HIV Genetic Diversity Consequences for diagnosis viral load

- Slides: 26
HIV Genetic Diversity Consequences for diagnosis, viral load and treatment monitoring Prof François SIMON & Jean - Christophe PLANTIER University Paris Diderot - Hospital Saint Louis – Paris 10
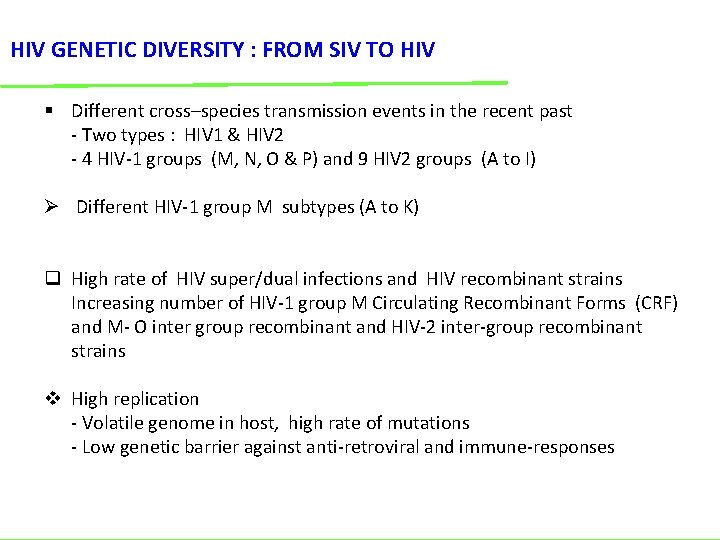
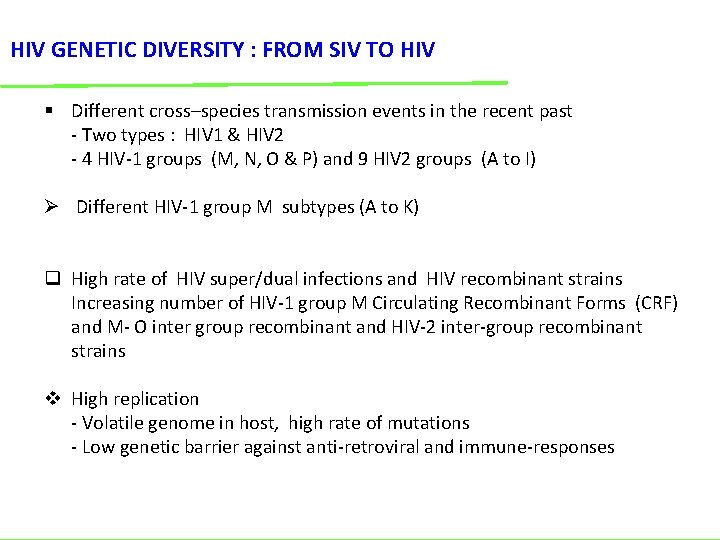
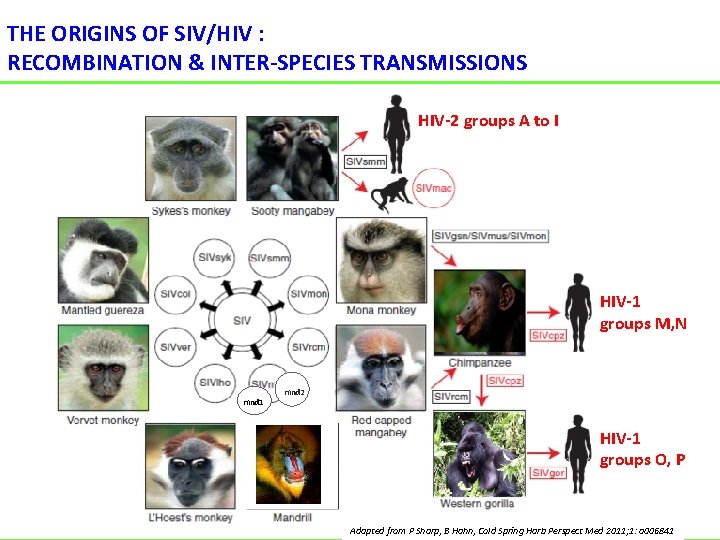
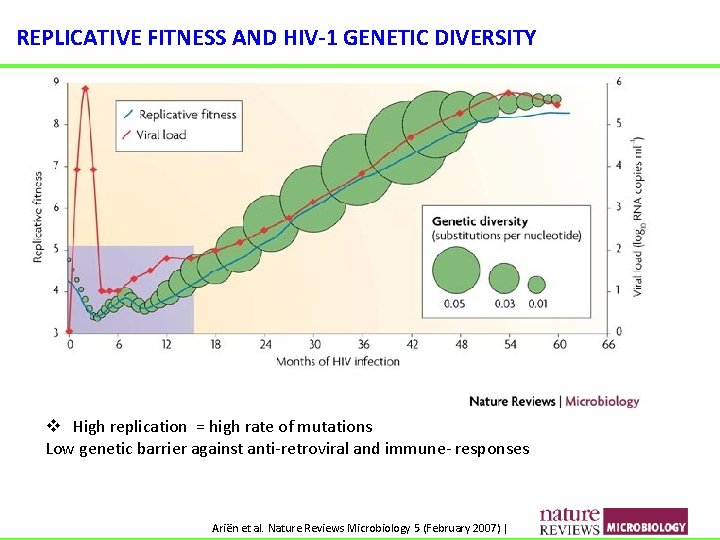
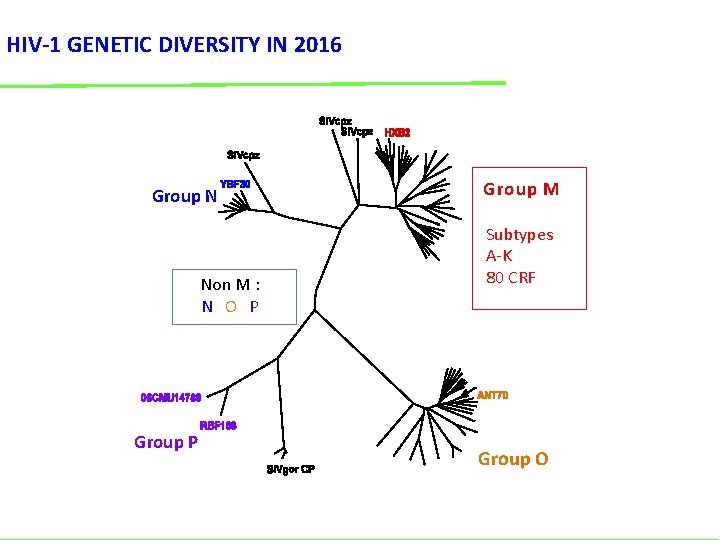
HIV GENETIC DIVERSITY : FROM SIV TO HIV § Different cross–species transmission events in the recent past - Two types : HIV 1 & HIV 2 - 4 HIV-1 groups (M, N, O & P) and 9 HIV 2 groups (A to I) Ø Different HIV-1 group M subtypes (A to K) q High rate of HIV super/dual infections and HIV recombinant strains Increasing number of HIV-1 group M Circulating Recombinant Forms (CRF) and M- O inter group recombinant and HIV-2 inter-group recombinant strains v High replication - Volatile genome in host, high rate of mutations - Low genetic barrier against anti-retroviral and immune-responses
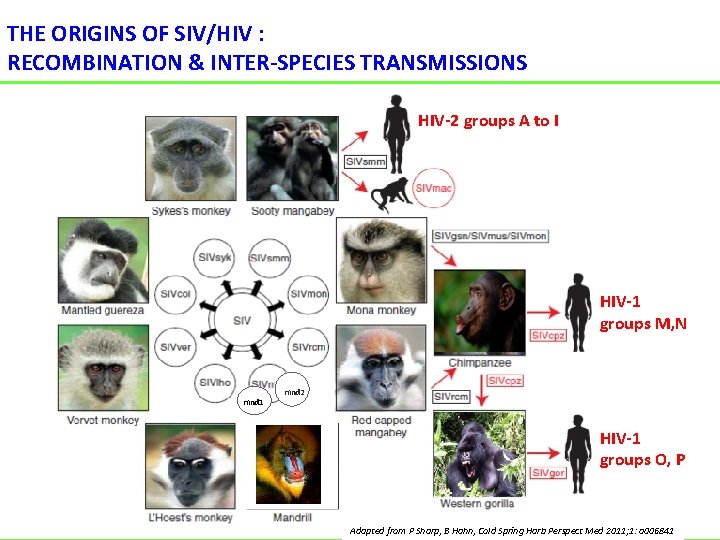
THE ORIGINS OF SIV/HIV : RECOMBINATION & INTER-SPECIES TRANSMISSIONS HIV-2 groups A to I HIV-1 groups M, N mnd 1 mnd 2 HIV-1 groups O, P Adapted from P Sharp, B Hahn, Cold Spring Harb Perspect Med 2011; 1: a 006841
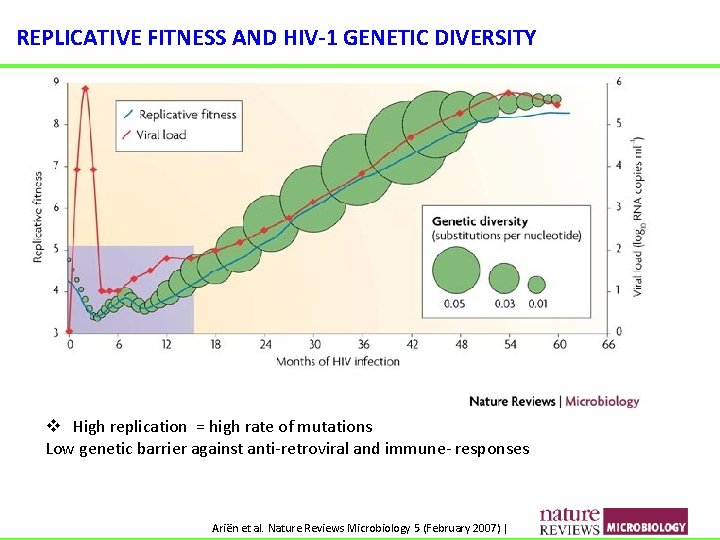
REPLICATIVE FITNESS AND HIV-1 GENETIC DIVERSITY v High replication = high rate of mutations Low genetic barrier against anti-retroviral and immune- responses Ariën et al. Nature Reviews Microbiology 5 (February 2007) |
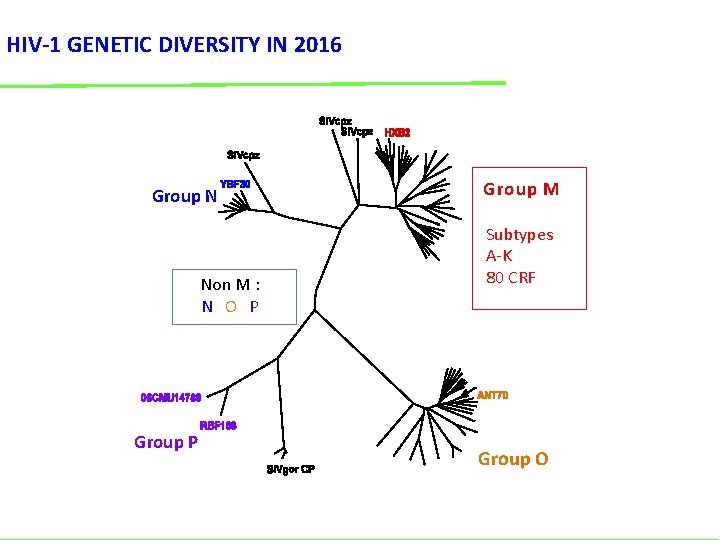
HIV-1 GENETIC DIVERSITY IN 2016 Group N Non M : N O P Group M Subtypes A-K 80 CRF Group O
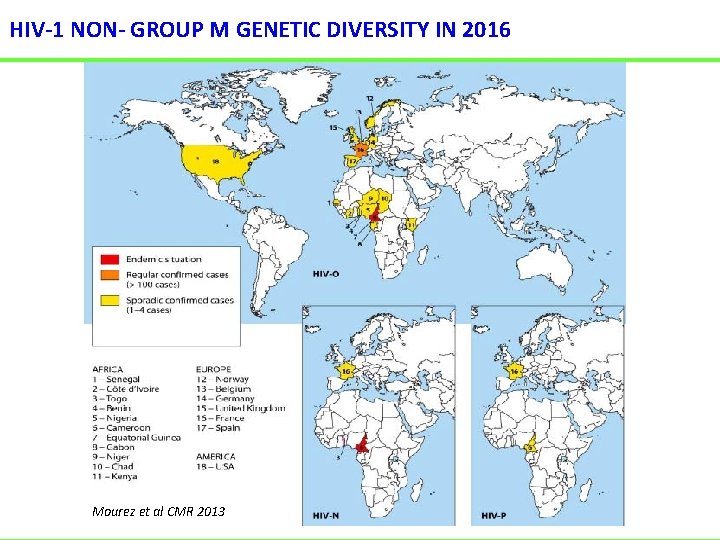
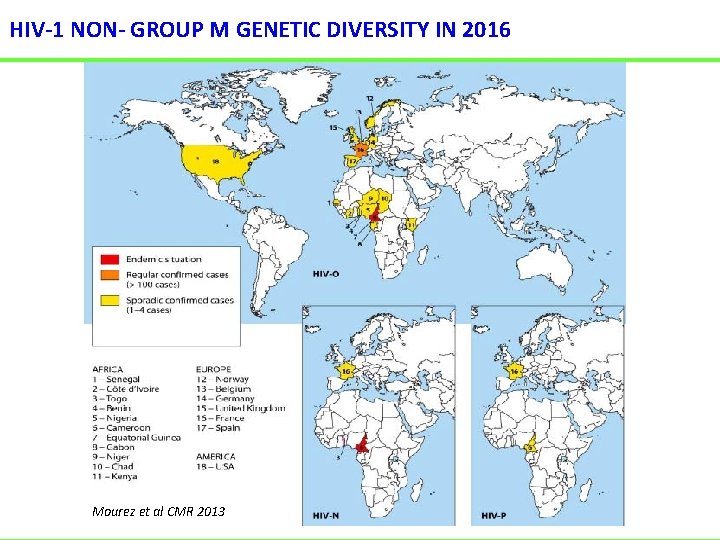
HIV-1 NON- GROUP M GENETIC DIVERSITY IN 2016 Mourez et al CMR 2013
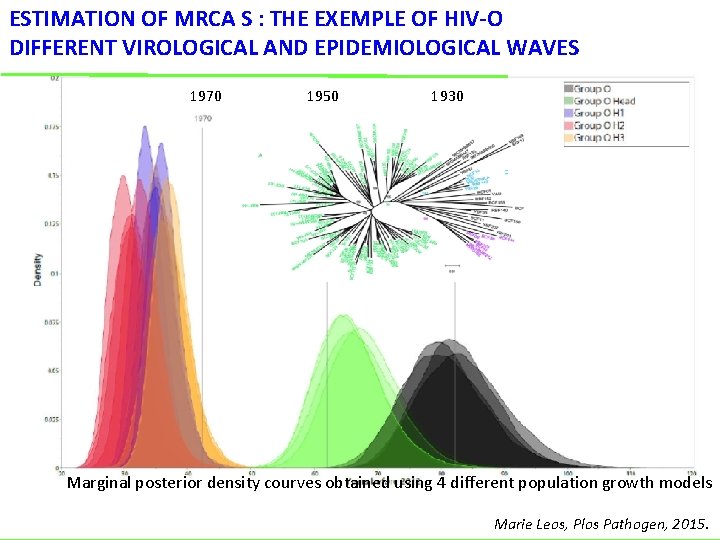
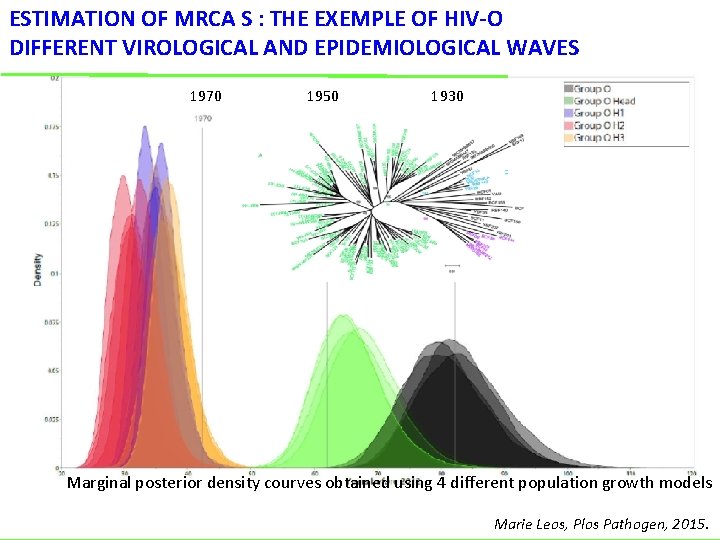
ESTIMATION OF MRCA S : THE EXEMPLE OF HIV-O DIFFERENT VIROLOGICAL AND EPIDEMIOLOGICAL WAVES 1970 1950 1930 Marginal posterior density courves obtained using 4 different population growth models Marie Leos, Plos Pathogen, 2015.
HIV-O MAIN CHARACTERISTICS • 1% of HIV-infected patients in Cameroon 143 cases diagnosed in France mainly in Cameroonian Pts • Pathogenic, sexual and vertical transmission documented • Lower replicativity than HIV-1 group M • 70% of the HIV-O are naturally resistant (Y 181 C) to NNRTI according to the phylogenetic position • Sensitive to enfuvirtide in vitro and in vivo despite N 42 D in 100%
HIV-N MAIN CHARACTERISTICS • Group N is close from the SIV cpz : cross species transmission occurring in the last decades • Pathogenic, sexual and vertical transmission documented • Low prevalence but strain trafficking outside of Cameroon, in Europe • Sensitive to all the ARV like group M strains • Low epidemic (to date) • a lower transmission rate ?
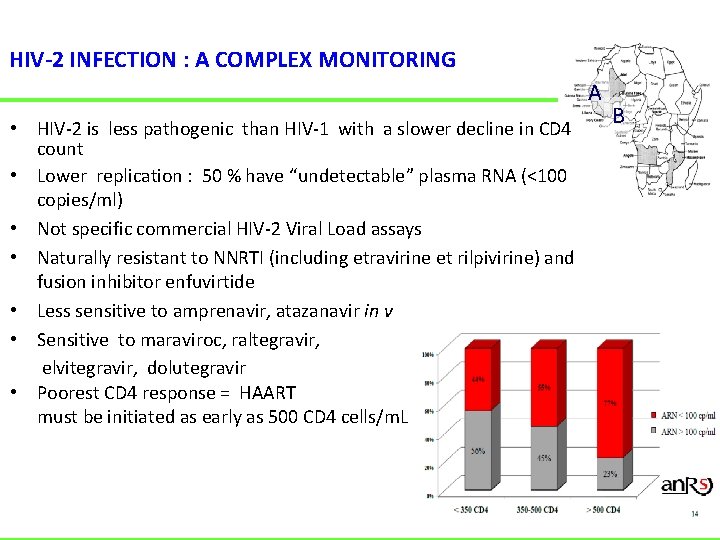
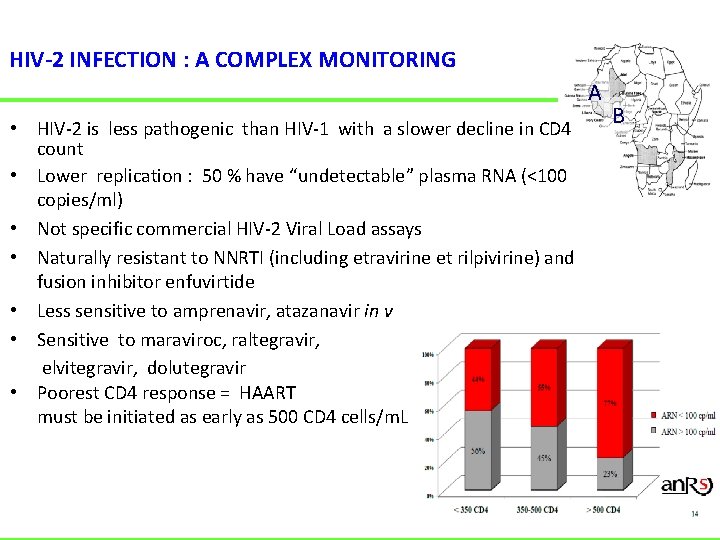
HIV-2 INFECTION : A COMPLEX MONITORING A • HIV-2 is less pathogenic than HIV-1 with a slower decline in CD 4 count • Lower replication : 50 % have “undetectable” plasma RNA (<100 copies/ml) • Not specific commercial HIV-2 Viral Load assays • Naturally resistant to NNRTI (including etravirine et rilpivirine) and fusion inhibitor enfuvirtide • Less sensitive to amprenavir, atazanavir in vitro • Sensitive to maraviroc, raltegravir, elvitegravir, dolutegravir • Poorest CD 4 response = HAART must be initiated as early as 500 CD 4 cells/m. L B
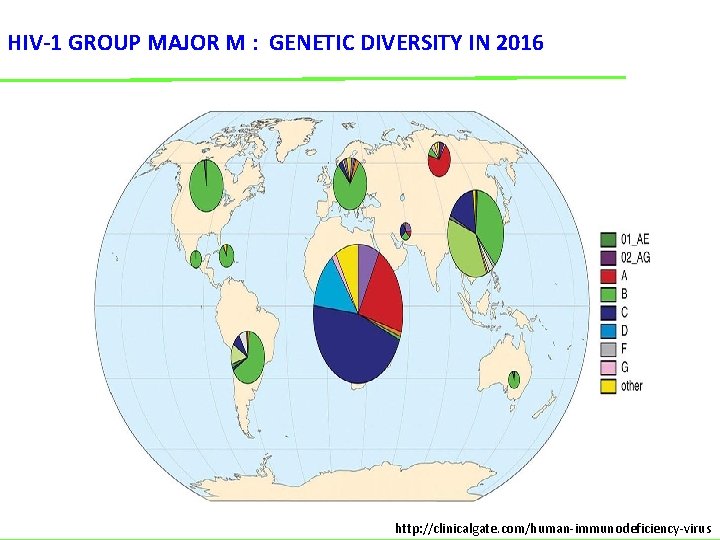
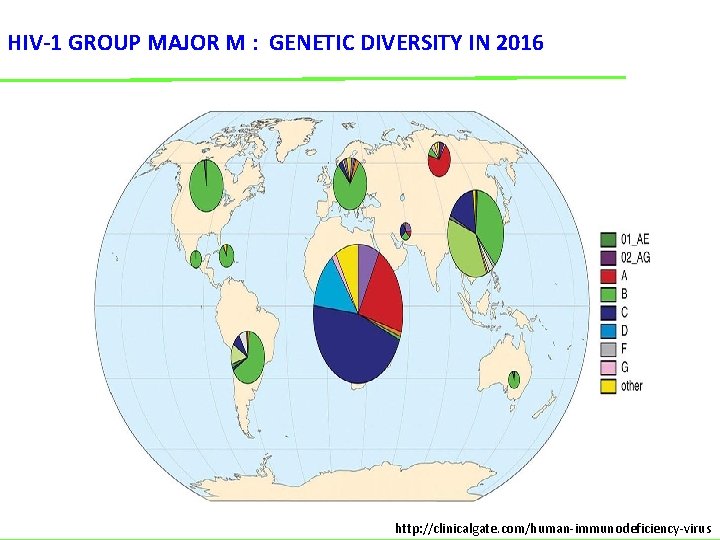
HIV-1 GROUP MAJOR M : GENETIC DIVERSITY IN 2016 http: //clinicalgate. com/human-immunodeficiency-virus
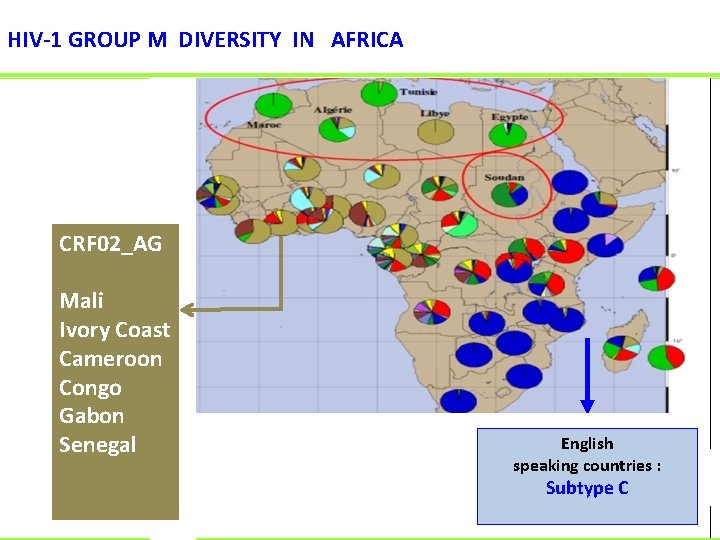
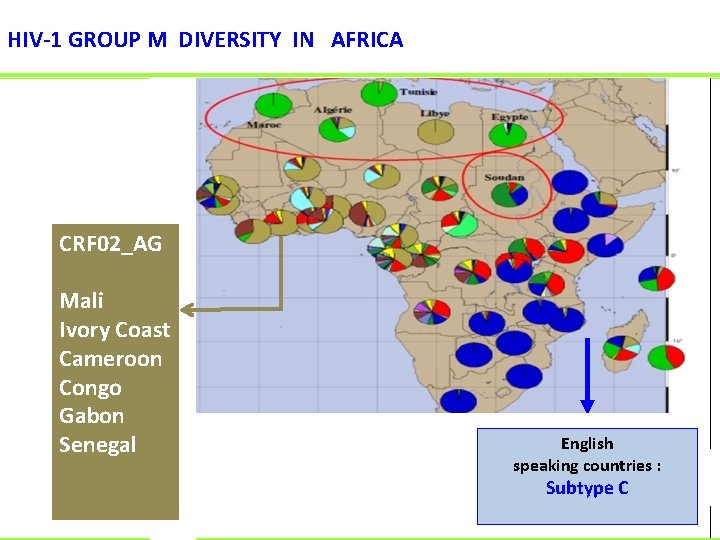
HIV-1 GROUP M DIVERSITY IN AFRICA CRF 02_AG Mali Ivory Coast Cameroon Congo Gabon Senegal D G English speaking countries : Subtype C FC Javaugue
HIV-1 group M diversity Main consequences in 2016 • Detection of HIV-1 non B during primary infection • Viral Load miss-identification • Drug sensitivity
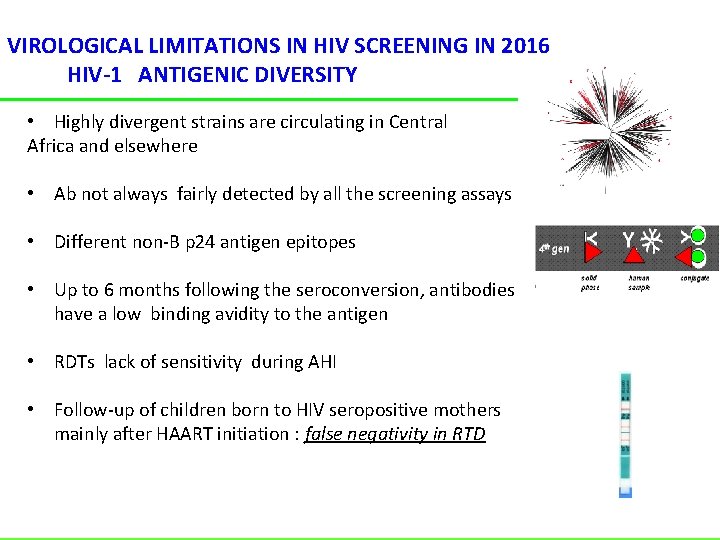
VIROLOGICAL LIMITATIONS IN HIV SCREENING IN 2016 HIV-1 ANTIGENIC DIVERSITY • Highly divergent strains are circulating in Central Africa and elsewhere • Ab not always fairly detected by all the screening assays • Different non-B p 24 antigen epitopes • Up to 6 months following the seroconversion, antibodies have a low binding avidity to the antigen • RDTs lack of sensitivity during AHI • Follow-up of children born to HIV seropositive mothers mainly after HAART initiation : false negativity in RTD
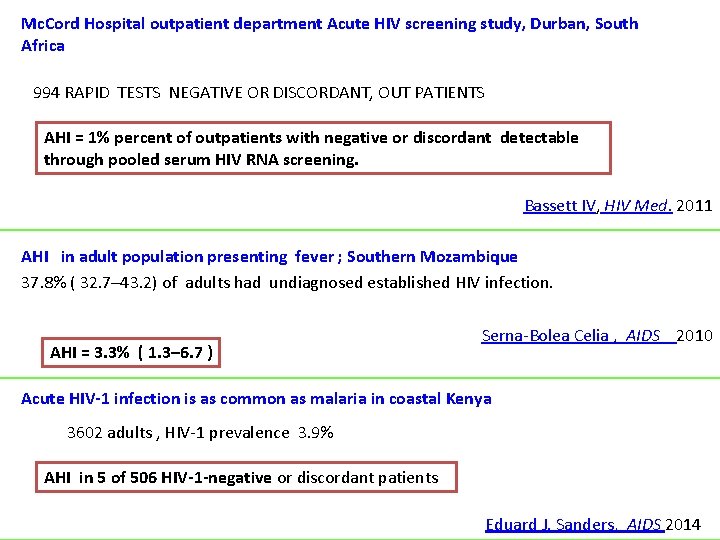
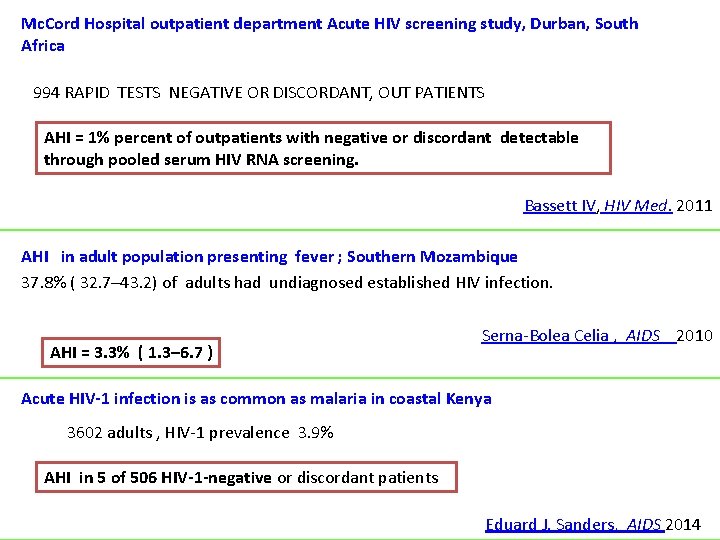
Mc. Cord Hospital outpatient department Acute HIV screening study, Durban, South Africa 994 RAPID TESTS NEGATIVE OR DISCORDANT, OUT PATIENTS AHI = 1% percent of outpatients with negative or discordant detectable through pooled serum HIV RNA screening. Bassett IV, HIV Med. 2011 AHI in adult population presenting fever ; Southern Mozambique 37. 8% ( 32. 7– 43. 2) of adults had undiagnosed established HIV infection. AHI = 3. 3% ( 1. 3– 6. 7 ) Serna-Bolea Celia , AIDS 2010 Acute HIV-1 infection is as common as malaria in coastal Kenya 3602 adults , HIV-1 prevalence 3. 9% AHI in 5 of 506 HIV-1 -negative or discordant patients Eduard J. Sanders, AIDS 2014
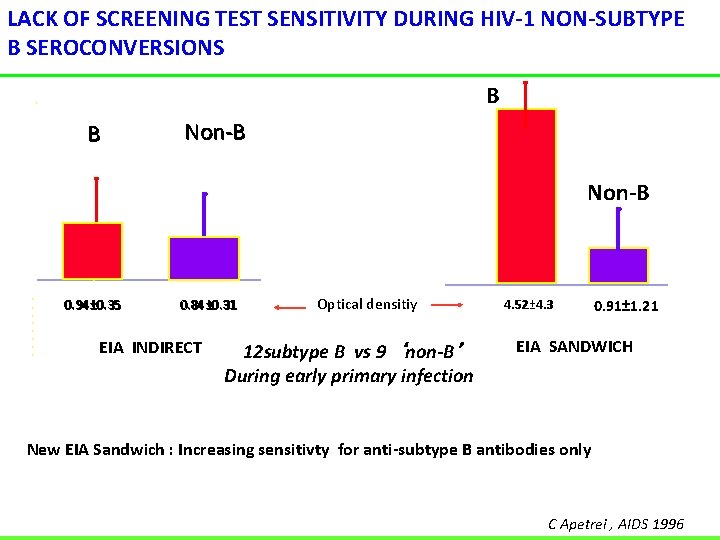
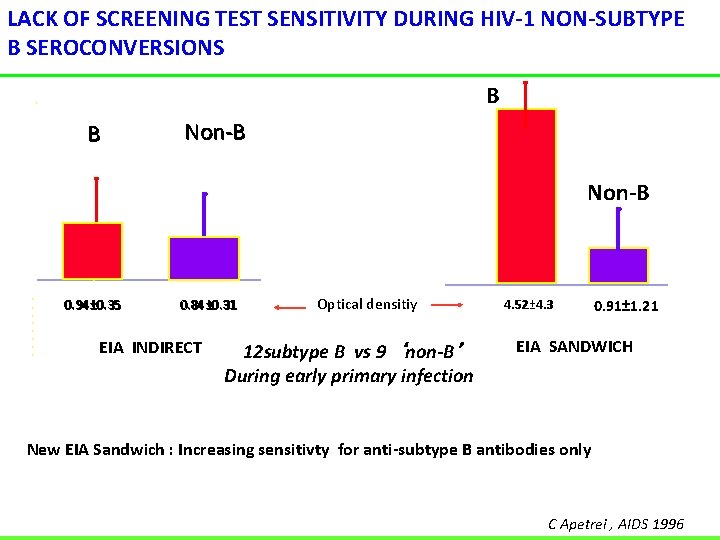
LACK OF SCREENING TEST SENSITIVITY DURING HIV-1 NON-SUBTYPE B SEROCONVERSIONS B B Non-B 0. 94± 0. 35 0. 84± 0. 31 EIA INDIRECT Optical densitiy 12 subtype B vs 9 ‘non-B’ During early primary infection 4. 52± 4. 3 0. 91± 1. 21 EIA SANDWICH New EIA Sandwich : Increasing sensitivty for anti-subtype B antibodies only C Apetrei , AIDS 1996
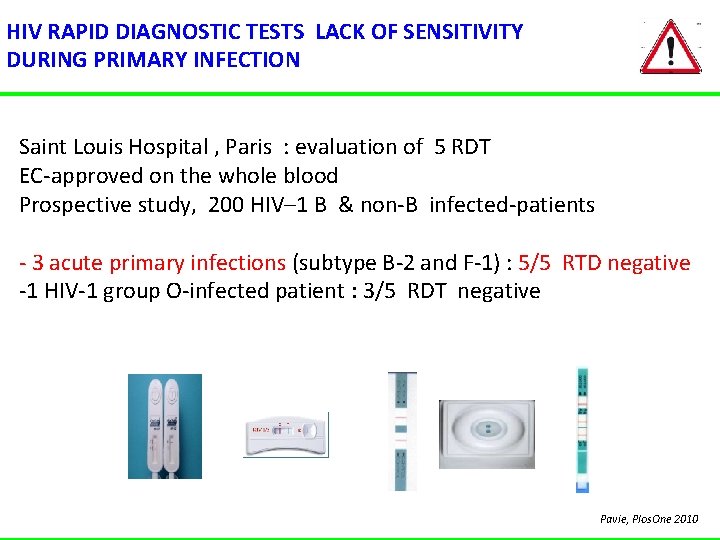
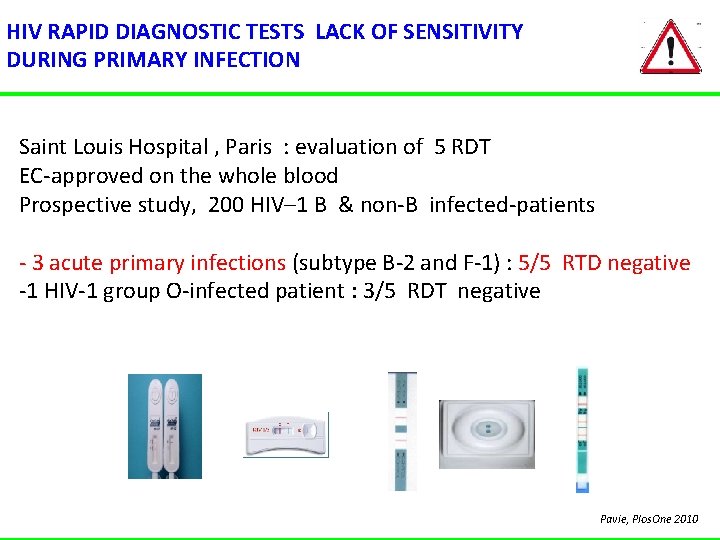
HIV RAPID DIAGNOSTIC TESTS LACK OF SENSITIVITY DURING PRIMARY INFECTION Saint Louis Hospital , Paris : evaluation of 5 RDT EC-approved on the whole blood Prospective study, 200 HIV– 1 B & non-B infected-patients - 3 acute primary infections (subtype B-2 and F-1) : 5/5 RTD negative -1 HIV-1 group O-infected patient : 3/5 RDT negative Pavie, Plos. One 2010
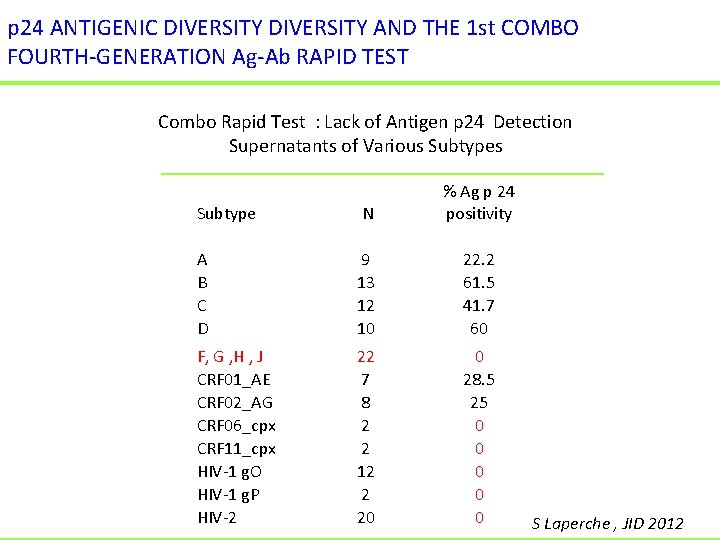
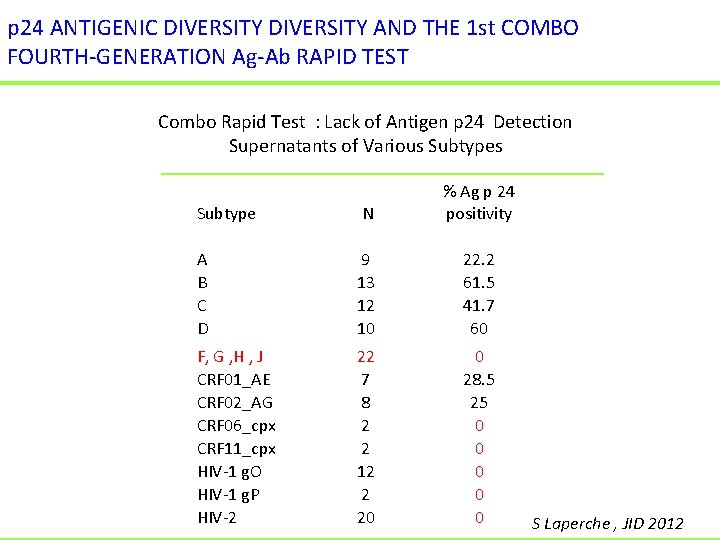
p 24 ANTIGENIC DIVERSITY AND THE 1 st COMBO FOURTH-GENERATION Ag-Ab RAPID TEST Combo Rapid Test : Lack of Antigen p 24 Detection Supernatants of Various Subtype N % Ag p 24 positivity A B C D 9 13 12 10 22. 2 61. 5 41. 7 60 F, G , H , J CRF 01_AE CRF 02_AG CRF 06_cpx CRF 11_cpx HIV-1 g. O HIV-1 g. P HIV-2 22 7 8 2 2 12 2 20 0 28. 5 25 0 0 0 S Laperche , JID 2012

VIRAL LOAD ASSAYS AND HIV DIVERSITY IN 2016 • • • 20 years for viral load Previously based only onto subtype B quantification High sensitivity performances (LOD 20 copies/m. L) Overpassing (now) the genomic diversity Random, Automation high throughput or unitary
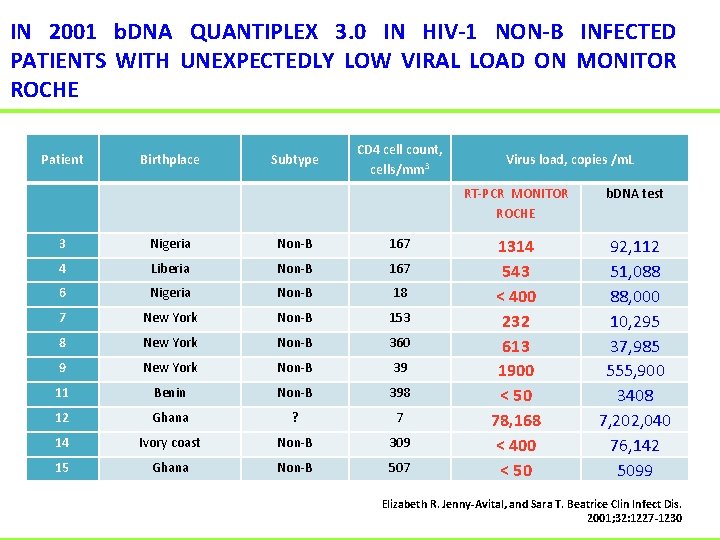
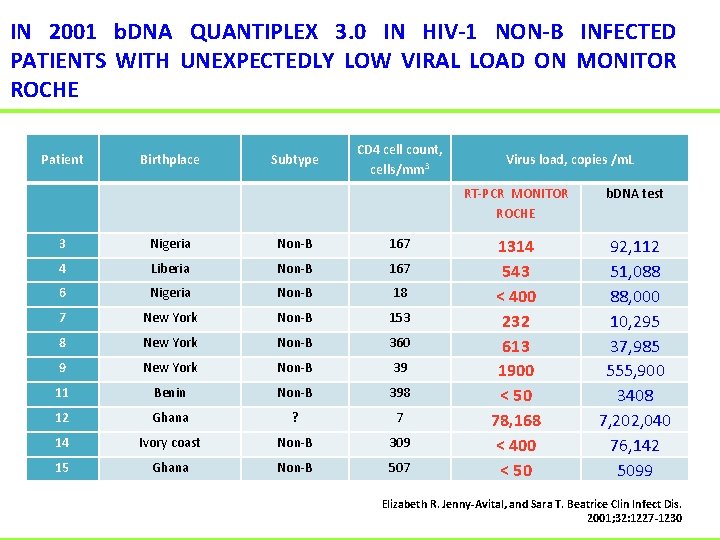
IN 2001 b. DNA QUANTIPLEX 3. 0 IN HIV-1 NON-B INFECTED PATIENTS WITH UNEXPECTEDLY LOW VIRAL LOAD ON MONITOR ROCHE Patient Birthplace Subtype CD 4 cell count, cells/mm 3 3 Nigeria Non-B 167 4 Liberia Non-B 167 6 Nigeria Non-B 18 7 New York Non-B 153 8 New York Non-B 360 9 New York Non-B 39 11 Benin Non-B 398 12 Ghana ? 7 14 Ivory coast Non-B 309 15 Ghana Non-B 507 Virus load, copies /m. L RT-PCR MONITOR ROCHE b. DNA test 1314 543 < 400 232 613 1900 < 50 78, 168 < 400 < 50 92, 112 51, 088 88, 000 10, 295 37, 985 555, 900 3408 7, 202, 040 76, 142 5099 Elizabeth R. Jenny-Avital, and Sara T. Beatrice Clin Infect Dis. 2001; 32: 1227 -1230
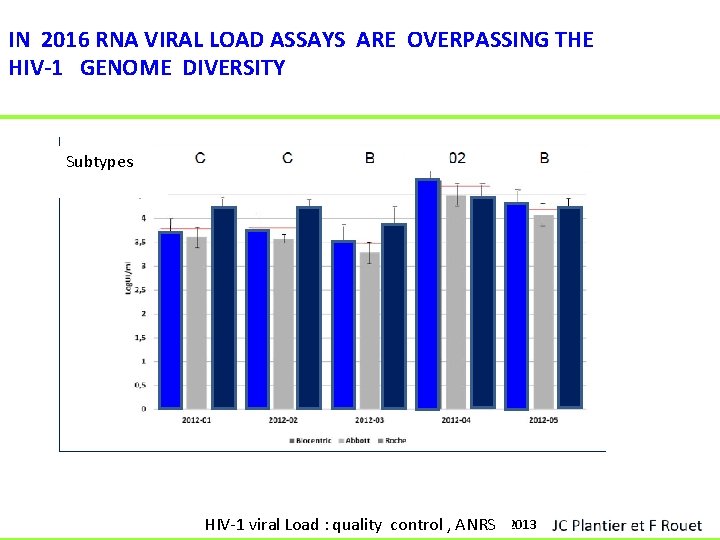
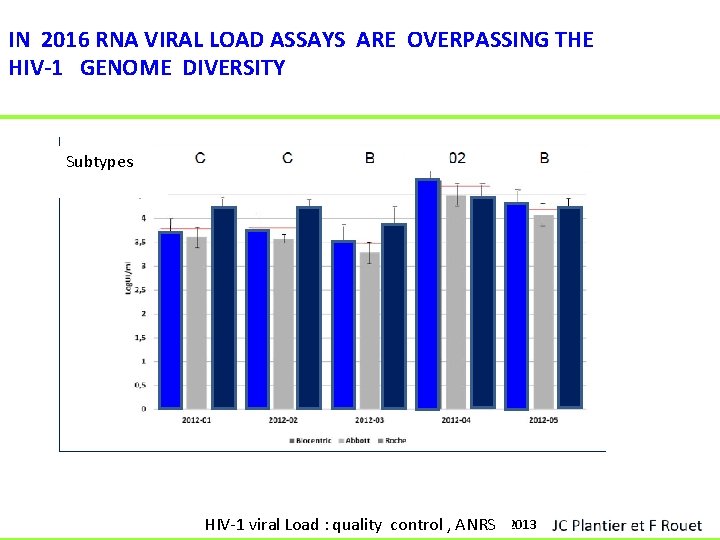
IN 2016 RNA VIRAL LOAD ASSAYS ARE OVERPASSING THE HIV-1 GENOME DIVERSITY Subtypes ANRS 2013 HIV-1 viral Load : quality control , ANRS
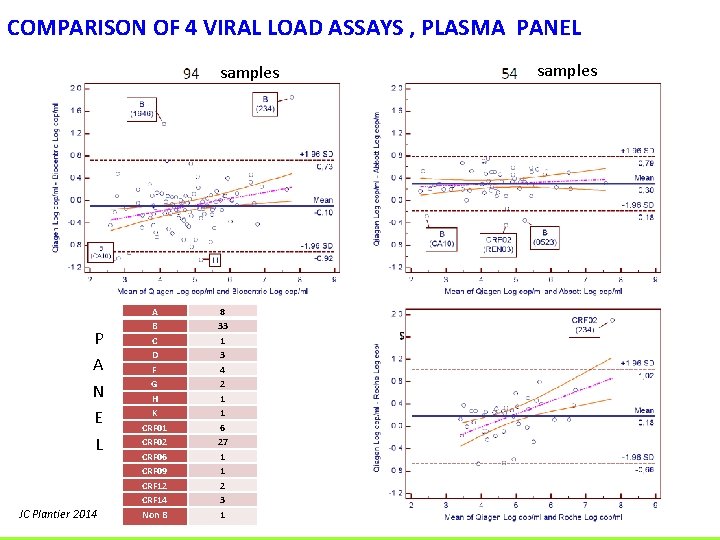
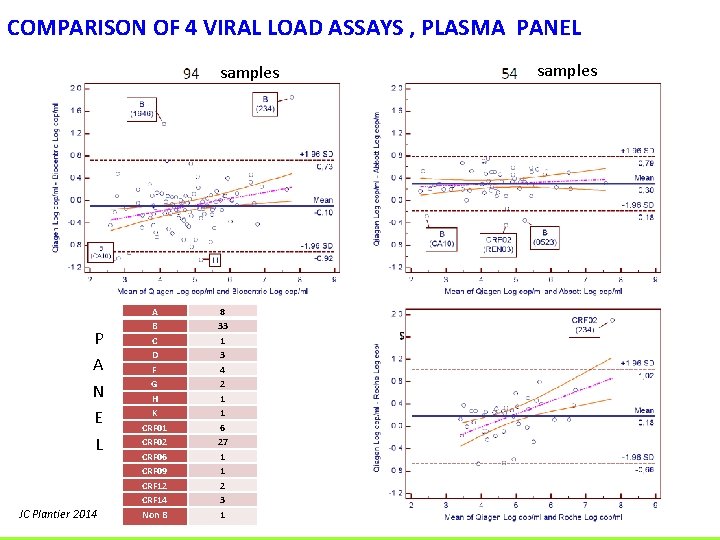
COMPARISON OF 4 VIRAL LOAD ASSAYS , PLASMA PANEL samples P A N E L JC Plantier 2014 A B C D F G H K CRF 01 CRF 02 CRF 06 CRF 09 CRF 12 CRF 14 Non B 8 33 1 3 4 2 1 1 6 27 1 1 2 3 1 samples
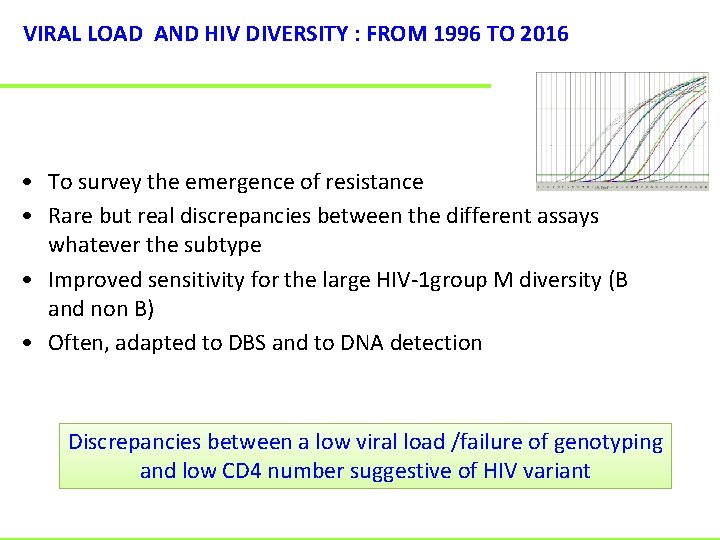
VIRAL LOAD AND HIV DIVERSITY : FROM 1996 TO 2016 • To survey the emergence of resistance • Rare but real discrepancies between the different assays whatever the subtype • Improved sensitivity for the large HIV-1 group M diversity (B and non B) • Often, adapted to DBS and to DNA detection Discrepancies between a low viral load /failure of genotyping and low CD 4 number suggestive of HIV variant
HIV- 1 GROUP M NON-B SUBTYPES ACQUIRED RESISTANCE TO ARV • Active sites for polymerase and integrase are highly – conserved • Subtype C propensity for K 65 R TDF-associated resistance mutation : limited consequences ( E White JID 2016) • Etravirine & Rilpivirine : 10 % non-B strains harbour a mutation present in the HIV-1 subtype B score for resistance • Natural polymorphism overlapping the acquired mutation againts PI • Anti-integrase resistance profiles similar whatever the subtypes
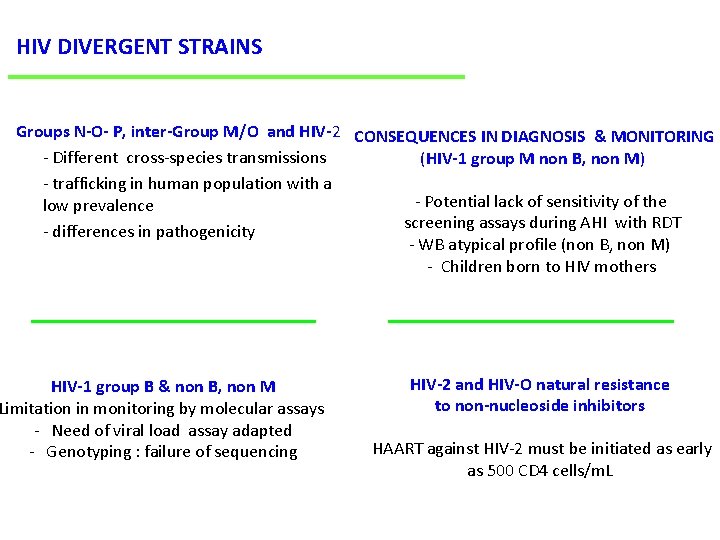
HIV DIVERGENT STRAINS Groups N-O- P, inter-Group M/O and HIV-2 CONSEQUENCES IN DIAGNOSIS & MONITORING - Different cross-species transmissions (HIV-1 group M non B, non M) - trafficking in human population with a - Potential lack of sensitivity of the low prevalence screening assays during AHI with RDT - differences in pathogenicity - WB atypical profile (non B, non M) - Children born to HIV mothers HIV-1 group B & non B, non M Limitation in monitoring by molecular assays - Need of viral load assay adapted - Genotyping : failure of sequencing HIV-2 and HIV-O natural resistance to non-nucleoside inhibitors HAART against HIV-2 must be initiated as early as 500 CD 4 cells/m. L
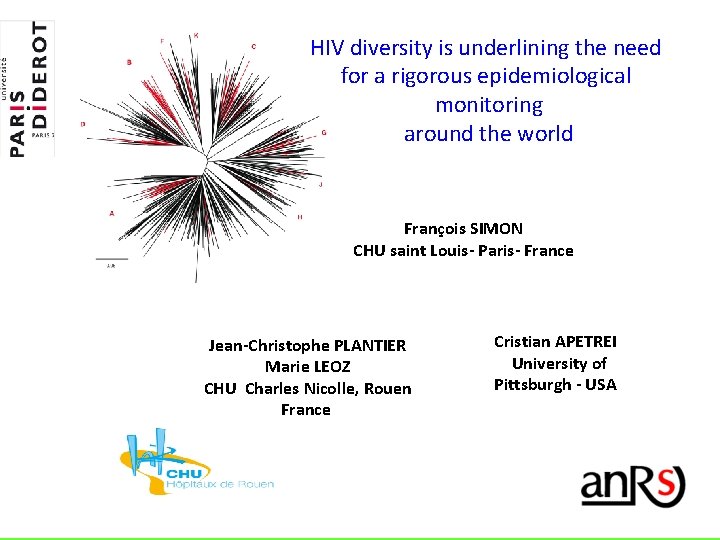
HIV diversity is underlining the need for a rigorous epidemiological monitoring around the world François SIMON CHU saint Louis- Paris- France Jean-Christophe PLANTIER Marie LEOZ CHU Charles Nicolle, Rouen France Cristian APETREI University of Pittsburgh - USA
 Genetic diversity vs species diversity
Genetic diversity vs species diversity Genetic diversity vs species diversity
Genetic diversity vs species diversity Sample rejection criteria
Sample rejection criteria Hiv diagnosis algorithm
Hiv diagnosis algorithm Genetic programming vs genetic algorithm
Genetic programming vs genetic algorithm What is gene flow and genetic drift
What is gene flow and genetic drift Gene pool
Gene pool What is the difference between genetic drift and gene flow
What is the difference between genetic drift and gene flow Genetic programming vs genetic algorithm
Genetic programming vs genetic algorithm Gene po
Gene po Sexual reproduction
Sexual reproduction Why is genetic diversity important
Why is genetic diversity important Genetic diversity
Genetic diversity Why is genetic diversity important
Why is genetic diversity important Red dot
Red dot Taper roller bearing advantages and disadvantages
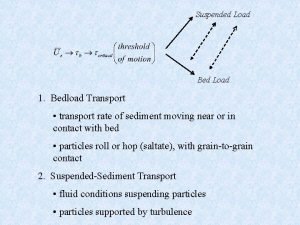
Taper roller bearing advantages and disadvantages Bed load and suspended load transport
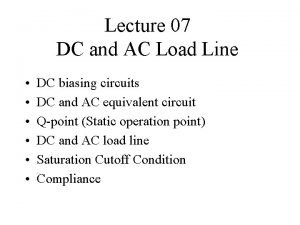
Bed load and suspended load transport The point of intersection of dc and ac load line is called
The point of intersection of dc and ac load line is called Collaborative nursing interventions
Collaborative nursing interventions Perbedaan diagnosis gizi dan diagnosis medis
Perbedaan diagnosis gizi dan diagnosis medis Medical diagnosis and nursing diagnosis difference
Medical diagnosis and nursing diagnosis difference Medical diagnosis and nursing diagnosis difference
Medical diagnosis and nursing diagnosis difference Objectives of nursing process
Objectives of nursing process Viral entry
Viral entry Trivalent vaccin herpes
Trivalent vaccin herpes Inmunidad
Inmunidad Section 24-1 viral structure and replication
Section 24-1 viral structure and replication