EVAR Not Just For Surgeons Anymore J Michael





- Slides: 27
EVAR: “Not Just For Surgeons Anymore” J Michael Bacharach MD, MPH, FACC Section Head, Vascular Medicine & Intervention North Central Heart Institute Professor of Clinical Medicine, Sanford School of Medicine, University of South Dakota Associate Professor of Surgery, Mayo Clinic Graduate School of Medicine
J. Michael Bacharach, MD, MPH I/we have no real or apparent conflicts of interest to report.

“Busting The Myths”
MYTHS • Aneurysmal disease can only be treated by surgeons • Endografts require surgical cut-down for access • Inability to perform open aneurysmectomy or emergently convert a patient to open repair prohibits an operator from performing endovascular repairs • EVAR is so complicated that non-surgeons cannot learn how to do it
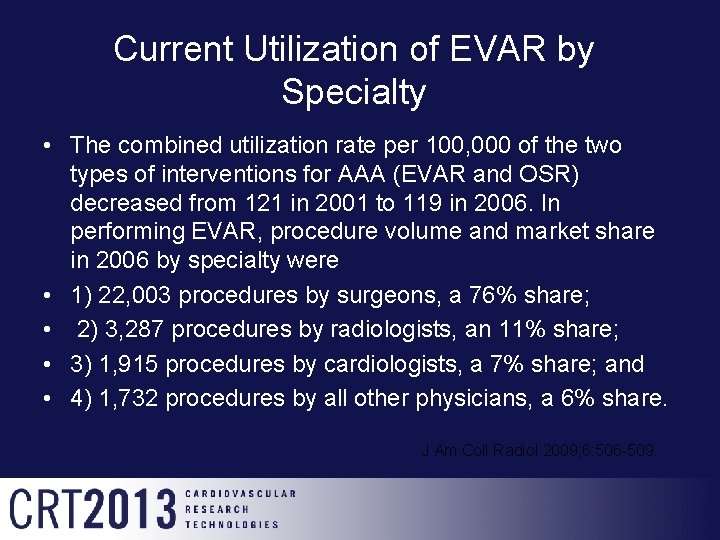
Current Utilization of EVAR by Specialty • The combined utilization rate per 100, 000 of the two types of interventions for AAA (EVAR and OSR) decreased from 121 in 2001 to 119 in 2006. In performing EVAR, procedure volume and market share in 2006 by specialty were • 1) 22, 003 procedures by surgeons, a 76% share; • 2) 3, 287 procedures by radiologists, an 11% share; • 3) 1, 915 procedures by cardiologists, a 7% share; and • 4) 1, 732 procedures by all other physicians, a 6% share. J Am Coll Radiol 2009; 6: 506 -509.
“What Hasn’t Changed “
Elements of Management of the Patient With AAA • Recognize and diagnose aneurysmal disease • Apply appropriate imaging to risk stratify and determine need for intervention • Risk factor management and management of co-morbidities • Intervention • On-going care and surveillance
Components of Treating Patients with Aneurysmal Disease • Recognition…. clearly a physician trained to care for patients can through history, examination and adjunctive imaging identify aneurysmal disease • Imaging…. requires familiarity with both advances and limitations of modern imaging, and the ability to convert the imaging into data that can be translated into determining the suitability of a patient for endovascular treatment
Components of Treating Patients with Aneurysmal Disease • Judgment and experience…. knowing when to say “NO” • Catheter-based skills…. needed for procedural success, familiarity with device characteristics and the ability to adapt the best device to achieve the best outcome • Surveillance…. commitment to continue to follow and care for the patient after the procedure
“What Has Changed? ”
Changes in Technology • This change in technology has required a new set of skills • Imaging and the recognition that certain aortic morphology is well suited for EVAR and recognizing those who are not • Catheter based skills • No longer is cutting and suturing required • Rather manipulation of small catheters and wires under fluoroscopic guidance and without the aid of direct tactile manipulation
Development Mature Technology Development Innovation 1) Percutaneous approach with pre-close 2) Development of smaller delivery systems that allow percutaneous placement. 3) Newer smaller profile graft systems
Advances • Historically devices were very large and required surgical access • Sheath and delivery systems were very large, difficult to deliver • Complications when they occurred often led to surgical conversion
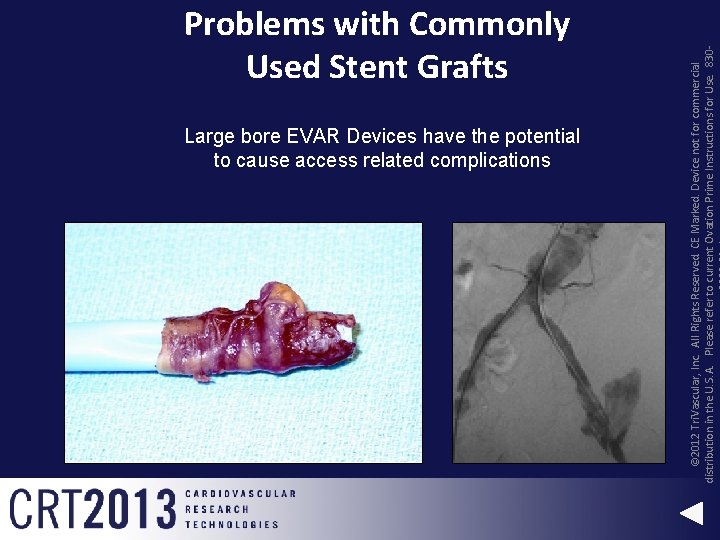
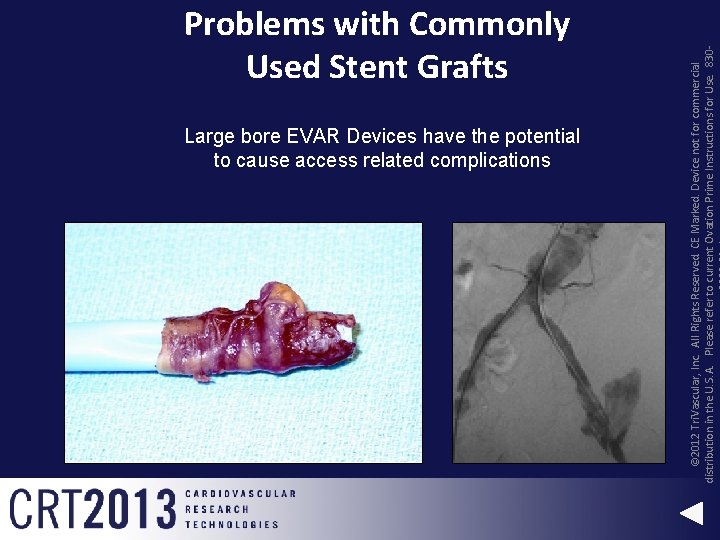
Large bore EVAR Devices have the potential to cause access related complications © 2012 Tri. Vascular, Inc. All Rights Reserved. CE Marked. Device not for commercial distribution in the U. S. A. Please refer to current Ovation Prime Instructions for Use. 830 - Problems with Commonly Used Stent Grafts


Access • Improved sheath systems for safer delivery • Smaller and coated delivery systems • Preclose technique for percutaneous access
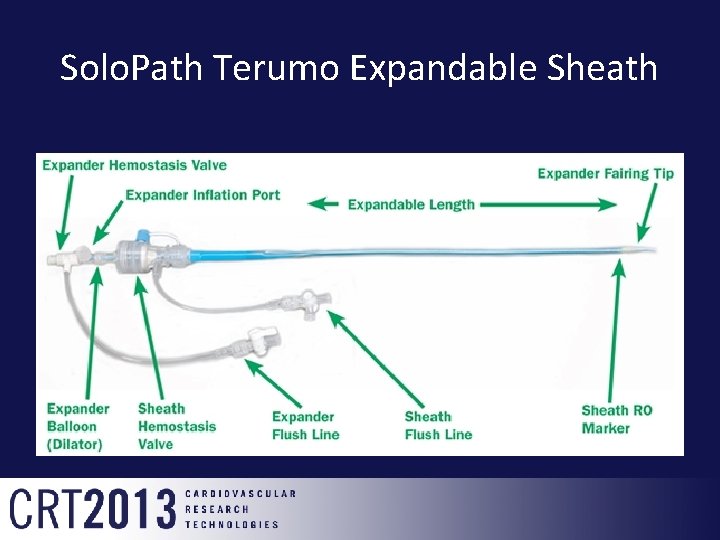
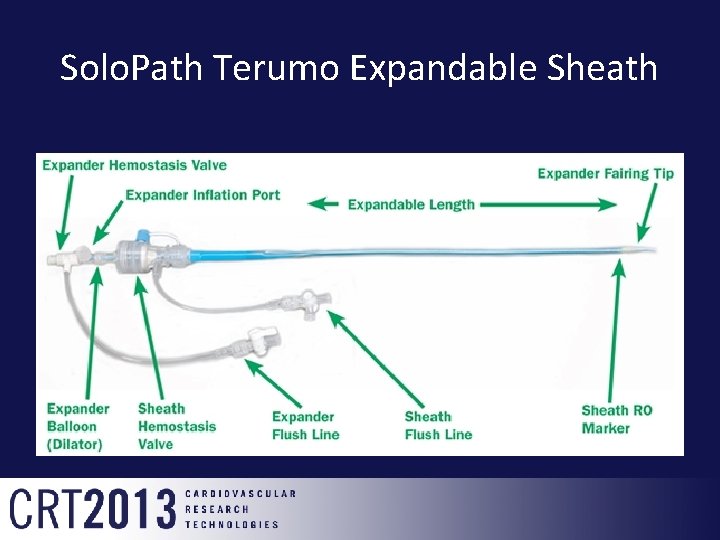
Solo. Path Terumo Expandable Sheath
Percutaneous Approach • Improvements in device delivery systems, smaller sheath sizes and shorter procedure times have contributed to success • The key has been the development of suture-mediated closure devices


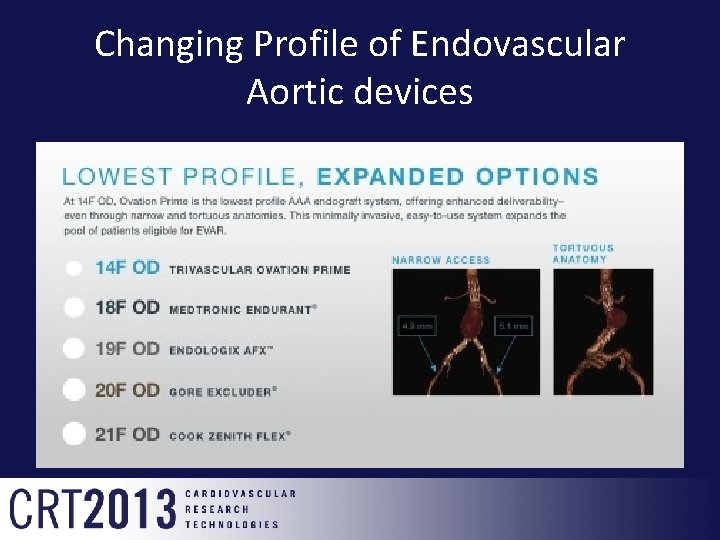
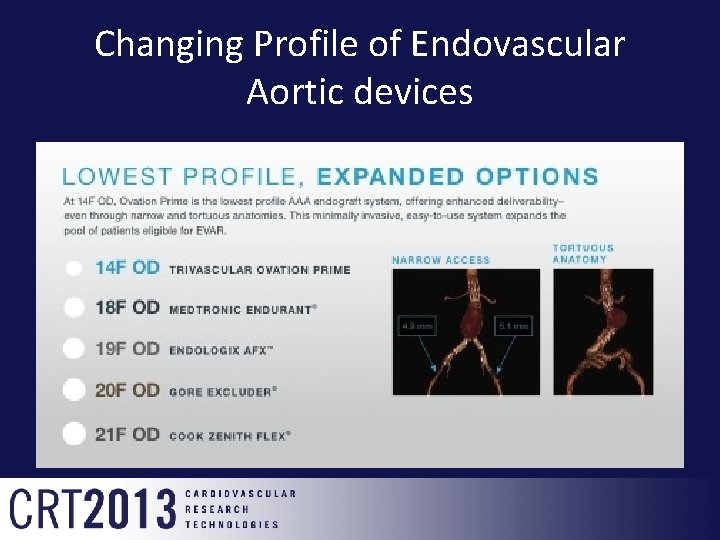
Changing Profile of Endovascular Aortic devices
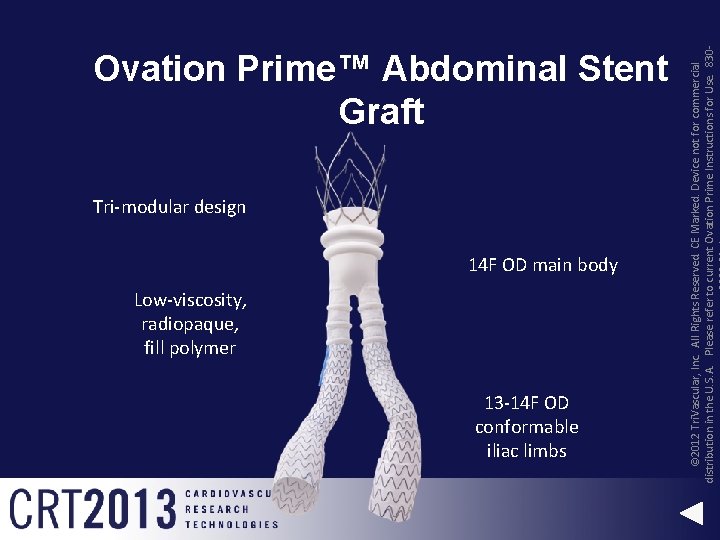
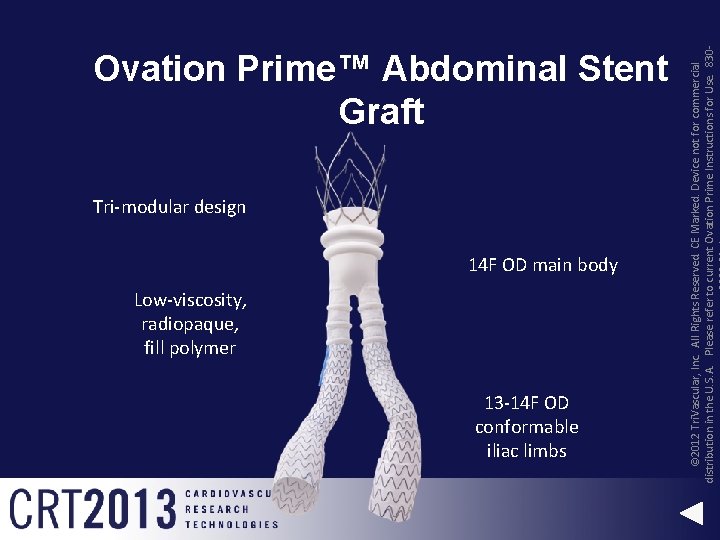
Tri-modular design 14 F OD main body Low-viscosity, radiopaque, fill polymer 13 -14 F OD conformable iliac limbs © 2012 Tri. Vascular, Inc. All Rights Reserved. CE Marked. Device not for commercial distribution in the U. S. A. Please refer to current Ovation Prime Instructions for Use. 830 - Ovation Prime™ Abdominal Stent Graft
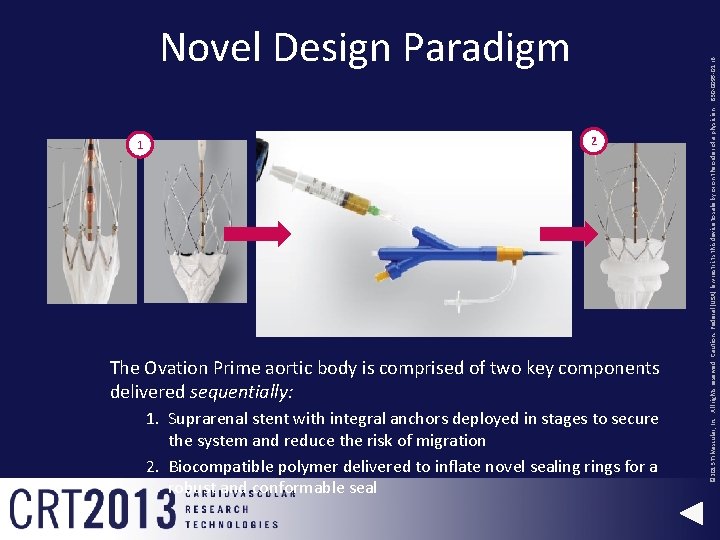
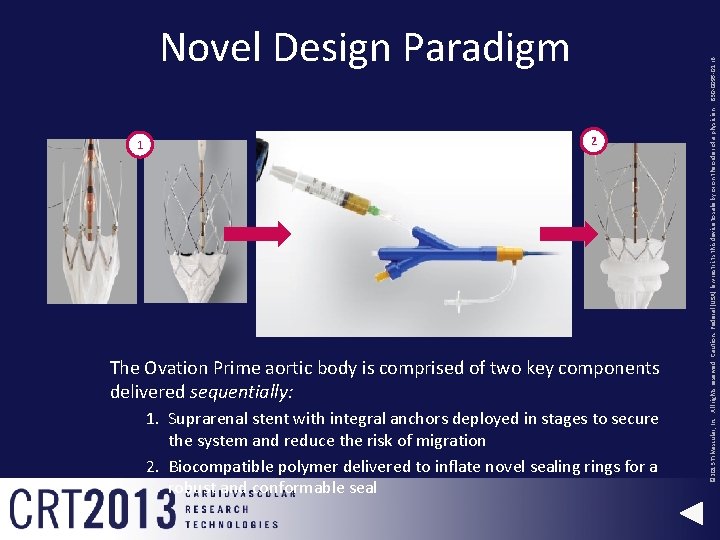
1 2 The Ovation Prime aortic body is comprised of two key components delivered sequentially: 1. Suprarenal stent with integral anchors deployed in stages to secure the system and reduce the risk of migration 2. Biocompatible polymer delivered to inflate novel sealing rings for a robust and conformable seal © 2013 Tri. Vascular, Inc. All rights reserved. Caution: Federal (USA) law restricts this device to sale by or on the order of a physician. 830 -0095 -01 r. B Novel Design Paradigm
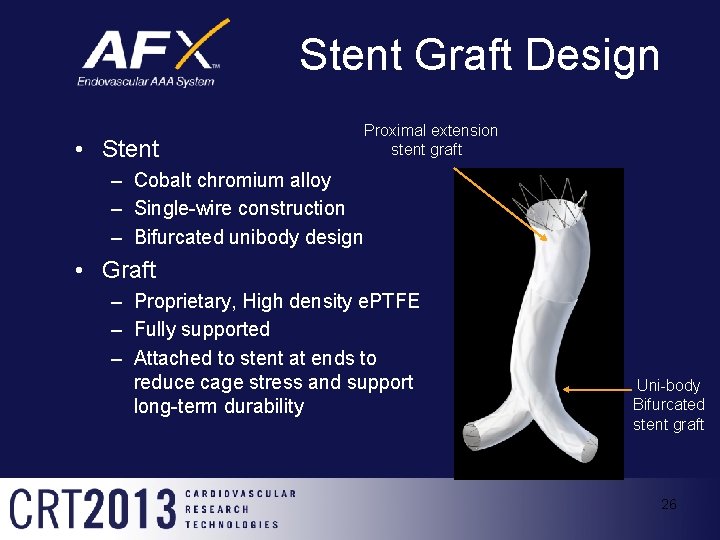
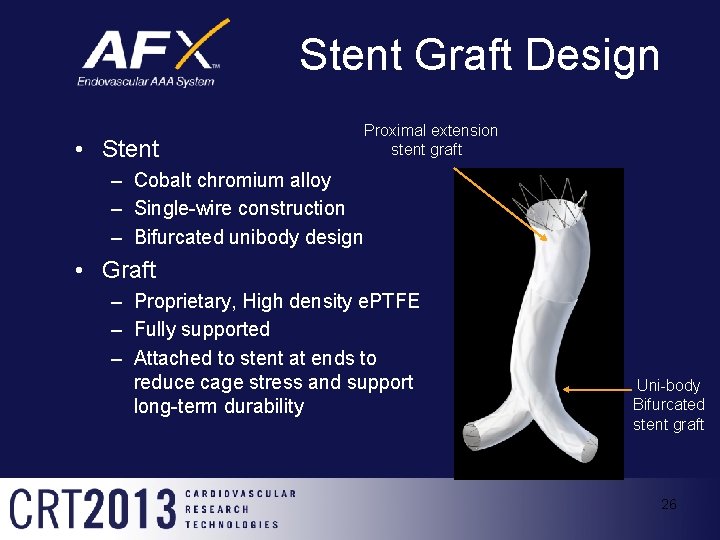
Stent Graft Design • Stent Proximal extension stent graft – Cobalt chromium alloy – Single-wire construction – Bifurcated unibody design • Graft – Proprietary, High density e. PTFE – Fully supported – Attached to stent at ends to reduce cage stress and support long-term durability Uni-body Bifurcated stent graft 26
PEVAR Trial • A 94% procedural technical success rate was achieved in a multicenter setting • The primary trial endpoint was met (P<. 0036), demonstrating non-inferiority of PEVAR to surgical EVAR • Favorable trending of PEVAR in several clinical utility outcomes including reduced anesthesia time, reduced blood loss and need for transfusion, shorter hospital length of stay, and less analgesics prescribed for groin pa
Summary • The clinical recognition and elements of management of aortic aneurysm have not changed • Technologic improvements in devices , delivery systems and newer access management techniques have allowed for safer and percutaneous treatment options