Mapping the Clinicopathologic and Molecular Genetic Evolution of
- Slides: 15
Mapping the Clinicopathologic and Molecular Genetic Evolution of Cutaneous T-Cell Lymphoma Peter Louis 1, Michael Berger Ph. D 1, Rose Brannon Ph. D 1, Helen Won 1, Christiane Querfeld MD PHD 2, Steven Horwitz MD 2, Patricia L. Myskowski MD 2, Melissa Pulitzer MD 1 Department of Pathology 1 and Department of Medicine 2 Memorial Sloan Kettering Cancer Center
Purpose The aim of this study is to determine if there is molecular genetic heterogeneity within chronologically and spatially distinct lesions of patients with Cutaneous T-Cell Lymphoma (CTCL), and to compare any such changes with clinical and pathologic characteristics.
Background � CTCL is a rare but potentially lethal malignancy of skin-homing T-lymphocytes. � The annual incidence of CTCL in the United States is between 4 -8 per 1, 000 persons � Mycosis Fungoides (MF) is the most prevalent subset of CTCL, accounting for over 50% of cases � While the overall mortality of MF is low, at approximately 100 deaths per year, patients with tumor stage disease have a 5 -year disease specific survival of 30% � Currently, there is no curative therapy for patients with advanced stage MF
Background · Little is known in specific cancers, if genetic and epigenetic changes are conserved throughout the chronologic or spatial progression of a tumor · Recent data suggests that mutational intratumoral heterogeneity may be greater than expected · In this context, our objective is to evaluate sequential and spatially distinct specimens from select MF patients, in order to evaluate the molecular evolution of their tumors, and to relate genetic findings with clinical and pathologic features.
Background � Patch stage lesions are typically thin, non-infiltrated, pink, and slightly scaly. The sites of predilections are the sun-protected areas such as the buttocks. � Plaque stage lesions are generally flat, indurated and elevated above the skin surface. Any area of the body surface may be involved. � Tumor stage MF most commonly presents as nodules. � Erythrodermic MF presents as widespread erythema. � Lymph node and visceral involvement, as well as large cell transformation, usually occur in the late stage of the disease.
Study Design • We identified patients with a clinicopathologic diagnosis of advanced stage MF, confirmed by review of clinical records, and by examination of pathology slides and reports • Seven patients were selected, who had in-house normal control tissue and sequential and/or synchronous biopsies of MF in skin and/or lymph node tissue. • Clinical and pathologic data, including demographics, immunophenotypic, and molecular findings were recorded. • Formalin-fixed paraffin embedded (FFPE) tumor tissues and normal controls were obtained from the MSKCC pathology archive • Genomic DNA was extracted from FFPE tissue sections using standard methods. Samples were analyzed for the presence of somatic point mutations, small indels and copy number alterations using publicly available algorithms survival, histologic,
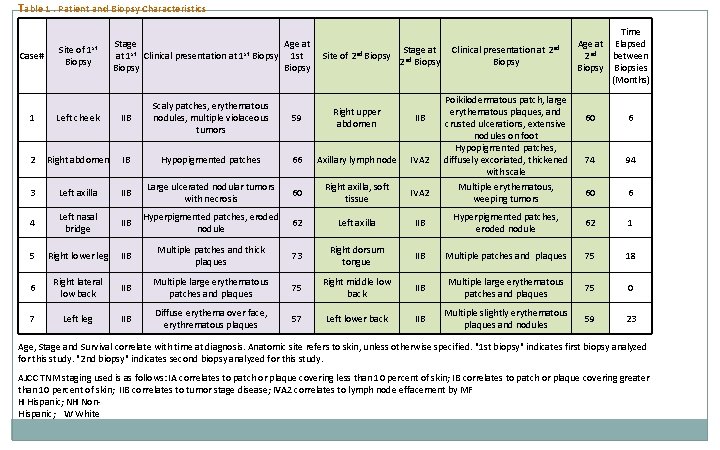
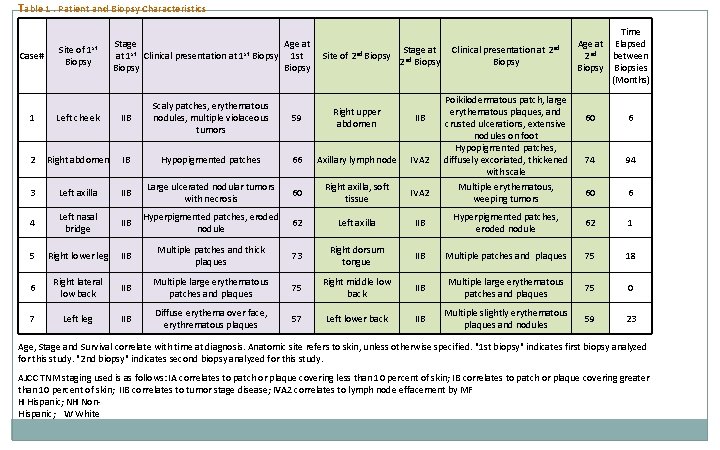
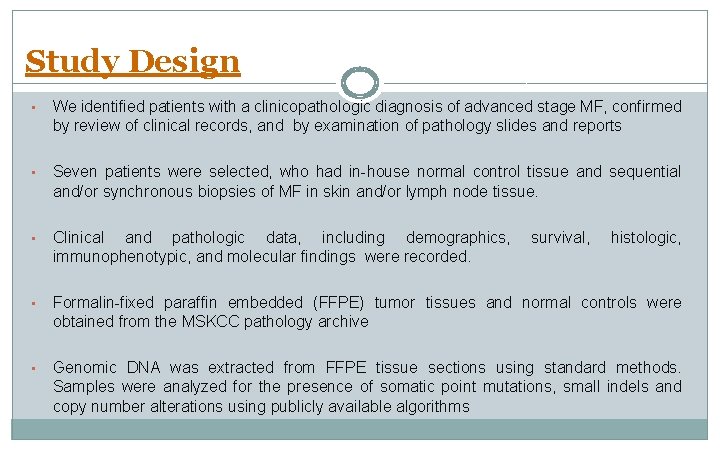
Table 1. Patient and Biopsy Characteristics Site of 1 st Biopsy Stage Age at at 1 st Clinical presentation at 1 st Biopsy Site of 2 nd Biopsy 1 Left cheek IIB Scaly patches, erythematous nodules, multiple violaceous tumors 59 Right upper abdomen IIB 2 Right abdomen IB Hypopigmented patches 66 Axillary lymph node IVA 2 3 Left axilla IIB Large ulcerated nodular tumors with necrosis 60 Right axilla, soft tissue IVA 2 4 Left nasal bridge IIB Hyperpigmented patches, eroded nodule 62 Left axilla 5 Right lower leg IIB Multiple patches and thick plaques 73 6 Right lateral low back IIB Multiple large erythematous patches and plaques 7 Left leg IIB Diffuse erythema over face, erythrematous plaques Case# Stage at 2 nd Biopsy Clinical presentation at 2 nd Biopsy Poikilodermatous patch, large erythematous plaques, and crusted ulcerations, extensive nodules on foot Hypopigmented patches, diffusely excoriated, thickened with scale Time Age at Elapsed 2 nd between Biopsy Biopsies (Months) 60 6 74 94 Multiple erythematous, weeping tumors 60 6 IIB Hyperpigmented patches, eroded nodule 62 1 Right dorsum tongue IIB Multiple patches and plaques 75 18 75 Right middle low back IIB Multiple large erythematous patches and plaques 75 0 57 Left lower back IIB Multiple slightly erythematous plaques and nodules 59 23 Age, Stage and Survival correlate with time at diagnosis. Anatomic site refers to skin, unless otherwise specified. "1 st biopsy" indicates first biopsy analyzed for this study. "2 nd biopsy" indicates second biopsy analyzed for this study. AJCC TNM staging used is as follows: IA correlates to patch or plaque covering less than 10 percent of skin; IB correlates to patch or plaque covering greater than 10 percent of skin; IIB correlates to tumor stage disease; IVA 2 correlates to lymph node effacement by MF H Hispanic; NH Non. Hispanic; W White
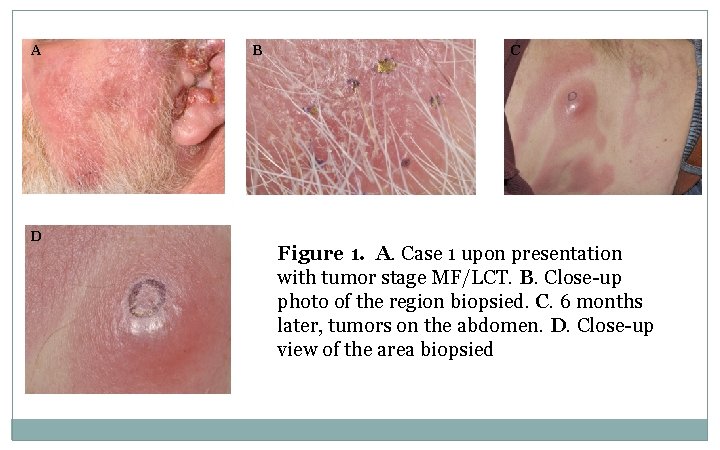
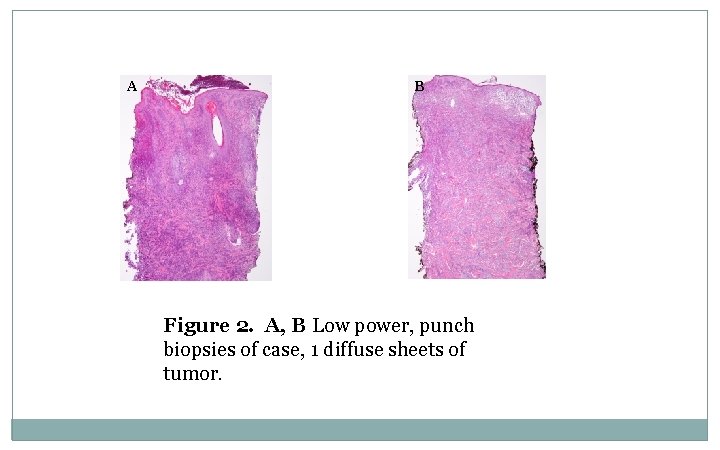
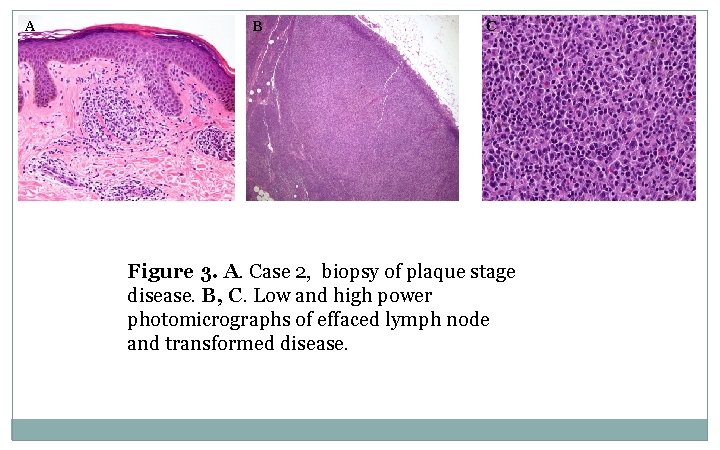
A D B C Figure 1. A. Case 1 upon presentation with tumor stage MF/LCT. B. Close-up photo of the region biopsied. C. 6 months later, tumors on the abdomen. D. Close-up view of the area biopsied
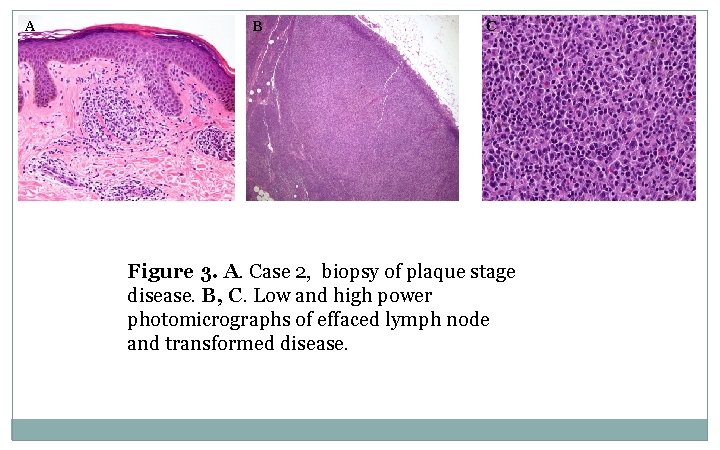
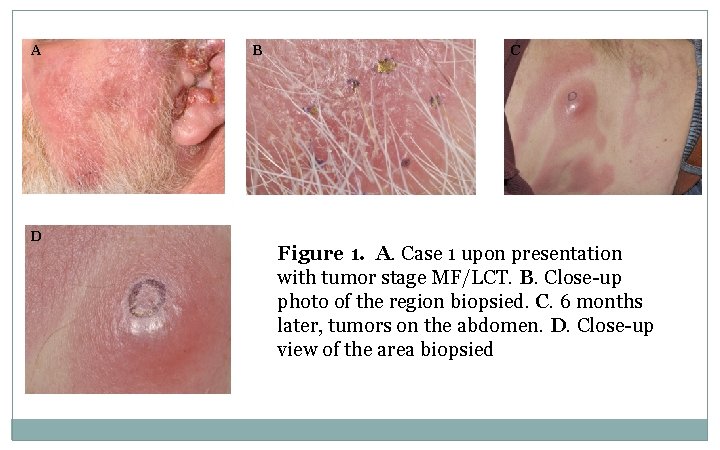
A B Figure 2. A, B Low power, punch biopsies of case, 1 diffuse sheets of tumor.
A B C Figure 3. A. Case 2, biopsy of plaque stage disease. B, C. Low and high power photomicrographs of effaced lymph node and transformed disease.
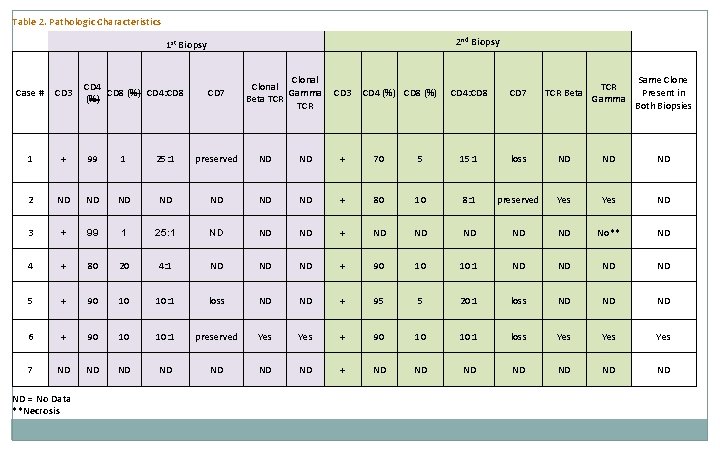
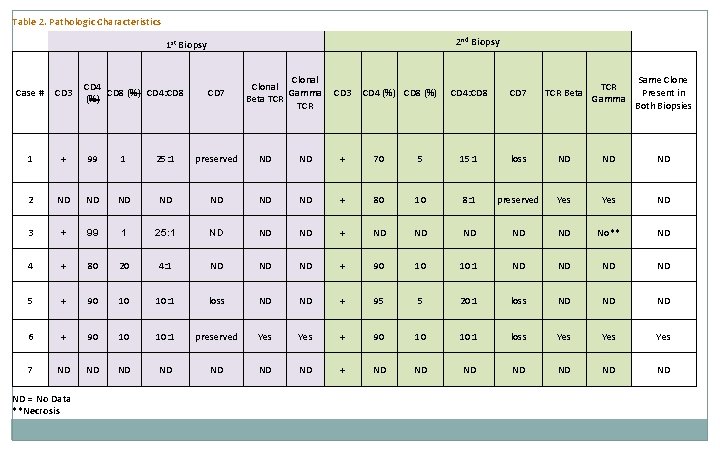
Table 2. Pathologic Characteristics 2 nd Biopsy 1 st Biopsy CD 4 CD 8 (%) CD 4: CD 8 (%) Case # CD 3 1 + 99 1 25: 1 preserved ND ND + 70 2 ND ND + 3 + 99 1 25: 1 ND ND ND 4 + 80 20 4: 1 ND ND 5 + 90 10 10: 1 loss 6 + 90 10 10: 1 7 ND ND ND = No Data **Necrosis CD 7 Clonal Gamma Beta TCR CD 3 CD 4 (%) CD 8 (%) TCR Beta Gamma Same Clone Present in Both Biopsies CD 4: CD 8 CD 7 5 15: 1 loss ND ND ND 80 10 8: 1 preserved Yes ND + ND ND ND No** ND ND + 90 10 10: 1 ND ND ND + 95 5 20: 1 loss ND ND ND preserved Yes + 90 10 10: 1 loss Yes Yes ND ND ND + ND ND
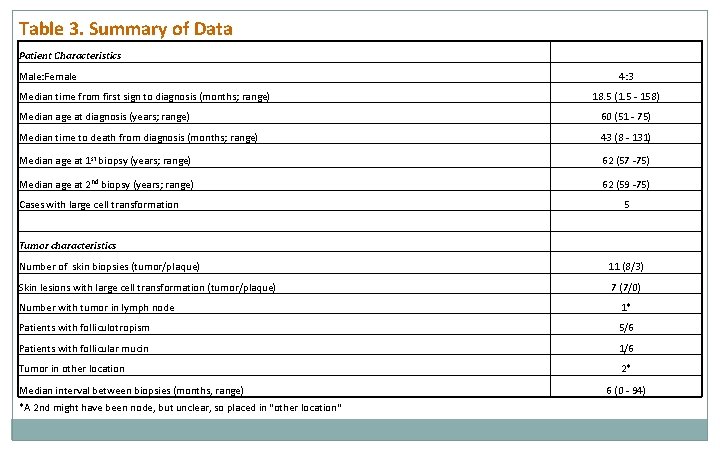
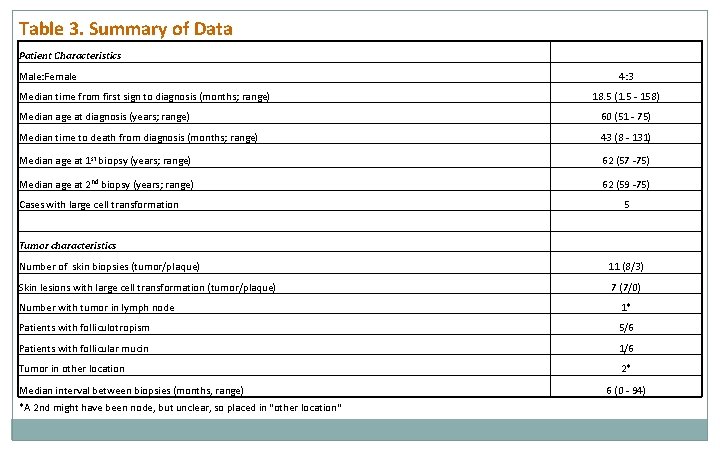
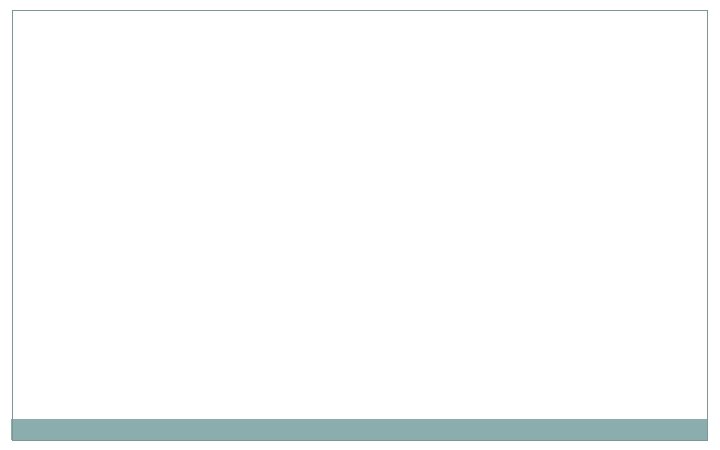
Table 3. Summary of Data Patient Characteristics Male: Female Median time from first sign to diagnosis (months; range) 4: 3 18. 5 (1. 5 - 158) Median age at diagnosis (years; range) 60 (51 - 75) Median time to death from diagnosis (months; range) 43 (8 - 131) Median age at 1 st biopsy (years; range) 62 (57 -75) Median age at 2 nd biopsy (years; range) 62 (59 -75) Cases with large cell transformation 5 Tumor characteristics Number of skin biopsies (tumor/plaque) 11 (8/3) Skin lesions with large cell transformation (tumor/plaque) 7 (7/0) Number with tumor in lymph node 1* Patients with folliculotropism 5/6 Patients with follicular mucin 1/6 Tumor in other location 2* Median interval between biopsies (months, range) *A 2 nd might have been node, but unclear, so placed in "other location" 6 (0 - 94)
Conclusions/Future Directions • Evolution of CTCL in our patients was characterized in part by clinical, histologic, and immunophenotypic changes, however, these changes are not consistent or predictable • We await the findings of our targeted mutational analysis to see if conservation or evolution of cancer-related mutations in CTCL better characterize progression of disease.
References 1. Zackheim, H. S. (2005). Cutaneous T-cell lymphoma : Mycosis Fungoides and Se zary syndrome. Boca Raton, Fla. , CRC Press. 2. Quaglino P, Pimpinelli N, Berti E, et al. Time course, clinical pathways, and long-term hazards risk trends of disease progression in patients with classic mycosis fungoides: A multicenter, retrospective follow-up study from the Italian Group of Cutaneous Lymphomas. Cancer. Jun 6 2012.