Dudley Vanguard MCP Development Steph Cartwright Director of





- Slides: 26
Dudley Vanguard MCP Development Steph Cartwright - Director of Organisational Development & HR Dr Steve Mann – Clinical Executive for MCP Development Neill Bucktin – Director of Commissioning
The journey so far. . .

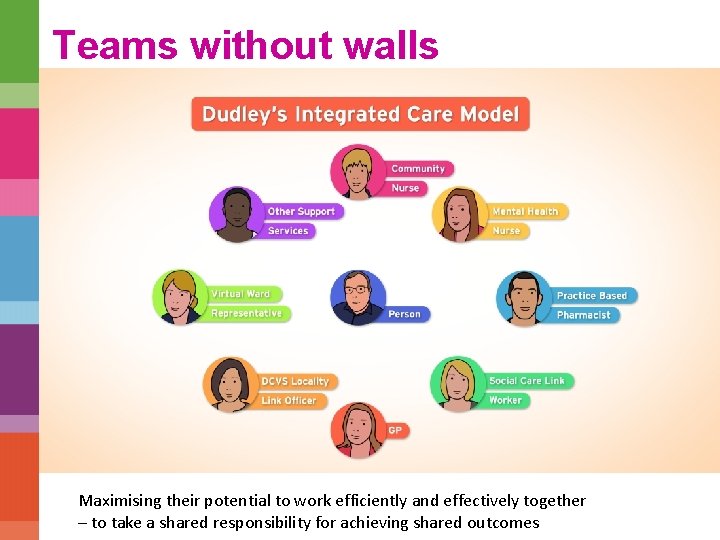
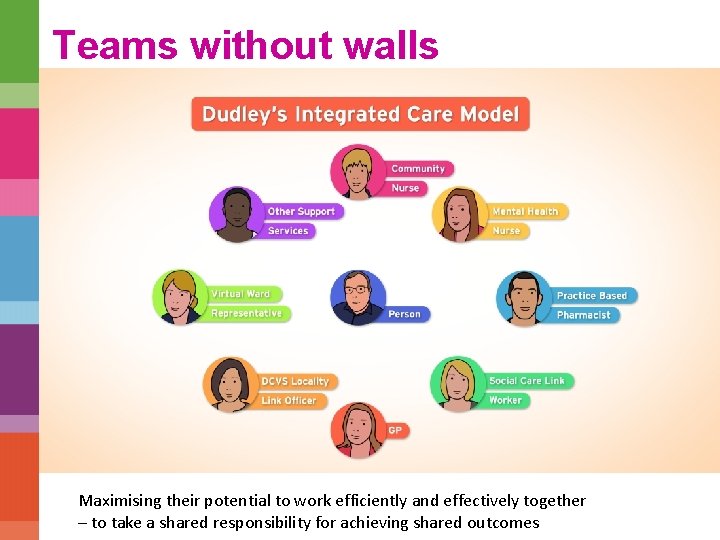
Teams without walls Maximising their potential to work efficiently and effectively together – to take a shared responsibility for achieving shared outcomes

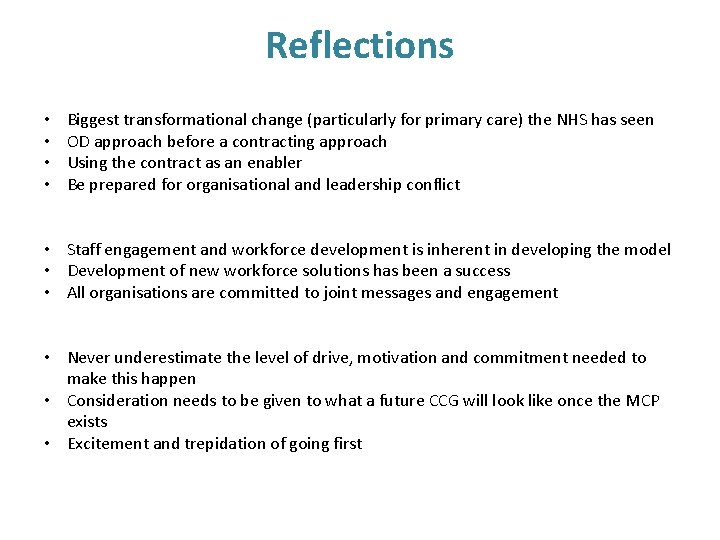
Reflections • • Biggest transformational change (particularly for primary care) the NHS has seen OD approach before a contracting approach Using the contract as an enabler Be prepared for organisational and leadership conflict • Staff engagement and workforce development is inherent in developing the model • Development of new workforce solutions has been a success • All organisations are committed to joint messages and engagement • Never underestimate the level of drive, motivation and commitment needed to make this happen • Consideration needs to be given to what a future CCG will look like once the MCP exists • Excitement and trepidation of going first
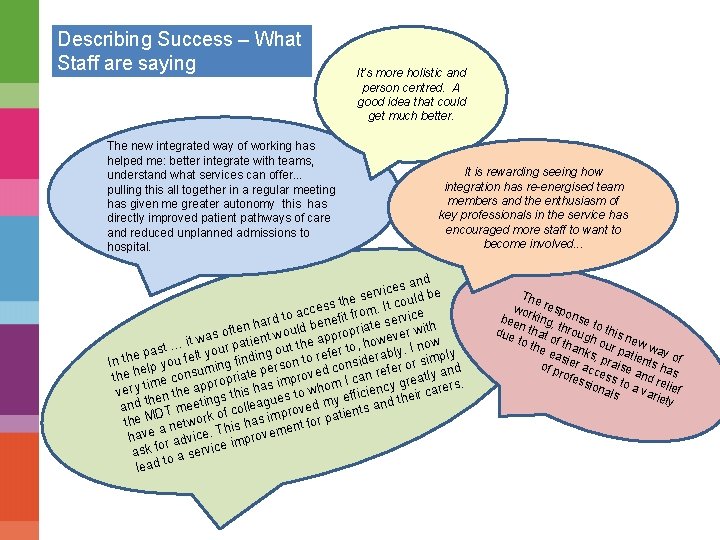
Describing Success – What Staff are saying The new integrated way of working has helped me: better integrate with teams, understand what services can offer. . . pulling this all together in a regular meeting has given me greater autonomy this has directly improved patient pathways of care and reduced unplanned admissions to hospital. It’s more holistic and person centred. A good idea that could get much better. It is rewarding seeing how integration has re-energised team members and the enthusiasm of key professionals in the service has encouraged more staff to want to become involved. . . nd ces a be i v r e ld es ss th m. It cou e c c a e ro rd to benefit f te servic h a h n ofte nt would ppropria ever wit s a w e t t … i your pati g out the fer to, ho bly. I now y s a p l t e n In the lp you fel ing findi rson to r considera r or simp d m fe e n pe the h me consu ropriate roved I can re greatly a. p m i m p s s ti y very en the ap s this ha es to who efficienc heir carer g t h y u and t T meetin f colleag proved m ients and D o t the M network his has im ent for pa a T have r advice. improvem e o ask f a servic to lead The wor respo bee king, nse to n due that throug this n o h e to t f he thank our pa w wa yo eas s, p tie f of p ier acc raise nts ha s a rofe e ssio ss to nd reli a nal var ef s iety
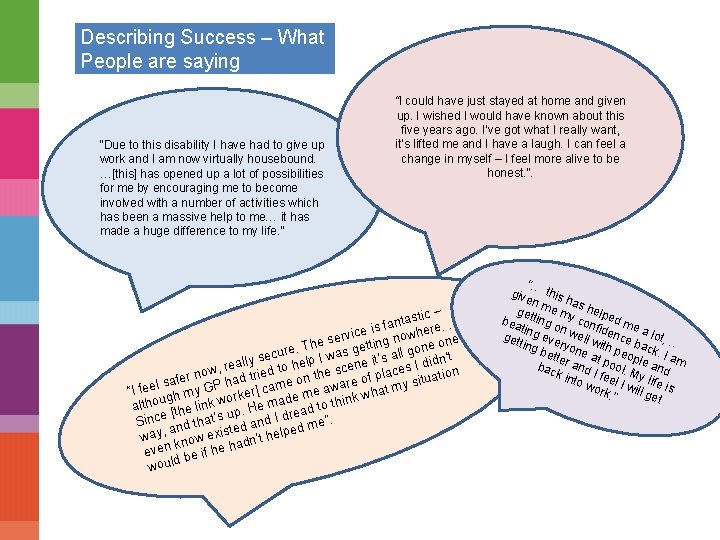
Describing Success – What People are saying “Due to this disability I have had to give up work and I am now virtually housebound. …[this] has opened up a lot of possibilities for me by encouraging me to become involved with a number of activities which has been a massive help to me… it has made a huge difference to my life. ” “I could have just stayed at home and given up. I wished I would have known about this five years ago. I’ve got what I really want, it’s lifted me and I have a laugh. I can feel a change in myself – I feel more alive to be honest. ”. – tastic. . n a f is re rvice g nowhe ne e s e n. Th as getti one o e r g u l l c a se Iw ’s n’t eally d to help scene it ces I did n r , w e o la ie no ituati ad tr me on th are of p afer s h s l y P e w a m “I fe gh my G orker] c me a ink what e d u w a o h k h lin alt He m read to t e. h t p [ u Since nd that’s d and I d d me”. a te e way, now exis dn’t help k a even be if he h d woul “… give this has n get me my helpe d bea ting o con fide me a ting nw lo n e e get ting veryo ll with ce bac t, … n k p bet ter e at p eople. I am o a a bac o n k in d I fee l. My nd l to w if l ork I will g e is. ” et

The GP Perspective
Primary Care in Dudley • Long history of strong GP engagement in Dudley • Practice based commissioning clusters transformed into CCG localities • Historic Dudley Commissioning Forum (now CCG Clinical Forum) established for over ten years • GP Engagement Lead who works with every GP practice in Dudley to aid their practice and commissioning development • Monthly locality meetings chaired by elected CCG Board GPs • 6 weekly CCG wide GP membership meetings attended by 100% of practices • Primary Care and Membership Development team in place since the establishment of the CCG
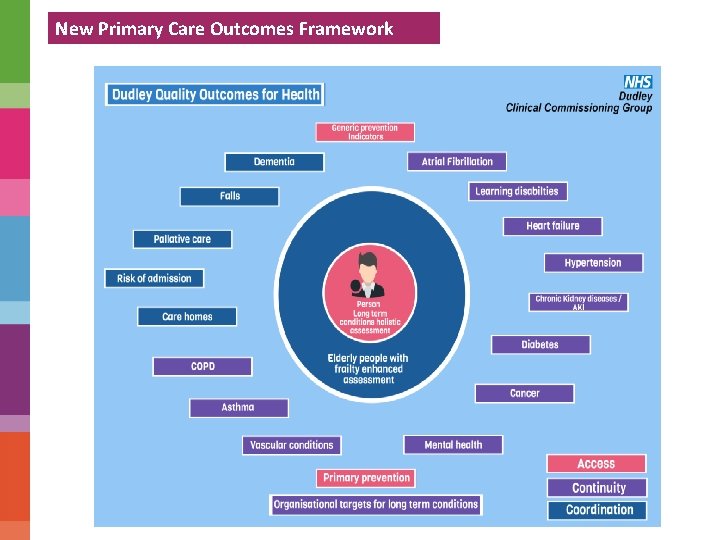
Development of Primary Care GP Collaborative: • 36 Practices have joined the GP collaborative • £ 1 million funding through the Value Proposition to support primary care • Primary Care Development Group with GP and PM leadership established to deliver projects such as combining back office functions, paramedic home visiting service, education for HCAs, records storage, digital dictation etc. Dudley Outcomes for Health Framework: • • Replacement of Qo. F framework for 40 out of 46 practices Outcomes based Focussed on providing optimum care for long term conditions patients Development of EMIS templates
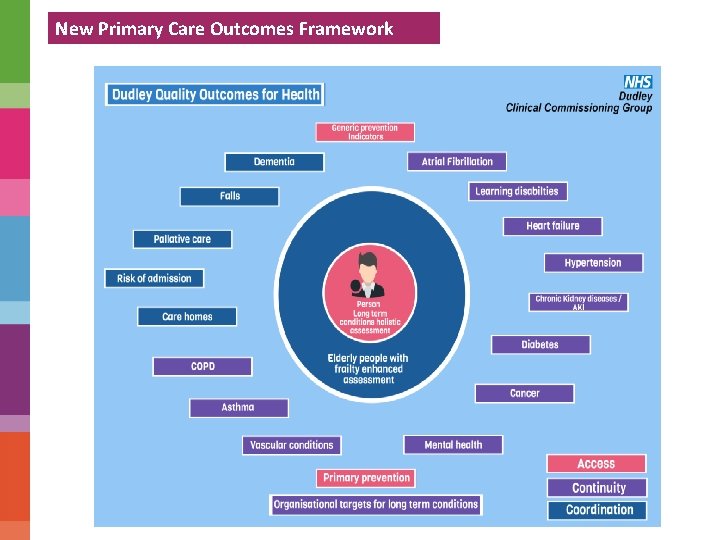
New Primary Care Outcomes Framework
Development of Primary Care MCP Development: • Dedicated team to develop the primary care element of the new model of care • Substantial negotiations need to take place to prepare for procurement process: • Between steering group and GP membership / collaborative • Between steering group and potential partners • Primary Care Team are: • Engaging the collaborative practices on what they want from the MCP (hosted contract or joint venture) • Developing the integration agreement between each GP practice and the MCP • Preparing the case to respond to both providers and the procurement process

Next Steps
What might the future look like? • Commissioning organisation • Provider 1 – hospital services – planned and urgent care. • Provider 2 – all community health services – physical health; mental health; children’s health; learning disability services; primary medical services and social care.
Provider 2 = MCP • Multi-Specialty – physical health, mental health, children, adults, social care, primary care…… • Community – services delivered out of hospital • Provider
How do we commission? • Funded for a population – 315, 000 people registered with Dudley GPs • We buy single events for patients – “procedures”, “admissions”, “attendances”, “contacts” • We have a statutory duty to reduce health inequalities but…. • We only commission “outcomes” from primary care
How would it work? • Commission for better outcomes for the whole population – not single events • Start with a defined population – general practice • Build the “multi-specialties” at practice level – the MDT • Connect to the rest of the system outwards • Aggregate as the MCP
How it works cont’d • No longer buy “events” • Buy outcomes • Single capitated budget for a whole population • MDT has shared responsibility and is held to account for its defined (practice) population • MCP has responsibility for the whole population and is held to account by its commissioner
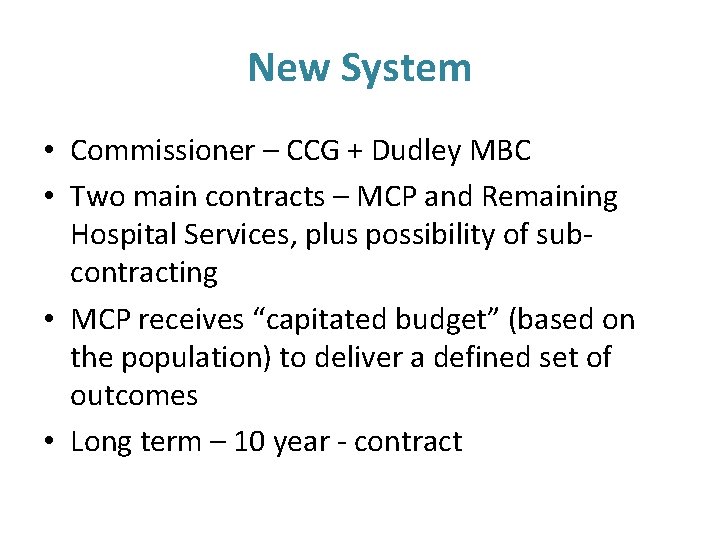
New System • Commissioner – CCG + Dudley MBC • Two main contracts – MCP and Remaining Hospital Services, plus possibility of subcontracting • MCP receives “capitated budget” (based on the population) to deliver a defined set of outcomes • Long term – 10 year - contract
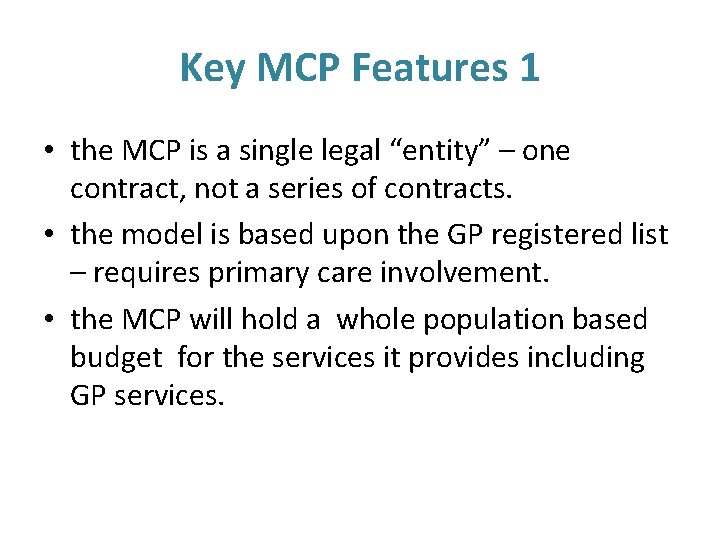
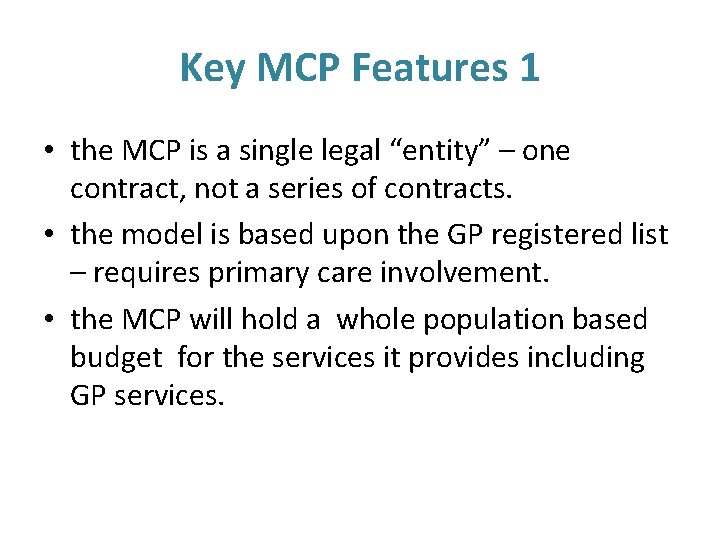
Key MCP Features 1 • the MCP is a single legal “entity” – one contract, not a series of contracts. • the model is based upon the GP registered list – requires primary care involvement. • the MCP will hold a whole population based budget for the services it provides including GP services.
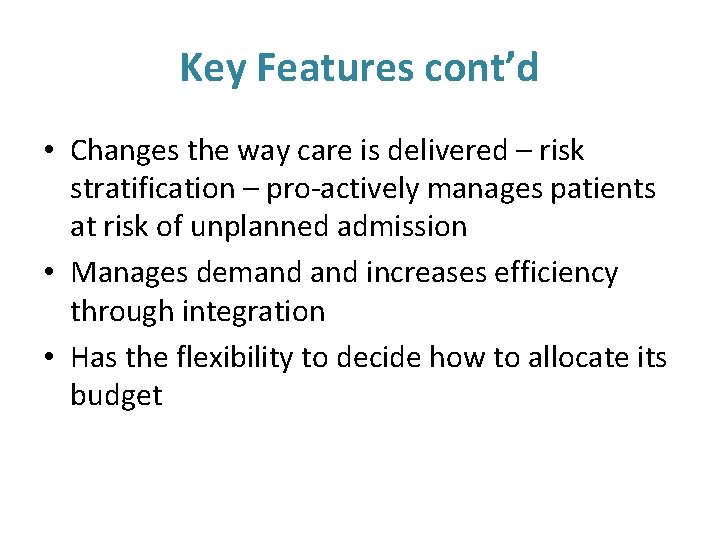
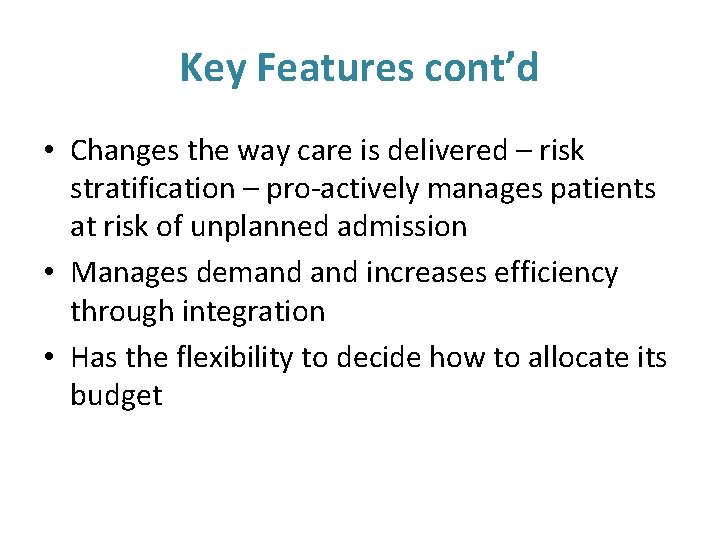
Key Features cont’d • Changes the way care is delivered – risk stratification – pro-actively manages patients at risk of unplanned admission • Manages demand increases efficiency through integration • Has the flexibility to decide how to allocate its budget
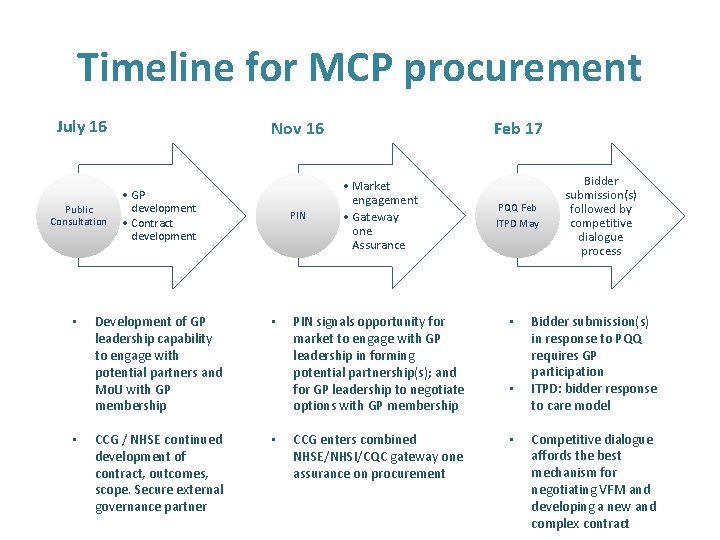
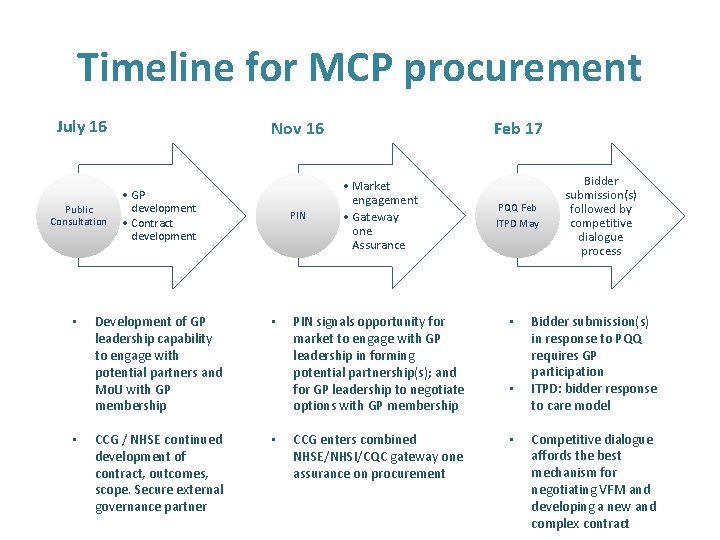
Timeline for MCP procurement July 16 Public Consultation • • Nov 16 • GP development • Contract development PIN Development of GP leadership capability to engage with potential partners and Mo. U with GP membership • CCG / NHSE continued development of contract, outcomes, scope. Secure external governance partner • Feb 17 • Market engagement • Gateway one Assurance PQQ Feb ITPD May PIN signals opportunity for market to engage with GP leadership in forming potential partnership(s); and for GP leadership to negotiate options with GP membership • CCG enters combined NHSE/NHSI/CQC gateway one assurance on procurement • • Bidder submission(s) followed by competitive dialogue process Bidder submission(s) in response to PQQ requires GP participation ITPD: bidder response to care model Competitive dialogue affords the best mechanism for negotiating VFM and developing a new and complex contract
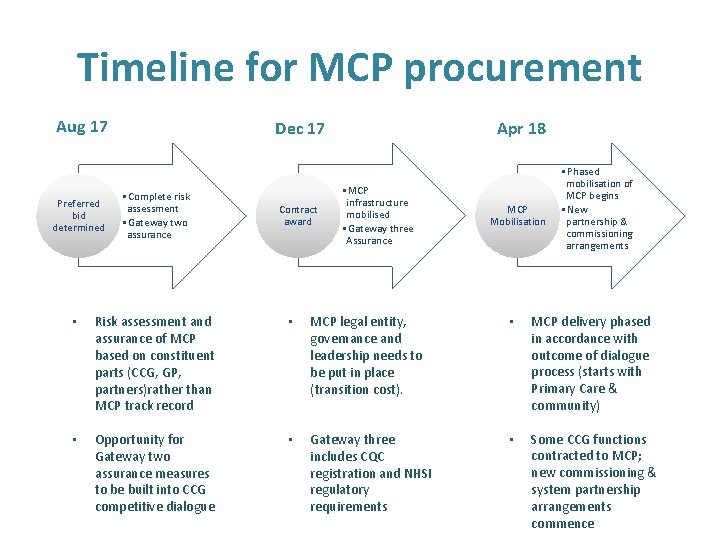
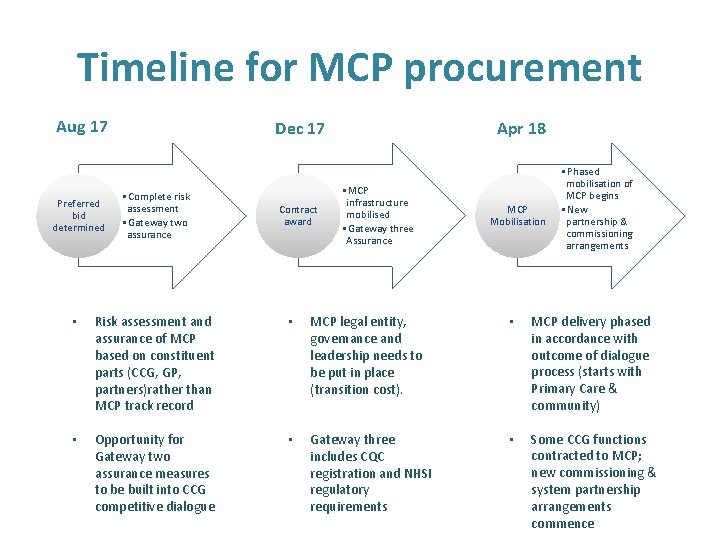
Timeline for MCP procurement Aug 17 Preferred bid determined Dec 17 • Complete risk assessment • Gateway two assurance Contract award Apr 18 • MCP infrastructure mobilised • Gateway three Assurance MCP Mobilisation • Phased mobilisation of MCP begins • New partnership & commissioning arrangements • Risk assessment and assurance of MCP based on constituent parts (CCG, GP, partners)rather than MCP track record • MCP legal entity, governance and leadership needs to be put in place (transition cost). • MCP delivery phased in accordance with outcome of dialogue process (starts with Primary Care & community) • Opportunity for Gateway two assurance measures to be built into CCG competitive dialogue • Gateway three includes CQC registration and NHSI regulatory requirements • Some CCG functions contracted to MCP; new commissioning & system partnership arrangements commence
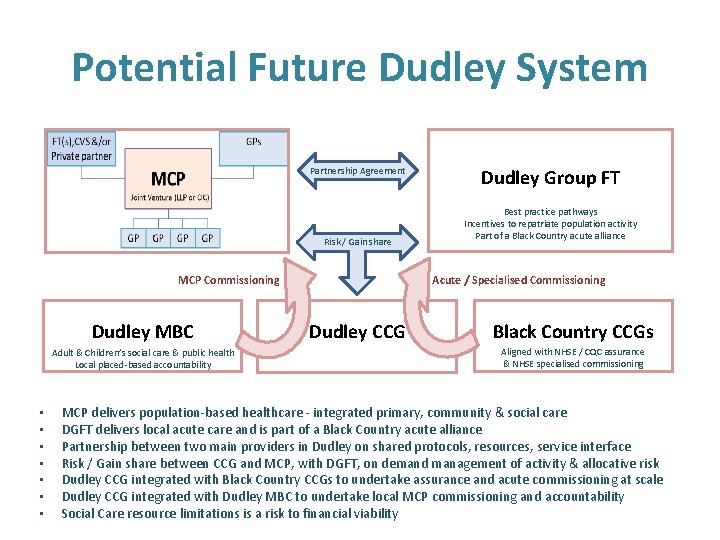
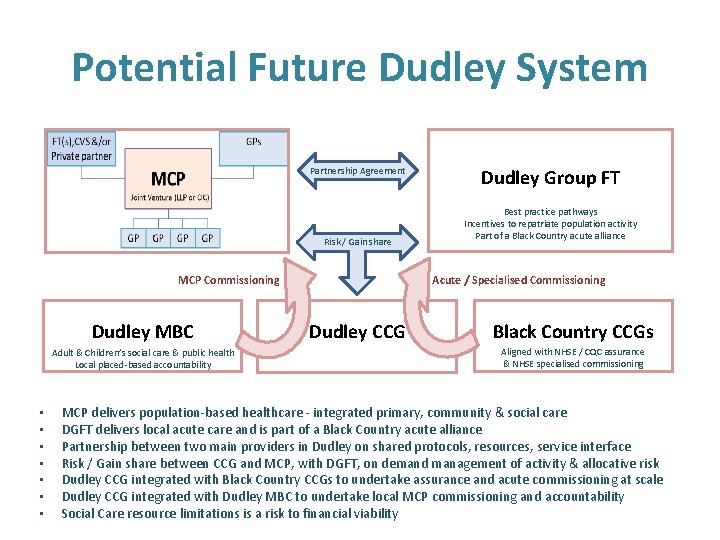
Potential Future Dudley System Partnership Agreement Risk / Gain share MCP Commissioning Dudley MBC Adult & Children’s social care & public health Local placed-based accountability • • Dudley Group FT Best practice pathways Incentives to repatriate population activity Part of a Black Country acute alliance Acute / Specialised Commissioning Dudley CCG Black Country CCGs Aligned with NHSE / CQC assurance & NHSE specialised commissioning MCP delivers population-based healthcare - integrated primary, community & social care DGFT delivers local acute care and is part of a Black Country acute alliance Partnership between two main providers in Dudley on shared protocols, resources, service interface Risk / Gain share between CCG and MCP, with DGFT, on demand management of activity & allocative risk Dudley CCG integrated with Black Country CCGs to undertake assurance and acute commissioning at scale Dudley CCG integrated with Dudley MBC to undertake local MCP commissioning and accountability Social Care resource limitations is a risk to financial viability

Questions and Discussion