Delivering Medicaid Supportive Housing Services Through the Managed



- Slides: 32
Delivering Medicaid Supportive Housing Services Through the Managed Care System Washington Low Income Housing Alliance The Source for Housing Solutions

Our Mission Advancing housing solutions that: Improve lives of vulnerable people Maximize public resources Build strong, healthy communities
Your Presenters Debbie Thiele Dr. Marcella Maguire Dr. Tanya Dansky Chief Medical Officer National Consulting Director of Health Amerigroup Washingt Director, CSH Systems Integration, Debbie. thiele@csh. o CSH rg Marcella. maguire@csh. org
Poll!
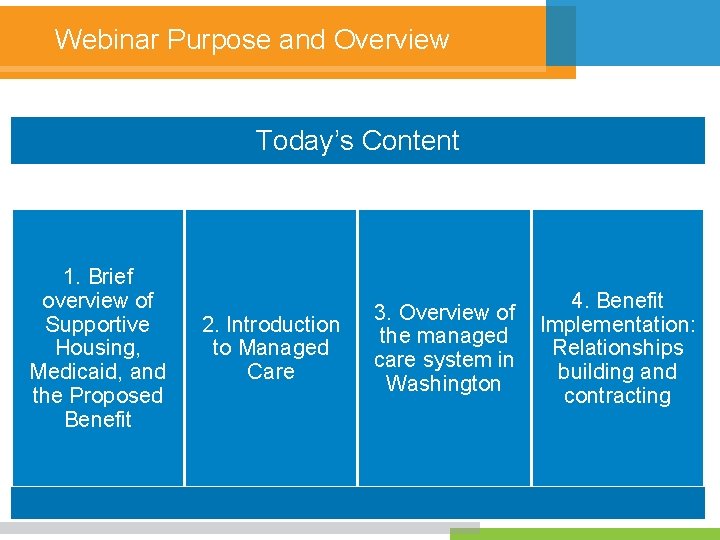
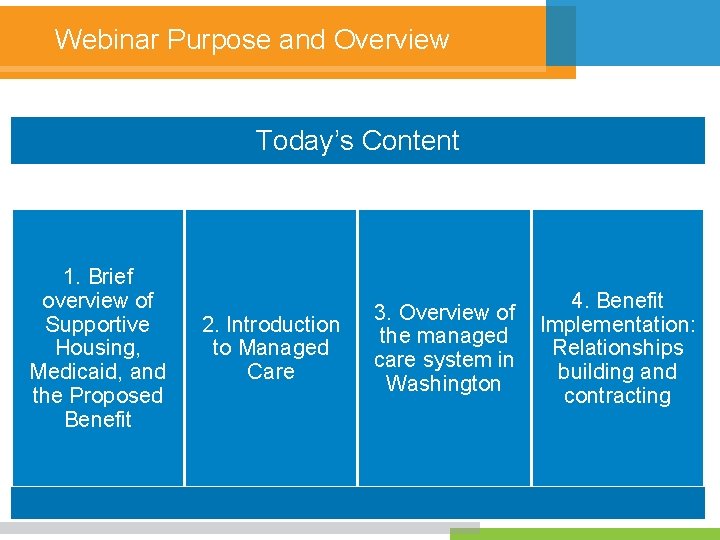
Webinar Purpose and Overview Today’s Content 1. Brief overview of Supportive Housing, Medicaid, and the Proposed Benefit 2. Introduction to Managed Care 3. Overview of the managed care system in Washington 4. Benefit Implementation: Relationships building and contracting
1. Overview of Supportive Housing, Medicaid, and the Proposed Supportive Housing Services Benefit The Source for Housing Solutions
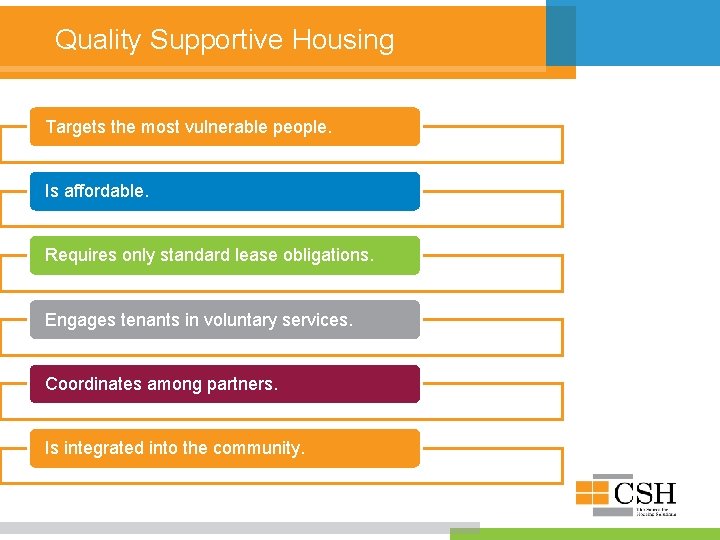
Quality Supportive Housing Targets the most vulnerable people. Is affordable. Requires only standard lease obligations. Engages tenants in voluntary services. Coordinates among partners. Is integrated into the community.
Medicaid
Medicaid & Supportive Housing Services The information in this Bulletin is based on evidence from studies demonstrating that providing housing-related activities and services facilitates community integration and is cost effective.
Eligible Services § Housing transition services that provide direct support to help individuals obtain housing, including: Housing assessment and development of a plan to address barriers. Assistance with applications, community resources, and outreach to landlords. § Housing tenancy sustaining services that help individuals maintain their housing, including: Education, training, coaching, resolving disputes, and advocacy.
2. Overview of Managed Care The Source for Housing Solutions

It’s a Whole New Language • Spanish • Italian – Bano – Gracias – Grazie – Dormitorio – Camera Da Letto
What is Medicaid Managed Care? § Managed Care is a health care delivery system organized to manage cost, utilization, and clinical and service quality. § Medicaid managed care provides for the delivery of Medicaid health benefits and additional services through contracted arrangements between state Medicaid agencies and managed care organizations (MCOs), such as health plans and behavioral health organizations (BHOs), that accept a set per member per month (capitation) payment for these services. 13
What is Medicaid Managed Care? § By contracting with MCOs, states can reduce Medicaid costs and better manage utilization of health services. § MCO contracts with the State Medicaid Agency are profitlimited contracts. § MCOs strive to reinvest cost savings through shared savings programs and provider partnerships. § Improvement in health plan performance, health care quality, and outcomes are key objectives of Medicaid managed care. 14
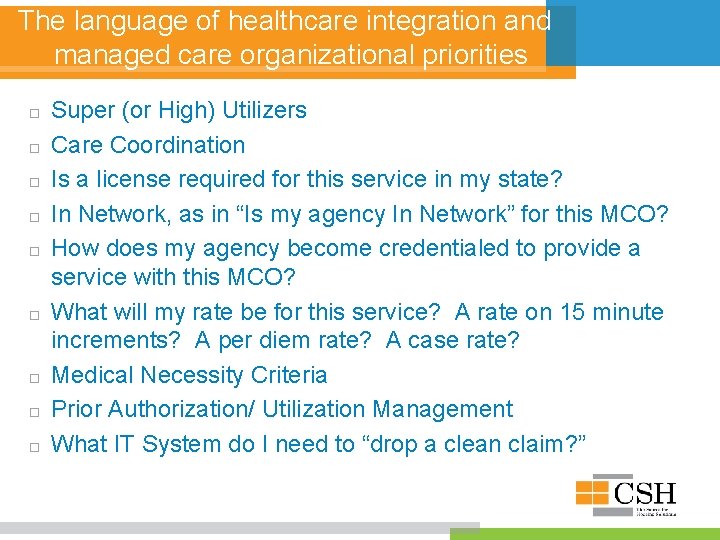
The language of healthcare integration and managed care organizational priorities Super (or High) Utilizers Care Coordination Is a license required for this service in my state? In Network, as in “Is my agency In Network” for this MCO? How does my agency become credentialed to provide a service with this MCO? What will my rate be for this service? A rate on 15 minute increments? A per diem rate? A case rate? Medical Necessity Criteria Prior Authorization/ Utilization Management What IT System do I need to “drop a clean claim? ”
3. Introduction to Washington’s Managed Care System The Source for Housing Solutions
Poll!
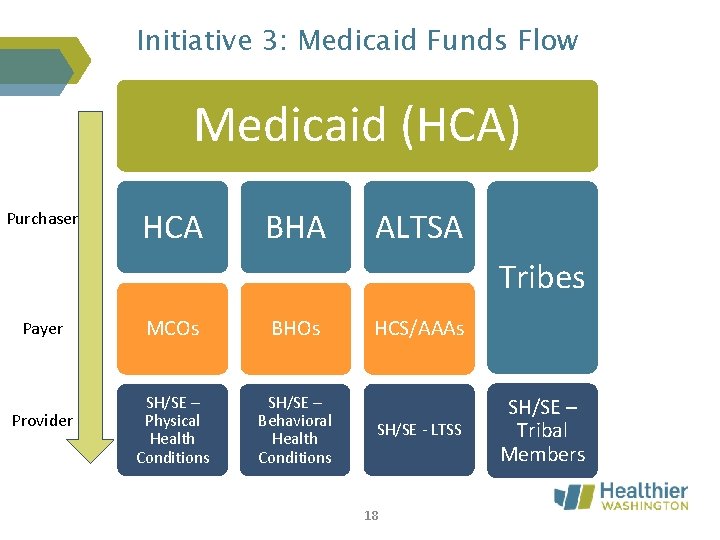
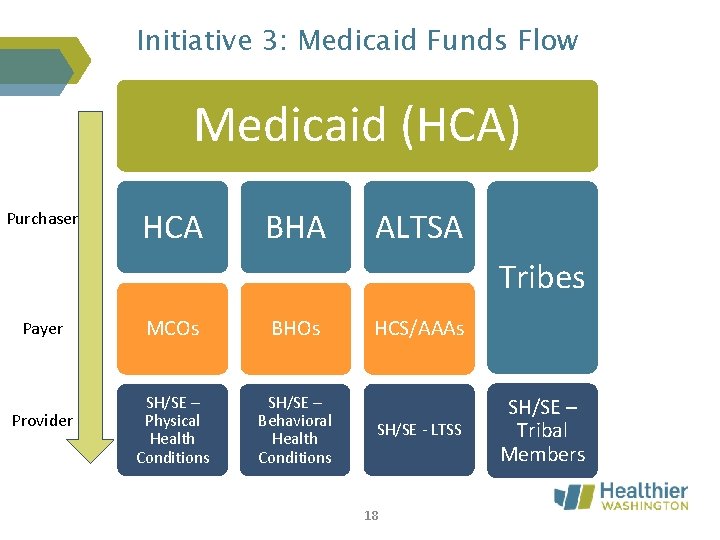
Initiative 3: Medicaid Funds Flow Medicaid (HCA) Purchaser HCA BHA ALTSA Tribes Payer Provider MCOs BHOs SH/SE – Physical Health Conditions SH/SE – Behavioral Health Conditions HCS/AAAs SH/SE - LTSS 18 SH/SE – Tribal Members
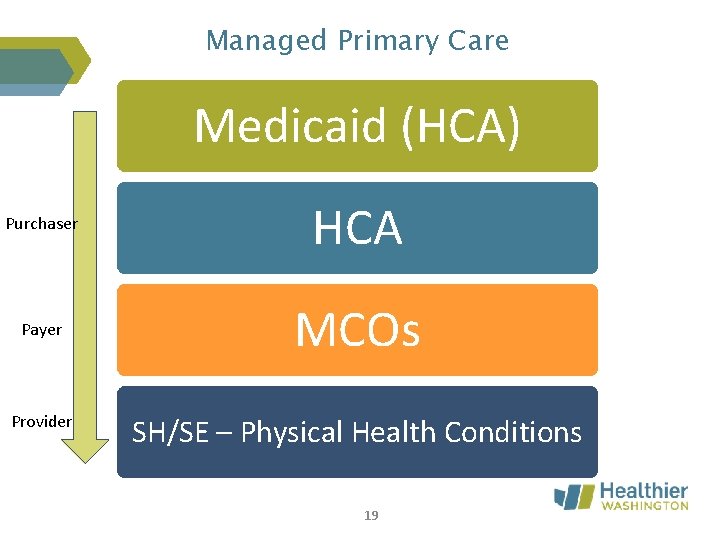
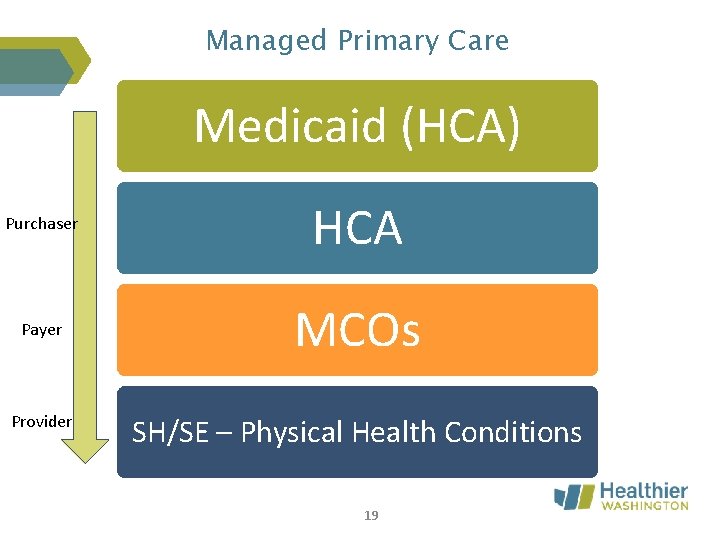
Managed Primary Care Medicaid (HCA) Purchaser HCA Payer MCOs Provider SH/SE – Physical Health Conditions 19
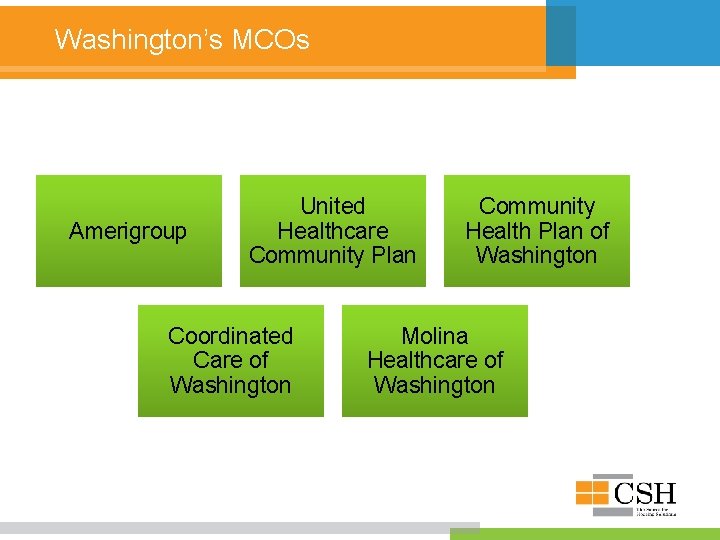
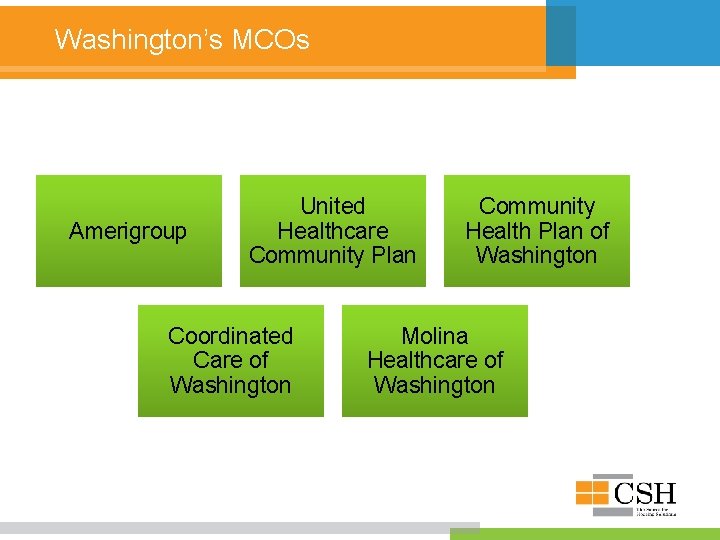
Washington’s MCOs Amerigroup United Healthcare Community Plan Coordinated Care of Washington Community Health Plan of Washington Molina Healthcare of Washington
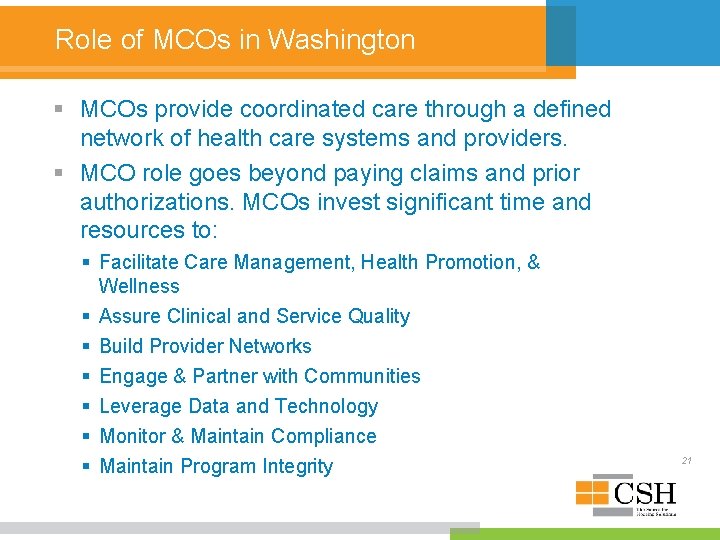
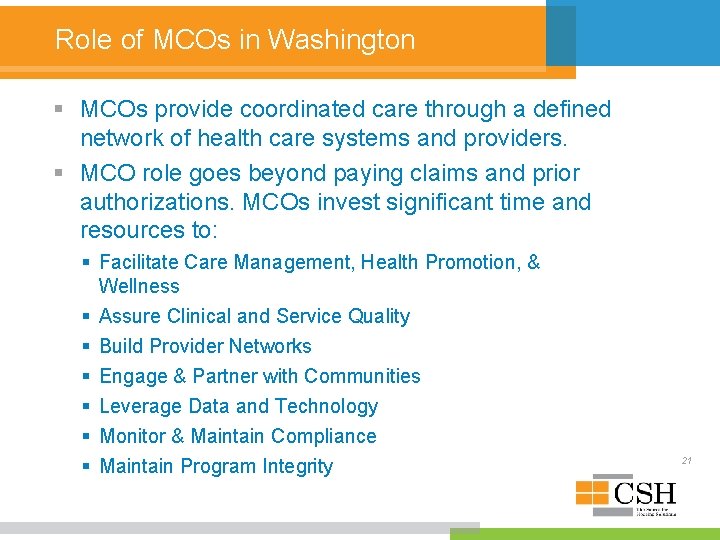
Role of MCOs in Washington § MCOs provide coordinated care through a defined network of health care systems and providers. § MCO role goes beyond paying claims and prior authorizations. MCOs invest significant time and resources to: § Facilitate Care Management, Health Promotion, & Wellness § Assure Clinical and Service Quality § Build Provider Networks § Engage & Partner with Communities § Leverage Data and Technology § Monitor & Maintain Compliance § Maintain Program Integrity 21
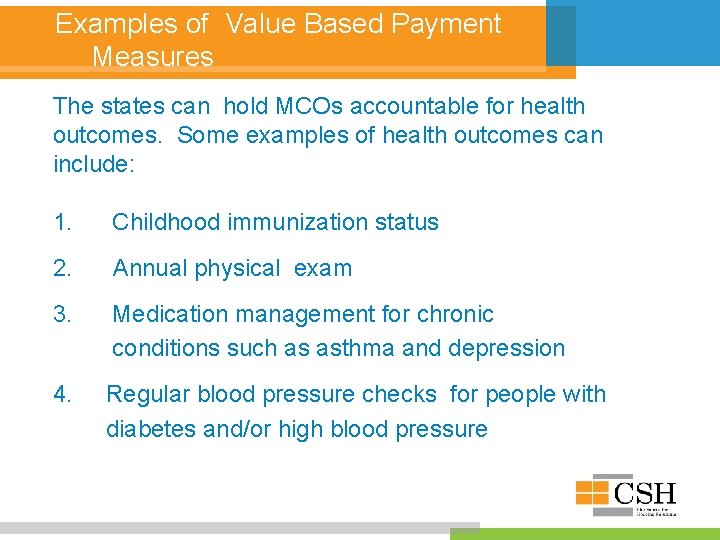
Examples of Value Based Payment Measures The states can hold MCOs accountable for health outcomes. Some examples of health outcomes can include: 1. Childhood immunization status 2. Annual physical exam 3. Medication management for chronic conditions such as asthma and depression 4. Regular blood pressure checks for people with diabetes and/or high blood pressure
Social Determinants Of Health § MCOs bring the capacity to focus on Social Determinants of Health such as Housing Education Employment support § Data analytics for activities such as mapping, identifying gaps in care and hot spotting § Opportunities for partnerships such as with supportive housing providers or healthy food providers, or educational support.
Finance Capacity § MCOs hold the financial risk for covering care within their budgets. § Medicaid rates, paid by the state to the MCOs are required to meet actuarial soundness. These rates are risk-adjusted and set up by the state. § MCOs are profit-limited. The State Medicaid agency sets a maximum profit. If their profit in any year goes over this amount, they are required to return those funds to the state. § Medical/ Loss ratio 24
4. Benefit Implementation: Relationship Building and Contracting The Source for Housing Solutions
Poll!
§ Is your agency already contracted with an MCO? § Relationships Who do you know in common? Do you have a Board member who works for an MCO? You probably should. Who do you know at your state Medicaid Agency? § Are MCOs looking for their high utilizers and can’t find them. HMIS might tell them where they are. § Outcomes MCOs have contracts with the state for certain outcomes.
MCO Provider Networks MCOs are required to have an adequate provider network. In contracts with providers, most MCOs offer a continuum of payment approaches. Networks are routinely monitored by the Health Care Authority to ensure Access & Availability standards are maintained
Most common questions between SH providers and MCOs Providers need to ask MCOS How are rates negotiated? (To an MCO, you are asking about ‘rates’. ) What licenses must my agency have? What staff qualifications are needed? Who can I talk to about IT issues?
Most common questions between SH providers and MCOs need to ask Supportive Housing Providers Can you help us find our high utilizers? Can you help us bring down their health care costs? How can we find affordable and/or supportive housing for our members? Where should we discharge our inpatient or hospitalized members who are experiencing homelessness? How do you identify your prospective tenants”?

Why supportive housing matters to MCOs. Amerigroup’s perspective
More Information & Next Steps § Webinar series § Medicaid Academy for SH service providers (focus on MCO and BHO implementation) § ALTSA provider meetings § Resources on WLIHA’s website