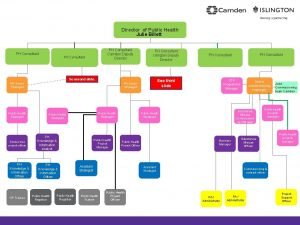
Stuart minty camden planning consultant Nutraceutical consultant
Nutraceutical consultant