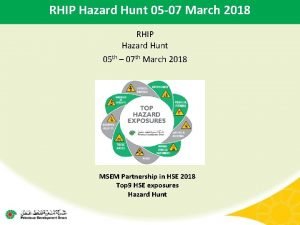
Maryland Rural Health Implementation Plan RHIP Michelle G




- Slides: 31
Maryland Rural Health Implementation Plan (RHIP) Michelle G. Clark, MSW, MPH Project Director, State Office of Rural Health October 2, 2008

Presentation Overview n n n Office of Health Policy and Planning (OHPP) State Office of Rural Health (SORH) Workforce Programs (Loan Assistance Repayment Program – LARP) Maryland Rural Health Plan MRHA Listening Sessions Maryland Rural Health Implementation Plan

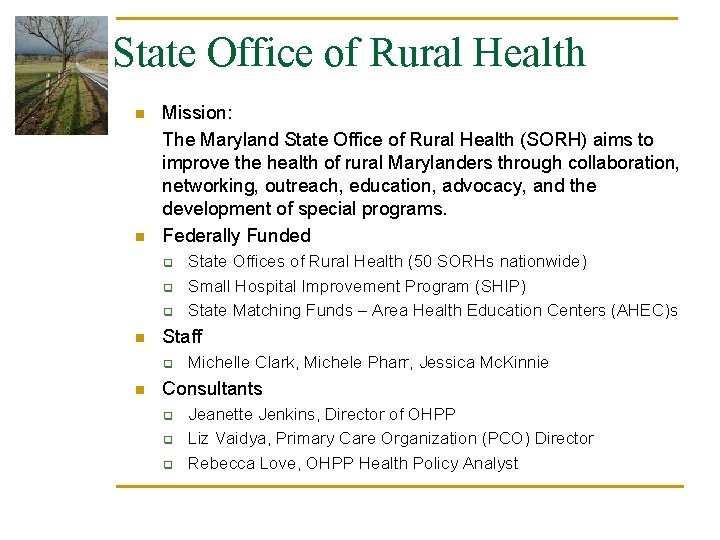
State Office of Rural Health n n Mission: The Maryland State Office of Rural Health (SORH) aims to improve the health of rural Marylanders through collaboration, networking, outreach, education, advocacy, and the development of special programs. Federally Funded q q q n Staff q n State Offices of Rural Health (50 SORHs nationwide) Small Hospital Improvement Program (SHIP) State Matching Funds – Area Health Education Centers (AHEC)s Michelle Clark, Michele Pharr, Jessica Mc. Kinnie Consultants q q q Jeanette Jenkins, Director of OHPP Liz Vaidya, Primary Care Organization (PCO) Director Rebecca Love, OHPP Health Policy Analyst
Workforce Programs Within OHPP Loan Assistance Repayment Program Federal Loan Assistance Repayment Program (LARP) § Purpose § To provide repayment of educational loans to physicians who agree to practice in an approved practice/underserved area for a period of time § Program is jointly administered by: § Primary Care Office (PCO) in the OHHP in Family Health Administration for DHMH § Maryland Higher Education Commission (MHEC)
Workforce Programs Within OHPP LARP Funding § Federal funds § § § Competitive funding among the states Requires state match (50: 50) State funds § § Source is physician licensure fees Funds provided to MD Higher Education Commission (MHEC) through legislatively mandated Janet L. Hoffman Program
Workforce Programs Within OHPP LARP Eligibility and Requirements Eligibility § Primarily for practicing physicians, but residents also allowed § Types of health professionals eligible § Currently only two physician specialties included – primary care and general psychiatrists Requirements § § § Only non-profits Federal funds for practice in a designated Health Professional Shortage Area only General funds may be used to fund state-only awards in state designated shortage areas


Is LARP effective at recruiting and retaining providers? n n Each year there are more applicants than funding One national study found that physicians serving obligations to state programs served in needier areas and remained longer in their practices (Pathman, Konrad, King, Taylor, and Koch, 2004) Another study found that 48 percent of students would be more likely to return to their home states if expanded loan repayment programs were available (Miller and Crittenden, 2001) In Maryland, of 24 providers who completed service between 2004 and 2006, 22 are still practicing
Workforce Programs Within OHPP n J-1 Visa Waiver Program q q n J-1 visa requires physicians with foreign nationalities to return to their home country for two years at the end of their medical training. The waiver is granted in exchange for the physician’s work in an underserved area for three years National Health Service Corp. q q Reviews sites’ eligibility per federal criteria Recommendations to NHSC of eligible sites for placement of eligible health professionals, but final decision is made by the federal government – HRSA in DHHS
Maryland Rural Health Plan http: //www. fha. state. md. us/ohpp/ruralhlth/pdf/DHMH_Rural_Health_Plan_07. pdf
Plan Goals n n n Raise awareness of rural health issues and strategies to address these issues (Vision) Assess the health status of Maryland’s rural residents relative to non-rural residents (health indicators for rural areas) Set forth an agenda to build state consensus on the Plan to gain funding and resource support
Rural Health Priority Areas n n Access to primary and specialty care and pharmacy services (availability of workforce and affordability) Behavioral health (mental health and addiction/substance abuse) Lifestyle issues (nutrition, obesity, wellness) Oral health
Priority Recommendations 1. Increase efforts to improve recruitment and retention of rural health providers 2. Establish preventive health centers in rural areas, especially in those areas lacking or underserved by Federally Qualified Health Centers 3. Increase accessibility to pharmaceuticals for low-income rural residents
Rural Health Plan in Action n Maryland Rural Health Association (MRHA) Listening Sessions - 7 Total q October 2007 – 3 on the Eastern Shore q December 2007 – 3 in Western Maryland q April 2008 – Southern Maryland n Disseminated results n Rural Health Steering Committee had 5 Meetings in last 6 months n Rural Health Implementation Plan (RHIP)
Listening Sessions n n n Recruitment & retention of rural health providers Comprehensive Electronic Medical Records Provider reimbursement Telehealth reimbursement Increase and efficiency of Loan Repayment for Rural Providers Primary preventive health services
Maryland Rural Health Implementation Goals 1. Increase Recruitment and Retention of Rural Health Care Providers 2. Expand Enhance telehealth to bring primary and specialty care to rural areas through technology 3. Provide preventive health education and resources in rural areas 4. Increased dental access to low income rural residents, especially the adult population 5. Establish preventive health centers in rural areas, especially those areas lacking or underserved by a Federally Qualified Health Center (FQHC)s 6. Improve healthcare access for the aging population through increased services in rural areas and training of health professionals 7. Increase access to Pharmaceuticals for low income rural residents 8. Support the development of a continuous, integrated systems of care for co-occurring disorders in rural communities
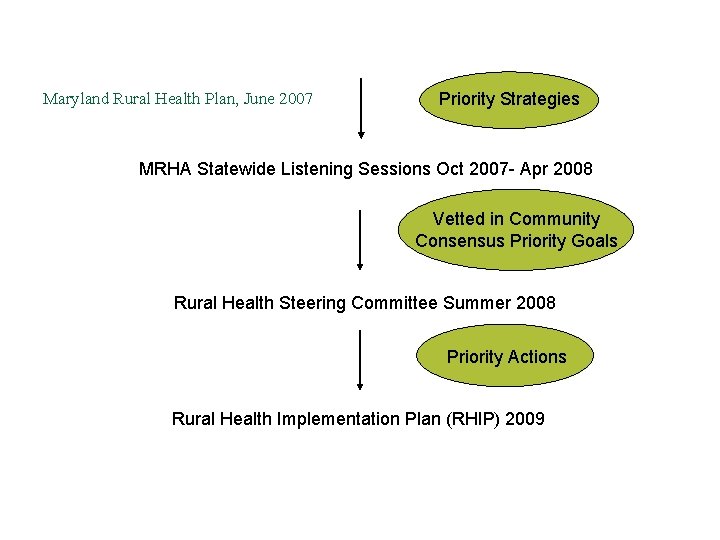
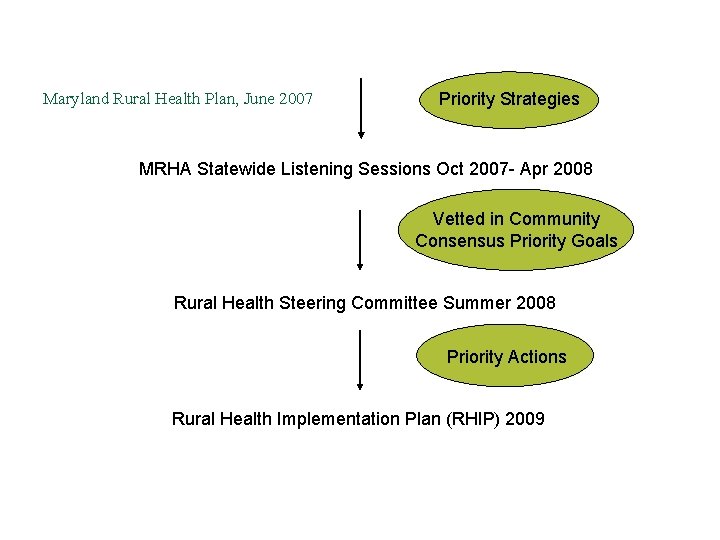
Maryland Rural Health Plan, June 2007 Priority Strategies MRHA Statewide Listening Sessions Oct 2007 - Apr 2008 Vetted in Community Consensus Priority Goals Rural Health Steering Committee Summer 2008 Priority Actions Rural Health Implementation Plan (RHIP) 2009
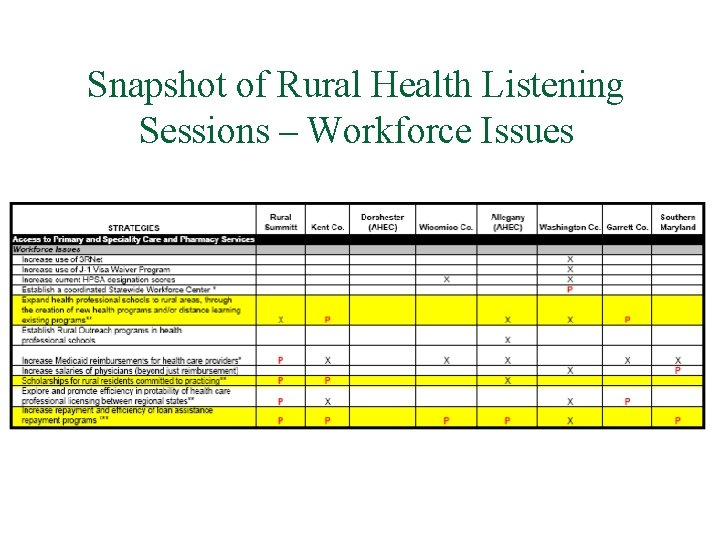
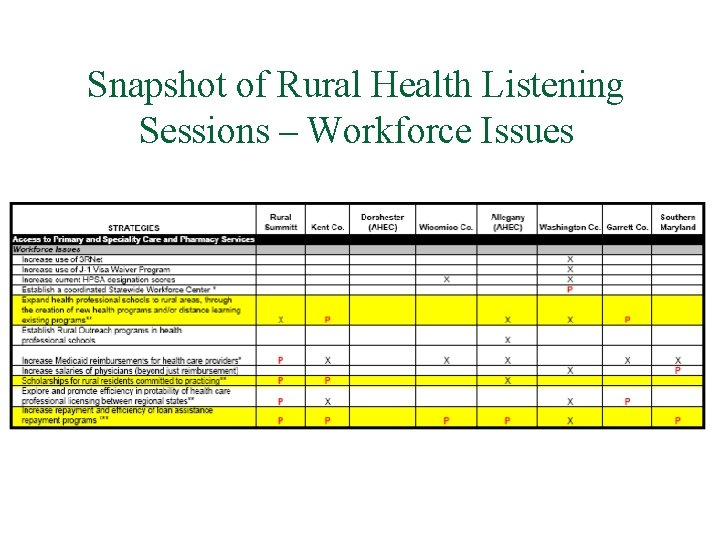
Snapshot of Rural Health Listening Sessions – Workforce Issues
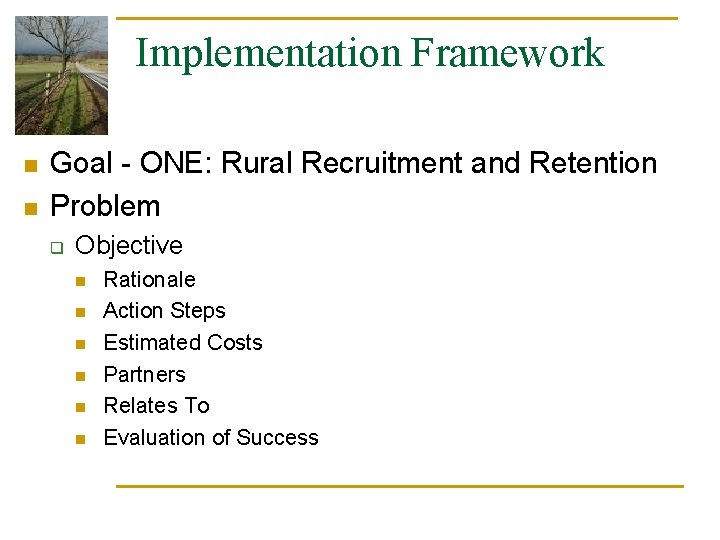
Implementation Framework n n Goal - ONE: Rural Recruitment and Retention Problem q Objective n n n Rationale Action Steps Estimated Costs Partners Relates To Evaluation of Success
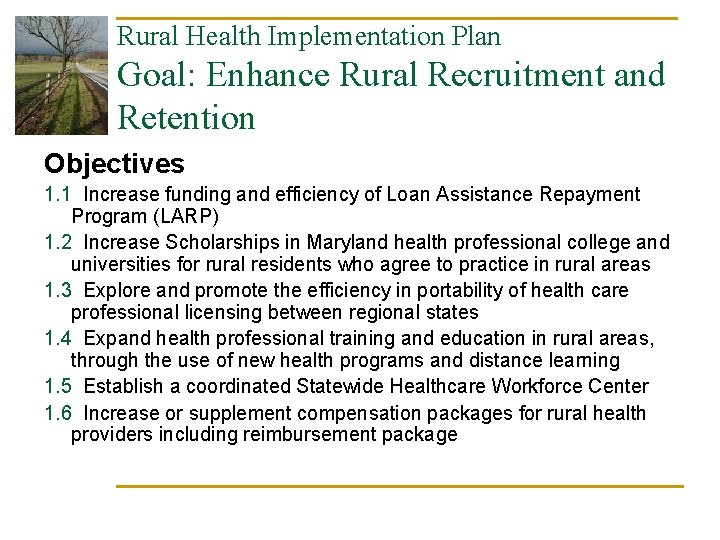
Rural Health Implementation Plan Goal: Enhance Rural Recruitment and Retention Objectives 1. 1 Increase funding and efficiency of Loan Assistance Repayment Program (LARP) 1. 2 Increase Scholarships in Maryland health professional college and universities for rural residents who agree to practice in rural areas 1. 3 Explore and promote the efficiency in portability of health care professional licensing between regional states 1. 4 Expand health professional training and education in rural areas, through the use of new health programs and distance learning 1. 5 Establish a coordinated Statewide Healthcare Workforce Center 1. 6 Increase or supplement compensation packages for rural health providers including reimbursement package
Objective 1. 1 Increase funding and efficiency of Loan Assistance Repayment Program (LARP) n n n Increase state funding for LARP for at least 20 years of additional loan repayment through legislation, physician fees, or hospital surcharges to allow more flexibility with the use of funds and program staff. Assess the needs of rural Maryland workforce shortages and identify those areas that do not qualify for a federally designated shortage area but are in need of physicians. Restructure Maryland physician LARP program to allow more flexibility with state funds and repayment in rural areas designated as Maryland Health Professional Shortage Areas.
Objective 1. 2 Increase scholarships in Maryland health professional colleges and universities for rural residents who agree to practice rural areas. n n Assess the number of rural Maryland students attending Maryland Graduate Schools in health professional programs. Create a Rural Health Scholarship Program that includes administrative and fiscal support for Maryland students committed to practicing in rural areas after training.
Objective 1. 3 Explore and promote the efficiency in portability of health care professional licensing between regional states n n Establish partnerships with other regional states adjoining Maryland to specifically address the need to have more portable licenses. In coordination with neighboring states, identify the capacity of health professionals who practice in more the one state and serve rural populations.
Objective 1. 4 Expand health professional training and education in rural areas, through the use of new health programs and distance learning n n n Assess professional schools that have expanded to serve rural areas and identify best practices and models for the potential to be replicated across the state. Explore opportunities to create new health professional programs in rural areas. Encourage and fund distance learning capabilities of health professional schools to expand scope training available for of students in rural areas.
Objective 1. 5 Establish a coordinated Statewide Healthcare Workforce Center n n Build upon workforce shortage areas to determine specific healthcare shortages Develop a statewide healthcare workforce center with all agencies involvement to serve as hub for q q q Healthcare workforce programs (including marketing of programs) AHECs Educate healthcare providers & employers regarding recruitment strategies
Objective 1. 6 Increase or supplement compensation packages for rural health providers including reimbursement package n n Increase state Medicaid payments to providers in designated health professional shortage areas similar to the CMS Medicare incentive payment Provide tax incentives to rural providers working within health professional shortage areas
Questions/Comments!
Contact Information n Michelle Clark, MSW, MPH, Project Director, State Office of Rural Health, Office of Health Policy and Planning q n Michele Pharr, MA, Health Policy Analyst, State Office of Rural Health, Office of Health Policy and Planning q n mclark@dhmh. state. md. us; 410 -767 -5121 mpharr@dhmh. state. md. us; 410 -767 -3543 http: //www. fha. state. md. us/ohpp/ruralhlth/
References Miller, JB and Crittenden, RA. (2001) “The effects of payback and loan repayment programs on medical student career plans. ” Journal of Rural Health, 17(3): 160 -164. Pathman, DE, Konrad, TR, Taylor, DH Jr. , and Koch, GG. (2004) “Outcomes of states’ scholarships, loan repayment, and related programs for physicians. ” Medical Care, 42(6): 560 -568.
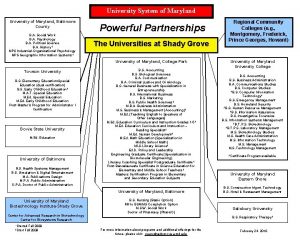
 University of maryland capital region health medical group
University of maryland capital region health medical group Maryland health connection
Maryland health connection Colorado physicians health program
Colorado physicians health program Logan ahs
Logan ahs Maryland health services cost review commission
Maryland health services cost review commission Mchrc
Mchrc Maryland health enterprise zones
Maryland health enterprise zones Crisp health information exchange
Crisp health information exchange Mental health policy, plans and programmes michelle funk
Mental health policy, plans and programmes michelle funk Palominas rural clinic
Palominas rural clinic Behavioral health alliance of rural pennsylvania
Behavioral health alliance of rural pennsylvania Albany area primary health care dental
Albany area primary health care dental Minnesota rural health association
Minnesota rural health association Rural health care
Rural health care National rural health mission
National rural health mission Rural health clinic coding
Rural health clinic coding Medicare rural health clinic billing
Medicare rural health clinic billing Rural health
Rural health National association of rural health clinics
National association of rural health clinics Assessment planning implementation and evaluation
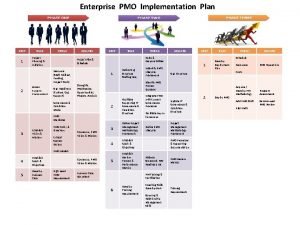
Assessment planning implementation and evaluation Strategic implementation plan
Strategic implementation plan Siem
Siem Swot analysis of school improvement plan
Swot analysis of school improvement plan Isms implementation project plan
Isms implementation project plan Iso 14001 implementation project plan
Iso 14001 implementation project plan Itil implementation plan
Itil implementation plan Office 365 implementation steps
Office 365 implementation steps Intune deployment planning, design and implementation guide
Intune deployment planning, design and implementation guide Power bi implementation plan
Power bi implementation plan Identifying a lease
Identifying a lease Enterprise implementation plan
Enterprise implementation plan Efficient master data management strategy
Efficient master data management strategy