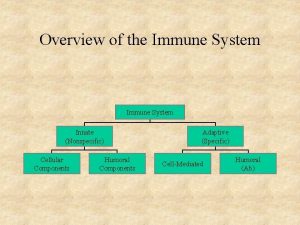
Innate Nonspecific Immunity Overview of the Immune System
- Slides: 33
Innate (Nonspecific) Immunity
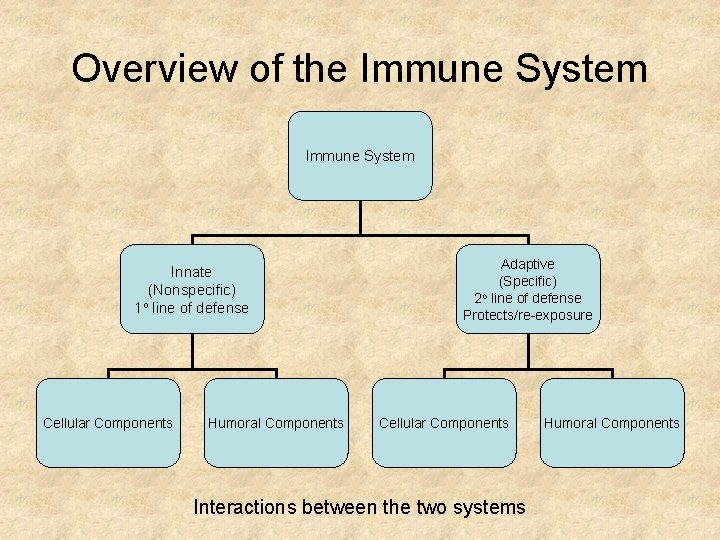
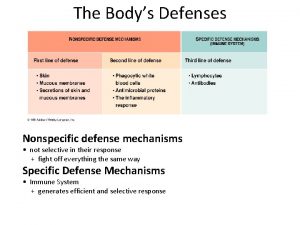
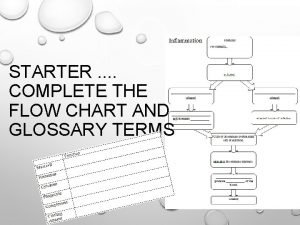
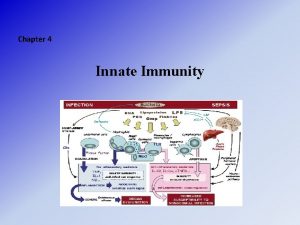
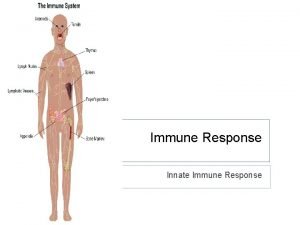
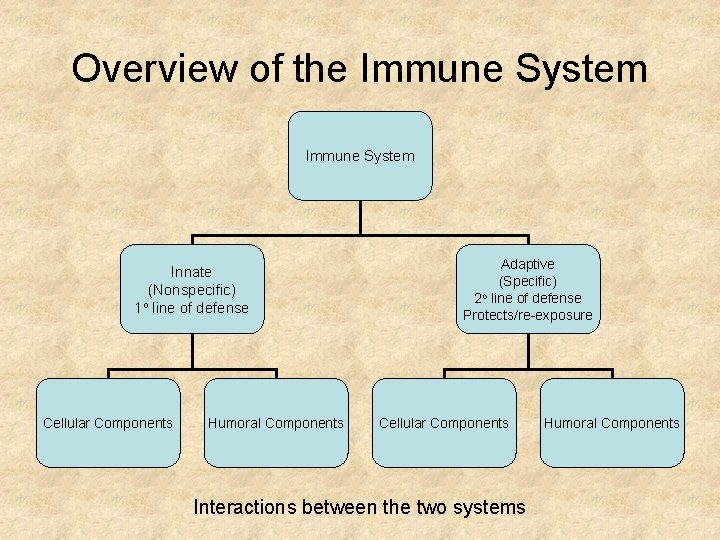
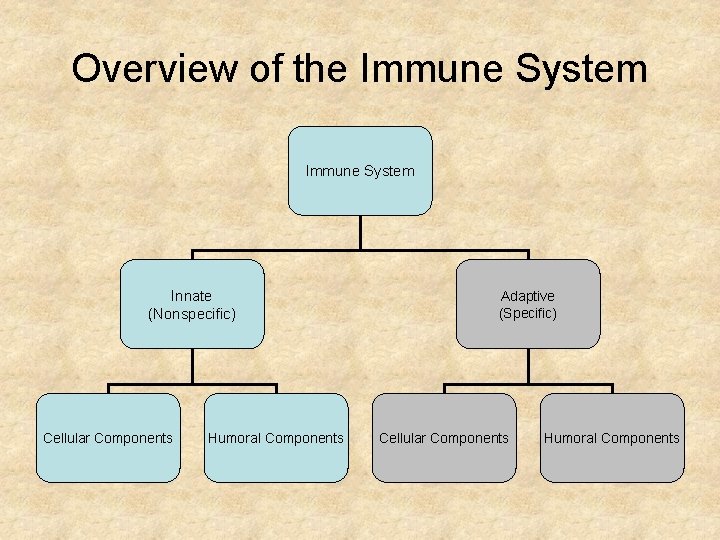
Overview of the Immune System Innate (Nonspecific) 1 o line of defense Cellular Components Humoral Components Adaptive (Specific) o 2 line of defense Protects/re-exposure Cellular Components Interactions between the two systems Humoral Components
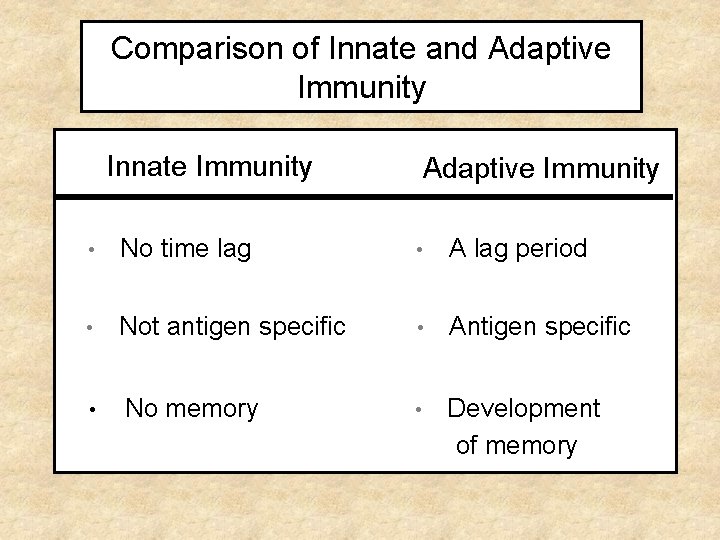
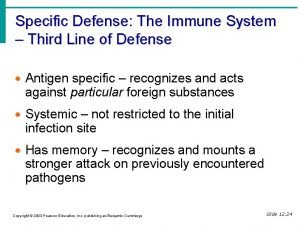
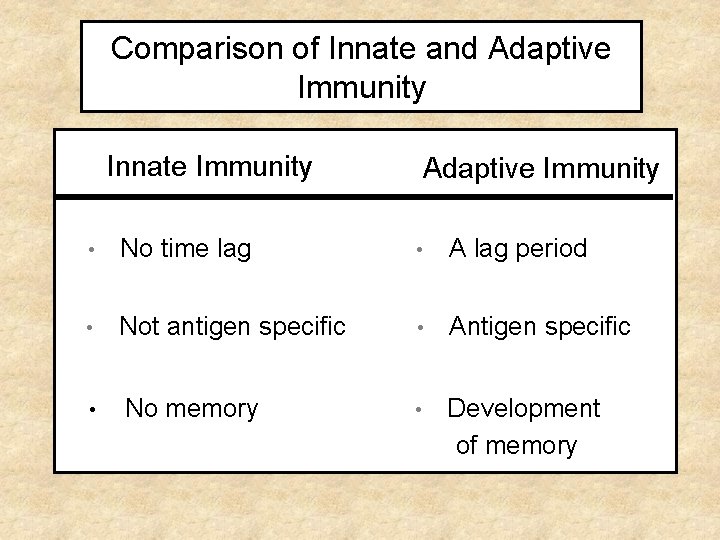
Comparison of Innate and Adaptive Immunity Innate Immunity Adaptive Immunity • No time lag • A lag period • Not antigen specific • Antigen specific • No memory • Development of memory
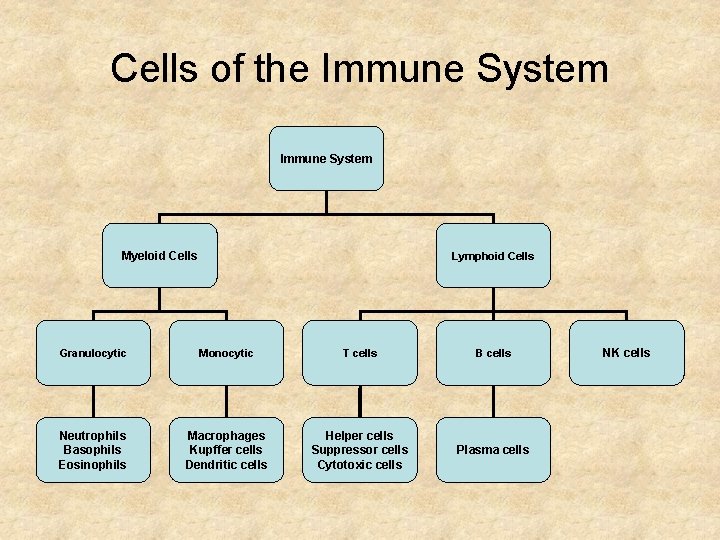
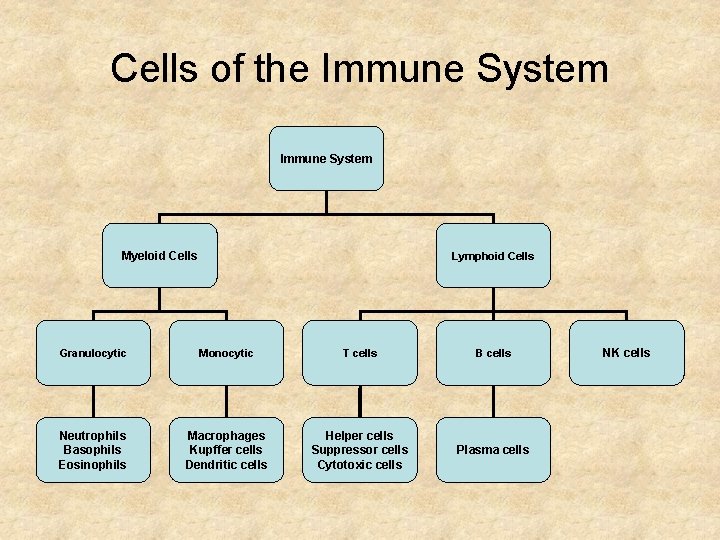
Cells of the Immune System Myeloid Cells Lymphoid Cells Granulocytic Monocytic T cells B cells Neutrophils Basophils Eosinophils Macrophages Kupffer cells Dendritic cells Helper cells Suppressor cells Cytotoxic cells Plasma cells NK cells
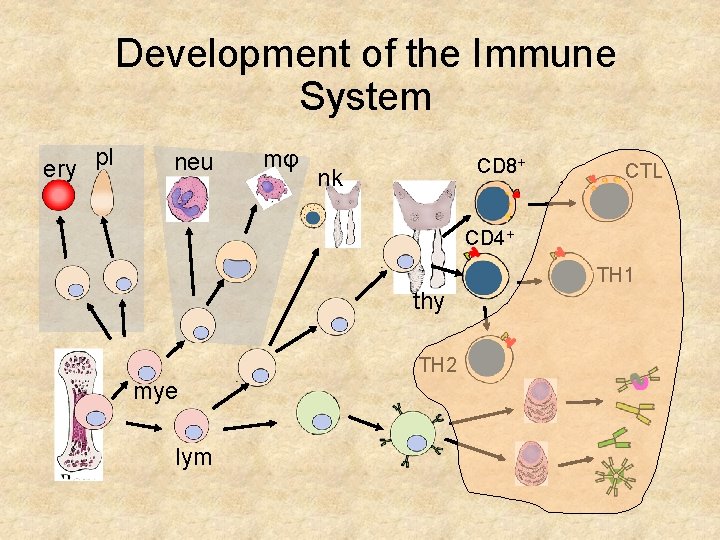
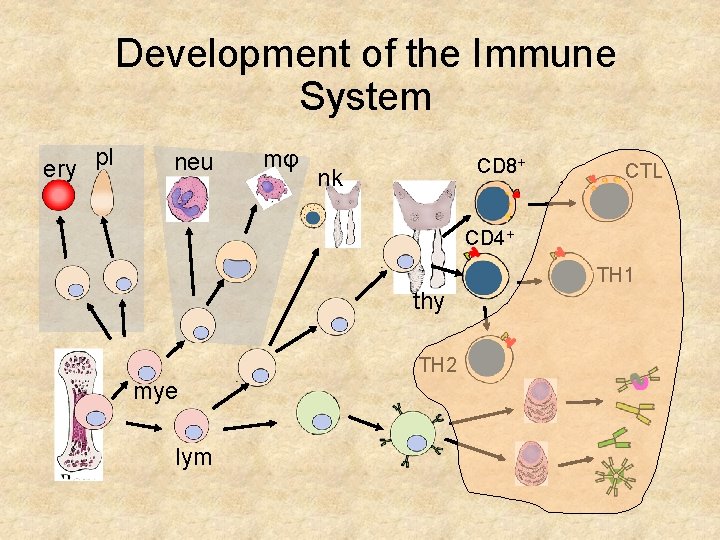
Development of the Immune System ery pl mφ neu CD 8+ nk CD 4+ TH 1 thy TH 2 mye lym CTL
Function of the Immune System (Self/Non-self Discrimination) • To protect from pathogens • • Intracellular (e. g. viruses and some bacteria and parasites) Extracellular (e. g. most bacteria, fungi and parasites) • To eliminate modified or altered self
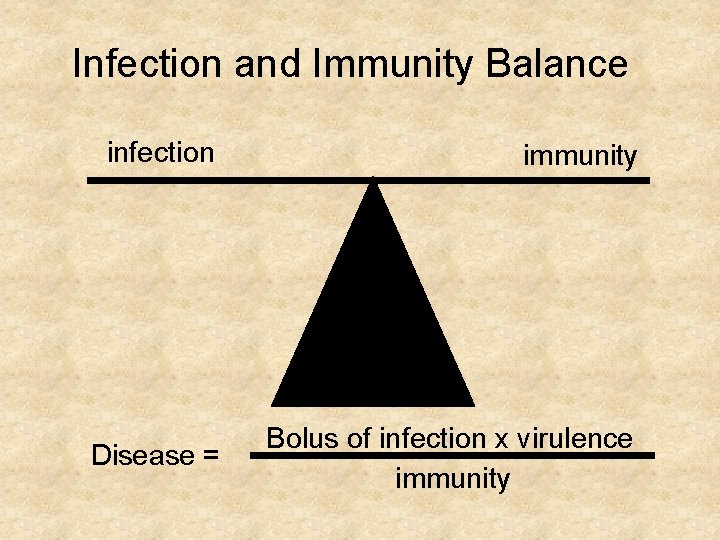
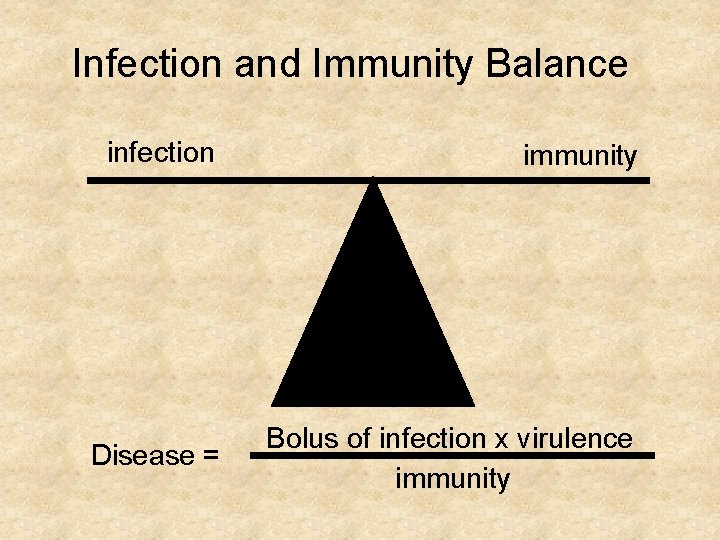
Infection and Immunity Balance infection immunity Disease = Bolus of infection x virulence immunity
Effects of the Immune System • Beneficial: • • Protection from Invaders • Elimination of Altered Self Detrimental: • Discomfort and collateral damage (inflammation) • Damage to self (hypersensitivity or autoimmunity)
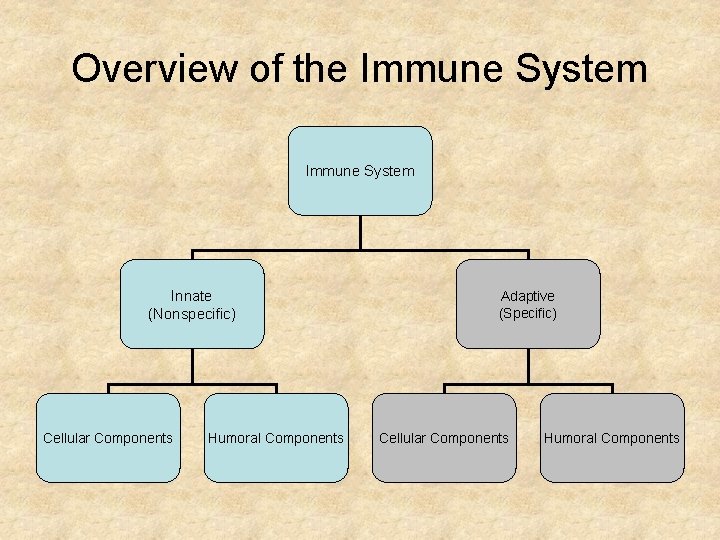
Overview of the Immune System Innate (Nonspecific) Cellular Components Humoral Components Adaptive (Specific) Cellular Components Humoral Components
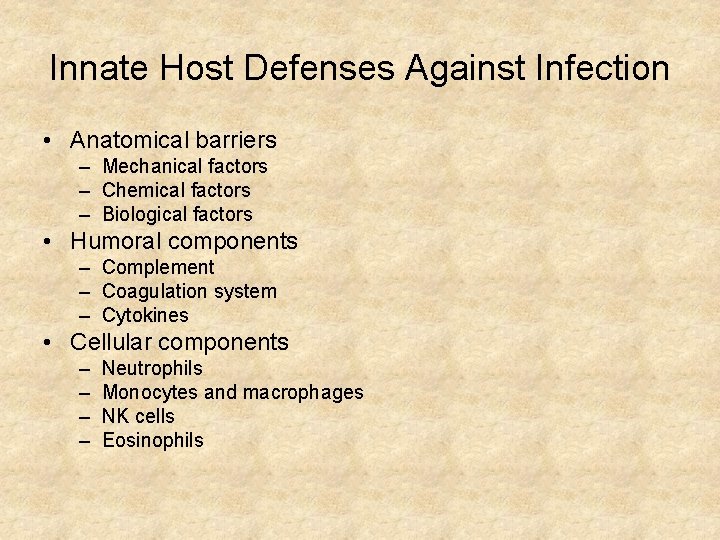
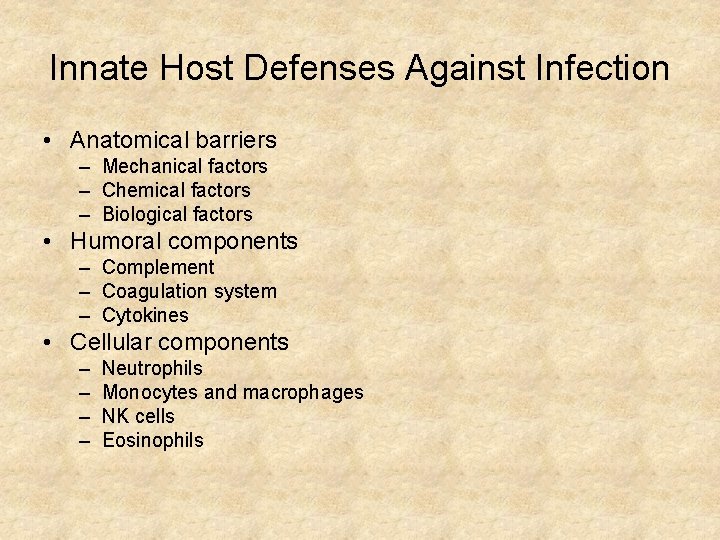
Innate Host Defenses Against Infection • Anatomical barriers – Mechanical factors – Chemical factors – Biological factors • Humoral components – Complement – Coagulation system – Cytokines • Cellular components – – Neutrophils Monocytes and macrophages NK cells Eosinophils
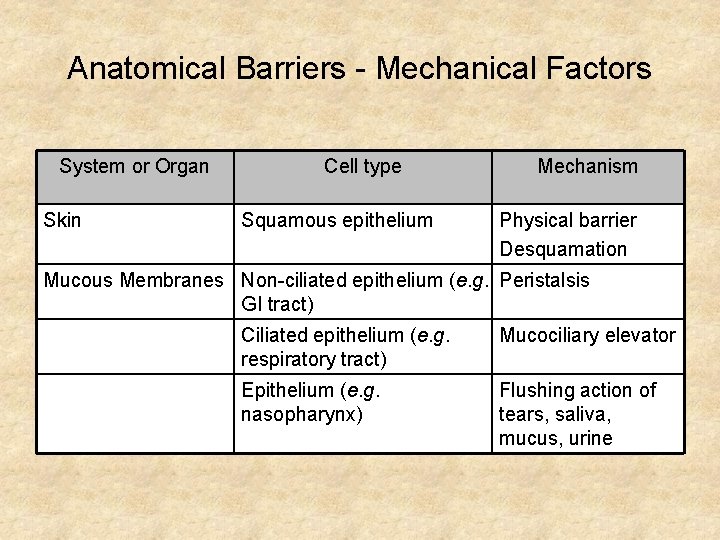
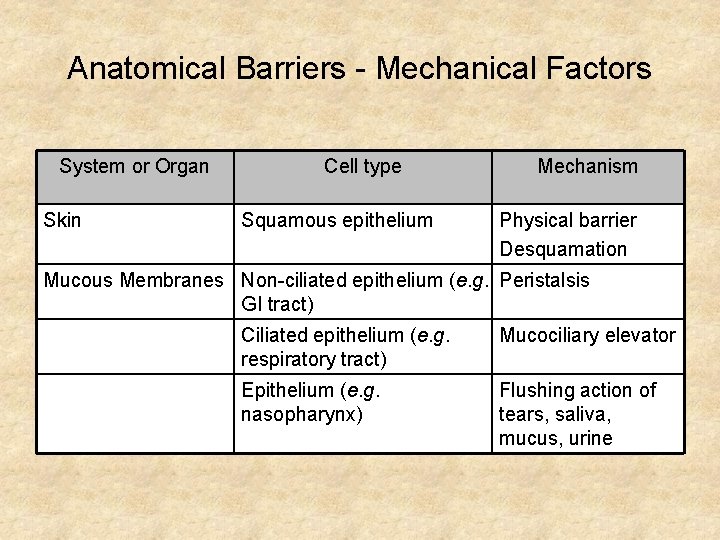
Anatomical Barriers - Mechanical Factors System or Organ Skin Cell type Squamous epithelium Mechanism Physical barrier Desquamation Mucous Membranes Non-ciliated epithelium (e. g. Peristalsis GI tract) Ciliated epithelium (e. g. respiratory tract) Mucociliary elevator Epithelium (e. g. nasopharynx) Flushing action of tears, saliva, mucus, urine
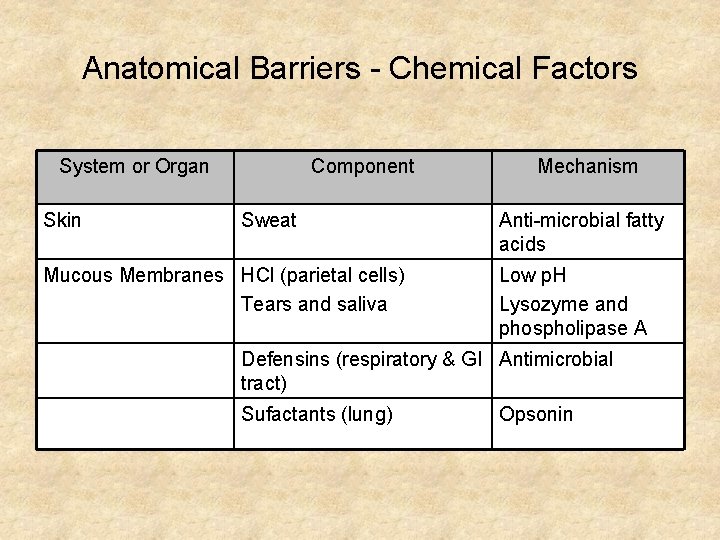
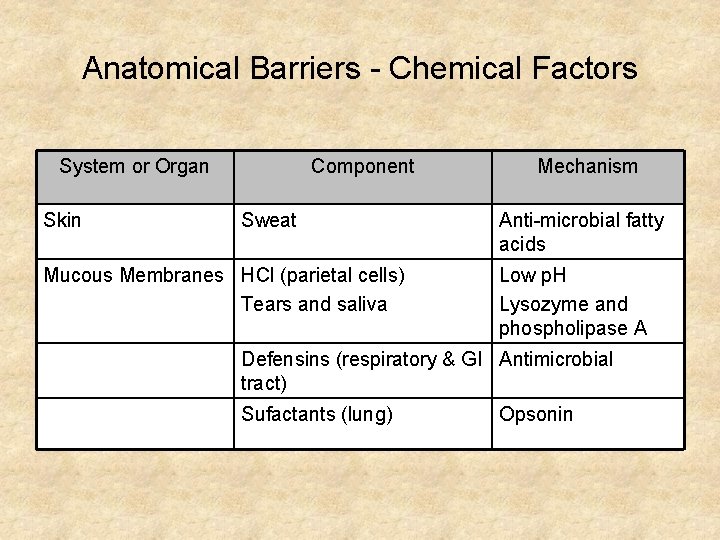
Anatomical Barriers - Chemical Factors System or Organ Skin Component Sweat Mucous Membranes HCl (parietal cells) Tears and saliva Mechanism Anti-microbial fatty acids Low p. H Lysozyme and phospholipase A Defensins (respiratory & GI Antimicrobial tract) Sufactants (lung) Opsonin
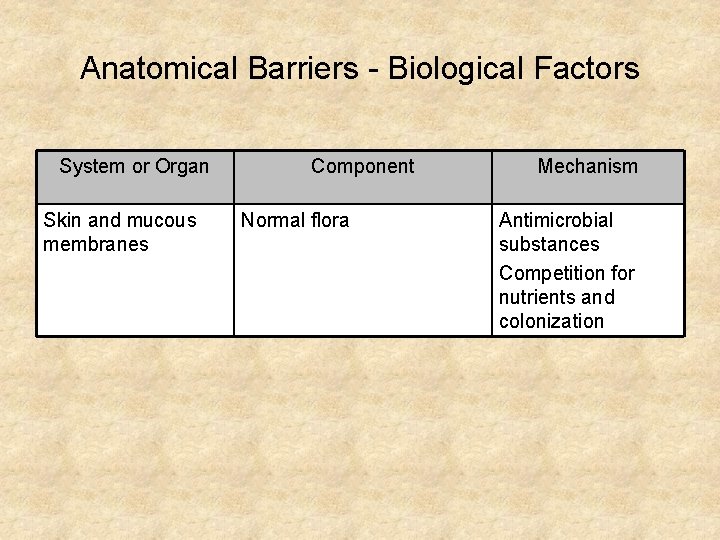
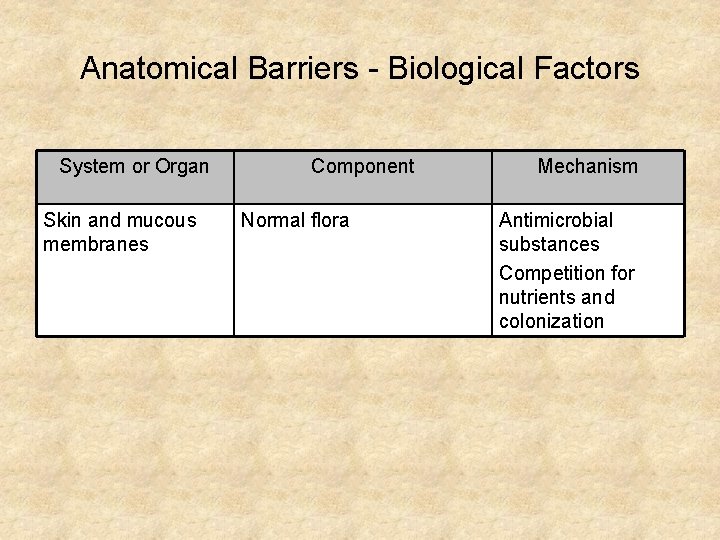
Anatomical Barriers - Biological Factors System or Organ Skin and mucous membranes Component Normal flora Mechanism Antimicrobial substances Competition for nutrients and colonization
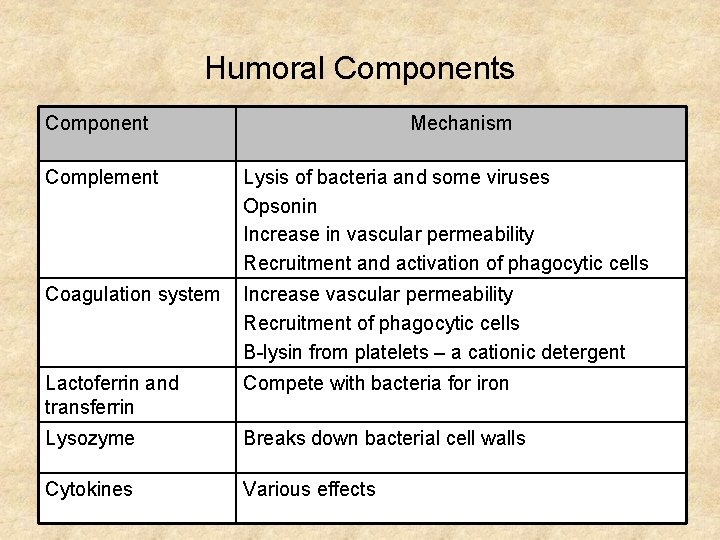
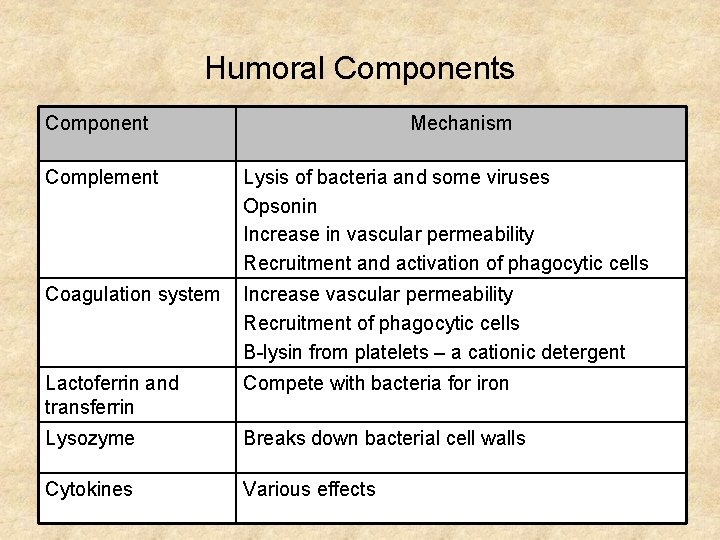
Humoral Components Component Mechanism Complement Lysis of bacteria and some viruses Opsonin Increase in vascular permeability Recruitment and activation of phagocytic cells Coagulation system Increase vascular permeability Recruitment of phagocytic cells Β-lysin from platelets – a cationic detergent Lactoferrin and transferrin Compete with bacteria for iron Lysozyme Breaks down bacterial cell walls Cytokines Various effects
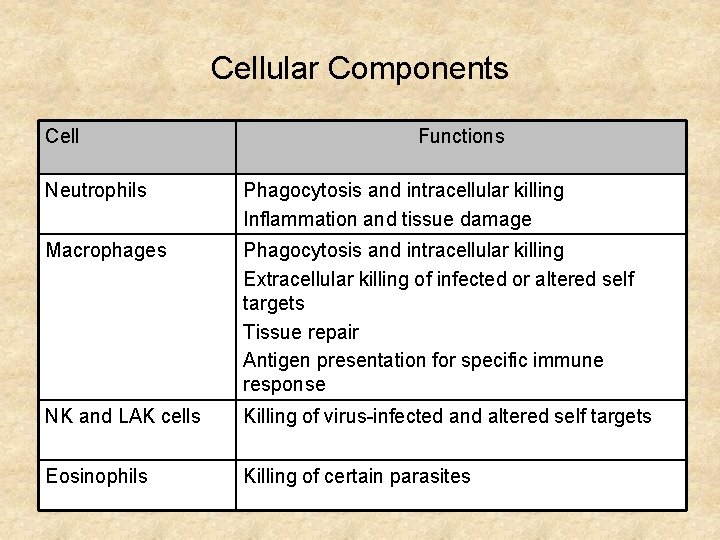
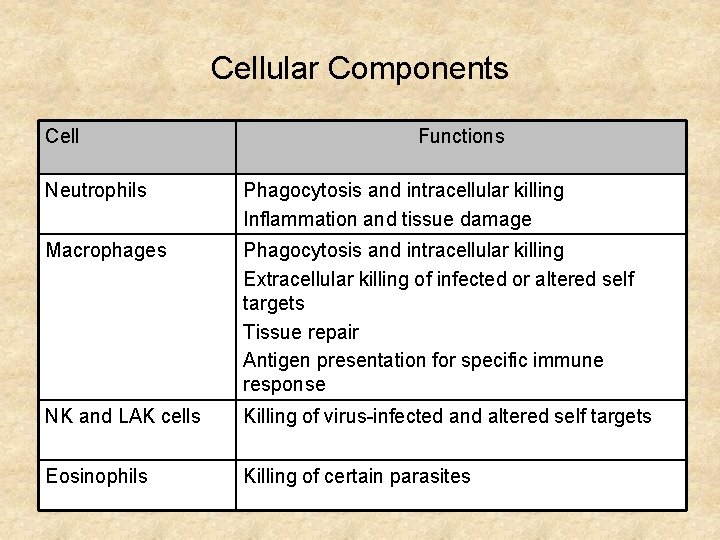
Cellular Components Cell Functions Neutrophils Phagocytosis and intracellular killing Inflammation and tissue damage Macrophages Phagocytosis and intracellular killing Extracellular killing of infected or altered self targets Tissue repair Antigen presentation for specific immune response NK and LAK cells Killing of virus-infected and altered self targets Eosinophils Killing of certain parasites
Phagocytosis and Intracellular Killing
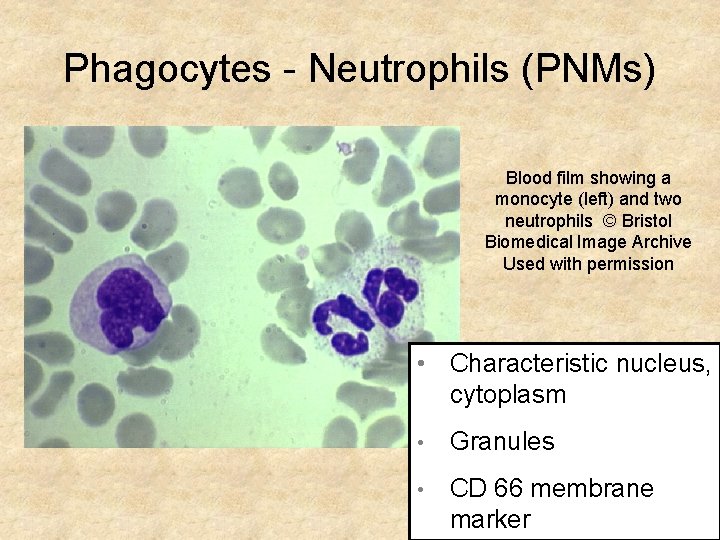
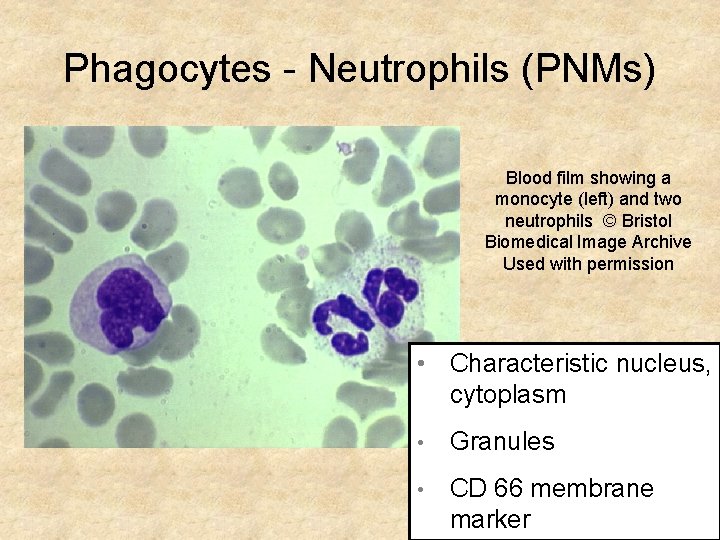
Phagocytes - Neutrophils (PNMs) Blood film showing a monocyte (left) and two neutrophils © Bristol Biomedical Image Archive Used with permission • Characteristic nucleus, cytoplasm • Granules • CD 66 membrane marker
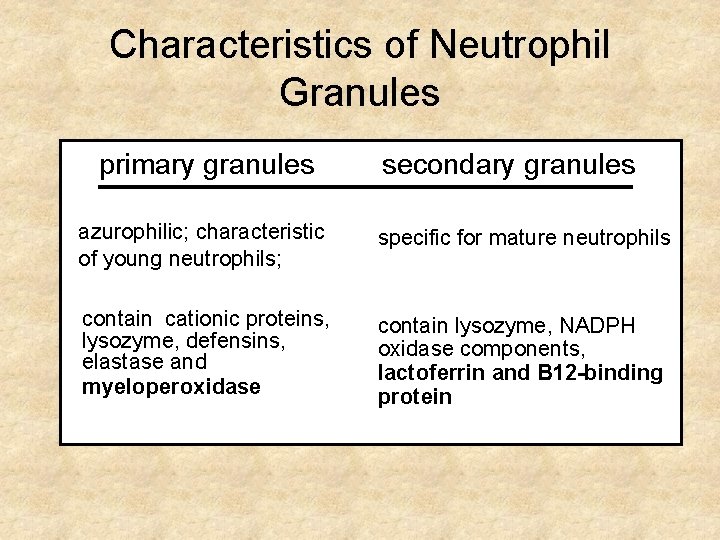
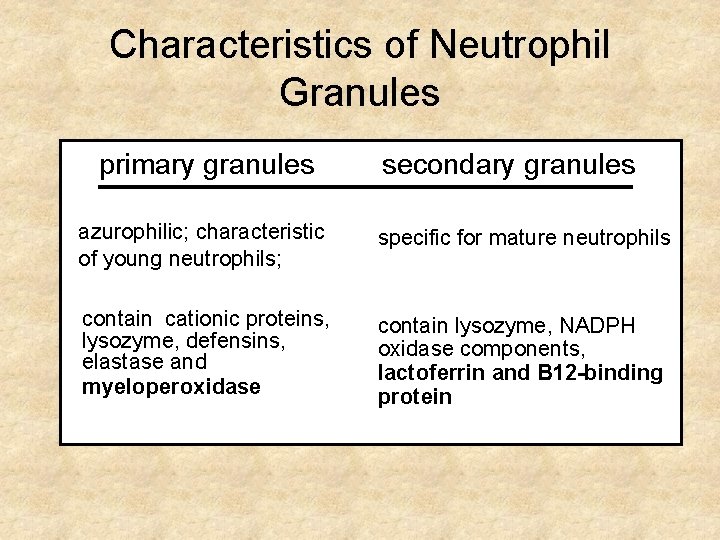
Characteristics of Neutrophil Granules primary granules secondary granules azurophilic; characteristic of young neutrophils; specific for mature neutrophils contain cationic proteins, lysozyme, defensins, elastase and myeloperoxidase contain lysozyme, NADPH oxidase components, lactoferrin and B 12 -binding protein
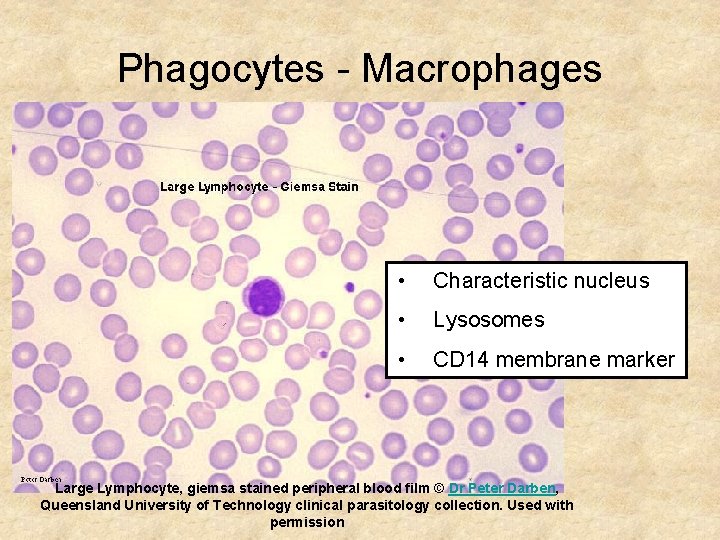
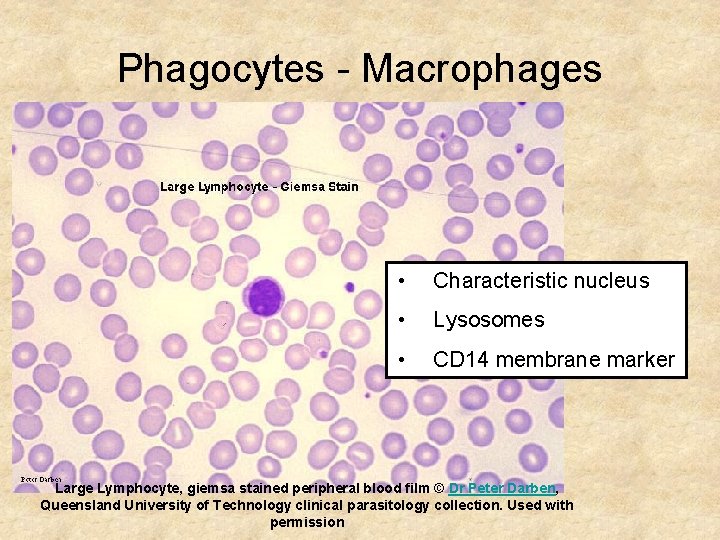
Phagocytes - Macrophages • Characteristic nucleus • Lysosomes • CD 14 membrane marker Large Lymphocyte, giemsa stained peripheral blood film © Dr Peter Darben, Queensland University of Technology clinical parasitology collection. Used with permission
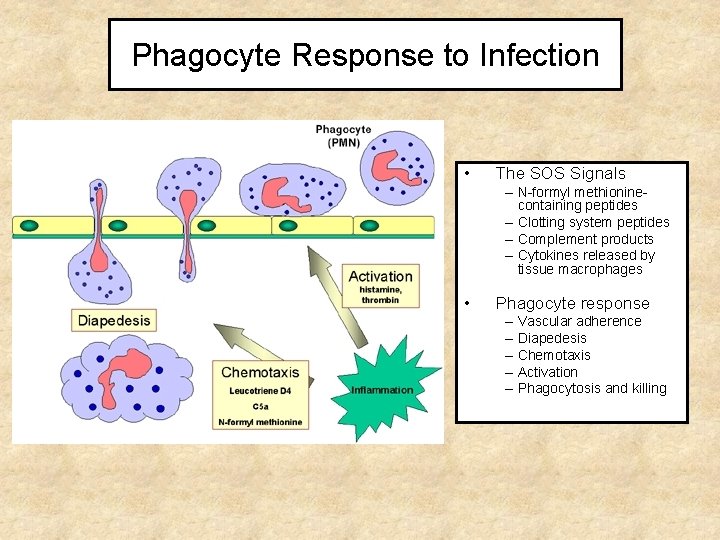
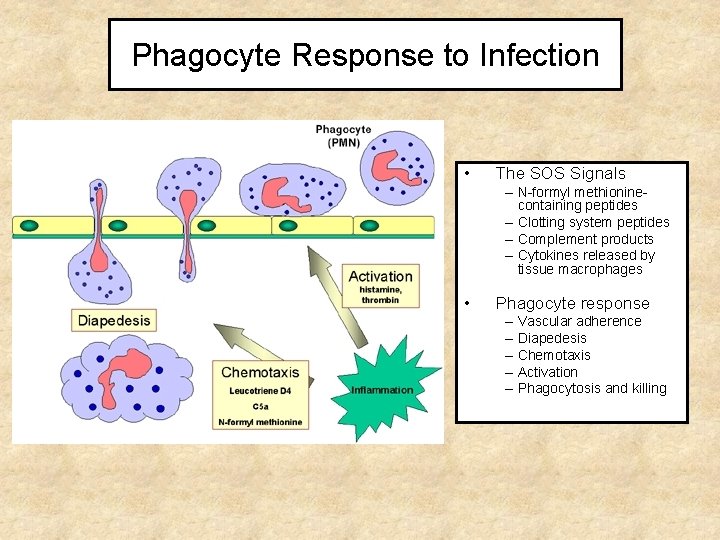
Phagocyte Response to Infection • The SOS Signals – N-formyl methioninecontaining peptides – Clotting system peptides – Complement products – Cytokines released by tissue macrophages • Phagocyte response – – – Vascular adherence Diapedesis Chemotaxis Activation Phagocytosis and killing
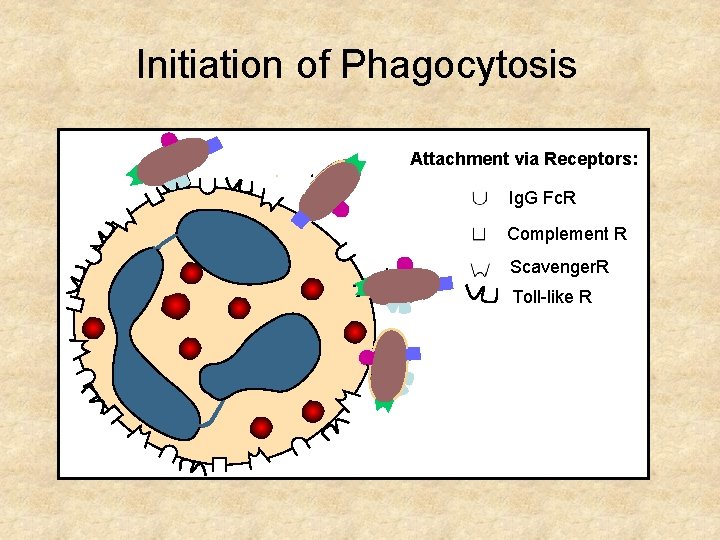
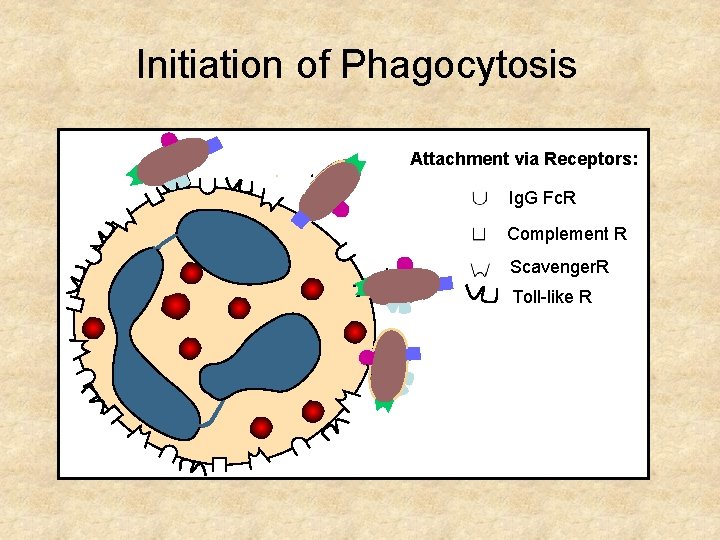
Initiation of Phagocytosis Attachment via Receptors: Ig. G Fc. R Complement R Scavenger. R Toll-like R
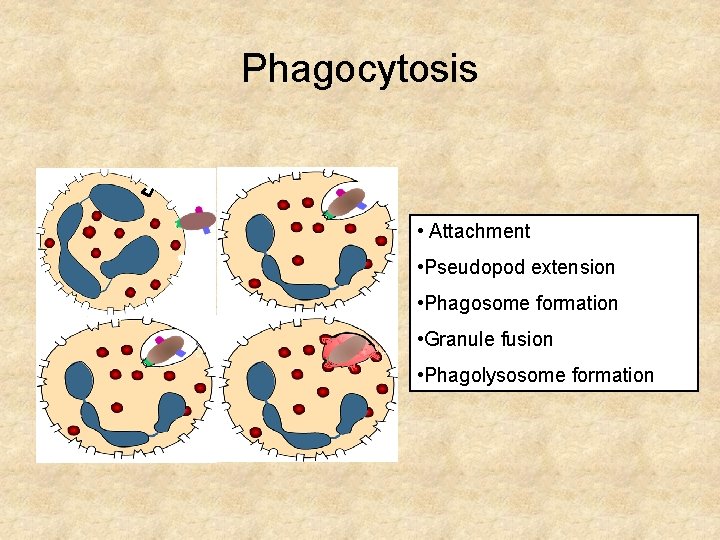
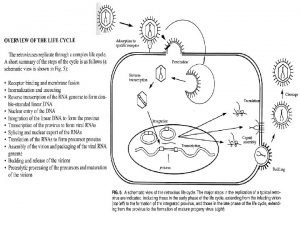
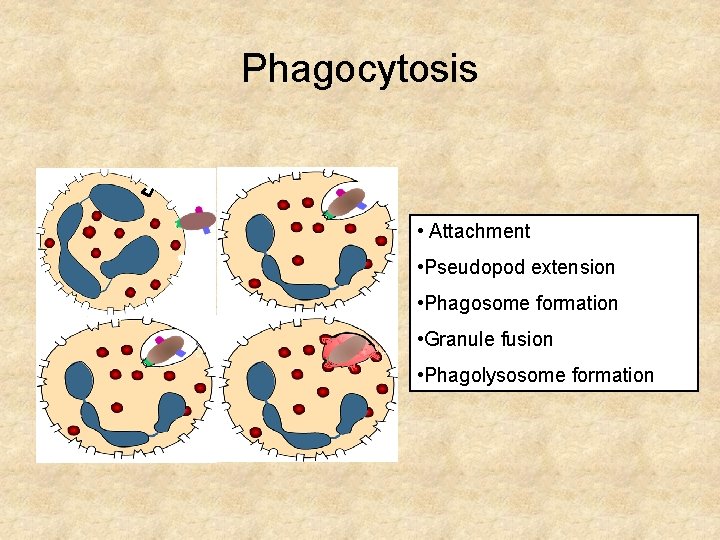
Phagocytosis • Attachment • Pseudopod extension • Phagosome formation • Granule fusion • Phagolysosome formation
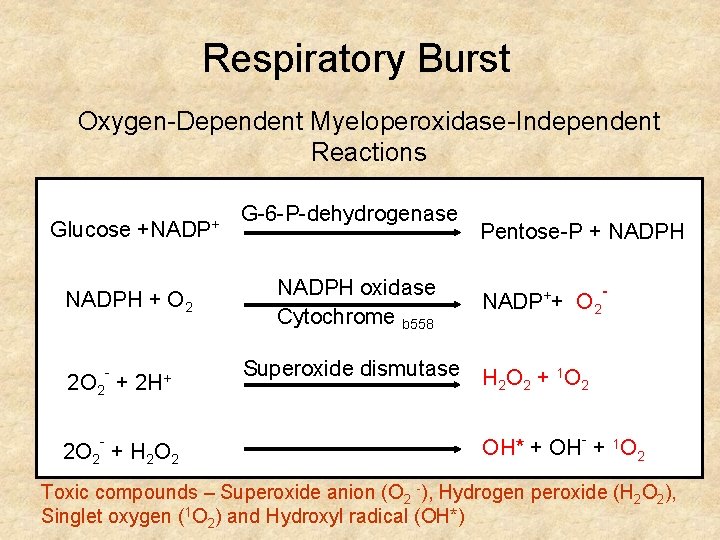
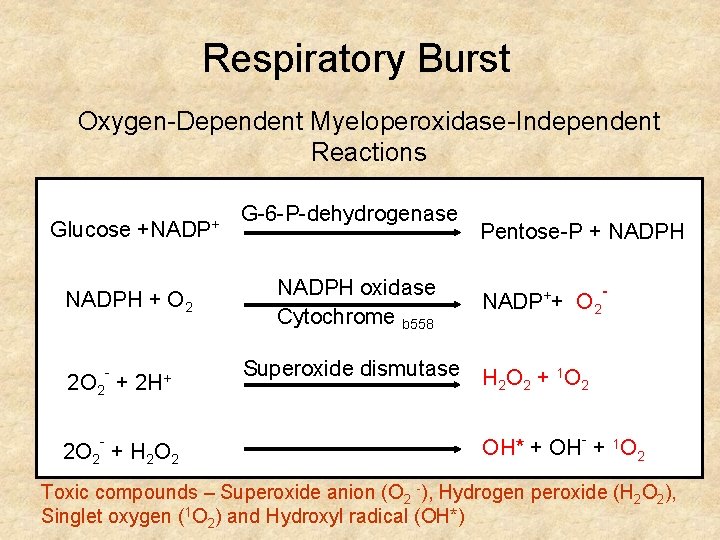
Respiratory Burst Oxygen-Dependent Myeloperoxidase-Independent Reactions Glucose +NADPH + O 2 2 O 2 - - + 2 H+ 2 O 2 + H 2 O 2 + G-6 -P-dehydrogenase NADPH oxidase Cytochrome b 558 Pentose-P + NADPH + NADP + O 2 - Superoxide dismutase H O + 1 O 2 2 2 OH* + OH- + 1 O 2 Toxic compounds – Superoxide anion (O 2 -), Hydrogen peroxide (H 2 O 2), Singlet oxygen (1 O 2) and Hydroxyl radical (OH*)
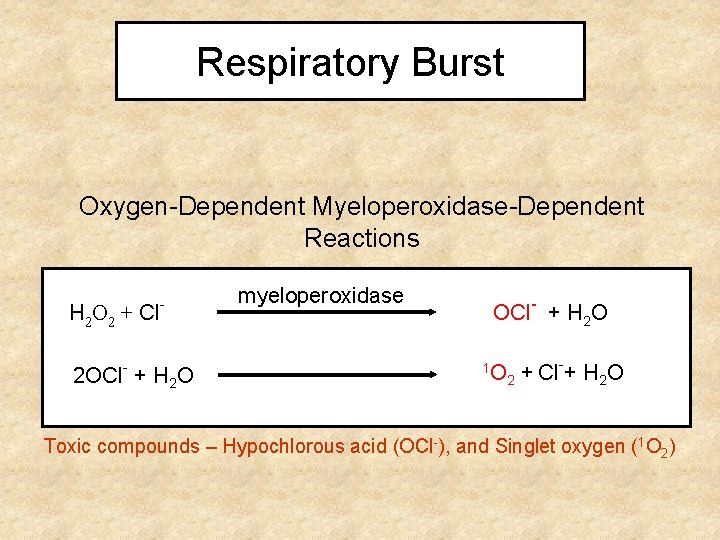
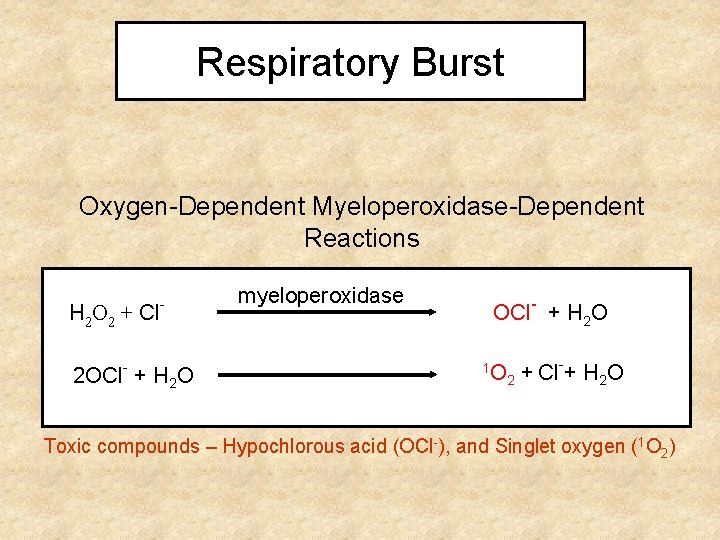
Respiratory Burst Oxygen-Dependent Myeloperoxidase-Dependent Reactions H 2 O 2 + Cl - 2 OCl- + H 2 O myeloperoxidase OCl- + H 2 O 1 O + Cl + H 2 O 2 Toxic compounds – Hypochlorous acid (OCl-), and Singlet oxygen (1 O 2)
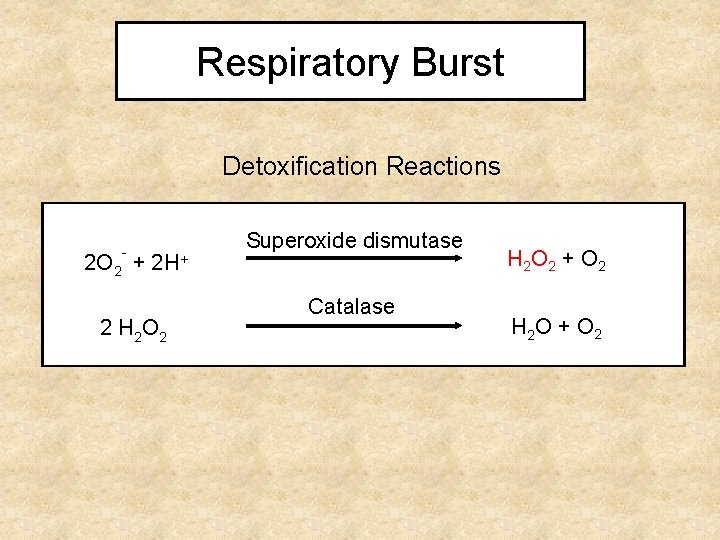
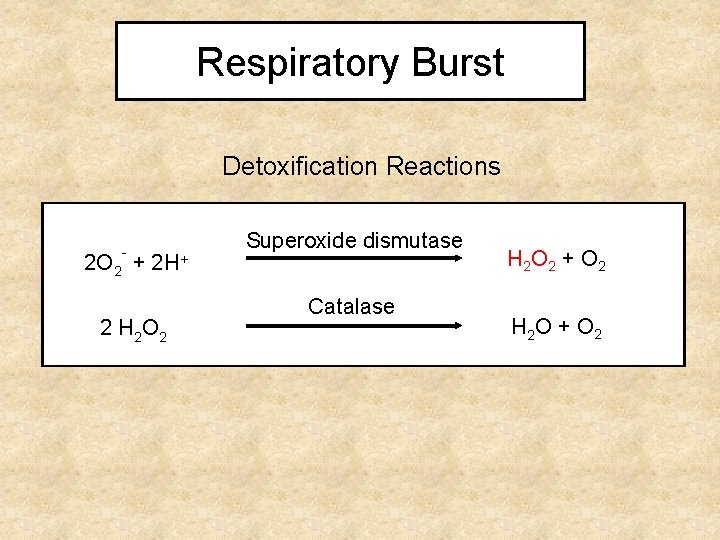
Respiratory Burst Detoxification Reactions - 2 O 2 + 2 H+ 2 H 2 O 2 Superoxide dismutase Catalase H 2 O 2 + O 2 H 2 O + O 2
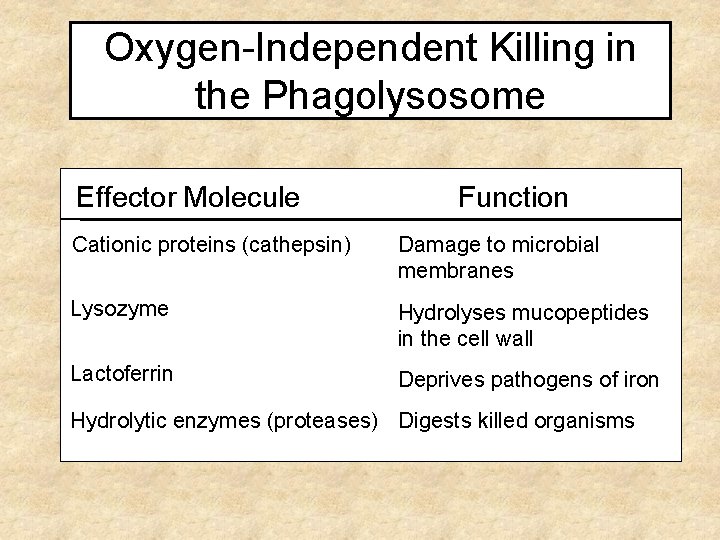
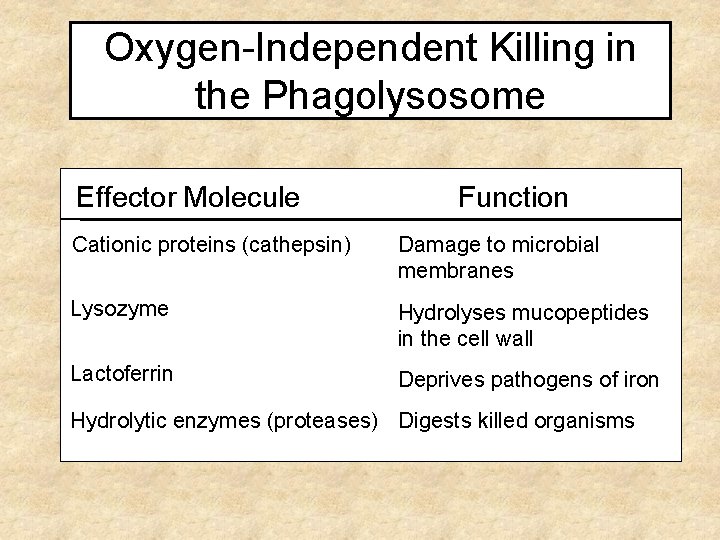
Oxygen-Independent Killing in the Phagolysosome Effector Molecule Function Cationic proteins (cathepsin) Damage to microbial membranes Lysozyme Hydrolyses mucopeptides in the cell wall Lactoferrin Deprives pathogens of iron Hydrolytic enzymes (proteases) Digests killed organisms
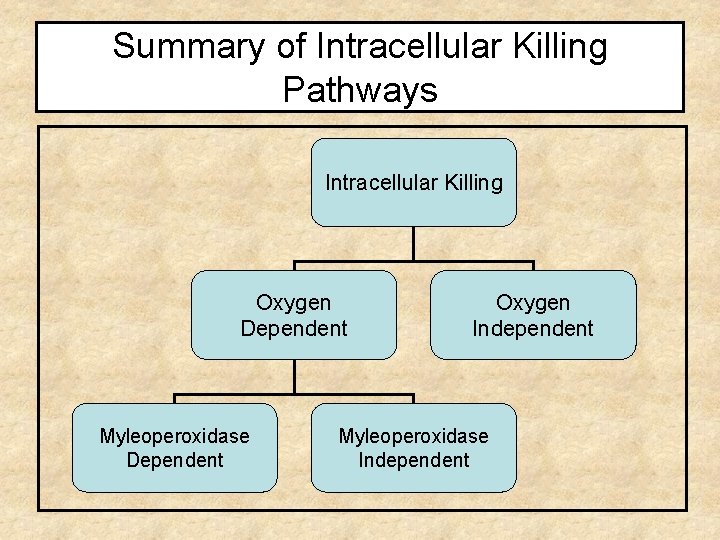
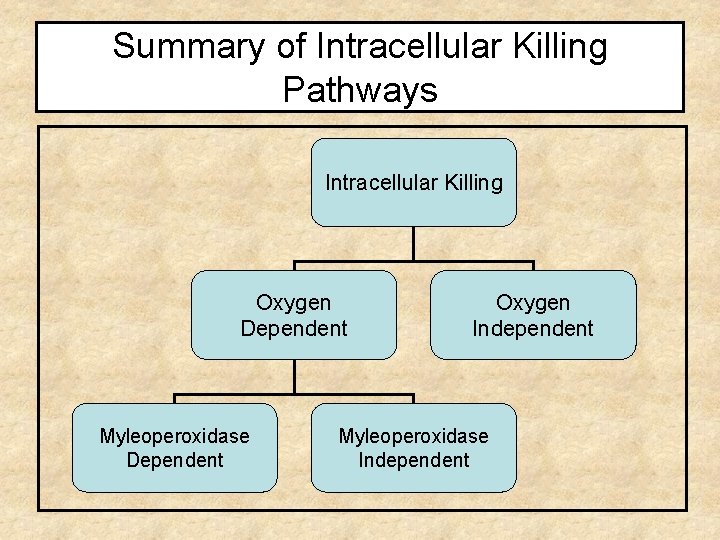
Summary of Intracellular Killing Pathways Intracellular Killing Oxygen Dependent Myleoperoxidase Dependent Oxygen Independent Myleoperoxidase Independent
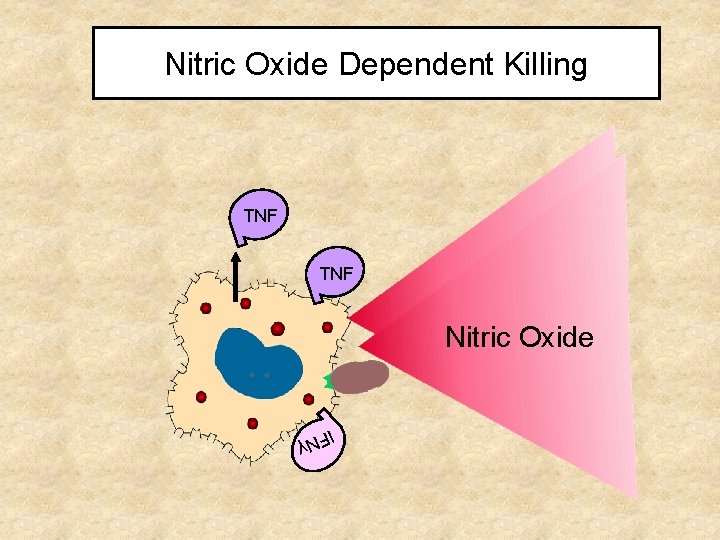
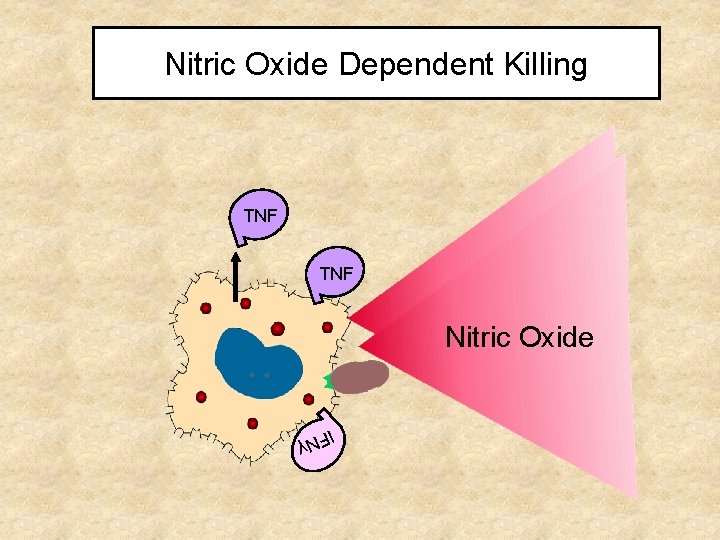
Nitric Oxide Dependent Killing TNF Nitric Oxide γ IFN
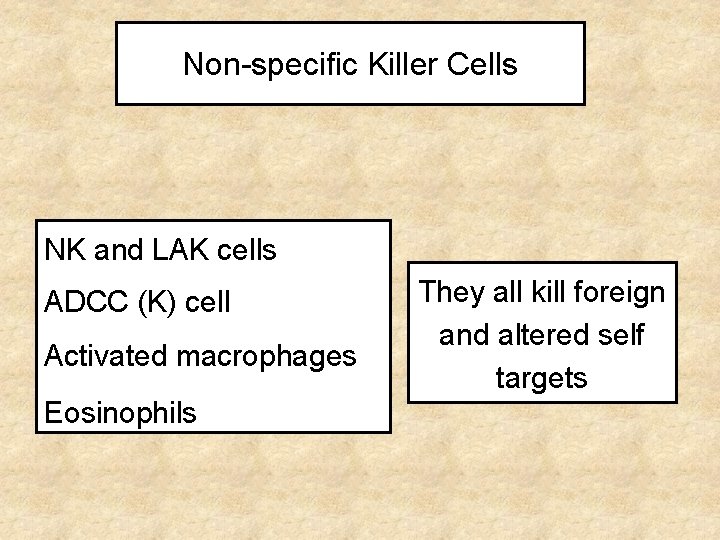
Non-specific Killer Cells NK and LAK cells ADCC (K) cell Activated macrophages Eosinophils They all kill foreign and altered self targets
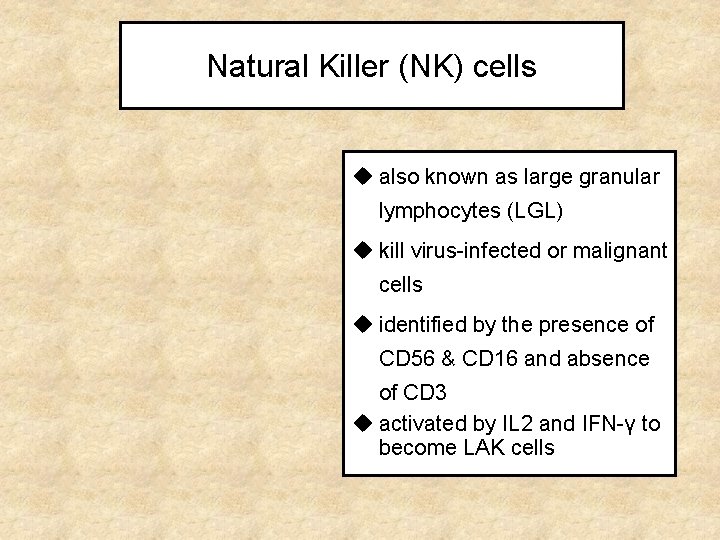
Natural Killer (NK) cells u also known as large granular lymphocytes (LGL) u kill virus-infected or malignant cells u identified by the presence of CD 56 & CD 16 and absence of CD 3 u activated by IL 2 and IFN-γ to become LAK cells
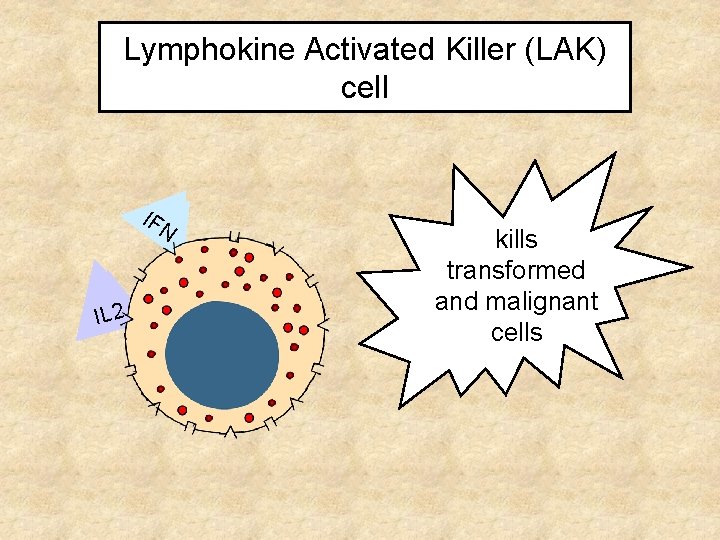
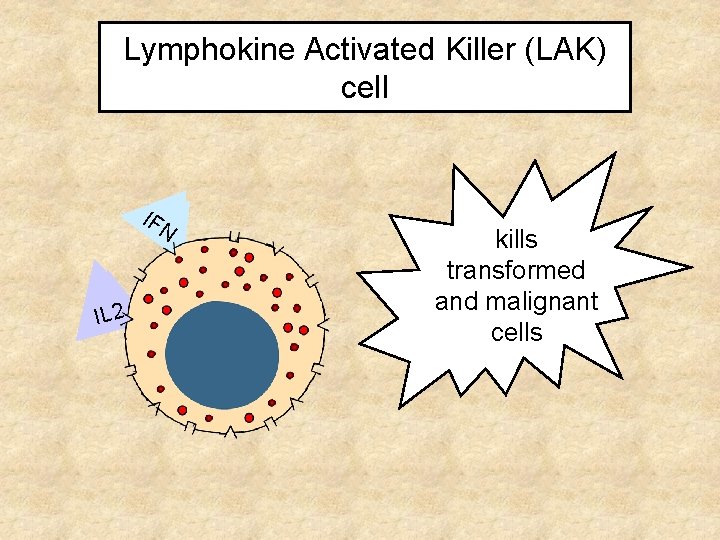
Lymphokine Activated Killer (LAK) cell IFIF NN IILL 22 kills transformed malignant and malignant cells
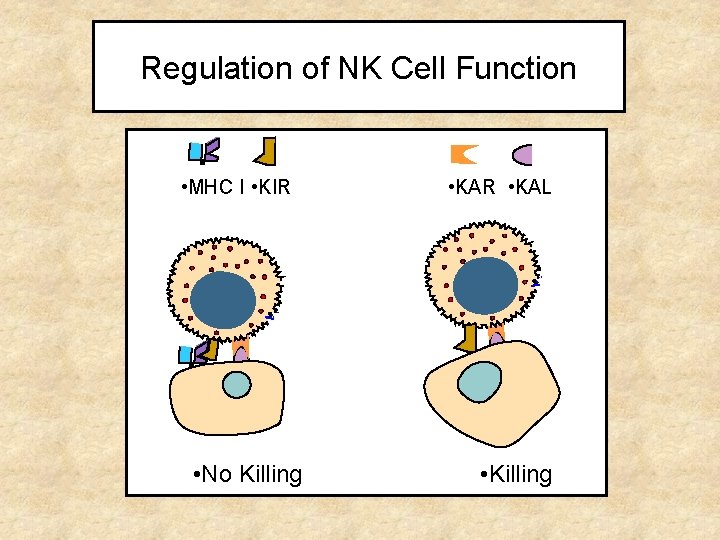
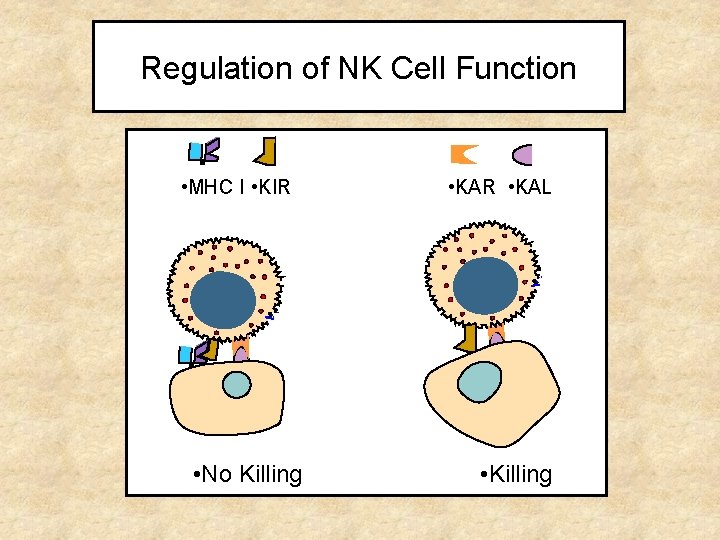
Regulation of NK Cell Function • MHC I • KIR • No Killing • KAR • KAL • Killing
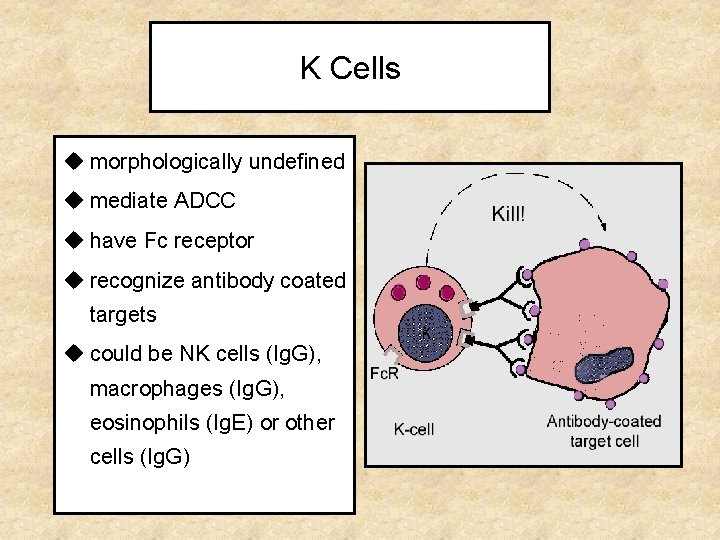
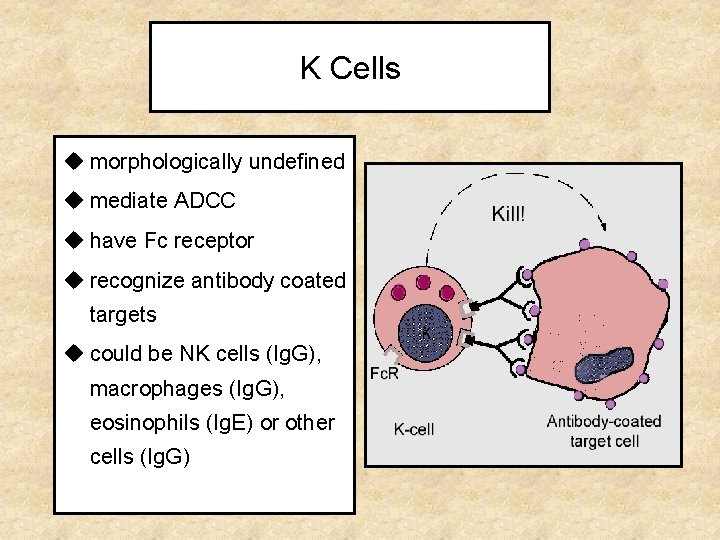
K Cells u morphologically undefined u mediate ADCC u have Fc receptor u recognize antibody coated targets u could be NK cells (Ig. G), macrophages (Ig. G), eosinophils (Ig. E) or other cells (Ig. G)
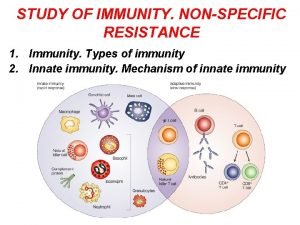
 Difference between acquired immunity and innate immunity
Difference between acquired immunity and innate immunity Specific vs nonspecific immunity
Specific vs nonspecific immunity Malt tonsils
Malt tonsils Primary immune response and secondary immune response
Primary immune response and secondary immune response Assis. prof.
Assis. prof. Innate immunity examples
Innate immunity examples Non specific innate immunity
Non specific innate immunity Innate immunity first line of defense
Innate immunity first line of defense Innate immunity
Innate immunity Innate immunity first line of defense
Innate immunity first line of defense Innate immunity first line of defense
Innate immunity first line of defense Innate immunity first line of defense
Innate immunity first line of defense Cell lysis complement system
Cell lysis complement system Innate immunity
Innate immunity Specific defense vs nonspecific defense
Specific defense vs nonspecific defense Specific vs nonspecific defense
Specific vs nonspecific defense Abnormal vq scan images
Abnormal vq scan images Concave vs convex ekg
Concave vs convex ekg Nonspecific host defense mechanism
Nonspecific host defense mechanism Nonspecific vs specific defense
Nonspecific vs specific defense What is the third line of defense in the immune system
What is the third line of defense in the immune system Flow chart of wbc
Flow chart of wbc Third line of defense immune system
Third line of defense immune system Chapter 35 immune system and disease
Chapter 35 immune system and disease Primary vs secondary immune response
Primary vs secondary immune response Ap biology immune system
Ap biology immune system Lesson 12 blood and immune system
Lesson 12 blood and immune system Lesson 12 blood and immune system
Lesson 12 blood and immune system Immune system lymph nodes
Immune system lymph nodes Immunity assignment slideshare
Immunity assignment slideshare Overreactions of the immune system
Overreactions of the immune system Lymphatic vs immune system
Lymphatic vs immune system Lymphatic vs immune system
Lymphatic vs immune system Defination of tuberculosis
Defination of tuberculosis