Introduction to medical ethics Dr Leena AlQasem Topics
- Slides: 26
Introduction to medical ethics Dr Leena Al-Qasem
Topics covered: Ø Introduction Ø Definition of Ethics Ø Principles of ethical guidelines Ø Informed consent Ø Confidentiality
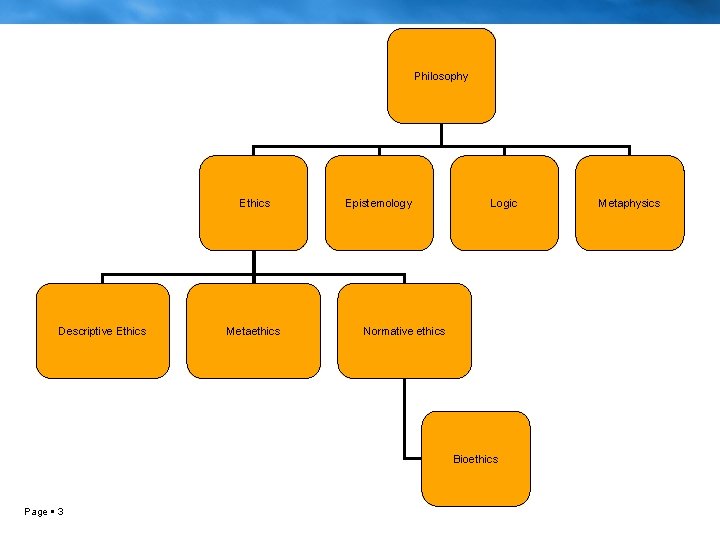
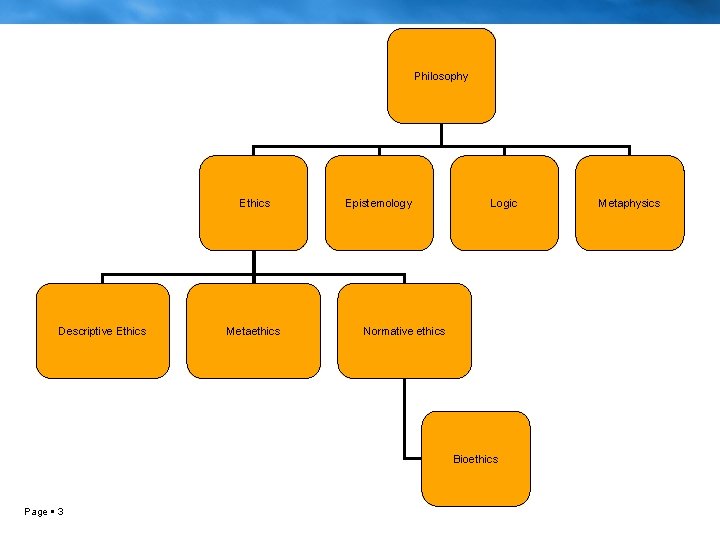
Philosophy Ethics Descriptive Ethics Metaethics Epistemology Logic Normative ethics Bioethics Page 3 Metaphysics
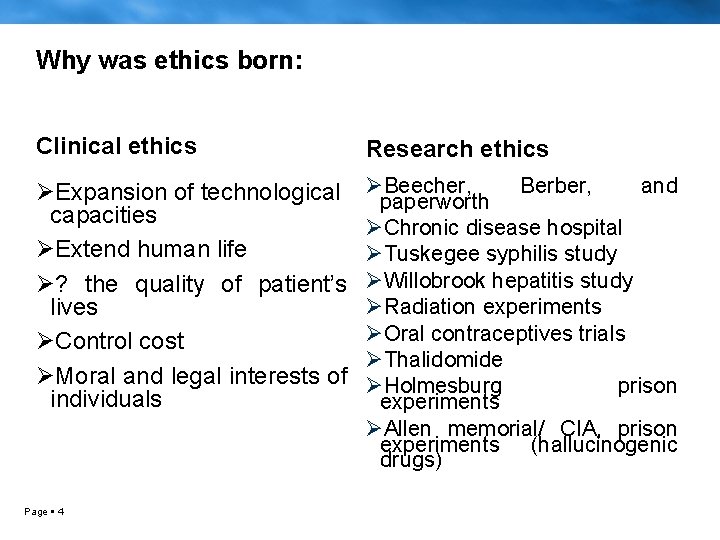
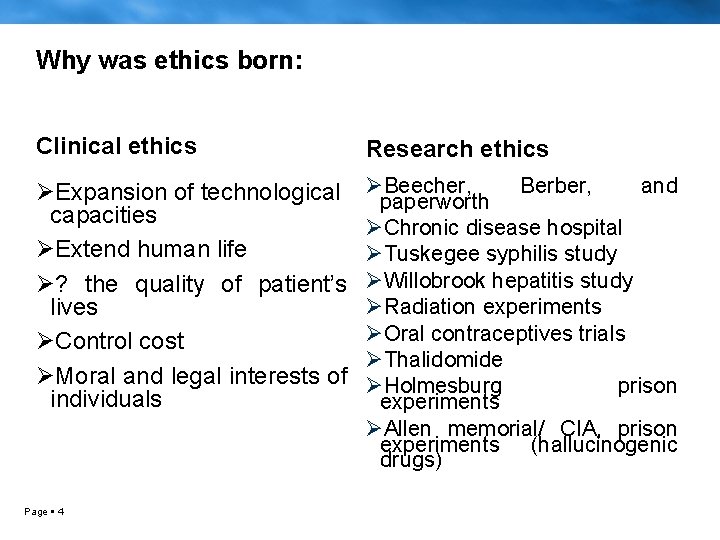
Why was ethics born: Clinical ethics Research ethics ØExpansion of technological capacities ØExtend human life Ø? the quality of patient’s lives ØControl cost ØMoral and legal interests of individuals ØBeecher, Berber, and paperworth ØChronic disease hospital ØTuskegee syphilis study ØWillobrook hepatitis study ØRadiation experiments ØOral contraceptives trials ØThalidomide ØHolmesburg prison experiments ØAllen memorial/ CIA, prison experiments (hallucinogenic drugs) Page 4
What does ethics mean to you? Page 5
Case I: You are caring for a patient with cancer. She is refusing to undergo surgery or receive chemotherapy for the treatment of her condition. What would the right action be in this case?
Case II: A patient is being treated by you for a certain condition. He wishes to use alternative forms of treatment for this condition, treatment which you do not believe is effective, due mainly to lack of scientific evidence. Moreover, you believe that the alternative treatment might interfere with the standard treatment and cause the patient’s condition to worsen. How you would handle this case?
Case III: You are a physician working in an intensive care unit with a capacity of five beds, four of which are occupied. You receive a call from the A&E where they have two patients needing ICU admission. The mother of one of those patients, whom you know, pleads with you to save her young son. The other patient, as you find out later is a foreigner with no relatives in the country. What would be the right action in this case?
Case IV: A 32 years old male is diagnosed with bacterial meningitis. After the physician explained his diagnosis to him, the risks and benefits, the patient refused to be treated for his illness and insisted on going home.
Principles of ethical guidelines: ØAutonomy ØBeneficence ØNonmaleficence ØSocial Justice
Autonomy: ØSelf-determination, independence, and freedom. ØPatients may choose among medically feasible alternatives. ØPatients may refuse unwanted medical interventions. Øpatients have the right to make choices that conflict with the wishes of family members or the recommendations of their physician.
Autonomy: Treating patients with respect entails several ethical obligations 1. Physicians must respect decisions of autonomous persons. 2. respect for persons with impaired decision making capacity 3. avoiding misrepresentation, maintaining confidentiality, and keeping promises
Autonomy is not absolute Ømay be justifiably restricted for several reasons: – person is incapable of making informed decisions. Respecting autonomy < important than acting in the best interest of the patient. – constrained by the needs of other individuals or society at large. – not free to act in ways that violate the autonomy of other people, harm others, or impose unfair claims on society's resources.
Beneficence: ØRequires physicians to take positive actions for the benefit of patients. ØBecause patients do not possess medical expertise and maybe vulnerable because of their illness, they rely on physicians to provide sound advice and to promote their well being. Page 14
ØPromotes patient best interest by: • Understanding patient perspective • Address misunderstandings and concern • Try to persuade patient • Negotiate a mutually acceptable plan of care • Ultimately let the patient decide Page 15
ØThe physician cannot be required to violate fundamental personal values, standards of scientific or ethical practice, or the law. ØIf the physician is unable to carry out the patient’s wishes, the physician must withdraw and/or transfer care of the patient Page 16
Nonmaleficence: DO NO HARM" forbids physicians: From providing ineffective therapies From acting maliciously or selfishly provides limited guidance since many interventions also entail serious risks and side effects. Provide standard care If no benefit, at least do not harm or make situation worse If benefit equals harm, do not intervene Page 17
Social Justice: The term in a general sense means fairness. In the health care setting, justice usually refers to the allocation of health care resources. Allocation is usually unavoidable because resources are limited and could be spent on other social goods, such as education or the environment, instead of health care
Social justice: ØIdeally allocation decisions are made by public policy and set by government officials ØPhysicians should participate in debates about allocation and help set policies.
Social justice: In general however, rationing medical care at the bedside should be avoided because it may be: – inconsistent, – discriminatory – ineffective. – At the bedside, physicians usually should act as patient advocates within constraints set by society and sound practice.
Social justice: If patients compete to limited resource e. g. time of physicians or bed in ICU Rationing by physicians should be done • according to patient's medical needs • probability and degree of benefit.
Difficulty with guidelines: However guidelines may be difficult to apply in new cases for several reasons Page 22
1. Guidelines need to be interpreted in the context of specific cases: ØCase to case variations inherent ØDifferent priorities and goals for care ØDistinguishing cases in ethically meaningful ways Page 23
2. Exceptions to guidelines may be appropriate: ØGuidelines are not absolute Øcases may have distinctive features ØTo ensure fairness, physicians who make an exception to a guideline should justify their decision ØThe justification should apply to all similar cases faced by other physicians Page 24
3. Different guidelines may conflict: ØIn many situations, following one ethical guideline would require the compromise of another guideline. Ømuch easier if there were a fixed hierarchy of ethical guidelines Page 25
Questions?
 Basic medical ethics
Basic medical ethics Business ethics presentation
Business ethics presentation Raija-leena söderholm
Raija-leena söderholm Ryhmähaastattelu työnhaussa
Ryhmähaastattelu työnhaussa Valkokello
Valkokello Leena jacob
Leena jacob The girl who couldn't see herself by leena dhingra
The girl who couldn't see herself by leena dhingra Leena pihlakoski
Leena pihlakoski Leena pihlakoski
Leena pihlakoski Leena koivusilta
Leena koivusilta Leena mittal
Leena mittal Leena yazan
Leena yazan Leena razzaq rate my professor
Leena razzaq rate my professor Leena yousef
Leena yousef Leena maria heikkola
Leena maria heikkola Leena linnainmaa
Leena linnainmaa Avointen kysymysten analysointi
Avointen kysymysten analysointi Leena maria heikkola
Leena maria heikkola Leena halila
Leena halila Leena hiltunen turku
Leena hiltunen turku Kovalentne side
Kovalentne side Paddle pop dinoterra
Paddle pop dinoterra Leena saraste
Leena saraste Leena wow
Leena wow Leena suurpää
Leena suurpää Moodle oamk
Moodle oamk Teoriatriangulaatio
Teoriatriangulaatio