Medicaid Managed Care and Health Insurance Exchanges Medicaid


- Slides: 11
Medicaid Managed Care and Health Insurance Exchanges Medicaid and CHIP Payment and Access Commission January 15, 2013 John Lovelace. President. Government Programs
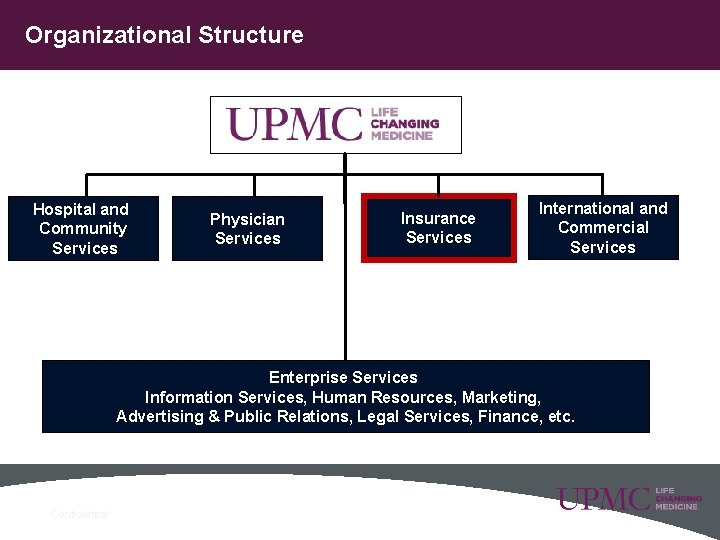
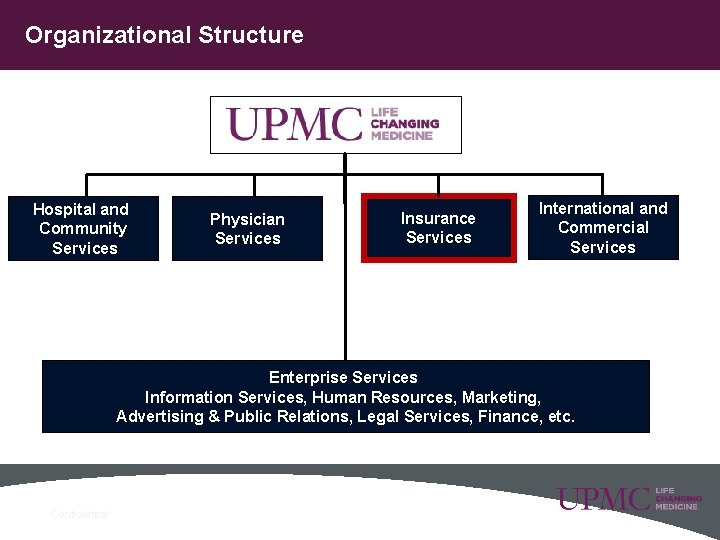
Organizational Structure Hospital and Community Services Physician Services Insurance Services International and Commercial Services Enterprise Services Information Services, Human Resources, Marketing, Advertising & Public Relations, Legal Services, Finance, etc. 2 Confidential

UPMC Insurance Services: A Diverse Product Portfolio • • • • 3 Confidential 2 nd Largest in Nation Provider Led 3 rd Largest Operating in PA 2. 0 M Members Annual Revenues $3. 8 B (run rate) 8, 800+ Employer Groups Fastest Growing Medicaid and CHIP Plan 10 th Largest SNP Nationally Top 10 Nationally in Medicaid Quality 4 Star Medicare Plan (15 th Largest Nationally) Highest Ranked Provider Satisfaction (PA) J. D. Power Certified Call Center National Business Group on Health Platinum Winner 2012 Global Call Center of the Year Awardee (ICMI)

Medicaid Climate in Pennsylvania • Mandatory enrollment in managed care, staged by geographic zone • Dual Eligibles – In FFS for PH – In Managed Care for BH • Disabled non-duals are included in mandatory enrollment • Children’s Health Insurance is administered separately from Medicaid and in a different state department • Behavioral Health Services are carved out and administered separately, primarily through county-based BH systems • No Medicaid expansion at this time • No State-run Exchange at this time 4
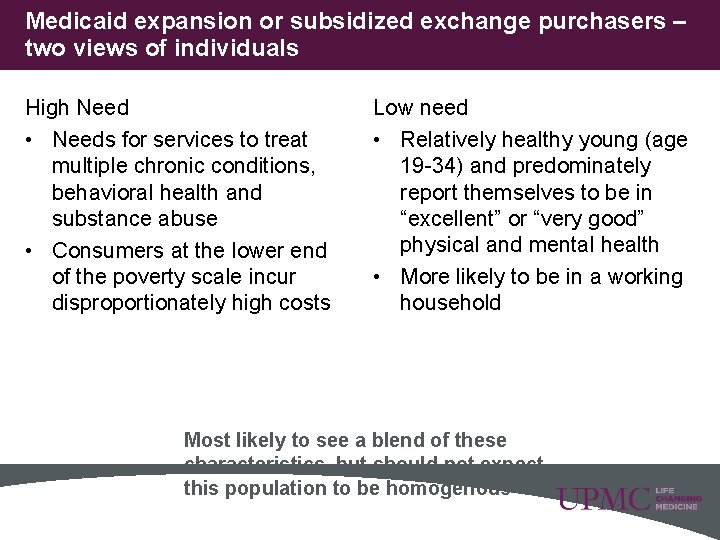
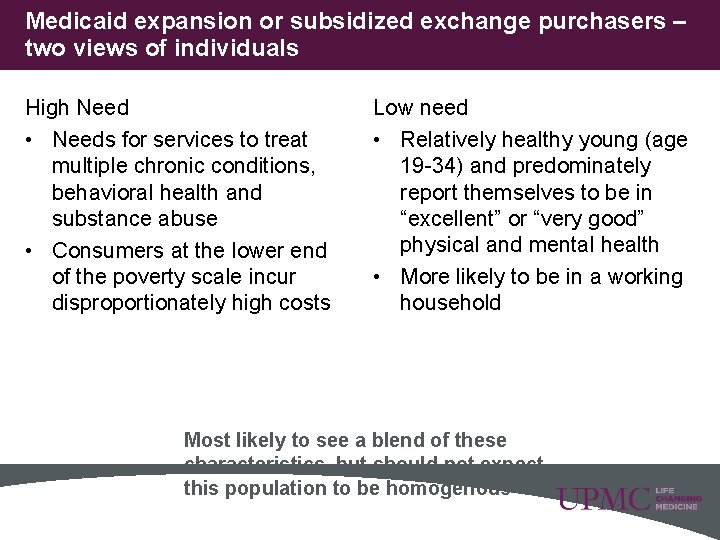
Medicaid expansion or subsidized exchange purchasers – two views of individuals High Need • Needs for services to treat multiple chronic conditions, behavioral health and substance abuse • Consumers at the lower end of the poverty scale incur disproportionately high costs Low need • Relatively healthy young (age 19 -34) and predominately report themselves to be in “excellent” or “very good” physical and mental health • More likely to be in a working household Most likely to see a blend of these characteristics, but should not expect this population to be homogenous 5
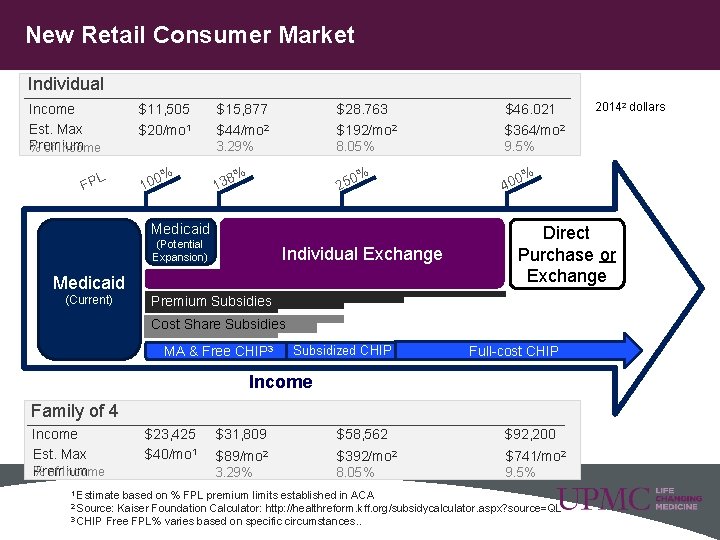
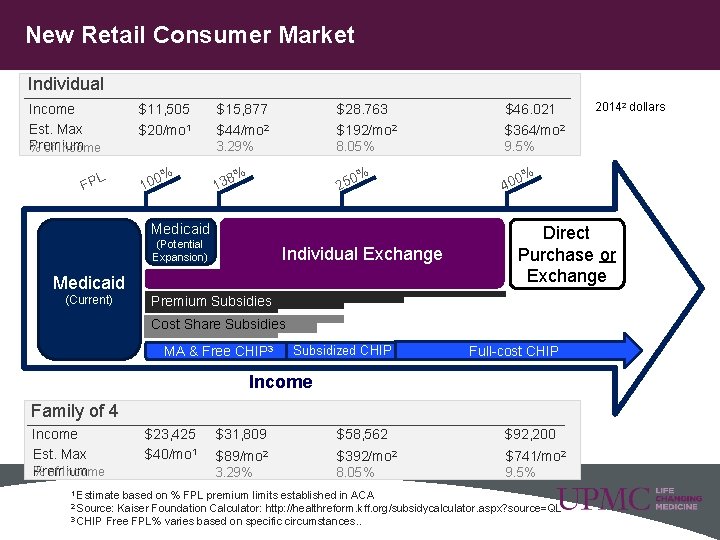
New Retail Consumer Market Individual Income Est. Max Premium % of Income L FP $11, 505 $20/mo 1 % 100 $15, 877 $28. 763 $46. 021 $44/mo 2 $192/mo 2 $364/mo 2 3. 29% 8. 05% 9. 5% % % 250 138 Medicaid (Potential Expansion) Individual Exchange Medicaid (Current) % 400 Direct Purchase or Exchange Premium Subsidies Cost Share Subsidies MA & Free CHIP 3 Subsidized CHIP. Full-cost CHIP Income Family of 4 Income Est. Max % of Income Premium 1 Estimate 6 $23, 425 $40/mo 1 $31, 809 $58, 562 $92, 200 $89/mo 2 $392/mo 2 $741/mo 2 3. 29% 8. 05% 9. 5% based on % FPL premium limits established in ACA Kaiser Foundation Calculator: http: //healthreform. kff. org/subsidycalculator. aspx? source=QL 3 CHIP Free FPL% varies based on specific circumstances. . 2 Source: 20142 dollars
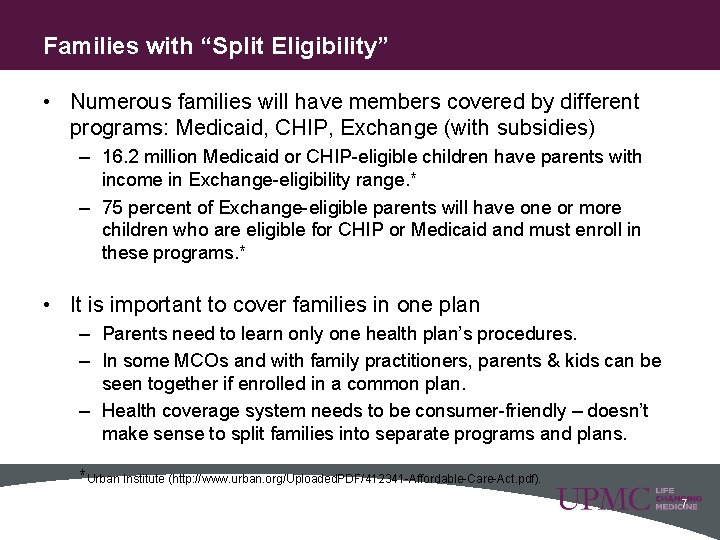
Families with “Split Eligibility” • Numerous families will have members covered by different programs: Medicaid, CHIP, Exchange (with subsidies) – 16. 2 million Medicaid or CHIP-eligible children have parents with income in Exchange-eligibility range. * – 75 percent of Exchange-eligible parents will have one or more children who are eligible for CHIP or Medicaid and must enroll in these programs. * • It is important to cover families in one plan – Parents need to learn only one health plan’s procedures. – In some MCOs and with family practitioners, parents & kids can be seen together if enrolled in a common plan. – Health coverage system needs to be consumer-friendly – doesn’t make sense to split families into separate programs and plans. *Urban Institute (http: //www. urban. org/Uploaded. PDF/412341 -Affordable-Care-Act. pdf). 7
Solutions: Aligning Coverage • Continuous plan enrollment for one year, with payment changes happening “in the background” • Consistency of care as individuals move (at the user’s option) • Network • Authorizations and care management • Benefits • Cost-sharing compatibility • Family coverage • Quality standards • Clinical interventions
Solutions: Product Design • Create product offerings that will retain current membership pull membership from competitors, and attract uninsured • Provide options at premium price points consumers are accustomed to • Provide options at coverage levels consumers are accustomed to – Simple, easy to understand products with no hidden cost shares – Build benefits that consumers can use for everyday, but protect them from high costs • Build Products with a focus on Consumers, not Competitors • We do not, and cannot know what products the competition will offer • Focus on consumer preferences
Specialized (Limited Benefit) Plans • Carve out supports a strong population management focus on individuals with chronic illness burden, such as serious mental illness or intellectual disabilities – This focus could occur in an integrated medical model but often does not due to special needs and stigma • Many of these individuals see the “specialty provider” as their primary points of contact • Carve out facilitates strong engagement with other human services (welfare, criminal justice, children and youth) • Tailored to meet consumer preference and provider expertise 10
Thank you John Lovelace President, Government Programs and Individual Advantage President, UPMC for You, Inc. UPMC Health Plan Pittsburgh, PA lovelacejg@upmc. edu 412 454 5269 11
 Apple health managed care plans
Apple health managed care plans Department of managed health care california
Department of managed health care california Ohio medicaid insurance
Ohio medicaid insurance The role of internet exchanges and peering
The role of internet exchanges and peering Health and social component 3
Health and social component 3 Unit 2 equality diversity and rights
Unit 2 equality diversity and rights Ppo managed care
Ppo managed care Managed care 101
Managed care 101 Managed care continuum
Managed care continuum Xx2021x
Xx2021x Managed care is categorized according to six models
Managed care is categorized according to six models History of managed care
History of managed care