Enteric fever Typhoid and paratyphoid fever Is a


- Slides: 25
. Enteric. fever ( Typhoid and paratyphoid fever ) Is a clinical syndrome characterized by constitutional and gastrointestinal symptoms and by headache. Etiologic agents of enteric fever • —S. Typhi and S. Paratyphi and have no known hosts other than humans


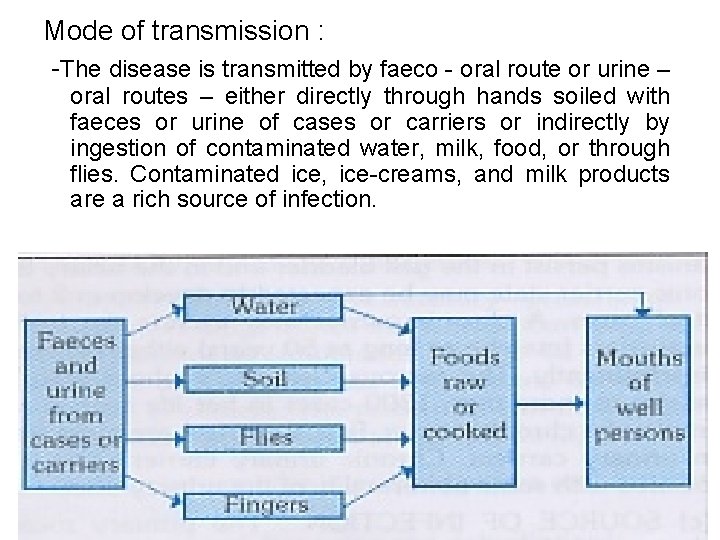
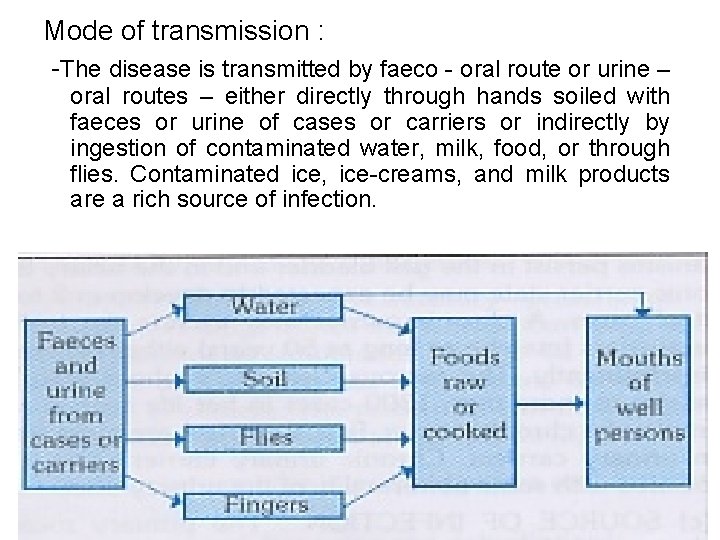
Mode of transmission : -The disease is transmitted by faeco - oral route or urine – oral routes – either directly through hands soiled with faeces or urine of cases or carriers or indirectly by ingestion of contaminated water, milk, food, or through flies. Contaminated ice, ice-creams, and milk products are a rich source of infection.
Age group : – Occurs at any age but it is considered to be a disease mainly of children and young adults. – In endemic areas, the highest attack rate occurs in children aged 8 -19 years.
Cont … Gender and race : – commonly seen in males than in females. Occupation : – Certain categories of persons handling the infective material and live cultures of S. typhi are at increased risk of acquiring infection. Socio-economic factors : – It is a disease of poverty as it is often associated with inadequate sanitation facilities and unsafe water supplies.
Cont. . Environmental factors : – peak incidence of typhoid fever is reported during July - September. This period coincides with the rainy season and a substantial increase in fly population. Social factors : – pollution of drinking water supplies, open air defecation, and urination, low standards of food and personal hygiene, and health ignorance.
Cont. . Nutritional status : – Malnutrition may enhance the susceptibility to typhoid fever by altering the intestinal flora or other host defences. Incubation period : – 10 -14 days Reservoir of infection : – Man is the only known reservoir of infection - cases or carriers. Period of communicability: – A case is infectious as long as the bacilli appear in stool or urine.
Cont. . – Carriers : - Temporary or Chronic. Temporary carriers : - usually excrete bacilli up to 6 -8 weeks. – By the end of one year, 3 -4 per cent of cases continue to excrete typhoid bacilli. Chronic carriers: -Persons who excrete the bacilli for more than a year after a clinical attack are called
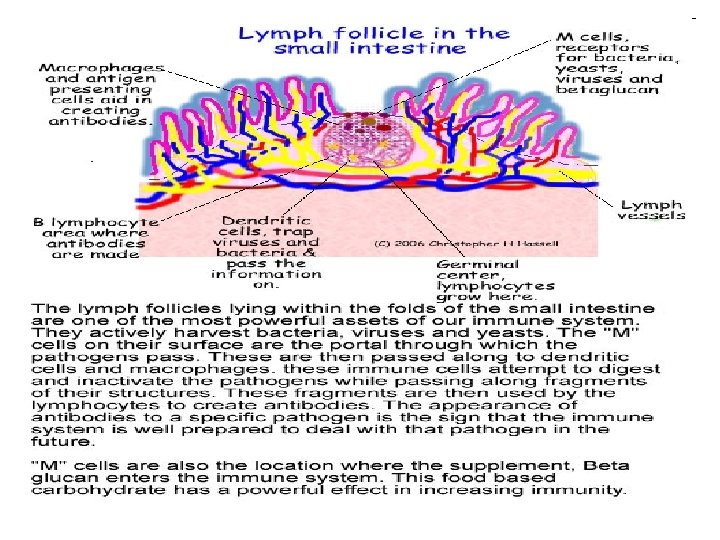
Pathogenesis – Ingestion ------penetration through the intestinal mucosa to the lymphoid tissue of the ileum -------proliferation of the bacteria----macrophages engulf the bacteria -------circulation ( via thoracic duct )-------primary bacteremia ------invasion of blood stream ( onset of fever )-----carried to liver , spleen , marrow where further multiplication occurs ------- secondary bacteremia ( release of large no. of bacteria from reticuloendothelial system----clinical diseases
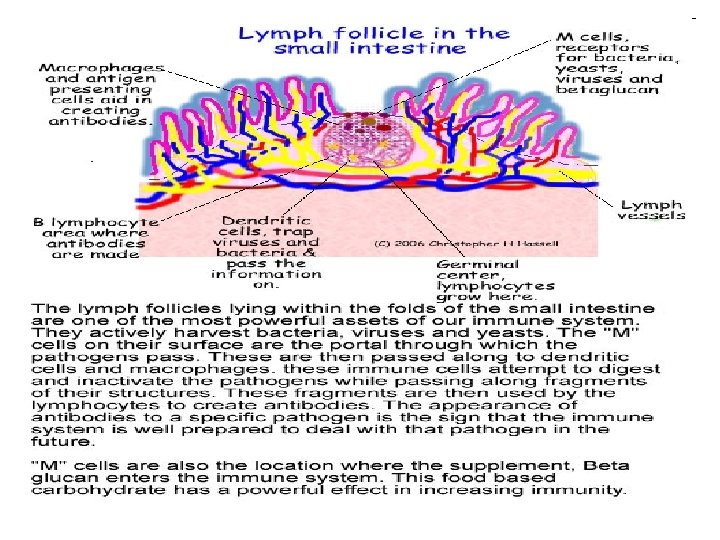
Cont … • Peyer`s patch : – are the most important organ to get infiltrated with chronic inflammatory cells – Sites for antibody production – Differentiate the ileum from the duodenum and jejunum At the end of 2 nd weeks : – Intestinal and mesenteric lymphnodes : swollen – Liver and spleen : congested and enlarged
Clinical features • Typhoid fever is characterized : – high fever 40 °C (104 °F), profuse sweating, gastroenteritis, and non-bloody diarrhea. – Less commonly a rash of flat, rose-colored spots • Classically, the course of untreated typhoid fever is divided into four individual stages, each lasting approximately one week.
In the first week : There is a slowly rising temperature with relative bradycardia, malaise, headache and cough. – Epistaxis and abdominal pain. – Leukopenia, – Eosinopenia and relative lymphocytosis, – Blood cultures are positive for Salmonella Typhi or Paratyphi.
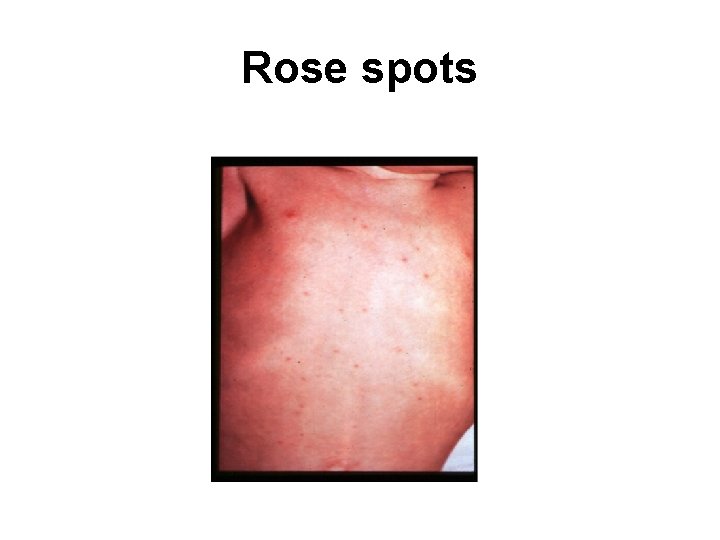
Cont. . In the second week : – High fever 40 °C (104 °F) and bradycardia – Dicrotic pulse wave. – Delirium is frequent. This delirium gives to typhoid the nickname of "nervous fever". – Rose spots appear on the lower chest and abdomen in around 1/3 patients. – Abdomen is distended and painful in the right lower quadrant
Cont… – Constipation – Spleen and liver are enlarged (hepatosplenomegaly) and tender – Widal reaction is strongly positive with anti. O and anti. H antibodies.
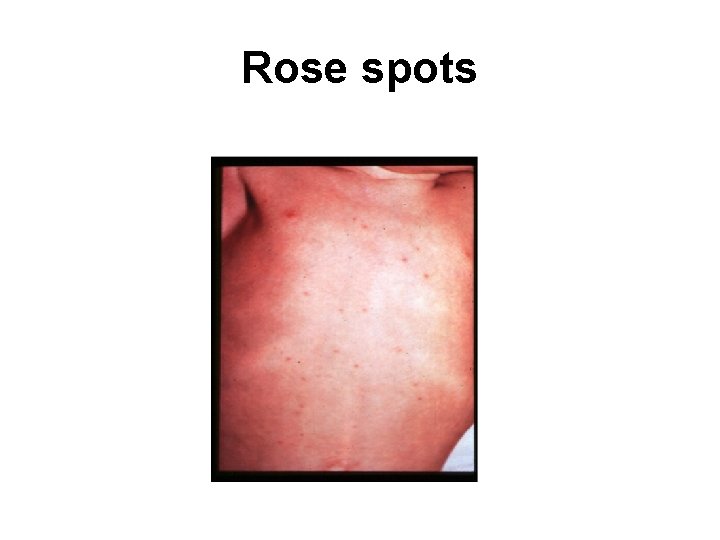
Rose spots
Cont. . • In the third week of typhoid fever a number of complications can occur: – Intestinal hemorrhage due to bleeding in congested Peyer's patches; this can be very serious but is usually non-fatal. – Intestinal perforation in distal ileum; this is a very serious complication and is frequently fatal. – Stool culture ---- positive
Cont. . In the fourth week : – Fever is still very high and oscillates very little over 24 hours. – Dehydration – Delirious (typhoid state) – Urine culture ------ positive
Diagnosis • 15– 25% of cases, leukopenia and neutropenia are detectable. (Leukocytosis is more common among children, during the first 10 days ) • Isolation of S. Typhi or S. Paratyphi from blood, bone marrow, other sterile sites, rose spots, stool, or urine. • Bone marrow culture remains highly (90%) sensitive despite 5 days of antibiotic therapy • Widal test for “Antigen – antibody ’’ • Remember “B A S U”
Treatment General: Supportive care includes : – Maintenance of adequate hydration. – Antipyretics. – Appropriate nutrition. Specific: Antimicrobial therapy is the mainstay treatment. Chloramphenicol , Ampicillin , Amoxicillin , ciprofloxacin, Trimethoprim &Sulphamethoxazole , In case of resistance – 3 rd generation cephalosporins ceftriaxone (50 -100 mg/kg/day in single or two divided doses IV for 5 -7 days) Cefixime (1 o-2 o mg/kg/day in 2 divided doses PO for 7 -10 days) • Treatment should be continued for 14 days
Cont… Treatment of complications : – Intestinal hemorrhage (blood transfusion) – Perforation (laparoscopy) Treatment of carriers : Ceftriaxone IV or ciprofloxacin IV in divided dose for 4 – 6 weeks.
Control Prevention and control Control of reservoir – – – Early diagnosis and notification Isolation- till three culture negative stool/urine Treatment Disinfection of urine/stool Surgery- chronic carrier Health education Control of sanitation – Water supply, basic sanitation, food hygiene, etc. Immunisation – Killed vaccine (anit-typhoid vaccine) – Live oral vaccine.
Specific protection THREE TYPES OF VACCINES 1. Whole cell salmonella typhi vaccine 2. Vi polysaccharide vaccine 3. Oral live attenuated Ty 21 a typhoid vaccine
Complications • • Orodental : Poor orodental hygiene, Parotitis Chest : Bronchitis, Pneumonia, Pulmonary infarct Heart : Myocarditis Liver , Gall bladder : Fatty liver , Hepatitis, Liver Abscess, Cholecystitis, Cholangitis, Pancreatitis. Gastrointestinal : Diarrhoea, Perforation of intestines, Peritonitis & hemorrhage from gut. Neurological : Encephalitis, Encephalopathy, Transverse myelitis, Meningitis, Peripheral neuritis, Aphasia, Cerebral vein thrombosis. Musculoskeletal : Chronic osteomyelitis, Suppurative arthritis, Polymyositis. Miscellaneous : Alopecia , Uveitis
 Paratyphoid symptoms
Paratyphoid symptoms Ploskirev medium
Ploskirev medium What are the stages of typhoid fever
What are the stages of typhoid fever Typhoid symptoms
Typhoid symptoms Defination of typhoid fever
Defination of typhoid fever Nursing care plan for typhoid fever slideshare
Nursing care plan for typhoid fever slideshare Introduction of typhoid fever
Introduction of typhoid fever Neil mooser reaction
Neil mooser reaction Typhoid fever treatment
Typhoid fever treatment Cholera
Cholera Enteric plexus
Enteric plexus Tablet definition
Tablet definition Advantages of enteric coated tablets
Advantages of enteric coated tablets Standard coating pan diagram
Standard coating pan diagram Definition of enteric
Definition of enteric Hektoen enteric agar
Hektoen enteric agar Enteric gram negative rods
Enteric gram negative rods Enteric gram negative bacilli
Enteric gram negative bacilli Typhoid ulcer and tuberculous ulcer
Typhoid ulcer and tuberculous ulcer Typhoid medicine course
Typhoid medicine course Swimmer itch
Swimmer itch Salwa touma
Salwa touma Typhosin
Typhosin Rasmussen syndrome
Rasmussen syndrome Welding causes cancer
Welding causes cancer Fever 1793 vocabulary
Fever 1793 vocabulary