INFORMING SHARED CLINICAL CARE SHARED RECORD PROFESSIONAL GUIDANCE

- Slides: 16
INFORMING SHARED CLINICAL CARE - SHARED RECORD PROFESSIONAL GUIDANCE PROJECT RCGP Informatics Group – June 2009 http: //www. rcgp. org. uk/get_involved/informatics_group/shared_record_professional_guidance. aspx
Purpose & scope • The purpose of the Shared Record Professional Guidance (SRPG) project was to develop a set of professionally led guidelines that would consider the governance, medico-legal and patient safety consequences of Shared Electronic Patient Record (SEPR) systems in the primary care domain. • Scope is local detailed care record in the form of current ESP (GPSo. C) and LSP Primary Care IT systems. • We recognised from the beginning that “information sharing” and “shared electronic patient records” are not synonymous.
Key questions for this project to address were; – What are the purposes of shared electronic patient record systems (s. DCRs)? – How can these requirements be delivered safely? – What are the principles and practice that ensure clarity, safety and continuity – At what level does responsibility for shared electronic patient record system governance lie?
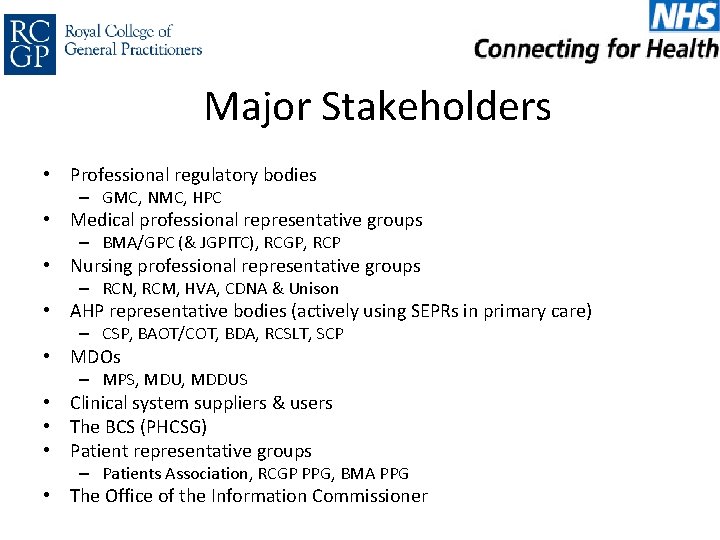
Major Stakeholders • Professional regulatory bodies – GMC, NMC, HPC • Medical professional representative groups – BMA/GPC (& JGPITC), RCGP, RCP • Nursing professional representative groups – RCN, RCM, HVA, CDNA & Unison • AHP representative bodies (actively using SEPRs in primary care) – CSP, BAOT/COT, BDA, RCSLT, SCP • MDOs – MPS, MDU, MDDUS • Clinical system suppliers & users • The BCS (PHCSG) • Patient representative groups – Patients Association, RCGP PPG, BMA PPG • The Office of the Information Commissioner
The reference report 1. The national context a) Review current/planned SEPR systems 2. Information governance a) The law, professional guidance & consent 3. Literature review 4. Clinical scenarios 5. Stakeholder survey
The literature review • This review aimed to identify studies on shared records, the key topics arising in sharing of data between healthcare professionals and summarise the literature according to topics. • We did not find a nationally successful shared electronic patient record, although the Emergency Care Summary in Scotland comes close to this. • The benefits of sharing patient data using an EPR have been addressed in the 33 studies that we reviewed. Improvements in the quality of care and a reduction in medical errors are the two main benefits, which support the implementation of a shared EPR. We found that preserving the privacy of patient data was the most important factor determining the patient’s acceptance of EPRs. • However, anticipated improvements in efficiency, safety, equity and costeffectiveness of care have not been realised in the few rigorous studies on a large scale anywhere in the world.
The clinical scenarios • There is uncertainty about what is meant by record sharing and thus in defining different types of shared record. We thought that looking at a small number of scenarios in detail would help to clarify matters. focus on inter-professional communication Information transfer on its own is not the same as communication Accurate recording of data is not sufficient to support shared care of a patient responsibility on every clinician to inform the practice of other professionals who may be involved, and to inform the patient too – Both practice, i. e. ways of working, and information systems need to be organised in parallel to facilitate effective shared care – contemporary communication between the professionals involved is more pertinent to patient care than historical archives of information – The primary care record contains items that are social rather than medical. Their inclusion in a shared medical record requires consideration. – –
The stakeholder survey • • • The main aim of the second phase of the stakeholder consultation process was to develop a set of professionally endorsed principles that would help define the clinical and information governance requirements for shared DCRs. Our aim was to build a consensus around the principles where there are high levels of agreement between the different stakeholder organisations that would inform the guidelines development process. The overall response rate to the survey was very high from the full range of stakeholder groups identified by the project team (40/43 = 93%). There was a clear trend from patient organisations suggesting that patients do want to actively participate in sharing decisions Overall level of agreement between AHPs, nurses and doctors was high The professional regulatory body responses were generally consistent throughout the survey, though the medical defence organisations were rather less so
The main report 1. 2. 3. 4. 5. Introduction, project background, methods Discussion & recommendations What are the purposes of shared DCRs? How can these requirements be delivered safely? What are the principles and practice that ensure clarity, safety & continuity? 6. At what level does responsibility for SEPR/s. DCR governance lie?
Discussion – purposes of SEPRs • The literature review concluded that improvements in the quality of care and a reduction in medical errors are the two main benefits, which support the implementation of a shared EPR. • The clinical scenarios demonstrated that clinical communication between health professionals is likely to be central to the concept of SEPRs/s. EHRs, to inform and shape the practice of colleagues • The stakeholder survey showed high levels of agreement across all respondents that appropriate information sharing is essential to the safe, effective provision of care

Discussion – deliver requirements safely • A community using a shared electronic health record needs to establish governance rules and processes that ensure the clear allocation of responsibility and define the rules and mechanisms by which responsibility can be transferred. The rules need to be clear on who has responsibility for content and for action based on the record content. • Maintaining good quality records that are complete, accurate and up-to-date requires significant effort both in their creation and ongoing maintenance. Those using records need education and training to understand the value in making this effort and to equip them with the skills to do so.
Discussion – principles & practice • Areas to be addressed – Semantics – “acts of translation”, language, interpretation, context – Errors - & differences of opinion reconciliation – Provenance – identify the originator or editor of entries – Relevance – different views, structured communications “Human communication is fundamental to the process of informing and cannot be substituted by a combination of computer algorithm and data bucket”
Discussion – clinical responsibility It is clear from the contents of the report so far, that responsibility for safe and effective governance of s. DCR systems exists at many levels and includes: • • • Government Clinical professions Health organisations Health professionals Patients
Recommendations - general • This report represents the first steps in developing professional guidance about the use of SEPR/s. DCR systems to support shared clinical care. • We have outlined a governance framework within which SEPR/s. DCRs should operate and drafted governance principles for such systems. • We have described and developed governance guidelines and principles to inform and support the clinical practice of health professionals working with shared records. • We believe that appropriate information sharing is essential to the safe, effective provision of care in a modern health service and implementing the principles & guidance in this report could increase public and professional confidence in these systems.
SRPG final report - outputs • Short main report • Main findings • 16 principles • 2 requirements • Reference report • • IG review Literature review Clinical scenarios Stakeholder survey • Quick reference guide
Other issues to consider • Extending consultation to organisations not included in this project? • Extending the scope of the guidance? – Mental health services – Child health & safety – Multi-agency care (e. g. SAP) – End-of life care