LARGE INTESTINE 2 ND YEAR ANATOMY LECTURE Dr
- Slides: 23
LARGE INTESTINE 2 ND YEAR ANATOMY LECTURE Dr Abeera Sarfraz/Dr Muhammad Zubair
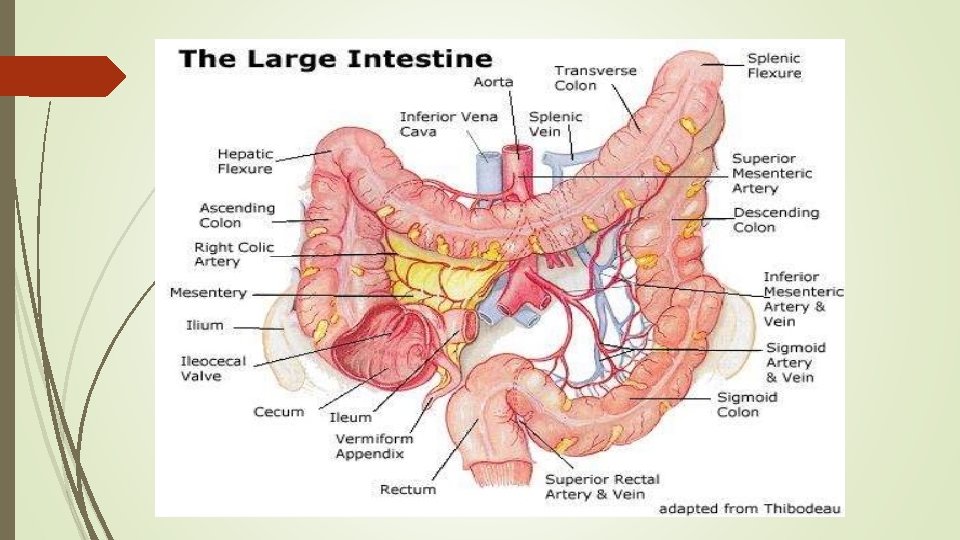
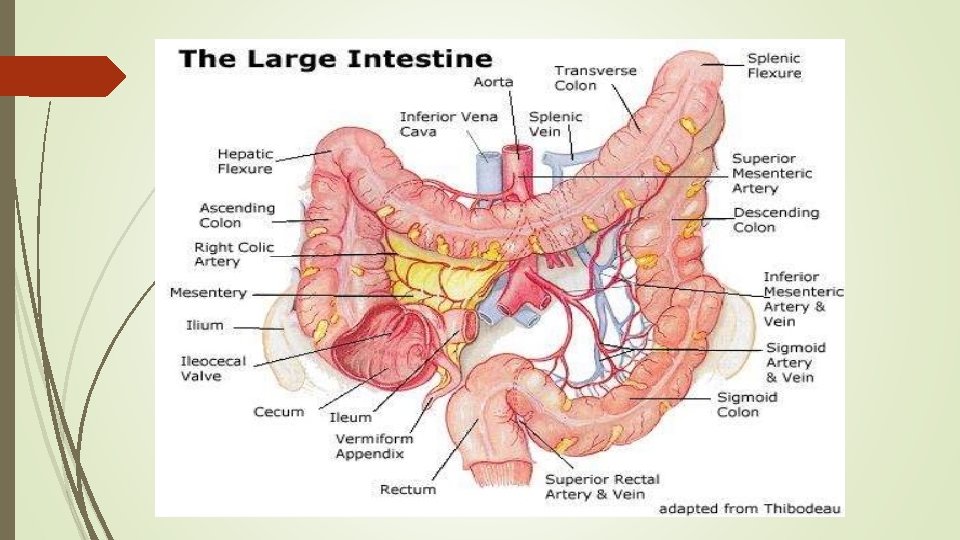
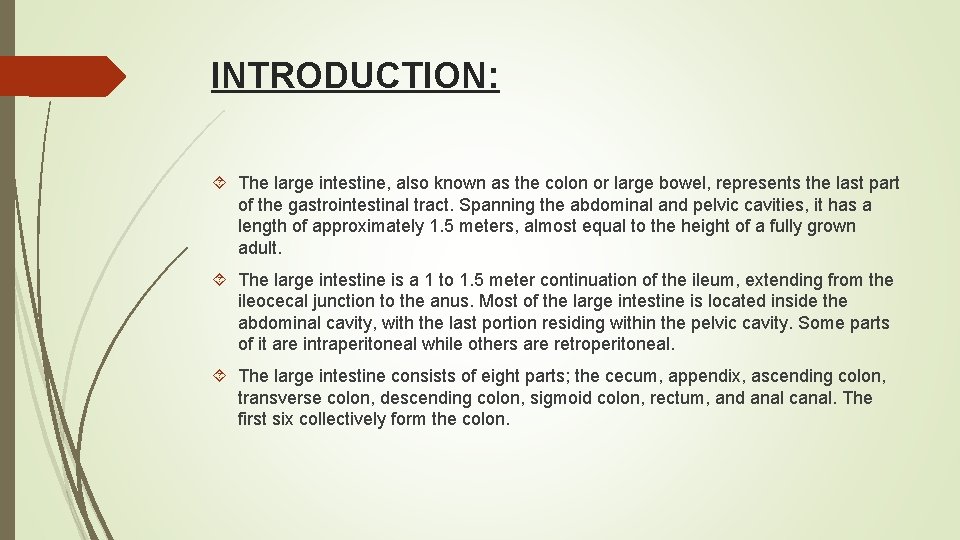
INTRODUCTION: The large intestine, also known as the colon or large bowel, represents the last part of the gastrointestinal tract. Spanning the abdominal and pelvic cavities, it has a length of approximately 1. 5 meters, almost equal to the height of a fully grown adult. The large intestine is a 1 to 1. 5 meter continuation of the ileum, extending from the ileocecal junction to the anus. Most of the large intestine is located inside the abdominal cavity, with the last portion residing within the pelvic cavity. Some parts of it are intraperitoneal while others are retroperitoneal. The large intestine consists of eight parts; the cecum, appendix, ascending colon, transverse colon, descending colon, sigmoid colon, rectum, and anal canal. The first six collectively form the colon.
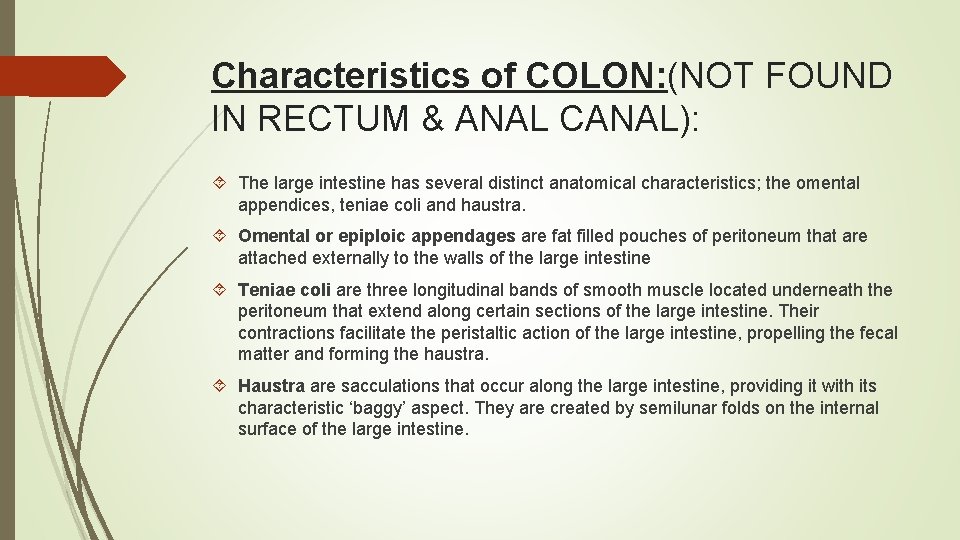
Characteristics of COLON: (NOT FOUND IN RECTUM & ANAL CANAL): The large intestine has several distinct anatomical characteristics; the omental appendices, teniae coli and haustra. Omental or epiploic appendages are fat filled pouches of peritoneum that are attached externally to the walls of the large intestine Teniae coli are three longitudinal bands of smooth muscle located underneath the peritoneum that extend along certain sections of the large intestine. Their contractions facilitate the peristaltic action of the large intestine, propelling the fecal matter and forming the haustra. Haustra are sacculations that occur along the large intestine, providing it with its characteristic ‘baggy’ aspect. They are created by semilunar folds on the internal surface of the large intestine.
PERITONEAL ATTACHMENTS: The transverse and sigmoid colon are completely peritonealized, hanging onto the transverse and the sigmoid mesocolon respectively. The transverse colon is readily identified by its attachment, along its free border, to the greater omentum. In contrast, the ascending and descending colons adhere to the peritoneum of the posterior abdominal wall. This adhesion is avascular, and enables the surgeon easily to mobilize these parts of the large bowel. The caecum is usually completely peritonealized, as may occasionally be the commencement of the ascending colon. The appendix usually hangs free on its own mesentery, although it may tuck itself extraperitoneally behind the ascending colon or adhere to the back of the caecum.
PARTS WITH MESENTERY: Transverse colon Sigmoid colon Appendix Cecum RETROPERITONEAL PARTS: Ascending colon Descending colon 3. Upper 2/3 of rectum PARTS DEVOID OF PERITONEAL COVERING: Lower 1/3 of rectum Anal canal
CECUM: The cecum is the first part of the large intestine, lying in the right iliac fossa of the abdomen. The cecum is intraperitoneal with various folds and pockets (retrocecal peritoneal recesses) surrounding it. The terminal ileum joins the cecum at the ileocolic junction. The ileocecal orifice is marked by the ileal papilla, which consists of two folds called ileocecal lips (superior, inferior). The folds fuse together around the orifice, forming the frenula of the ileal orifice, which prevents reflux of cecal contents into the ileum. An ileocecal valve regulates the passage of intestinal contents from the small into the large intestine. The functions of the cecum involve temporary storage of chyme, and fluid and electrolyte reabsorption.
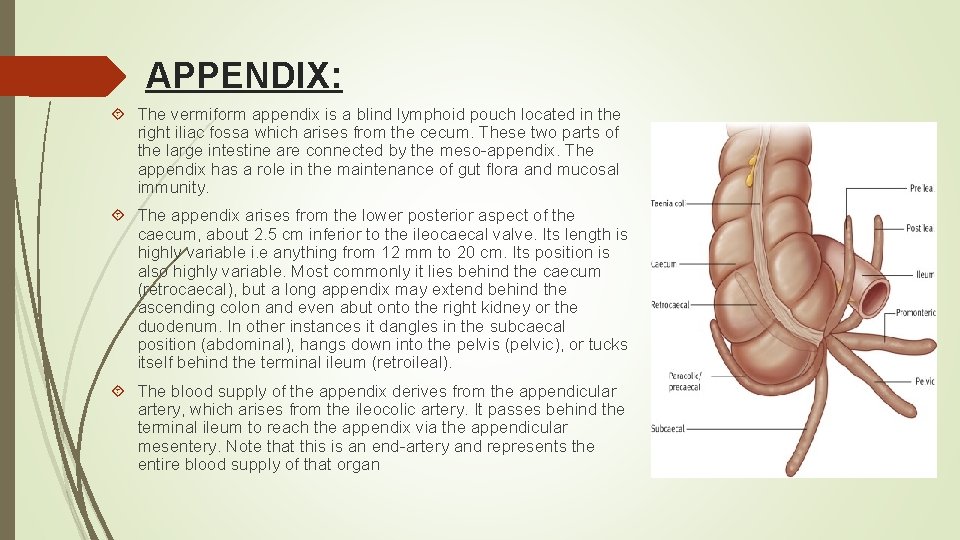
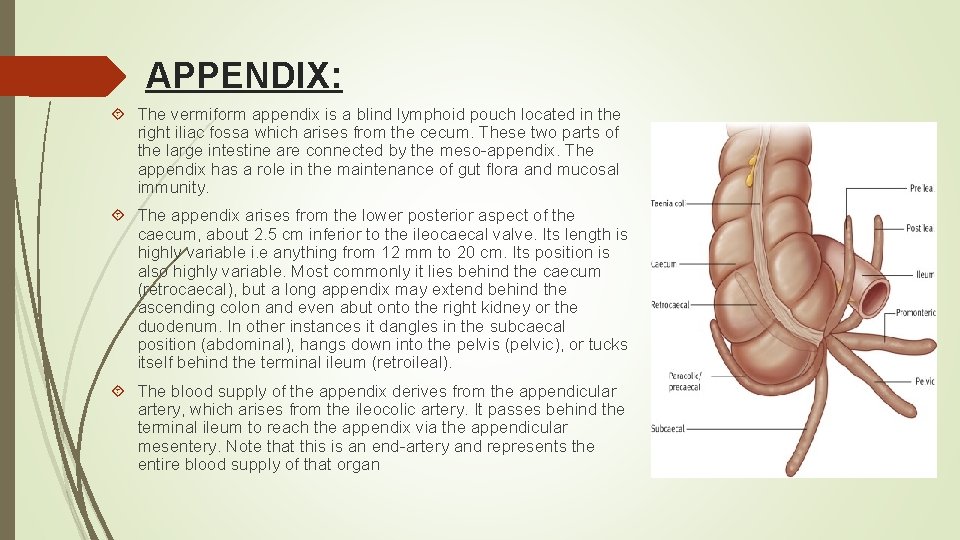
APPENDIX: The vermiform appendix is a blind lymphoid pouch located in the right iliac fossa which arises from the cecum. These two parts of the large intestine are connected by the meso-appendix. The appendix has a role in the maintenance of gut flora and mucosal immunity. The appendix arises from the lower posterior aspect of the caecum, about 2. 5 cm inferior to the ileocaecal valve. Its length is highly variable i. e anything from 12 mm to 20 cm. Its position is also highly variable. Most commonly it lies behind the caecum (retrocaecal), but a long appendix may extend behind the ascending colon and even abut onto the right kidney or the duodenum. In other instances it dangles in the subcaecal position (abdominal), hangs down into the pelvis (pelvic), or tucks itself behind the terminal ileum (retroileal). The blood supply of the appendix derives from the appendicular artery, which arises from the ileocolic artery. It passes behind the terminal ileum to reach the appendix via the appendicular mesentery. Note that this is an end-artery and represents the entire blood supply of that organ
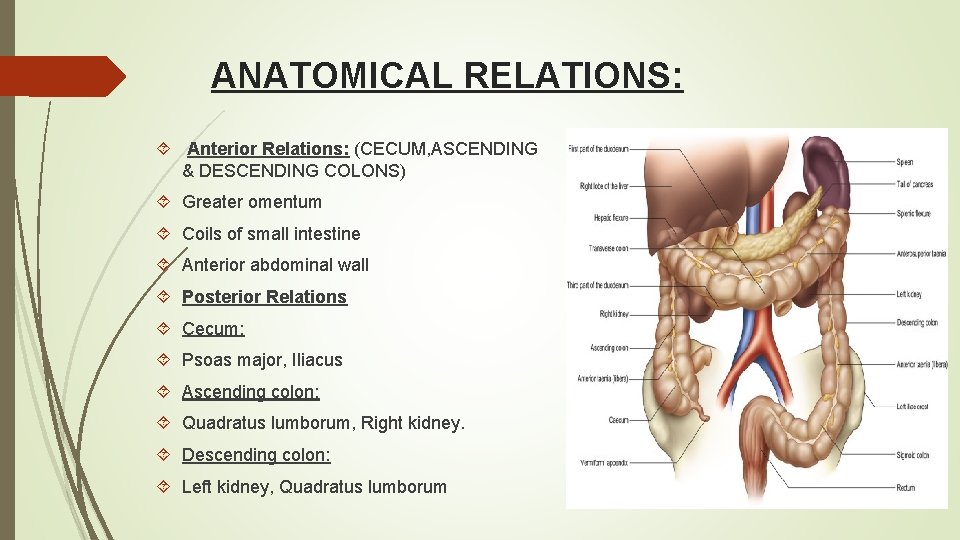
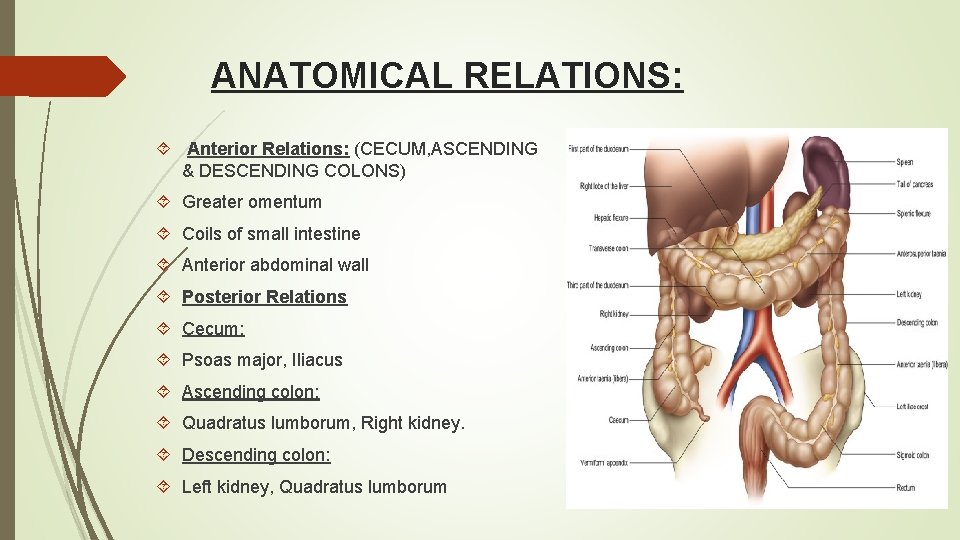
ANATOMICAL RELATIONS: Anterior Relations: (CECUM, ASCENDING & DESCENDING COLONS) Greater omentum Coils of small intestine Anterior abdominal wall Posterior Relations Cecum: Psoas major, Iliacus Ascending colon: Quadratus lumborum, Right kidney. Descending colon: Left kidney, Quadratus lumborum
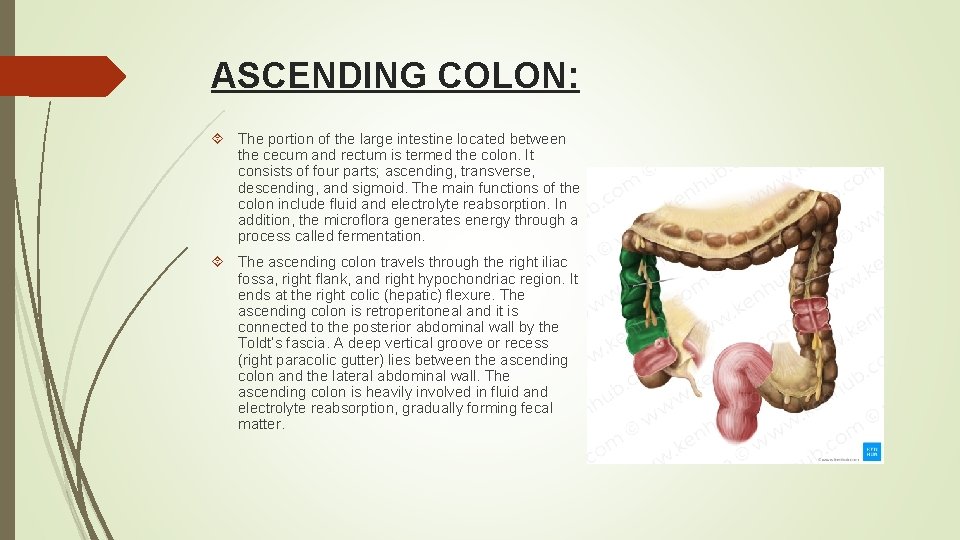
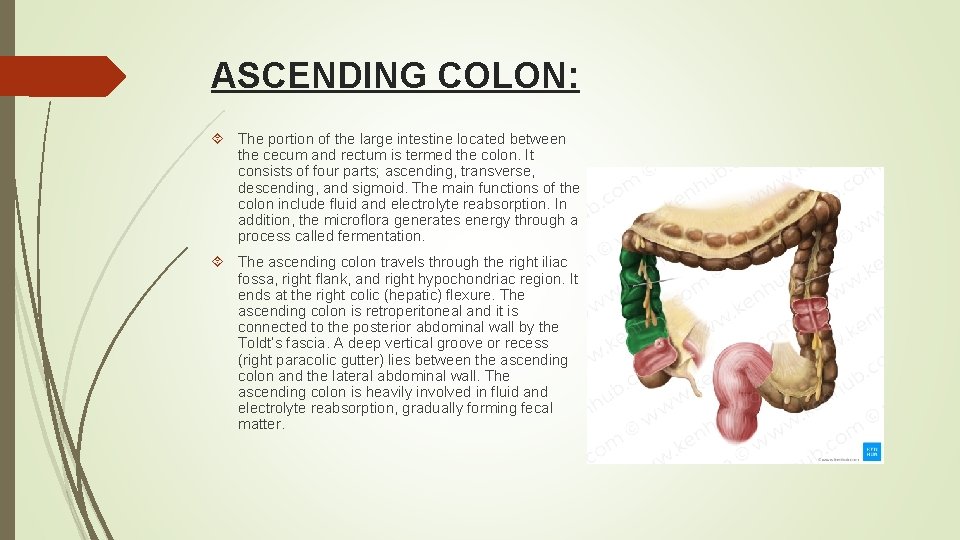
ASCENDING COLON: The portion of the large intestine located between the cecum and rectum is termed the colon. It consists of four parts; ascending, transverse, descending, and sigmoid. The main functions of the colon include fluid and electrolyte reabsorption. In addition, the microflora generates energy through a process called fermentation. The ascending colon travels through the right iliac fossa, right flank, and right hypochondriac region. It ends at the right colic (hepatic) flexure. The ascending colon is retroperitoneal and it is connected to the posterior abdominal wall by the Toldt’s fascia. A deep vertical groove or recess (right paracolic gutter) lies between the ascending colon and the lateral abdominal wall. The ascending colon is heavily involved in fluid and electrolyte reabsorption, gradually forming fecal matter.
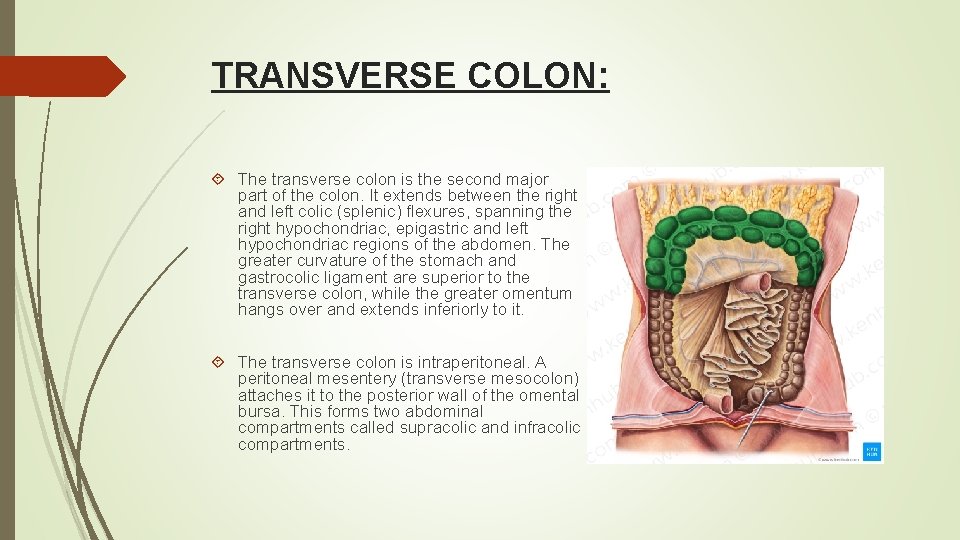
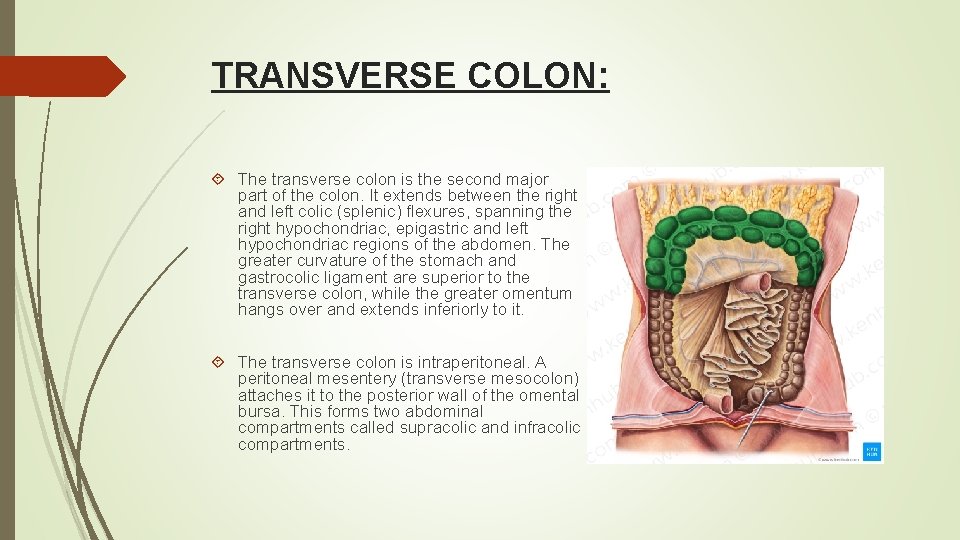
TRANSVERSE COLON: The transverse colon is the second major part of the colon. It extends between the right and left colic (splenic) flexures, spanning the right hypochondriac, epigastric and left hypochondriac regions of the abdomen. The greater curvature of the stomach and gastrocolic ligament are superior to the transverse colon, while the greater omentum hangs over and extends inferiorly to it. The transverse colon is intraperitoneal. A peritoneal mesentery (transverse mesocolon) attaches it to the posterior wall of the omental bursa. This forms two abdominal compartments called supracolic and infracolic compartments.
Relations of Transverse Colon: Anterior: greater omentum, anterior abdominal wall Posterior: 2 nd part of duodenum , pancreas & superior mesenteric vessels. Superior: liver, gall bladder, stomach Inferior: coils of small intestine
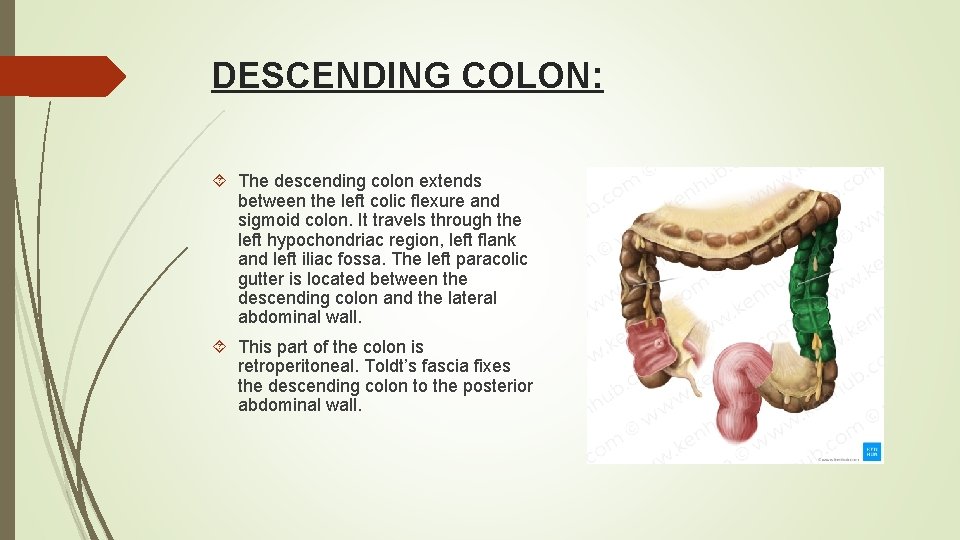
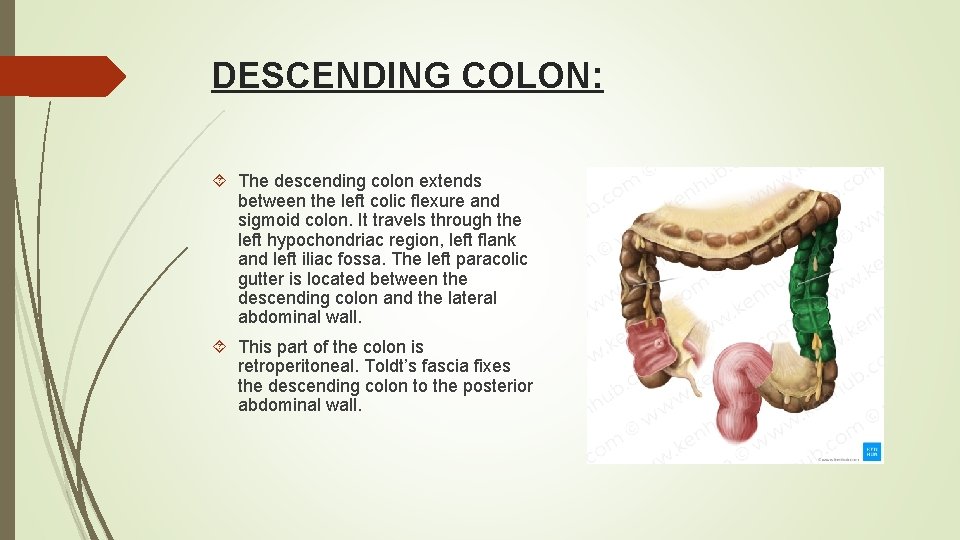
DESCENDING COLON: The descending colon extends between the left colic flexure and sigmoid colon. It travels through the left hypochondriac region, left flank and left iliac fossa. The left paracolic gutter is located between the descending colon and the lateral abdominal wall. This part of the colon is retroperitoneal. Toldt’s fascia fixes the descending colon to the posterior abdominal wall.
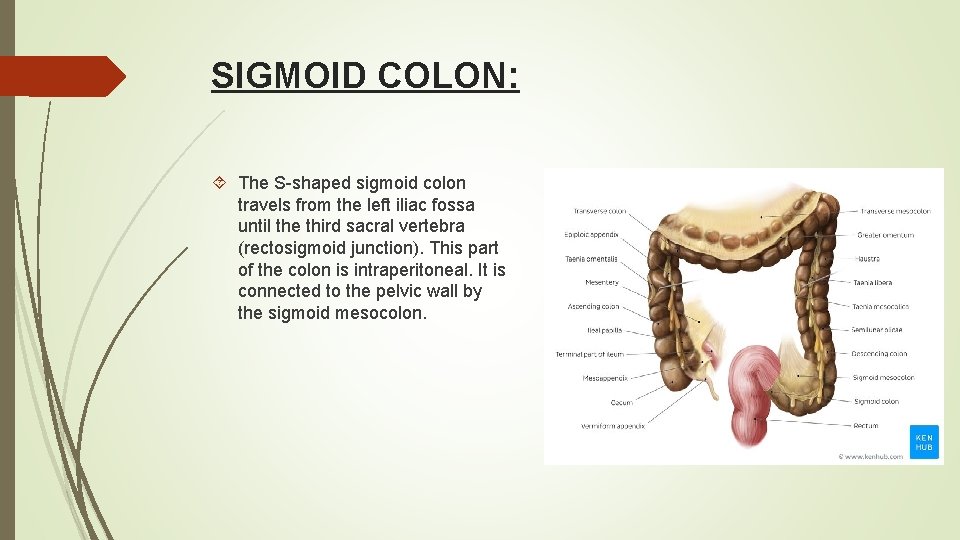
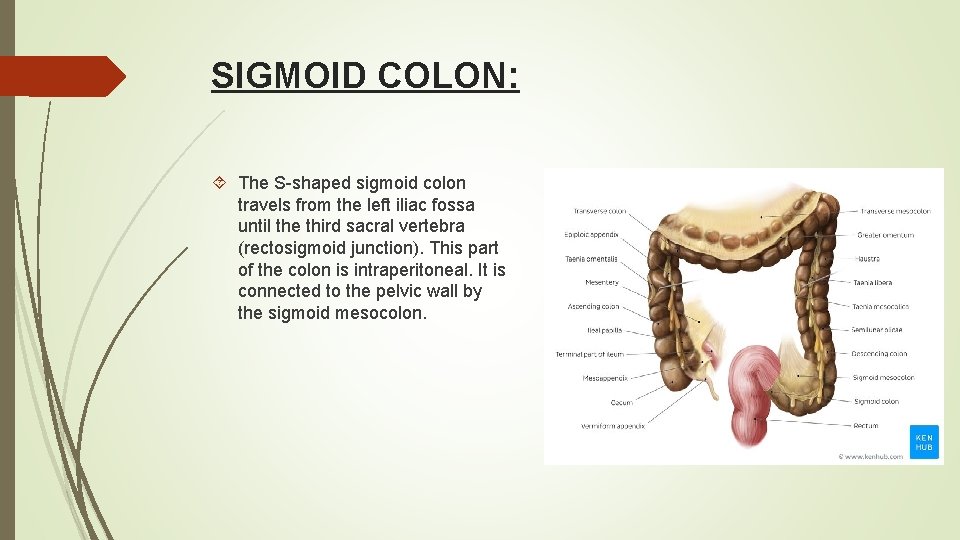
SIGMOID COLON: The S-shaped sigmoid colon travels from the left iliac fossa until the third sacral vertebra (rectosigmoid junction). This part of the colon is intraperitoneal. It is connected to the pelvic wall by the sigmoid mesocolon.
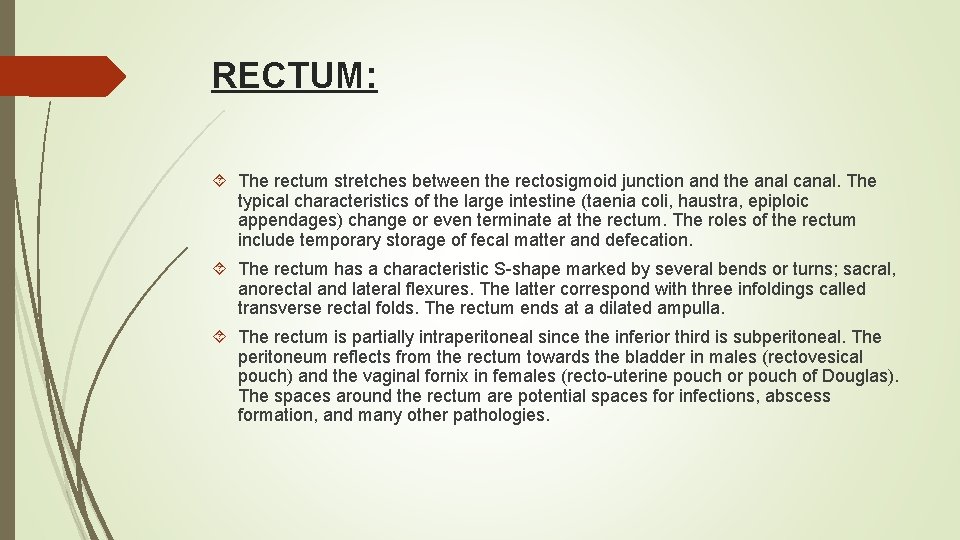
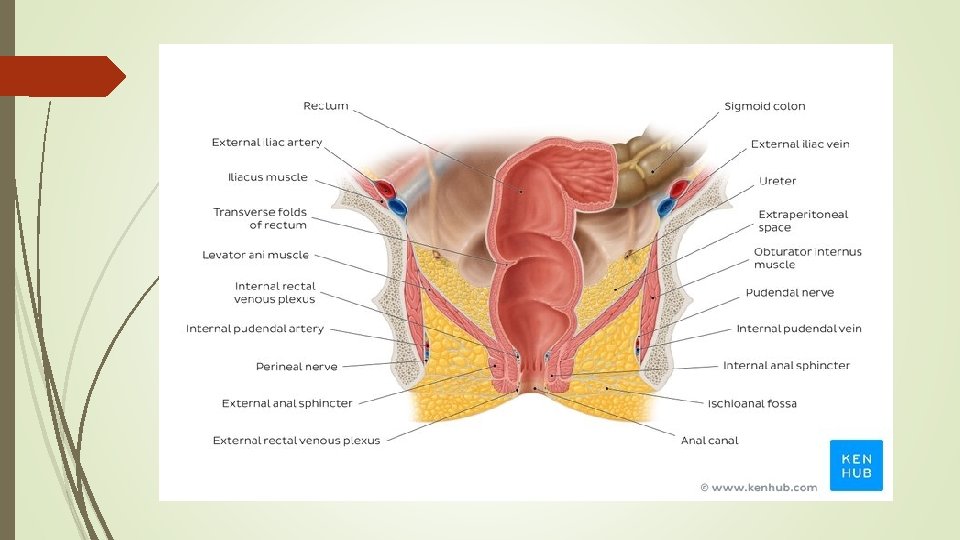
RECTUM: The rectum stretches between the rectosigmoid junction and the anal canal. The typical characteristics of the large intestine (taenia coli, haustra, epiploic appendages) change or even terminate at the rectum. The roles of the rectum include temporary storage of fecal matter and defecation. The rectum has a characteristic S-shape marked by several bends or turns; sacral, anorectal and lateral flexures. The latter correspond with three infoldings called transverse rectal folds. The rectum ends at a dilated ampulla. The rectum is partially intraperitoneal since the inferior third is subperitoneal. The peritoneum reflects from the rectum towards the bladder in males (rectovesical pouch) and the vaginal fornix in females (recto-uterine pouch or pouch of Douglas). The spaces around the rectum are potential spaces for infections, abscess formation, and many other pathologies.
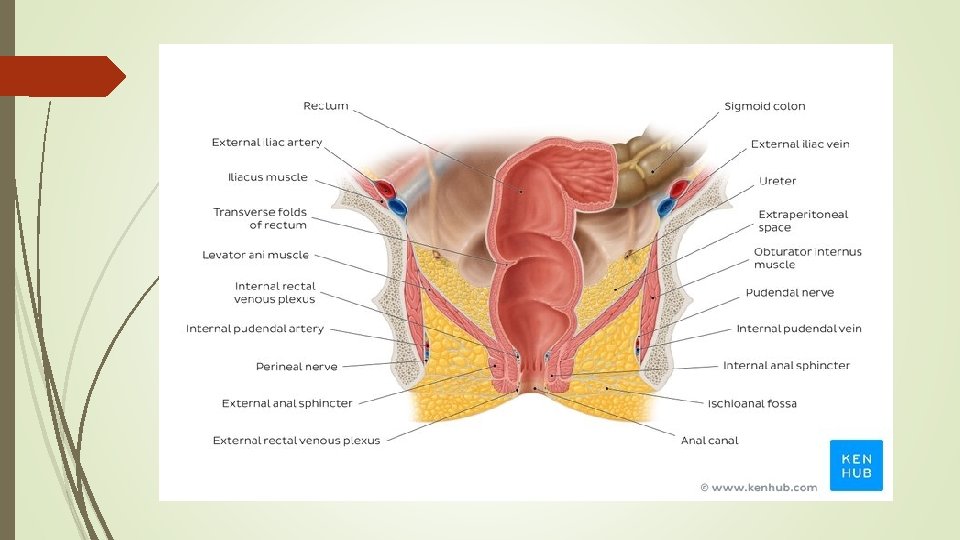
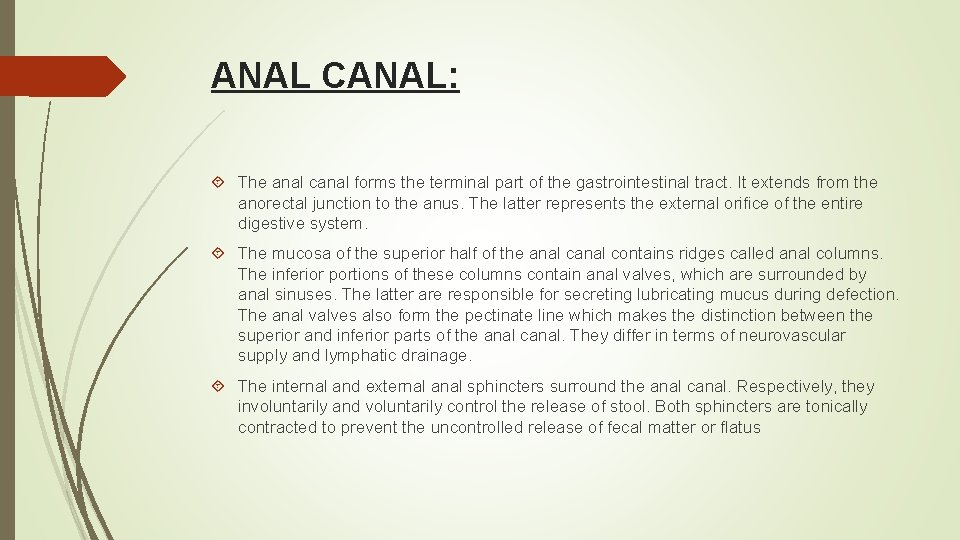
ANAL CANAL: The anal canal forms the terminal part of the gastrointestinal tract. It extends from the anorectal junction to the anus. The latter represents the external orifice of the entire digestive system. The mucosa of the superior half of the anal contains ridges called anal columns. The inferior portions of these columns contain anal valves, which are surrounded by anal sinuses. The latter are responsible for secreting lubricating mucus during defection. The anal valves also form the pectinate line which makes the distinction between the superior and inferior parts of the anal canal. They differ in terms of neurovascular supply and lymphatic drainage. The internal and external anal sphincters surround the anal canal. Respectively, they involuntarily and voluntarily control the release of stool. Both sphincters are tonically contracted to prevent the uncontrolled release of fecal matter or flatus
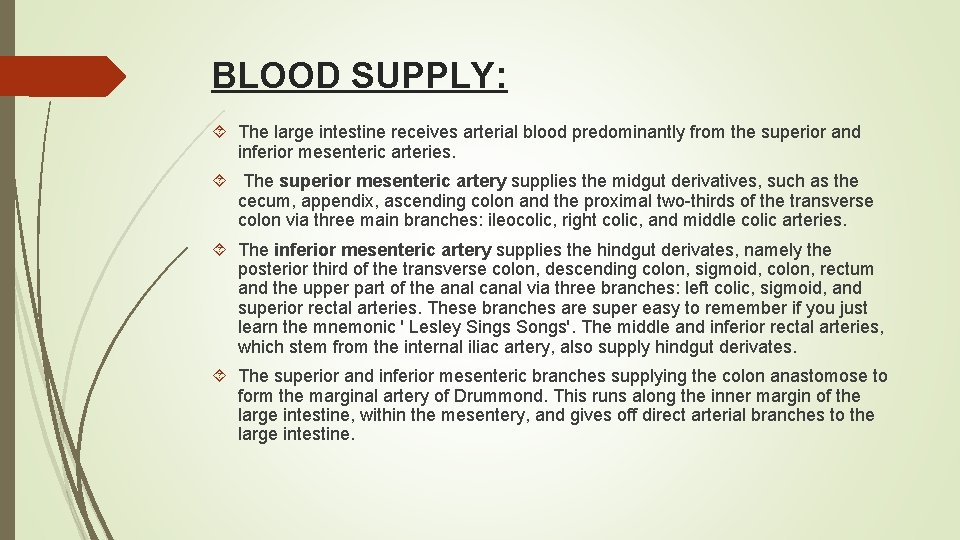
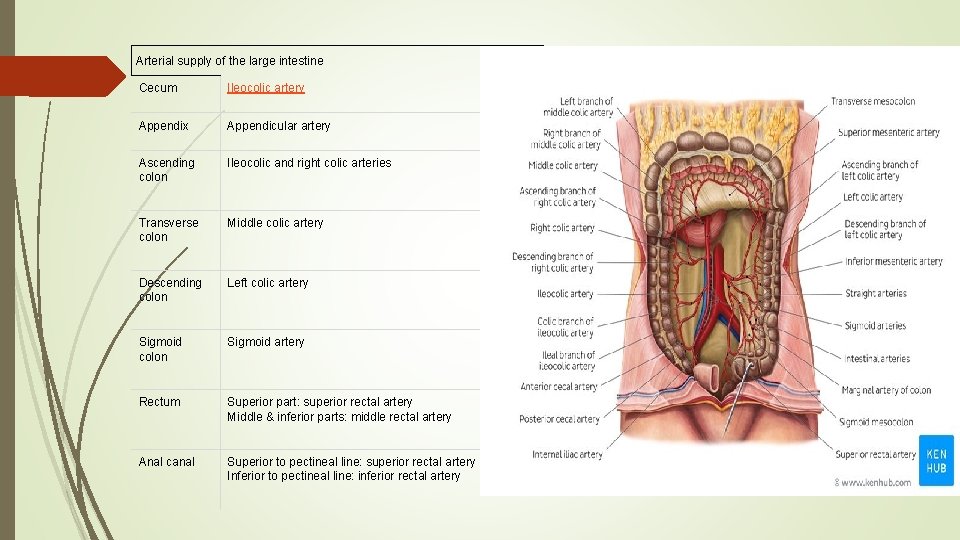
BLOOD SUPPLY: The large intestine receives arterial blood predominantly from the superior and inferior mesenteric arteries. The superior mesenteric artery supplies the midgut derivatives, such as the cecum, appendix, ascending colon and the proximal two-thirds of the transverse colon via three main branches: ileocolic, right colic, and middle colic arteries. The inferior mesenteric artery supplies the hindgut derivates, namely the posterior third of the transverse colon, descending colon, sigmoid, colon, rectum and the upper part of the anal canal via three branches: left colic, sigmoid, and superior rectal arteries. These branches are super easy to remember if you just learn the mnemonic ' Lesley Sings Songs'. The middle and inferior rectal arteries, which stem from the internal iliac artery, also supply hindgut derivates. The superior and inferior mesenteric branches supplying the colon anastomose to form the marginal artery of Drummond. This runs along the inner margin of the large intestine, within the mesentery, and gives off direct arterial branches to the large intestine.
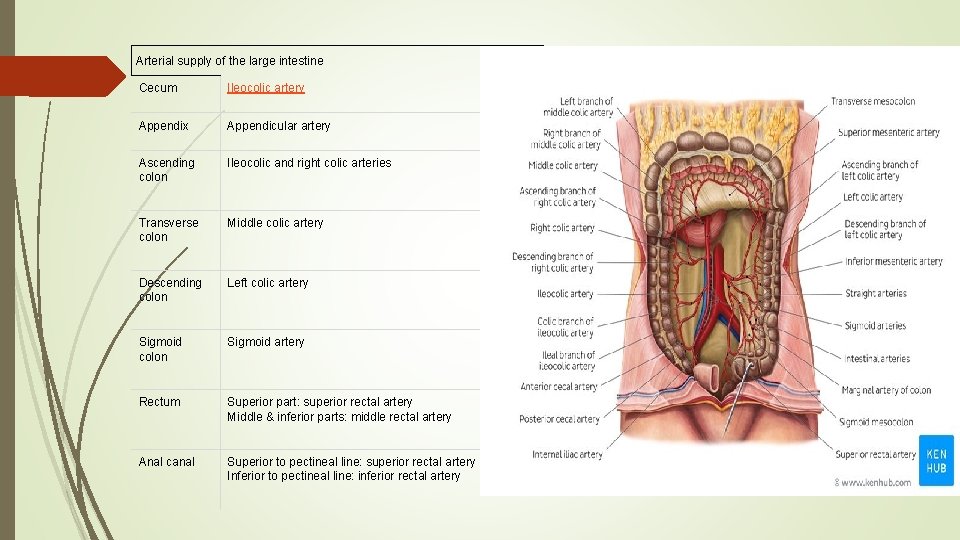
Arterial supply of the large intestine Cecum Ileocolic artery Appendix Appendicular artery Ascending colon Ileocolic and right colic arteries Transverse colon Middle colic artery Descending colon Left colic artery Sigmoid colon Sigmoid artery Rectum Superior part: superior rectal artery Middle & inferior parts: middle rectal artery Anal canal Superior to pectineal line: superior rectal artery Inferior to pectineal line: inferior rectal artery
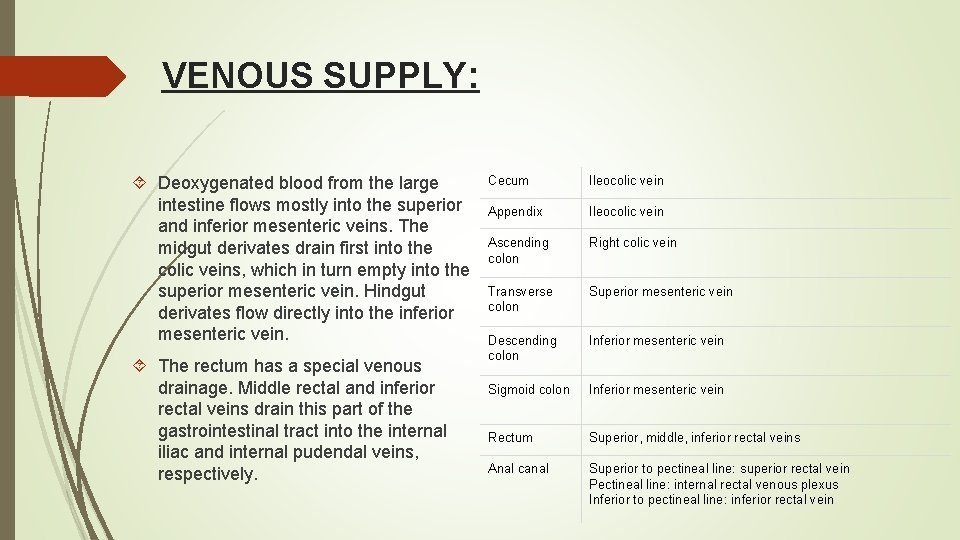
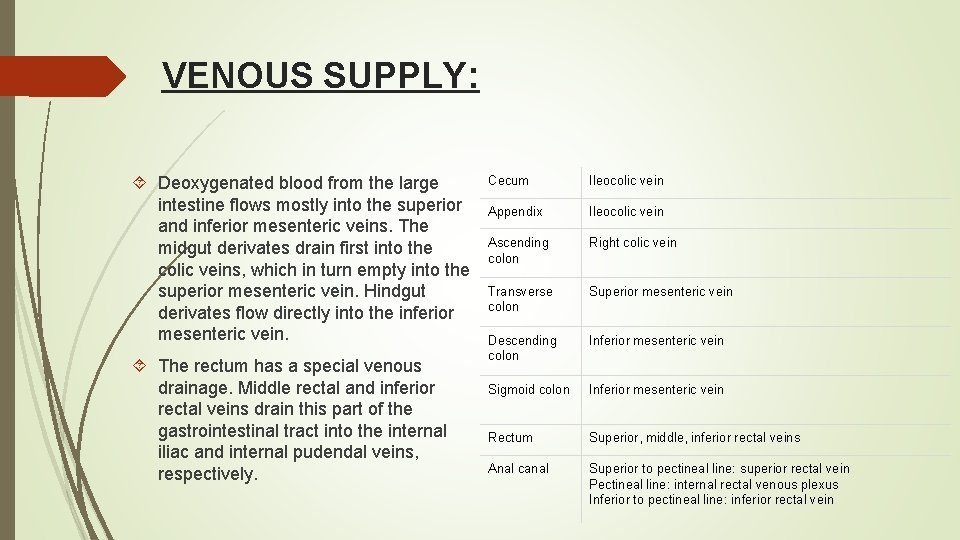
VENOUS SUPPLY: Deoxygenated blood from the large intestine flows mostly into the superior and inferior mesenteric veins. The midgut derivates drain first into the colic veins, which in turn empty into the superior mesenteric vein. Hindgut derivates flow directly into the inferior mesenteric vein. The rectum has a special venous drainage. Middle rectal and inferior rectal veins drain this part of the gastrointestinal tract into the internal iliac and internal pudendal veins, respectively. Cecum Ileocolic vein Appendix Ileocolic vein Ascending colon Right colic vein Transverse colon Superior mesenteric vein Descending colon Inferior mesenteric vein Sigmoid colon Inferior mesenteric vein Rectum Superior, middle, inferior rectal veins Anal canal Superior to pectineal line: superior rectal vein Pectineal line: internal rectal venous plexus Inferior to pectineal line: inferior rectal vein
INNERVATION: The large intestine receives innervation from two main sources: enteric and autonomic nervous systems. The enteric nervous system (ENS) is specific to the gastrointestinal tract. It consists of two nervous plexus called Meissner’s and Auerbach’s myenteric plexuses. The former is located within the submucosa of the large intestine, while the latter is situated between the longitudinal and circular muscle layers. The ENS is responsible for the peristaltic contractions of the large intestine, as well as mucosal secretions. The autonomic nervous system (ANS) is the second major contributor to the innervation of the large intestine. Sympathetic innervation to the midgut derivates originates from the T 5 -T 12 spinal nerves and travel to the celiac and superior mesenteric plexuses via the greater and lesser splanchnic nerves. Whilst, sympathetic innervation to the hindgut structures originates from the S 1 -S 2 spinal nerves and travel to the aortic, inferior mesenteric, hypogastric plexuses via the lumbar and sacral splanchnic nerves. Sympathetic nerves are responsible for slowing down motility within the large intestine and for inducing contractions of both the ileocecal valve and internal anal sphincter. The parasympathetic innervation to the midgut derivates travels via the vagus nerve (CN X) to the superior mesenteric and celiac plexuses. Hindgut structures receive parasympathetic innervation from the S 2 -S 4 spinal nerves via the pelvic splanchnic nerves. These subsequently project to the hypogastric nervous plexus. Parasympathetic innervation is responsible for increasing the motility within the large intestine, inducing defecation and relaxing the internal anal sphincter.
CLINICAL RELATIONS: Diverticulosis is a medical condition in which multiple sac-like protrusions called diverticula develop along the colon. Their highest frequency is within the sigmoid part. Diverticulosis has numerous risk factors, such as low fiber diet, physical inactivity, obesity and constipation. Diverticulosis is generally asymptomatic until the diverticula become inflamed (diverticulitis). This condition manifests with abdominal pain in the left iliac fossa, nausea, vomiting and low-grade fever. Uncomplicated diverticulitis is usually treated with oral antibiotics. Crohn’s disease is a chronic inflammatory bowel disease of unknown etiology which can affect any part of the alimentary tract, but most often the terminal ileum and colon. There are usually multiple inflammatory focuses leading to formation of multiple ulcers in the intestinal wall. The most common symptoms are fever, abdominal pain, diarrhea, and weight loss. Crohn’s disease is diagnosed by endoscopic and radiographic examination of the abdomen and is usually treated with immunosuppressants.
Haemorrhoids are vascular cushions found within the anal canal of healthy individuals, which help with the maintenance of faecal continence. If they become swollen and distended, they are referred to as pathological haemorrhoids. Pathological haemorrhoids are observed in people who suffer from constipation, prolonged straining when defecating, or raised intra-abdominal pressure (e. g pregnancy, ascites). Upon examination of the anal canal (with the patient in the lithotomy position), the haemorrhoids are typically located at the 3, 7 and 11 o’clock positions. They can cause bleeding and itchiness, and depending on the severity and can be managed conservatively or surgically.