Doc does my pet really need all these




- Slides: 87
Doc, does my pet really need all these medications to treat his liver disease? Lisa Carioto, DVM, DVSc, Diplomate ACVIM 1
What prompted me to choose such a title for this presentation? 2
Cody • Treatments à Mitotane (Lysodren®) à Vitamin E 200 IU per day à Vitamin B 50 complex 50 mg PO q 12 h à Silymarin (Milk thistle) 175 mg PO q 24 h à SAMe (Denosyl®) 90 mg PO q 12 h à Omega-3 fatty acids 1 capsule PO q 24 h 3
Objectives • Hepatic disease and the multitude of treatments that exist • Case studies 4
Taz • 3 year old MN Havanese • Referred for à Persistent ↑ of ALT à ↑ of serum bile acids (SBA) 5
Taz - History • At 1 year of age à Pre-anaesthetic blood work à ALT: elevated (result not available) • At 2 years, 2 months à Ocular discharge and excessive licking of paws à ALT: 240 (10 - 100 U/L) 6

Taz - History • At 2 years, 6 months à Vomiting and diarrhea / hematochezia à ALT : 147 (10 - 100 U/L) à Metronidazole x 4 days • 1 month post vomiting and diarrhea episode à SBA » Pre: » Post: 7 2. 0 74. 0 (0 - 6 umol/L) (0 - 15 umol/L)
Taz - History • Presumptive diagnosis of atopy +/or food allergy à Severe pruritus, worse during summer à Elimination diet initiated 1 week prior to referral » Duck and sweet potato » Multiple vitamin • Only pet in the house • Vaccines current • No history of medications 8
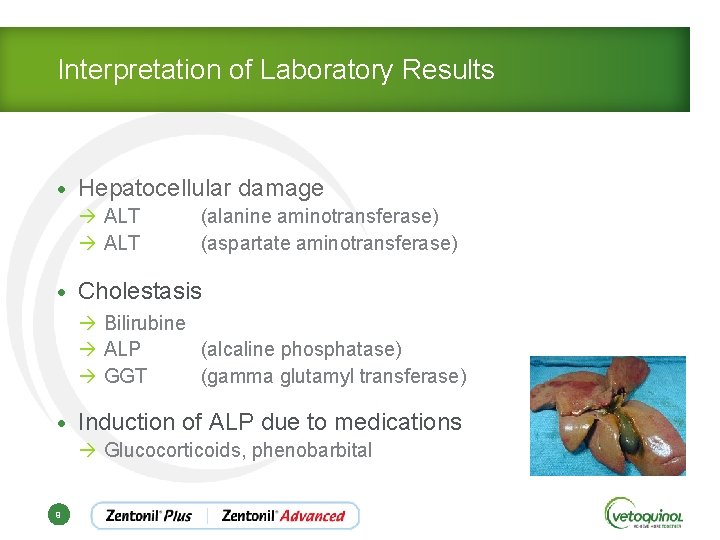
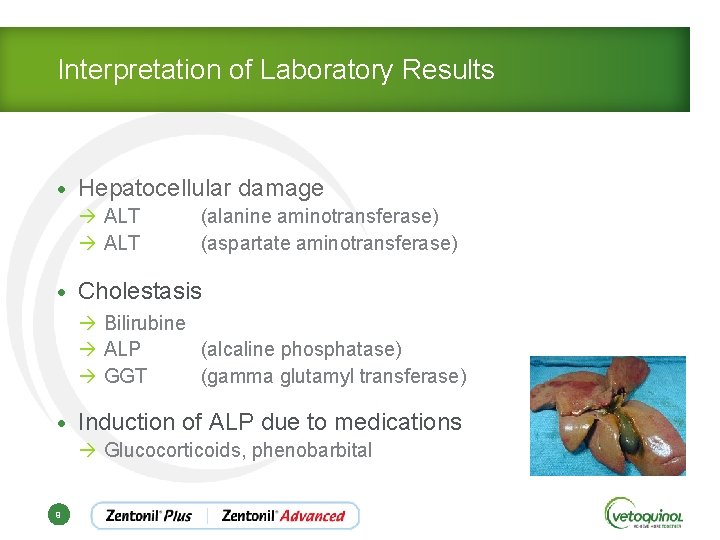
Interpretation of Laboratory Results • Hepatocellular damage à ALT (alanine aminotransferase) à ALT (aspartate aminotransferase) • Cholestasis à Bilirubine à ALP (alcaline phosphatase) à GGT (gamma glutamyl transferase) • Induction of ALP due to medications à Glucocorticoids, phenobarbital 9
Taz – Physical Exam • 8, 3 kg; body condition score 3/5 • BAR, active • No abnormal findings (NAF) other than ptyalism à Secondary to nausea due to transportation 10
Taz – Diagnostic Procedures • CBC • Serum biochemical profile • Urinalysis • Abdominal ultrasound 11
Taz – Diagnostic Procedures • CBF: NAF • Serum biochemical profile à ALT 64 U/L (4, 0 – 62 U/L) • Urinalysis (cystocentesis) à p. H 8 à DU 1, 047 12
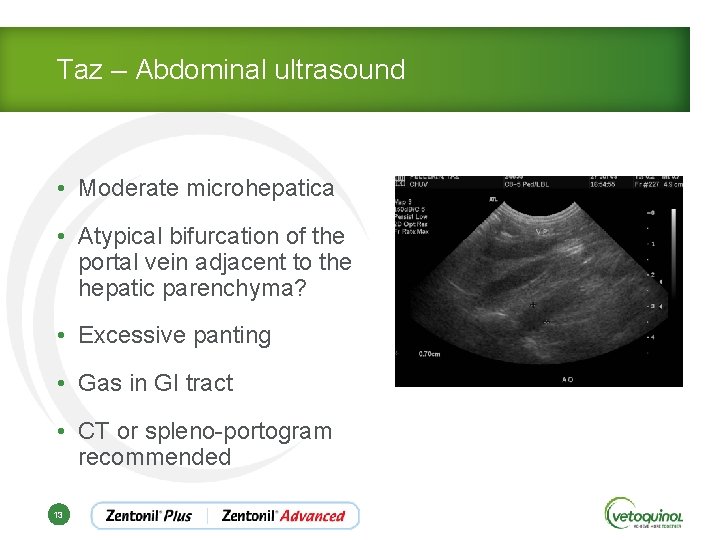
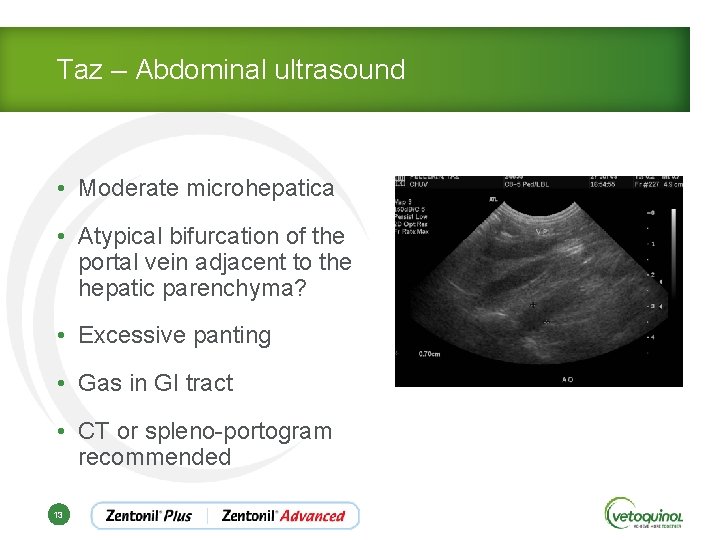
Taz – Abdominal ultrasound • Moderate microhepatica • Atypical bifurcation of the portal vein adjacent to the hepatic parenchyma? • Excessive panting • Gas in GI tract • CT or spleno-portogram recommended 13
Taz – Recommendations • Active hepatic damage suspected • +/- porto-systemic shunt (PSS) • Owner hesitant to pursue further work-up. . . • Re-evaluate hepatic profile and SBA in 2 -3 months • 6 months later (r. DVM) à SBA still elevated » Pre: » Post: 14 3, 0 69, 0 (0 - 6 umol/L) (0 - 15 umol/L)
Taz – 6 months later (FMV) • NAF on PE • Serum biochemical profile à ALT 41 U/L (4, 0 – 62 U/L) • Partial abdominal ultrasound of liver à Moderate microhepathica still present à No evidence of PSS • How can one explain the microhepatica? 15
Taz - Differential Diagnoses • Porto-systemic shunt (PSS) à Congenital (breed predisposition) à Acquired • Hepatic portal venous hypoplasia à Previously known as microvascular dysplasia à Microscopic shunts (breed predisposition) 16
Taz - Differential Diagnoses • History of an insult à Toxic? à Viral? Bacterial? à Immune-mediated (hepatitis) with 2° fibrosis? » Formerly chronic-active/idiopathic hepatitis à Familial hepatitis » Copper accumulation 17
Taz - Differential Diagnoses • Reactive hepatopathy à Extra-hepatic disease responsable of the increased liver enzymes » IBD, pyelonephritis, pancreatits, etc. • Others à Bone disease, growth (dogs), drugs, etc. 18
Taz - Other diagnostic tests? • CT scan à No evidence of a PSS • Aerobic and anaerobic culture: No growth • Copper level: 98 ppm (30 -100) • Hepatic biopsy à Early stages “lobular dissecting fibrosis” of unknown etiology 19
Taz - Treatment • SAMe 200 mg PO once a day and • Silymarin/silybin 20 – 50 mg/kg PO per day or • Zentonil® Advanced (Vetoquinol) 200 mg PO/day • Denamarin® (Nutramax) in US 20

Treatments for Hepatic Disease 21 21
Immunosuppressive Treatments Prednisone/Prednisolone • Anti-inflammatory • Immunosuppressive agent • Anti-fibrotic • Choleretic • Indication à Chronic hepatitis with mononuclear inflammation, without evidence of infection 22
Immunosuppressive Treatments Prednisone/Prednisolone • Cats must metabolise prednisone to prednisolone • Limited oral bioavailability in cats (Center, ACVIM 2010) • Prednisolone at 1 -2 mg/kg PO per day (ideal BW) • Gradual weaning q 2 weeks • Minimum effective dose (ex. q 48 h) for 2 -3 months … 23
Immunosuppressive Treatments Prednisone/Prednisolone • Some animals require steroids for 6 months to 1 year or possibly life long, depending upon the underlying cause of the inflammation • Steroids will increase liver enzyme activities in dogs à Difficult to determine efficacy of treatment 24
Other Immunosuppressive Agents • Second medication added to prednisone if necessary • Goal à Steroid sparing effect 25
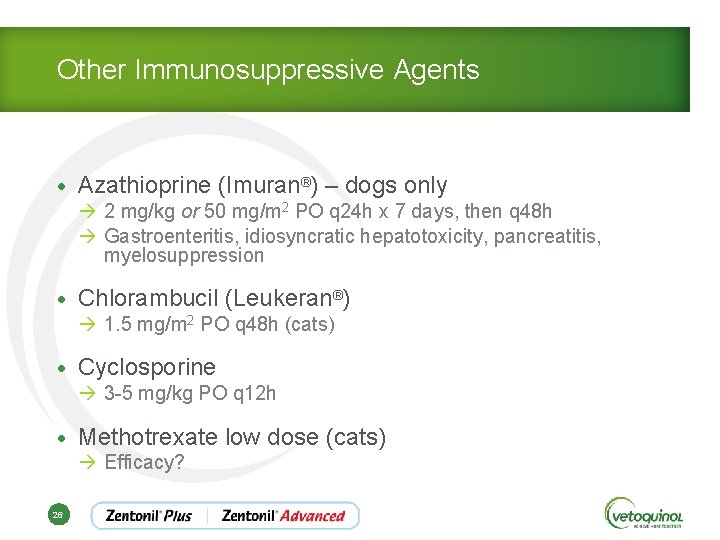
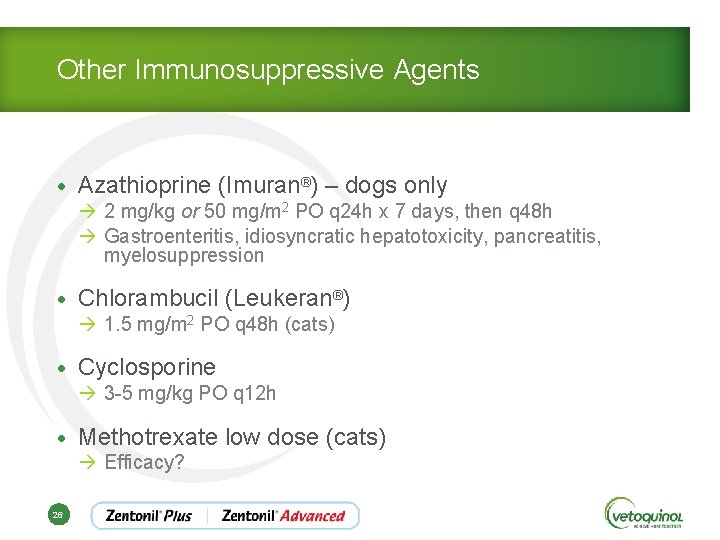
Other Immunosuppressive Agents • Azathioprine (Imuran®) – dogs only à 2 mg/kg or 50 mg/m 2 PO q 24 h x 7 days, then q 48 h à Gastroenteritis, idiosyncratic hepatotoxicity, pancreatitis, myelosuppression • Chlorambucil (Leukeran®) à 1. 5 mg/m 2 PO q 48 h (cats) • Cyclosporine à 3 -5 mg/kg PO q 12 h • Methotrexate low dose (cats) à Efficacy? 26
Treatments - Anti-fibrotics • Prednisone/prednisolone • Silymarin/silybin (Silybum marianum) à Milk thistle • S-adenosylmethionine (SAMe) • Zinc • Colchicine 27
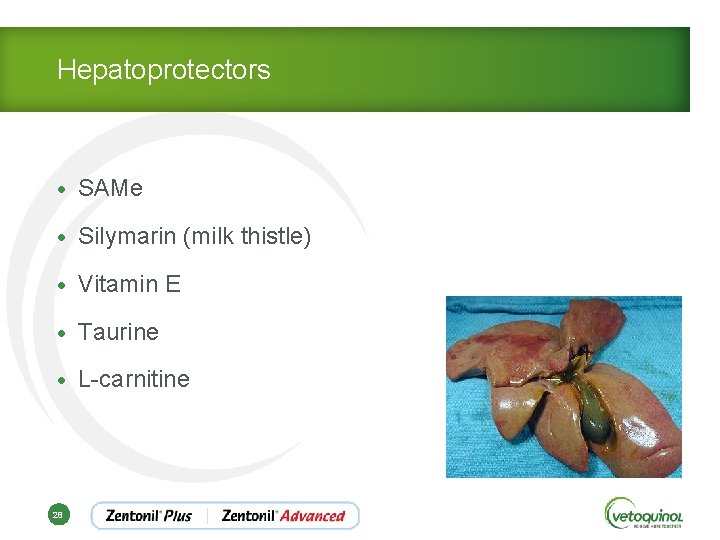
Hepatoprotectors • SAMe • Silymarin (milk thistle) • Vitamin E • Taurine • L-carnitine 28
Hepatoprotectors S-adenosylmethionine (SAMe) • Natural metabolite of hepatocytes • Decreased SAMe-synthetase enzyme during liver disease contributes to a decrease in SAMe and glutathion • Precursor of glutathion à The most important antioxidant 29
Hepatoprotectors - SAMe • Most important methyl donor of cellular metabolism • Transmethylation à Regulates the plasticity of cellular membranes and reinforces their integrity • Transsulfuration à Glutathione production 30
Hepatoprotectors - SAMe • Anti-oxydant à Helps prevent accumulation of free radicals by increasing hepatic glutathione levels in dogs and cats • Stabilization of the cell membrane function and improves fluidity of hepatocytes à Improvement in the conjugation of SBA à ↑ flow of bile 31
Hepatoprotectors - SAMe • Modulation of cytokine expression • Improves cellular regeneration • Anti-apoptotic effect in normal cells • Anti-fibrotic? • Anti-neoplastic (hepatocellular carcinoma) à Mice, in vitro human hepatic cells 32
Hepatoprotectors - SAMe • Crosses BBB sensation of well being à Anti-depressant in humans à Treatment of cognitive dysfunction » Rème CA et al. Veterinary Therapeutics, summer 2008 - Double blinded study - SAMe (Novifit® - Virbac) was more efficacious than placebo in increasing activity level, interest and therefore quality of life in older dogs 33
Hepatoprotectors - SAMe • Denosyl® SD 4 (Nutramax) • Zentonil™ (Vetoquinol) • Do not crush, chew or divide the tablets as will affect bioavailability of product • Question of owner compliance 34
Hepatoprotectors - SAMe • Zentonil™ remplaced by • Zentonil® Plus and Zentonil® Advanced à Microencapsulation technology allows one to divide, crush or chew tablets without affecting the bioavailability of SAMe à Palatable – meat flavor, vegetable origine à Rare side effects » Vomiting, cramps, diarrhea 35
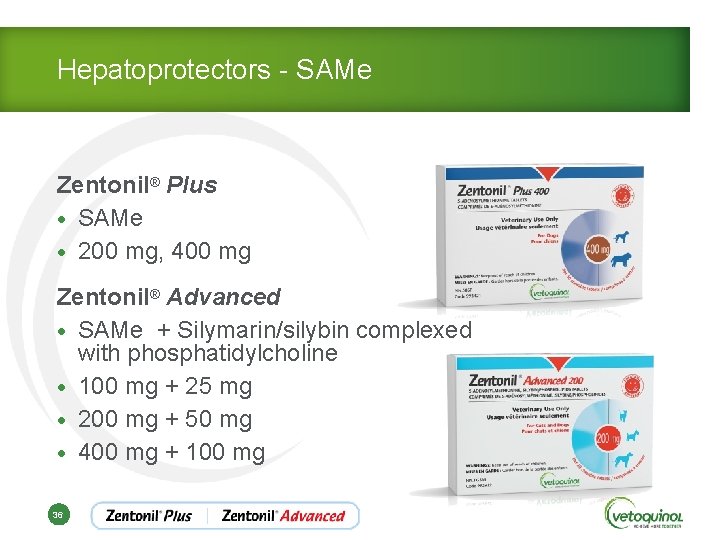
Hepatoprotectors - SAMe Zentonil® Plus • SAMe • 200 mg, 400 mg Zentonil® Advanced • SAMe + Silymarin/silybin complexed with phosphatidylcholine • 100 mg + 25 mg • 200 mg + 50 mg • 400 mg + 100 mg 36
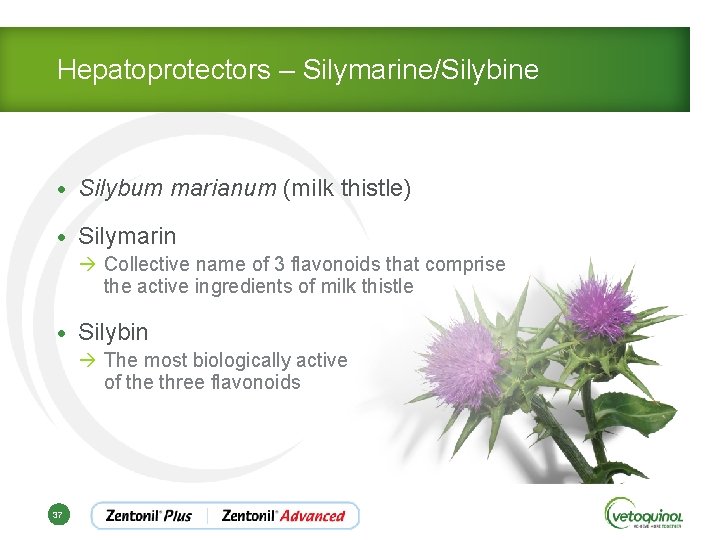
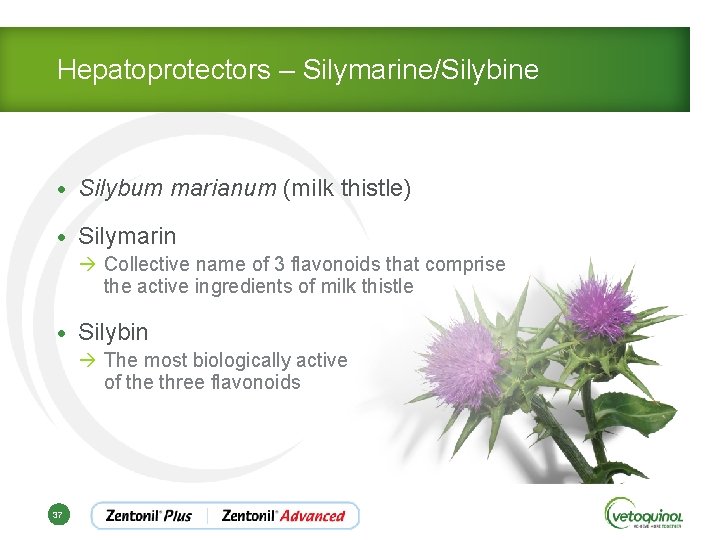
Hepatoprotectors – Silymarine/Silybine • Silybum marianum (milk thistle) • Silymarin à Collective name of 3 flavonoids that comprise the active ingredients of milk thistle • Silybin à The most biologically active of the three flavonoids 37

Hepatoprotectors – Silymarine/Silybine • Hepatoprotective properties of silybin are well documented à Anti-oxydant » Free radical scavenger » Regulator of intracellular concentrations of glutathione » Anti-inflammatory à Immuno-modulator 38
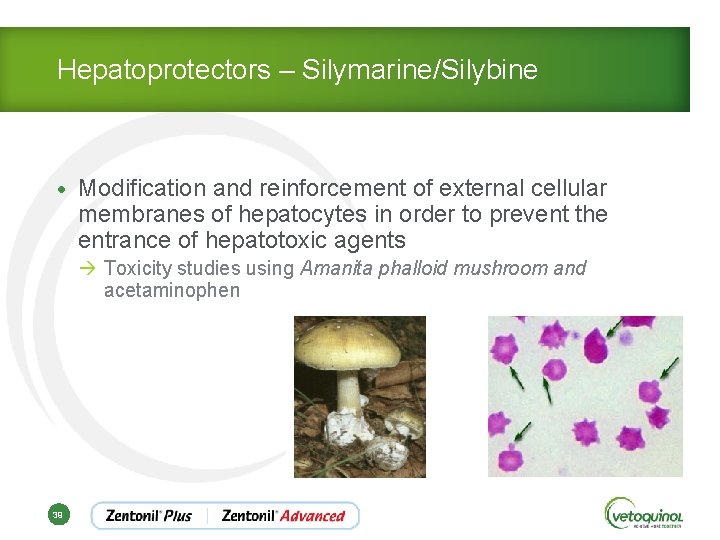
Hepatoprotectors – Silymarine/Silybine • Modification and reinforcement of external cellular membranes of hepatocytes in order to prevent the entrance of hepatotoxic agents à Toxicity studies using Amanita phalloid mushroom and acetaminophen 39
Hepatoprotectors – Silymarine/Silybine • Increased solubility of bile • Anti-fibrotic à Inhibits the transformation of Kupffer cells (stellate hepatocytes) into myofibroblasts • Stimulates hepatocyte regeneration à Promoter of ribosomal RNA synthesis 40
Hepatoprotectors – Silymarine/Silybine • Oral absorption and bioavailability of silybin are improved significantly when complexed with phosphatidylcholine • No side effects documented 41
Hepatoprotectors – Silymarine/Silybine • Use of human supplements à Concerns regarding » Quality control » Appropriate dose in dogs and cats? • Zentonil® Advanced (Vetoquinol) specifically developped for the veterinary market à Therapeutic dose 5 -10 mg/kg/day 42
Hepatoprotector - Vitamin E • Alpha-tocopherol • Anti-oxidant • Protect against different types of membrane peroxidation • Anti-inflammatory effect • Anti-fibrotic? • Dogs and cats à 10 - 15 UI/kg PO per day 43
Hepatoprotectors • Vitamins B 1, B 2, B 5, B 6, B 12 à Multiple roles in hepatic metabolism » Ex. : Cofactors, coenzymes, etc. • Omega-3 s à Anti-inflammatory » AEP: 40 mg/kg/day » ADH: 25 mg/kg/day 44
Hepatoprotector Ursodeoxycholic acid (Ursodiol®) • Natural BA • Choleretic à Stimulates bile flow à Medical management of sludge and mucocoeles • Changes the bile acid pool to a less hepatotoxic form • Anti-apoptosis, anti-oxidant, stabilizes mitochondriae, anti-inflammatory, immune-modulator 45
Hepatoprotector Ursodeoxycholic acid (Ursodiol®) • 10 -15 mg/kg PO per day, divided BID (chiens et chats) • Give with food • Contraindication à Biliary obstruction • Therapeutic effect of UA is increased by the concurrent administration of SAMe à Synergistic vs additive? 46
Treatments – Copper Chelators (dogs) • 2, 2, 2 -tetramine = Trientine HCl (Syprine®) • D-penicillamine • Zinc acetate 47
Treatments - Antibiotics Indications • Biliary infection or hepatic parenchyma à Neutrophilic leucocytosis, left shift, toxic/degenerative changes • Fever • Suppurative inflammation on histopathology • Hepatic encephalopathy à ↓ the population of colonic bacteria, therefore ↓ ammonia production 48
Treatments - Antibiotics • E. coli, Enterococcus, Clostridium, Staphylococcus, Streptococcus, Klebsiella, Clostridium, Bacteroides • Ampicillin ou amoxicillin • Amoxicillin/clavulanic acid à Clavaseptin®, Clavamox® • Metronidazole à Decreases anaerobic bacteria à Metabolized by the liver, therefore use 25 -50% of the standard dose à 7, 5 mg/kg PO q 12 h 49
Treatments - Antibiotics • Neomycin à Prevents the conversion of glutamine to ammonia by the enterocyte à Not systemically absorbed à 22 mg/kg PO q 12 h • Cepalosporins (cephalexin (PO), cefazolin (IV)) • +/- Fluoroquinolone 50
Treatments - Diet One must differentiate between hepatic disease and hepaætic insufficiency 51
Treatments - Diet • Hepatic disease à Elevation of enzyme activities, but hepatic function is adequate » Urea, albumin, glucose within normal limits à It is therefore NOT necessary to use a protein – restricted diet, however high quality protein diet is required » >14% of daily caloric requirements, ideally >20% • Protein restriction only if signs of HE 52
Treatments - Diet • Rich in soluble fibre à To ↓ the availability and production of ammonia at the level of the intestine à To bind noxious bile acids, endotoxins, etc. • Rich in vitamin B complex 53
Treatments - Diet • Supplemented with à K+, Zn 2+, Ca 2+, arginine, taurine, carnitine • Avoid à Iron, copper and sodium » If ascites is present (<0. 5 g Na/1000 kcal) • Small, frequent meals to avoid protein and ammonia overload of the liver 54
Monitoring • Clinical signs • Weight and BCS score • Blood tests à Albumin à Bilirubin à Urea à Glucose • Ideally: re-biopsy 55 - ALT - ALP - GGT - Electrolytes
Toby • 8 years old, MN Balinese • Intermittent episodes of anorexia, lethargy and fever (40. 7°C) x 5 months’ duration • Weight loss • Vomiting and diarrhea of a few days’ duration • Today: depressed anorexic 56
Toby • Tendency to eat foreign bodies à Vomiting episode after ingestion of adhesive tape (August) • Lives with another cat (Persian) • Both live indoors • Vaccines et deworming current 57
Toby • r. DVM in October à Temperature : 40, 4°C à Abdominal pain à Weight loss since August (approximately 3 months ago) à 3. 71 kg today vs. 3. 41 kg (August) 58
Toby • r. DVM in October à Treatments » Cefovecin (Convenia®) » Meloxicam (Metacam®) x 4 days » SQ fluids » Cyproheptadine (Periactin®) » Metronidazole x 14 days à Improvement noted, but recurrence 5 days after having discontinued the metronidazole 59
Toby – Physical exam • T: 39, 7°C P: 220 bpm R: 28 • Icteric • Prolonged skin tent • Tacky mucous membranes • Abdominal palpation à Pain and organomegaly 60
Toby – Problems List • Anorexia • Vomiting • Diarrhea • Icterus • Pyrexia • Abdominal pain and organomegaly • Dehydration estimated at ~ 8% 61
Toby – Differential Diagnoses • Cholangitis/cholangiohepatitis • Pancreatitis • Inflammatory bowel disease • Triaditis • Primary hepatic lipidosis • Neoplasia • FIP 62
Toby – Differential Diagnoses • CBC, serum biochemical profile, urinalysis • Urine culture • Fe. LV/FIV done at r. DVM (negative) • PT/PTT • f PLI • Abdominal radiographs • Abdominal ultrasound 63
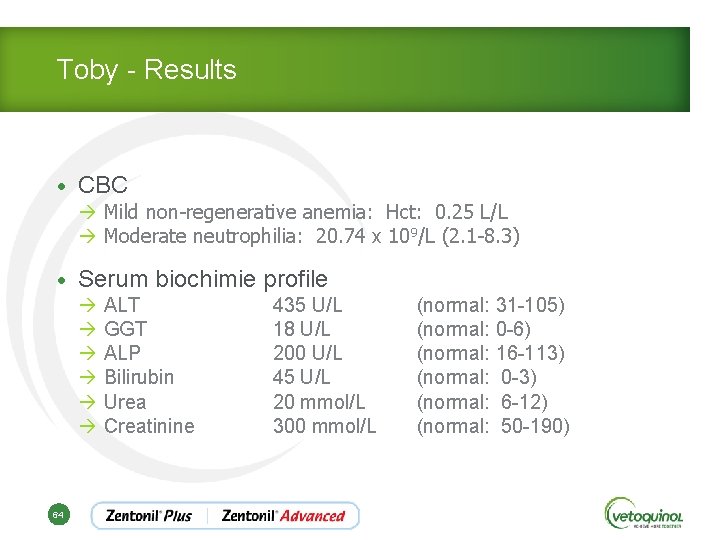
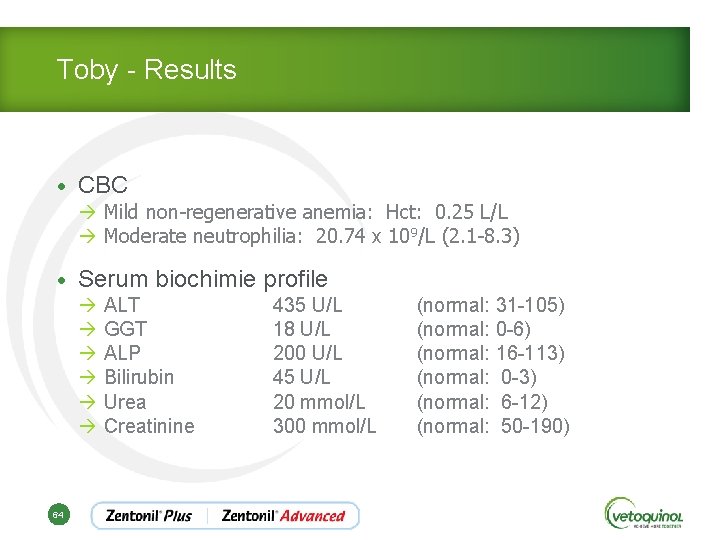
Toby - Results • CBC à Mild non-regenerative anemia: Hct: 0. 25 L/L à Moderate neutrophilia: 20. 74 x 109/L (2. 1 -8. 3) • Serum biochimie profile à ALT 435 U/L à GGT 18 U/L à ALP 200 U/L à Bilirubin 45 U/L à Urea 20 mmol/L à Creatinine 300 mmol/L 64 (normal: 31 -105) (normal: 0 -6) (normal: 16 -113) (normal: 0 -3) (normal: 6 -12) (normal: 50 -190)
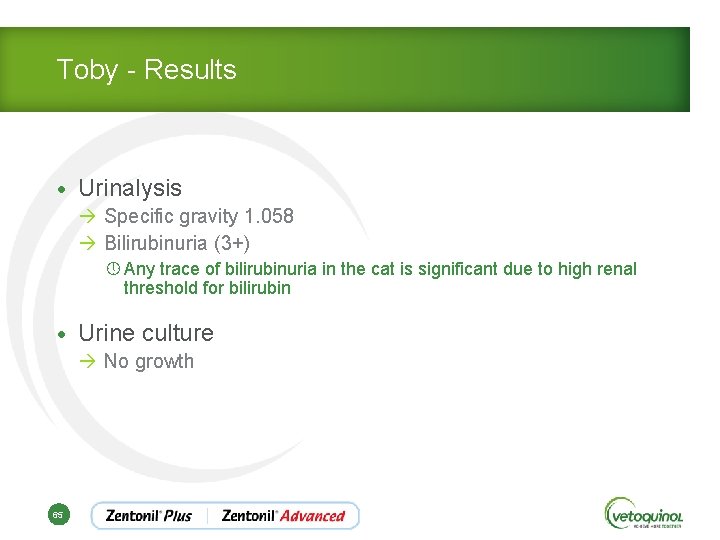
Toby - Results • Urinalysis à Specific gravity 1. 058 à Bilirubinuria (3+) » Any trace of bilirubinuria in the cat is significant due to high renal threshold for bilirubin • Urine culture à No growth 65
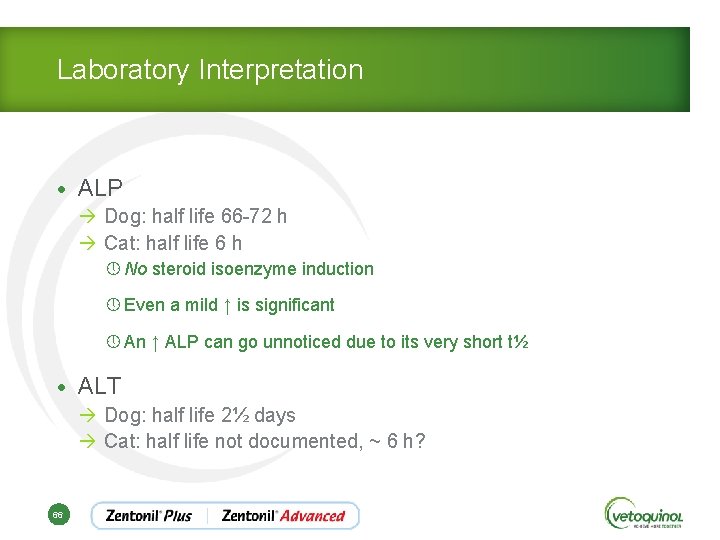
Laboratory Interpretation • ALP à Dog: half life 66 -72 h à Cat: half life 6 h » No steroid isoenzyme induction » Even a mild ↑ is significant » An ↑ ALP can go unnoticed due to its very short t½ • ALT à Dog: half life 2½ days à Cat: half life not documented, ~ 6 h? 66
Laboratory Interpretation • AST à Dog: half life 22 h à Cat: half life 77 minutes 67
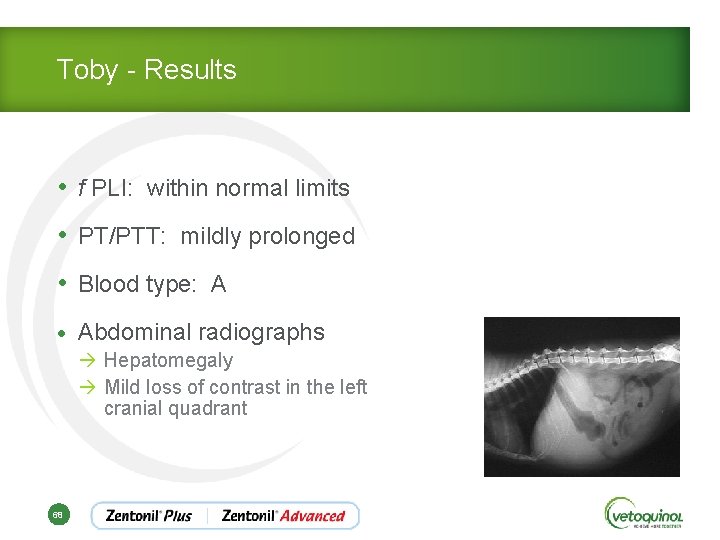
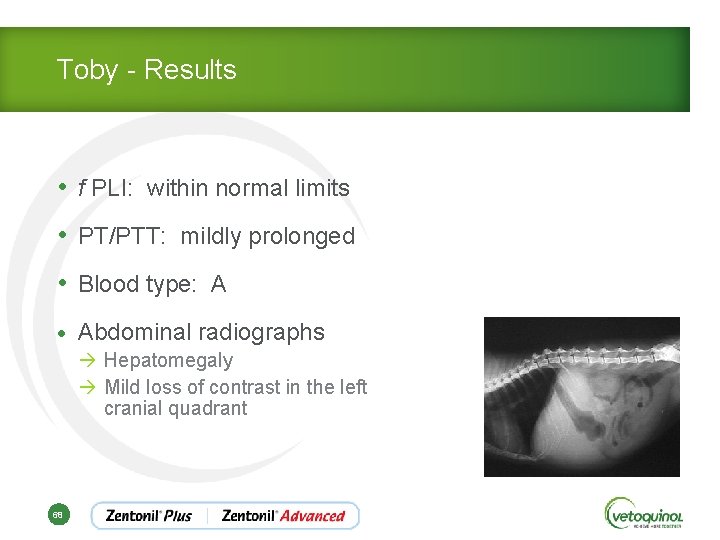
Toby - Results • f PLI: within normal limits • PT/PTT: mildly prolonged • Blood type: A • Abdominal radiographs à Hepatomegaly à Mild loss of contrast in the left cranial quadrant 68
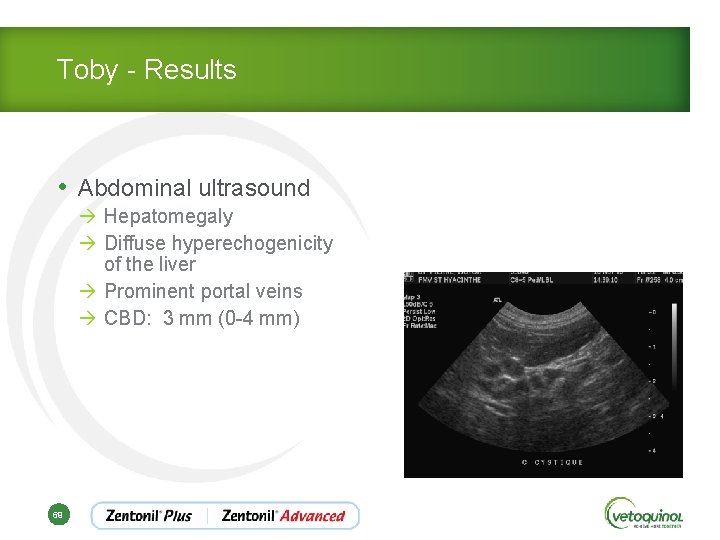
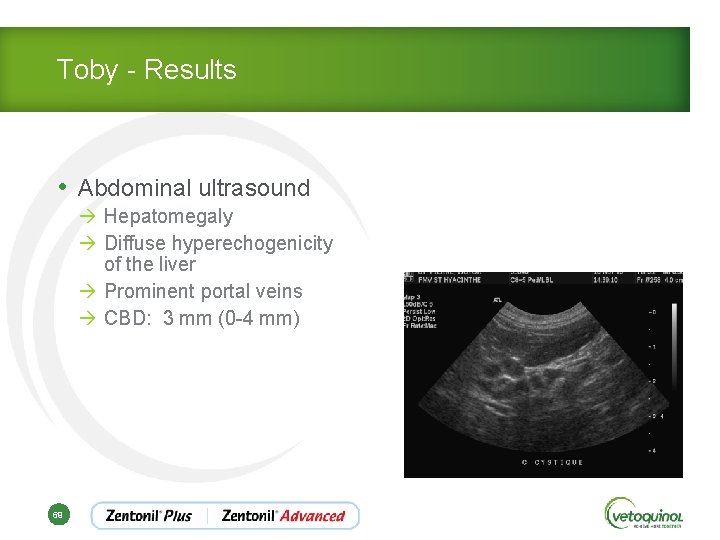
Toby - Results • Abdominal ultrasound à Hepatomegaly à Diffuse hyperechogenicity of the liver à Prominent portal veins à CBD: 3 mm (0 -4 mm) 69
Toby - Traitements • Intravenous fluids (IV) • Fresh frozen plasma (coagulation factors) • Vitamin K 1 SQ à 0. 5 -1 mg/kg q 8 -12 h à 1 to 3 doses prior to performing biopsies • Fine needle aspiration of liver and GB • Hepatic biopsy • Culture and sensitivity of bile and hepatic tissue 70
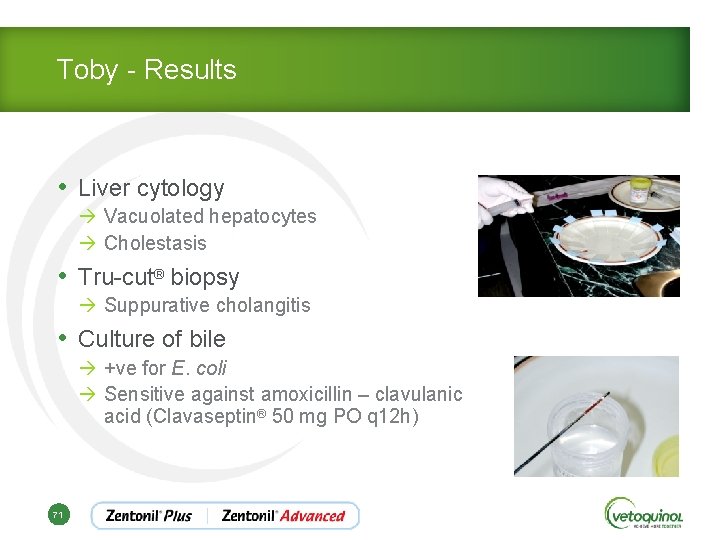
Toby - Results • Liver cytology à Vacuolated hepatocytes à Cholestasis • Tru-cut® biopsy à Suppurative cholangitis • Culture of bile à +ve for E. coli à Sensitive against amoxicillin – clavulanic acid (Clavaseptin® 50 mg PO q 12 h) 71
Toby - Treatments • Feeding via nasoesophagial tube • Ampicillin IV • Analgesics • Anti-emetics Once started eating • Clavaseptin® ~ 8 -12 weeks • Ursodiol® q 24 h • SAMe/silybin (Zentonil® Advanced) q 24 h 72
Toby - Treatments • Monitoring of hepatic enzymes q 4 -6 weeks • First re-evaluation (at 4 weeks) à BAR à Moderate improvement of ALT, ALP and GGT • Clavaseptin® q 12 h • Ursodiol® q 24 h • SAMe/silybin (Zentonil® Advanced) q 24 h 73
Toby - Treatments • 2 nd re-evalutaiton (at 8 weeks) à BAR, active, eating well à ALT very mildly elevated à ALP and GGT within normal limits • Clavaseptin® q 12 h • Ursodiol® PO q 48 heures x 1 month • Zentonil® Advanced q 24 h 74
Toby - Treatments • 3 rd re-evaluation (at 12 weeks) à à ALT, ALP and GGT within normal limits Clavaseptin®: continue an additional 2 weeks Ursodiol®: discontinue Zentonil® Advanced q 24 h • 4 th re-evaluation (at 16 weeks) à ALT, ALP and GGT within normal limits à Clavaseptin®: discontinue à Zentonil® Advanced q 48 h x 2 additional weeks 75
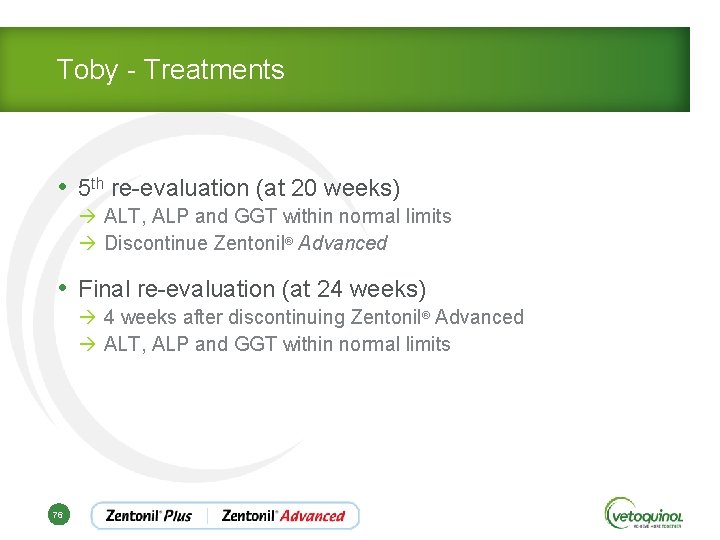
Toby - Treatments • 5 th re-evaluation (at 20 weeks) à ALT, ALP and GGT within normal limits à Discontinue Zentonil® Advanced • Final re-evaluation (at 24 weeks) à 4 weeks after discontinuing Zentonil® Advanced à ALT, ALP and GGT within normal limits 76
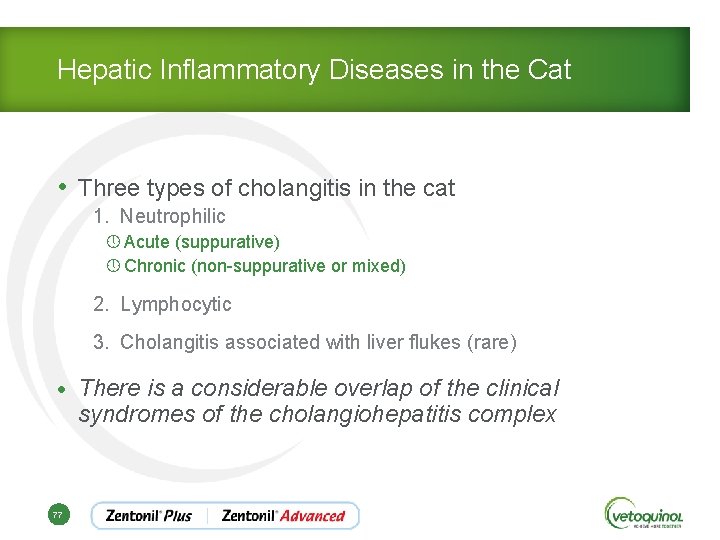
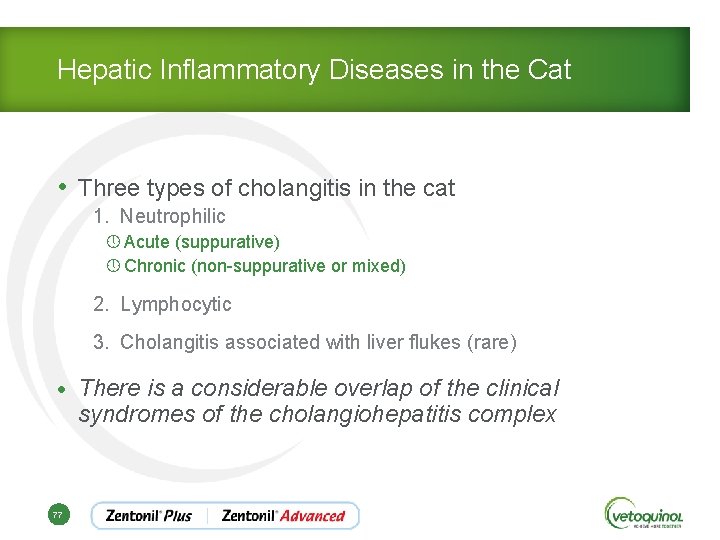
Hepatic Inflammatory Diseases in the Cat • Three types of cholangitis in the cat 1. Neutrophilic » Acute (suppurative) » Chronic (non-suppurative or mixed) 2. Lymphocytic 3. Cholangitis associated with liver flukes (rare) • There is a considerable overlap of the clinical syndromes of the cholangiohepatitis complex 77
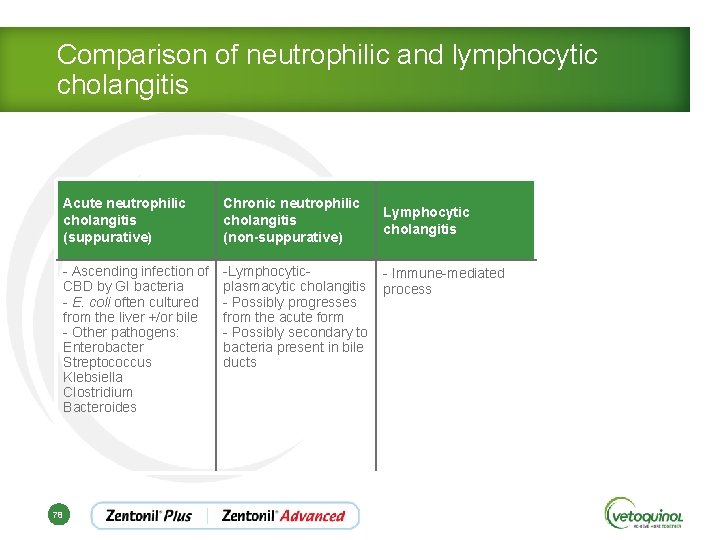
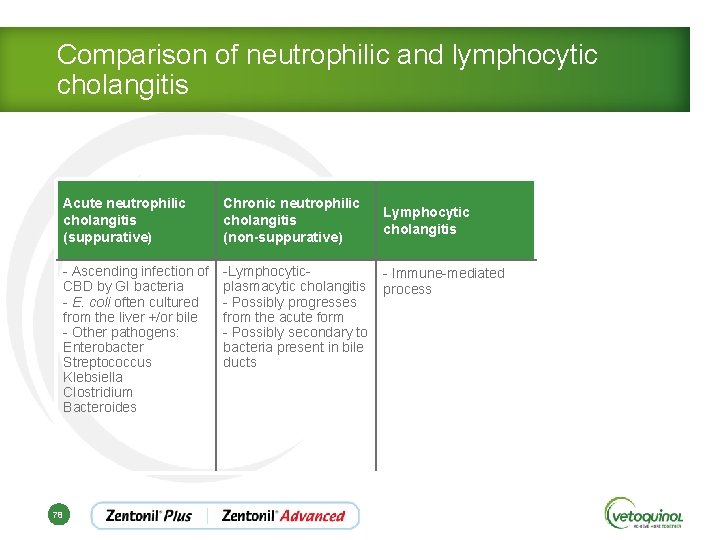
Comparison of neutrophilic and lymphocytic cholangitis Acute neutrophilic cholangitis (suppurative) Chronic neutrophilic cholangitis (non-suppurative) - Ascending infection of CBD by GI bacteria - E. coli often cultured from the liver +/or bile - Other pathogens: Enterobacter Streptococcus Klebsiella Clostridium Bacteroides -Lymphocytic- Immune-mediated plasmacytic cholangitis process - Possibly progresses from the acute form - Possibly secondary to bacteria present in bile ducts 78 Lymphocytic cholangitis
Inflammatory Hepatic Diseases in the Cat Treatments Acute neutrophilic cholangitis (suppurative) • IV fluids • Supportive treatment à Anti-emetics à Appetite stimulants 79
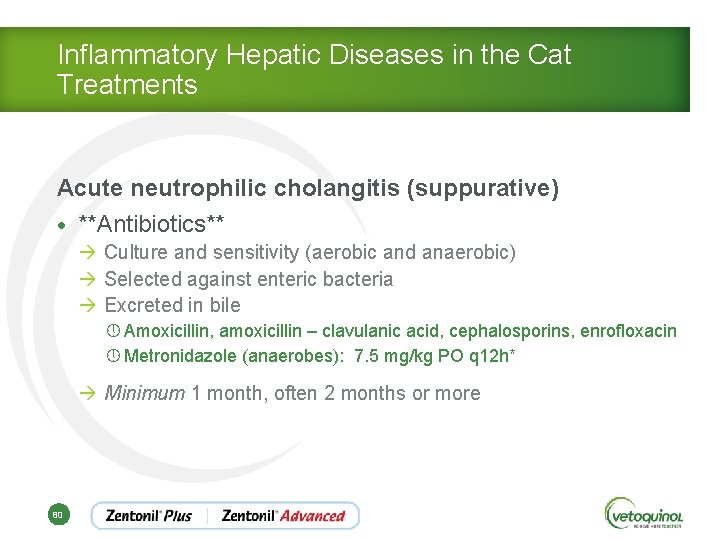
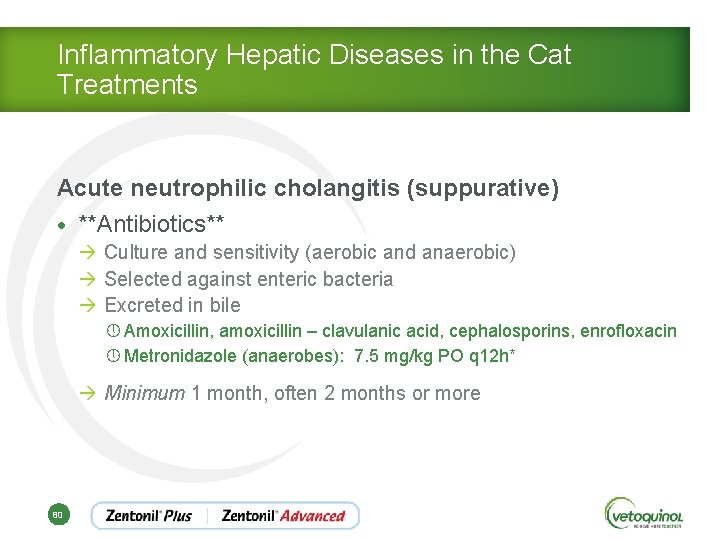
Inflammatory Hepatic Diseases in the Cat Treatments Acute neutrophilic cholangitis (suppurative) • **Antibiotics** à Culture and sensitivity (aerobic and anaerobic) à Selected against enteric bacteria à Excreted in bile » Amoxicillin, amoxicillin – clavulanic acid, cephalosporins, enrofloxacin » Metronidazole (anaerobes): 7. 5 mg/kg PO q 12 h* à Minimum 1 month, often 2 months or more 80
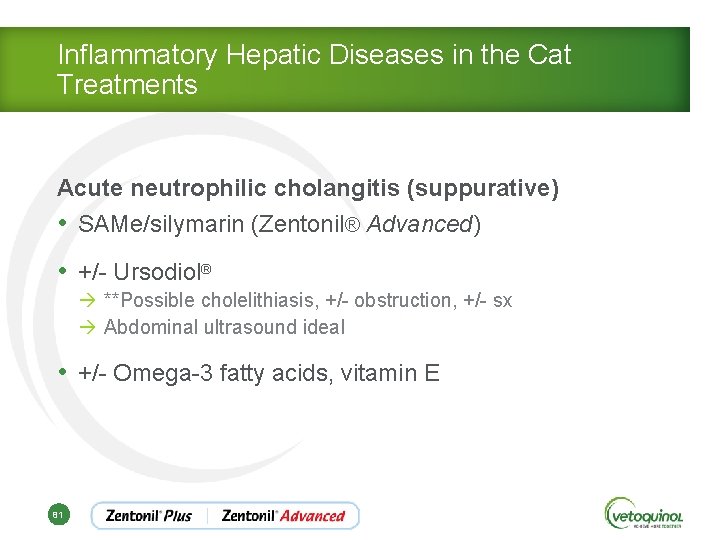
Inflammatory Hepatic Diseases in the Cat Treatments Acute neutrophilic cholangitis (suppurative) • SAMe/silymarin (Zentonil® Advanced) • +/- Ursodiol® à **Possible cholelithiasis, +/- obstruction, +/- sx à Abdominal ultrasound ideal • +/- Omega-3 fatty acids, vitamin E 81
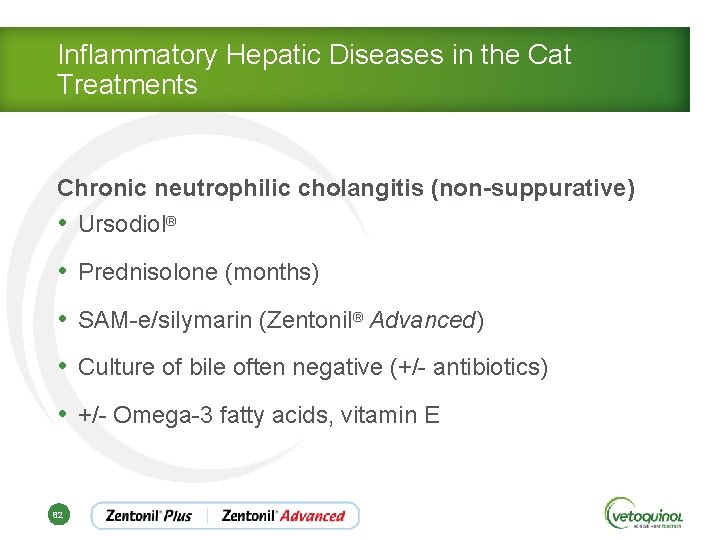
Inflammatory Hepatic Diseases in the Cat Treatments Chronic neutrophilic cholangitis (non-suppurative) • Ursodiol® • Prednisolone (months) • SAM-e/silymarin (Zentonil® Advanced) • Culture of bile often negative (+/- antibiotics) • +/- Omega-3 fatty acids, vitamin E 82
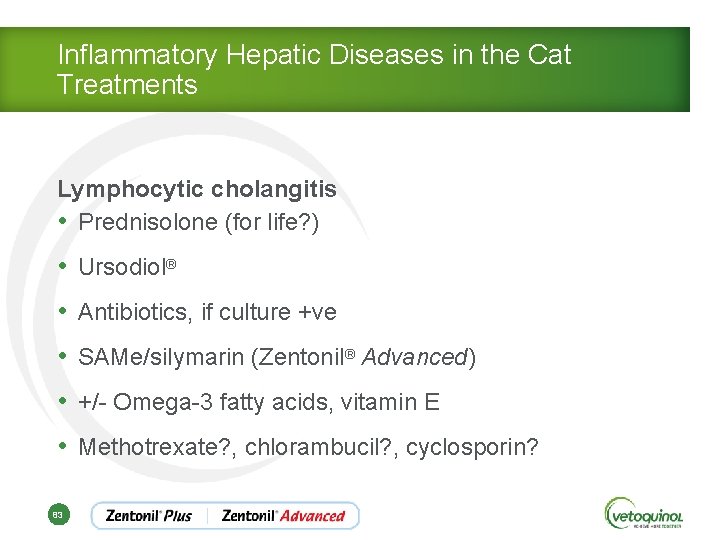
Inflammatory Hepatic Diseases in the Cat Treatments Lymphocytic cholangitis • Prednisolone (for life? ) • Ursodiol® • Antibiotics, if culture +ve • SAMe/silymarin (Zentonil® Advanced) • +/- Omega-3 fatty acids, vitamin E • Methotrexate? , chlorambucil? , cyclosporin? 83

What to do if client are unable to pursue a full work up? 84 84
Plan B • CBC, serum biochemical profile, urinalysis • Don’t run an f PLI or vitamin B 12 • Antibiotics à Minimum 1 month duration à If unable to re-evaluate liver enzyme activities, treat for 2 months 85
Plan B • SAMe/silymarin (Zentonil® Advanced) • +/- Vitamin B 12 injection • +/- Anti-emetics • +/- Appetite stimulant • If no, or little improvement noted after 2 -4 days… à Add prednisolone at an anti-inflammatory dose of 1 mg/kg/day 86
Conclusions • There a multitude of treatments available for hepatic disease • Adapt a treatment protocol for each individual • Introduce the treatments gradually to avoid overwhelming the patient and client 87