DoctorPatient relations Michael Wilson University of Illinois College







- Slides: 32
Doctor-Patient relations Michael Wilson University of Illinois College of Medicine University of Illinois Department of Psychology
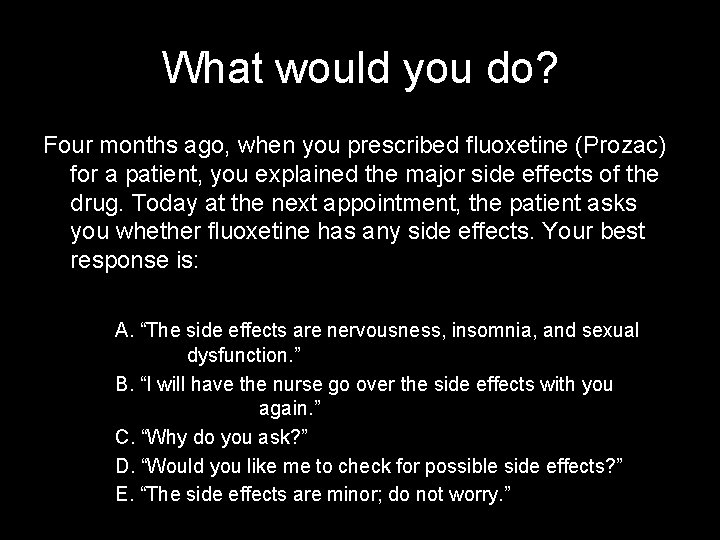
What would you do? Four months ago, when you prescribed fluoxetine (Prozac) for a patient, you explained the major side effects of the drug. Today at the next appointment, the patient asks you whether fluoxetine has any side effects. Your best response is: A. “The side effects are nervousness, insomnia, and sexual dysfunction. ” B. “I will have the nurse go over the side effects with you again. ” C. “Why do you ask? ” D. “Would you like me to check for possible side effects? ” E. “The side effects are minor; do not worry. ”
Learning objectives • • • What is effective communication? The biopsychosocial model Styles of relating Professional boundaries Issues of compliance Rules for handling difficult doctor-patient relationships
What this lecture is not… • …NOT about learning to take a patient history – You will learn this in M 2 • …NOT about psychiatric disorders – We will have a few lectures later – Also longer course on this in M 2 • …NOT going to be able to teach you everything about “people skills” – Understanding psychological & social aspects of your patients is life-long process

What is effective communication? • Essential part of doctor-patient relationship – an exchange between medical expert & consumer – on deeper level, interaction between 2 human beings about matters of health, illness, death – to be effective, usually includes • • • listening on the part of the clinician patient disclosure of medical/social info development of comfort participation in shared decision making patient satisfaction empathy
What is empathy? • distinct from sympathy or “feeling sorry” – vital element for the doctor-patient relationship – not just the “softer side” of medicine • research suggests increased patient satisfaction, patient compliance • = the ability to momentarily experience the feelings of another & communicate this – to put oneself in another person’s place

The biopsychosocial model
The biomedical model • Traditional approach to the patient – Only biologic & medical aspects of care discussed – Doesn’t include psychological factors • psychiatric illness & stress can worsen medical conditions • problems caused by illness can cause psych difficulties – Doesn’t include social environment • can affect susceptibility to illness & illness outcome

Complexity of psychosocial level • Other things besides biological effects of medication or procedure contribute to outcome – doctor-patient communication – patient understanding and beliefs of illness and treatment – social barriers & support – unconscious barriers and alliances from both patient and physician
Complexity of psychosocial level • Many patients will already have existing preconceptions of illness, of your profession – sick role • protective role given to ill or injured person; may be assumed by individual or imposed by custom – transference • preconceptions of patient about health care • may relate how patients relate to you – countertransference • preconceptions of you about your patients • may subtly influence how you relate to patients
Transference • Originally a technical psychotherapy term – now roughly “the transferring of past experiences and ways of relating to others by the patient onto the clinician” • May be positive or negative, depending on the individual – clinicians may be surprised when patient views them negatively
Countertransference • The opposite of transference • Different patients may elicit different emotions – adoring patients may elicit exaggerated concern – hostile patient may elicit defensiveness – older patients may elicit more deference • increasing research shows some patients receive different care in ways that does not appear to medically justified


Styles of relating • Relationship style may not be consciously chosen (modeling) – often adopted from mentors – some MDs may flexibly adapt style to fit clinical situation • Active-passive model – patient completely passive, takes no responsibility for their treatment – Stereotype of MD in early 1900 s as warm “father figure” – With technology, evolved into focus on disease • Still appropriate for infants or demented/agitated/unconscious patients
Styles of relating • Mutual participation model – – – – more interactive than active-passive model Equality & partnership between patient & MD MD brings expert advice patient brings personal experience & life priorities communication is less dominated by MD interaction typically warm & empathetic essential for chronic illnesses like diabetes, where active patient participation required for success
Styles of relating • Consumer-based style – options described by physician – decisions left in the hands of patient or bill-payer – occurs most frequently in non-serious illnesses (like plastic surgery) – interaction often cordial/businesslike – communication more dominated by patient – MD present to answer questions

Styles of relating • “Friendship” model – patients who feel “understood” often want to be friends – generally dysfunctional or unethical – professional boundaries may be blurred with sharing personal info, lending money, sexual contact • if severe, can lead to a malpractice suit or loss of license
Professional boundaries • Doctor-patient relationship is a fiduciary one that has at its core the element of trust – fiduciary = One that stands in a special relation of trust, confidence, or responsibility in certain obligations to others – [Latin fīdūciārius, from fīdūcia, trust]
Professional boundaries • Physician-patient relationship is not equal – – no matter how egalitarian you are patients seek your help as an expert you may be described as almost superhuman you are generally seen as an authority figure • like teachers or lawyers – usually present in a distressed or fearful state • intensity of emotional experience usually more powerful
Professional boundaries • Since some emotional involvement is good (ie, empathy), where to draw the line? – in general not well defined, but involve breach of fiduciary relationship • • business transactions gifts & services special scheduling or duration of appointments romantic physical contact – this is always unethical
Professional boundaries • Professional organizations/Hippocratic oath state sex with patients to be unethical – Risk of exploitation since meaningful consent impossible – less clear about former patients – less clear about “key third parties” – AMA estimates 5 -10% of MDs have had romantic contact with patients • usually starts with nonsexual boundary violations
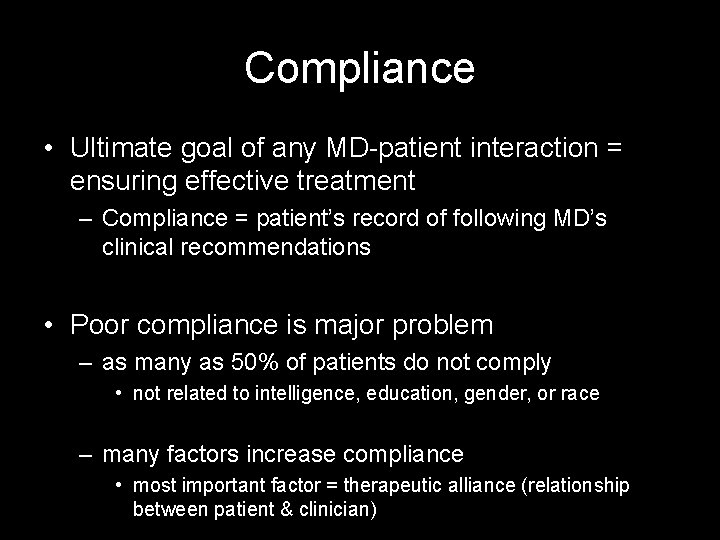
Compliance • Ultimate goal of any MD-patient interaction = ensuring effective treatment – Compliance = patient’s record of following MD’s clinical recommendations • Poor compliance is major problem – as many as 50% of patients do not comply • not related to intelligence, education, gender, or race – many factors increase compliance • most important factor = therapeutic alliance (relationship between patient & clinician)
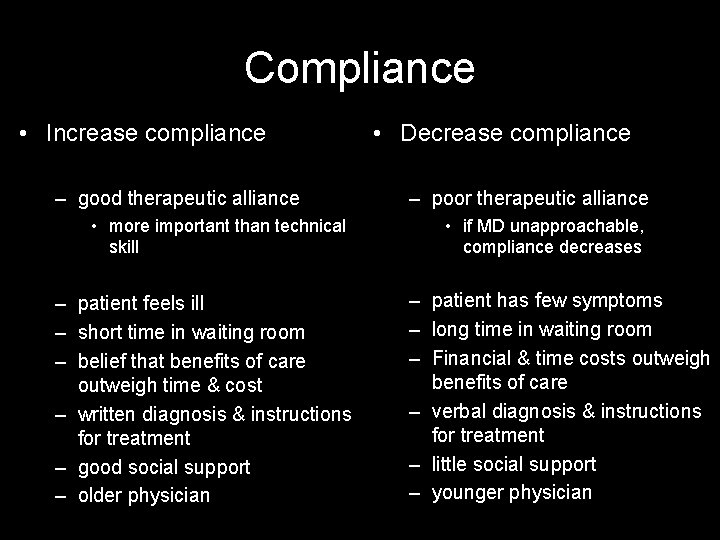
Compliance • Increase compliance – good therapeutic alliance • more important than technical skill – patient feels ill – short time in waiting room – belief that benefits of care outweigh time & cost – written diagnosis & instructions for treatment – good social support – older physician • Decrease compliance – poor therapeutic alliance • if MD unapproachable, compliance decreases – patient has few symptoms – long time in waiting room – Financial & time costs outweigh benefits of care – verbal diagnosis & instructions for treatment – little social support – younger physician
Difficult relationships • In general, difficult situations • Rules of thumb when dealing with difficult patients (or difficult patient questions) – you have primary responsibility for treating illness; referral inappropriate unless patient needs care you can’t provide – you must not let your patient’s emotions interfere with your judgment – you must always tell your patient the truth – you must identify problems that are a barrier to treatment • includes psychological problems (anger) or social problems (inability to comply)
Difficult relationships • A 50 year-old businessman angrily greets the doctor in the emergency department by complaining how long he had to wait before being seen.
Difficult relationships • A 34 year-old female patient behaves in a seductive manner and asks for the physician’s home phone number
Difficult relationships • A 50 year-old patient who smokes 2 packs of cigarettes a day comes to your office. After explaining the health hazards of smoking, you step out of the room. The patient then steps outside and begins to smoke.
Difficult relationships • A 44 year-old male comes to your office and complains about both his previous doctor’s treatment and your new secretary.
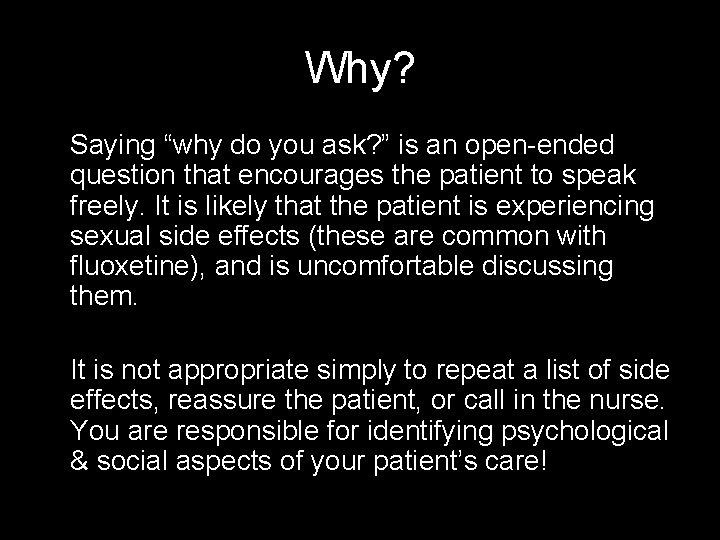
What would you do? Four months ago, when you prescribed fluoxetine (Prozac) for a patient, you explained the major side effects of the drug. Today at the next appointment, the patient asks you whether fluoxetine has any side effects. Your best response is: C. “Why do you ask? ”
Why? Saying “why do you ask? ” is an open-ended question that encourages the patient to speak freely. It is likely that the patient is experiencing sexual side effects (these are common with fluoxetine), and is uncomfortable discussing them. It is not appropriate simply to repeat a list of side effects, reassure the patient, or call in the nurse. You are responsible for identifying psychological & social aspects of your patient’s care!
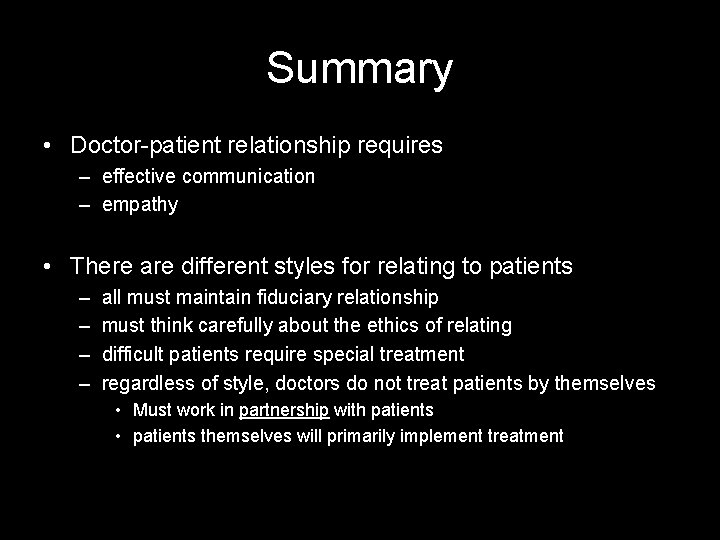
Summary • Doctor-patient relationship requires – effective communication – empathy • There are different styles for relating to patients – – all must maintain fiduciary relationship must think carefully about the ethics of relating difficult patients require special treatment regardless of style, doctors do not treat patients by themselves • Must work in partnership with patients • patients themselves will primarily implement treatment

Readings • Read Fadem (BRS) chapter 21
 沈榮麟
沈榮麟 Employee relations in public relations
Employee relations in public relations Southern illinois university human resources
Southern illinois university human resources Duo mobile uiuc
Duo mobile uiuc Student accounts illinois state
Student accounts illinois state Net math uiuc
Net math uiuc Ibm academic initiative
Ibm academic initiative Lomonosov moscow state university international relations
Lomonosov moscow state university international relations Michael gutierrez sacramento city college
Michael gutierrez sacramento city college St michael's catholic college sixth form
St michael's catholic college sixth form Gst 111 communication in english
Gst 111 communication in english Wake tech admissions
Wake tech admissions Early college high school at midland college
Early college high school at midland college Definition of tourism
Definition of tourism Stranmillis university college
Stranmillis university college Norwegian police university college
Norwegian police university college Lincoln memorial university college of veterinary medicine
Lincoln memorial university college of veterinary medicine King saud university college of medicine
King saud university college of medicine King saud university college of medicine
King saud university college of medicine King saud university college of medicine
King saud university college of medicine University of iowa college of dentistry
University of iowa college of dentistry Clark university college board
Clark university college board Artesis plantijn university college of antwerp
Artesis plantijn university college of antwerp Norwegian defence university college
Norwegian defence university college King saud university college of pharmacy
King saud university college of pharmacy King saud university college of medicine
King saud university college of medicine Lms ucj
Lms ucj Oslo and akershus university college
Oslo and akershus university college University b.t. & evening college
University b.t. & evening college University college of norwegian correctional service
University college of norwegian correctional service Queen's university early childhood education
Queen's university early childhood education Bangkok university international college
Bangkok university international college Stranmillis university college
Stranmillis university college