Cultivating Resilience Vicarious Trauma PostTraumatic Growth and SelfCare





- Slides: 75
Cultivating Resilience Vicarious Trauma, Post-Traumatic Growth, and Self-Care Practices Alicia Boccellari, Ph. D. August 1, 2016
Acknowledgements Slides adapted from: • UCSF Trauma Recovery Center (Margaret Lamb, Cecilia Lipp, Ann Tran, Stacey Wiggall and Vanessa Kelly) • Office for Victims of Crime, Office of Justice Programs, U. S. Department of Justice • San Francisco Department of Public Health UCSF University of California, San Francisco
Goals ü Review the impact that violence and trauma have on the people we serve ü Increase your ability to recognize the signs and symptoms of vicarious trauma ü Increase your ability to cope with these signs and symptoms of vicarious trauma ü To enhance your overall professional health and longevity
“The expectation that we can be immersed in suffering and loss daily and not be touched by it is as unrealistic as expecting to be able to walk through water without getting wet. ” (Remen, 2006) (OVC)
WHAT IS TRAUMA? UCSF University of California, San Francisco 5
What is Trauma? Trauma results from an event, series of events, or set of circumstances that is experienced by an individual as physically or emotionally harmful or life threatening and that may have lasting adverse effects on the individual’s functioning and mental, physical, social, emotional, or spiritual well-being. - SAMHSA UCSF University of California, San Francisco 6
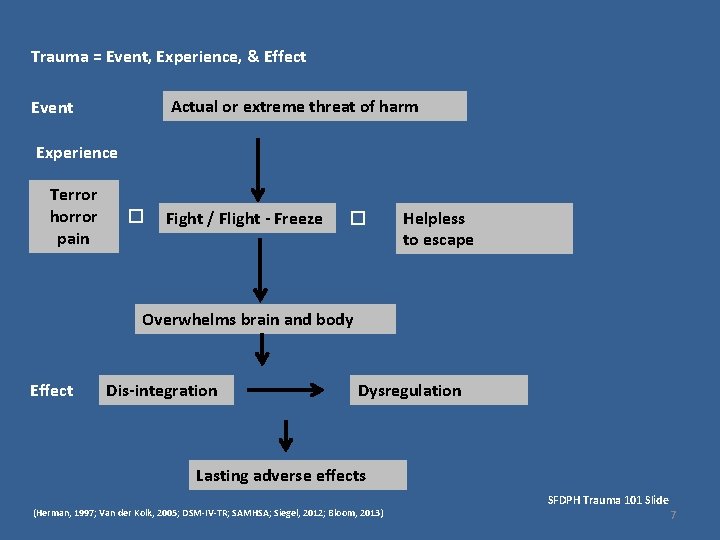
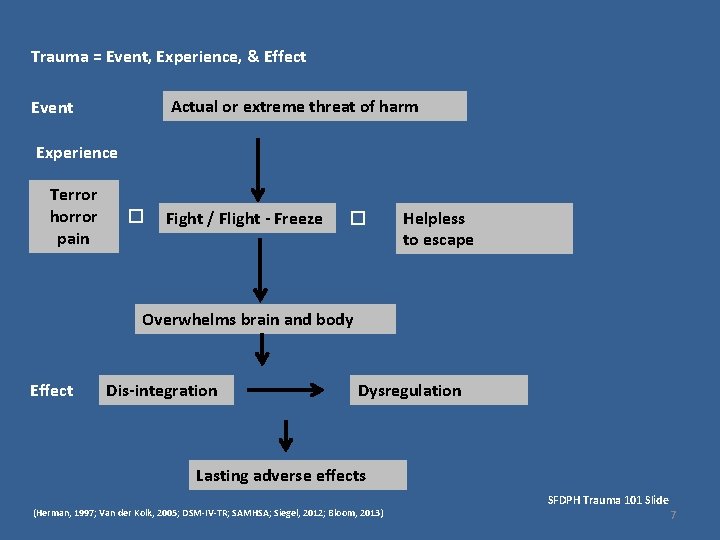
Trauma = Event, Experience, & Effect Actual or extreme threat of harm Event Experience Terror horror pain � Fight / Flight - Freeze � Helpless to escape Overwhelms brain and body Effect Dis-integration Dysregulation Lasting adverse effects (Herman, 1997; Van der Kolk, 2005; DSM-IV-TR; SAMHSA; Siegel, 2012; Bloom, 2013) SFDPH Trauma 101 Slide 7
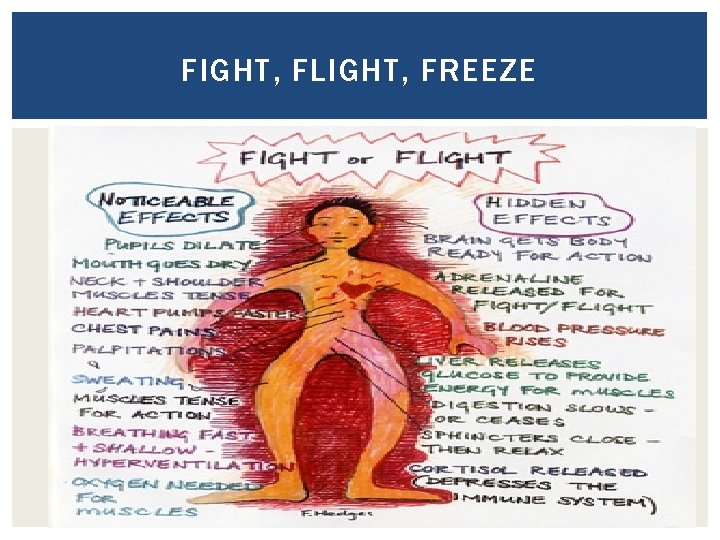
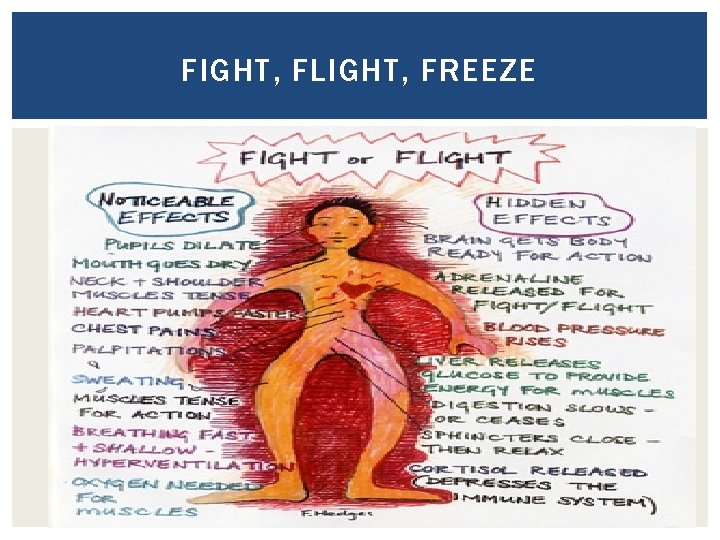
FIGHT, FLIGHT, FREEZE
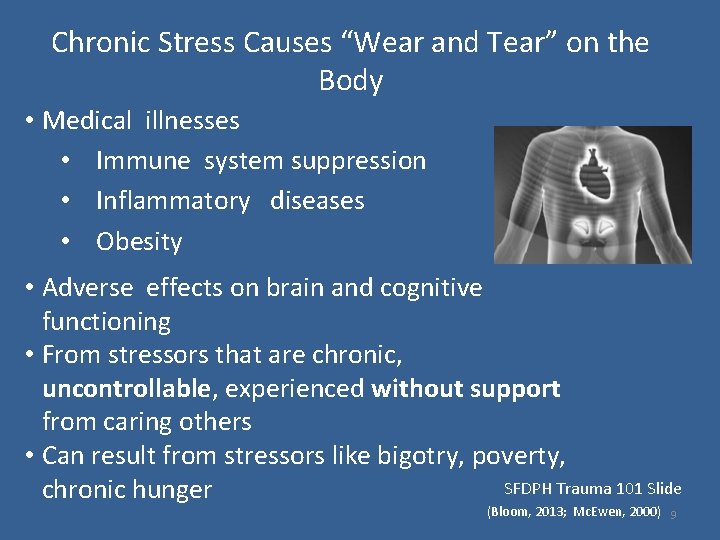
Chronic Stress Causes “Wear and Tear” on the Body • Medical illnesses • Immune system suppression • Inflammatory diseases • Obesity • Adverse effects on brain and cognitive functioning • From stressors that are chronic, uncontrollable, experienced without support from caring others • Can result from stressors like bigotry, poverty, SFDPH Trauma 101 Slide chronic hunger (Bloom, 2013; Mc. Ewen, 2000) 9
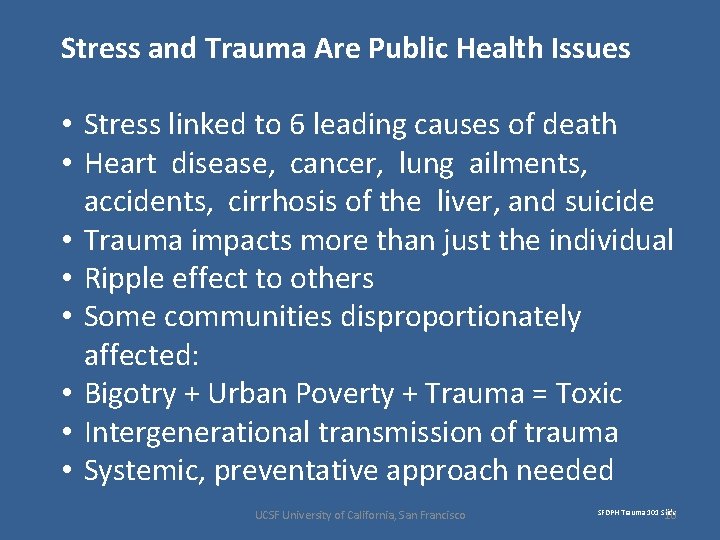
Stress and Trauma Are Public Health Issues • Stress linked to 6 leading causes of death • Heart disease, cancer, lung ailments, accidents, cirrhosis of the liver, and suicide • Trauma impacts more than just the individual • Ripple effect to others • Some communities disproportionately affected: • Bigotry + Urban Poverty + Trauma = Toxic • Intergenerational transmission of trauma • Systemic, preventative approach needed UCSF University of California, San Francisco SFDPH Trauma 101 Slide 10
How does trauma effect the individual? Trauma shapes the survivor’s basic beliefs about themselves, others, their world view, spirituality. q Who am I? q The world is no longer safe q Others can’t be trusted q I have to protect myself no matter what q I can’t believe in anything now.
Basic capacities damaged by trauma: continued • Trust: – Inability to trust – Too trusting (can contribute to revictimization)
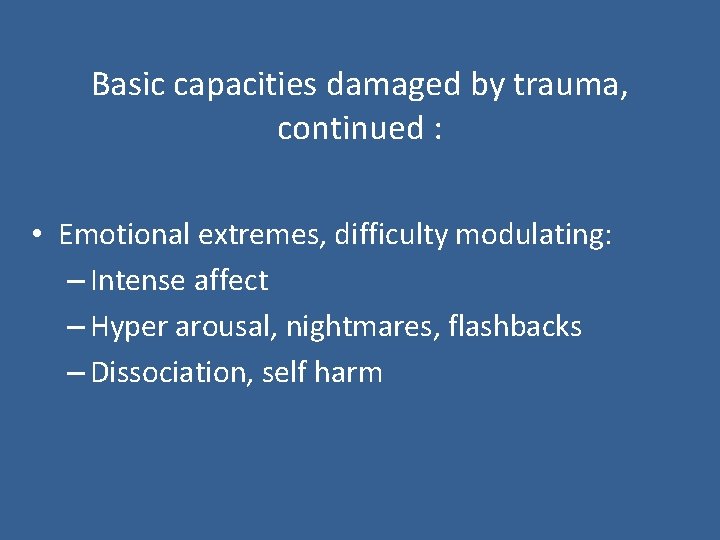
Basic capacities damaged by trauma, continued : • Emotional extremes, difficulty modulating: – Intense affect – Hyper arousal, nightmares, flashbacks – Dissociation, self harm
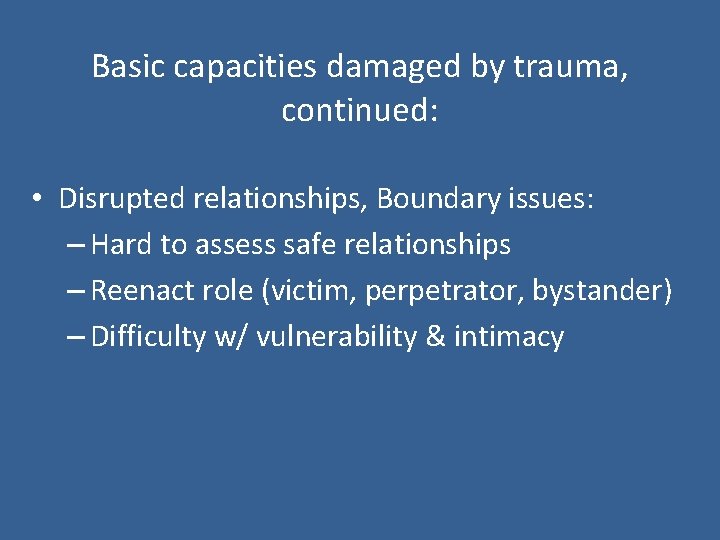
Basic capacities damaged by trauma, continued: • Disrupted relationships, Boundary issues: – Hard to assess safe relationships – Reenact role (victim, perpetrator, bystander) – Difficulty w/ vulnerability & intimacy
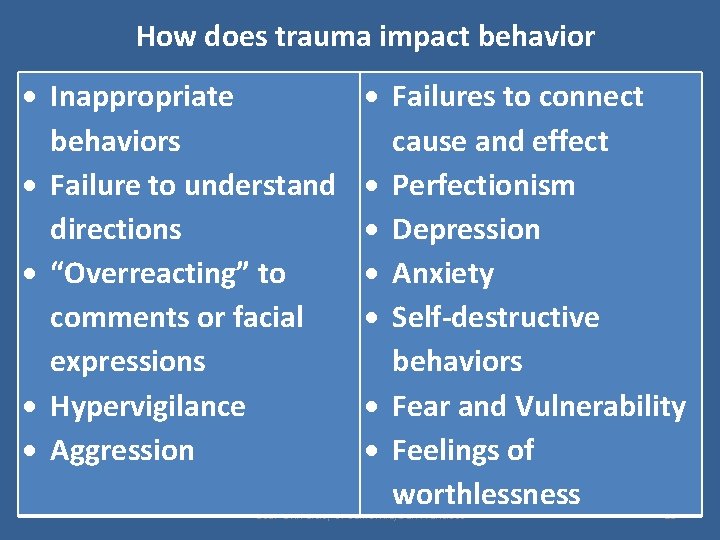
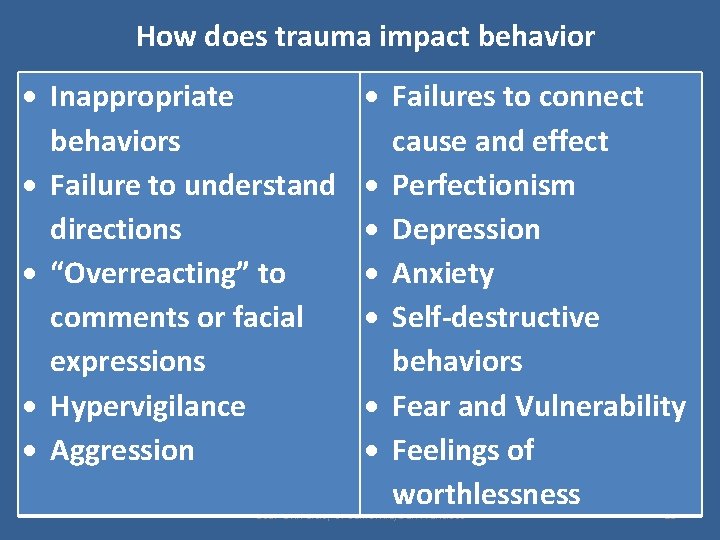
How does trauma impact behavior Inappropriate behaviors Failure to understand directions “Overreacting” to comments or facial expressions Hypervigilance Aggression Failures to connect cause and effect Perfectionism Depression Anxiety Self-destructive behaviors Fear and Vulnerability Feelings of worthlessness UCSF University of California, San Francisco 15
Compassion Have compassion for everyone you meet even if they don’t want it. What seems conceit, bad manners, or cynicism is always a sign of things no ears have heard, no eyes have seen. You do not know what wars are going on down there where the spirit meets the bone. Miller Williams UCSF University of California, San Francisco 16
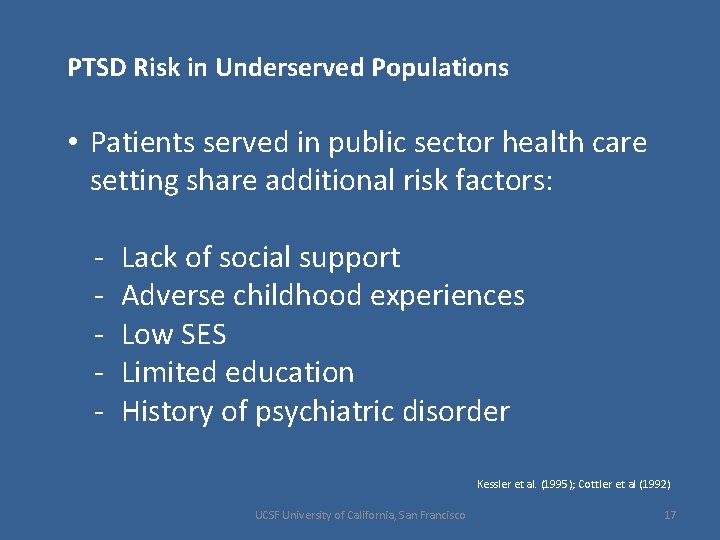
PTSD Risk in Underserved Populations • Patients served in public sector health care setting share additional risk factors: - Lack of social support Adverse childhood experiences Low SES Limited education History of psychiatric disorder Kessler et al. (1995); Cottler et al (1992) UCSF University of California, San Francisco 17
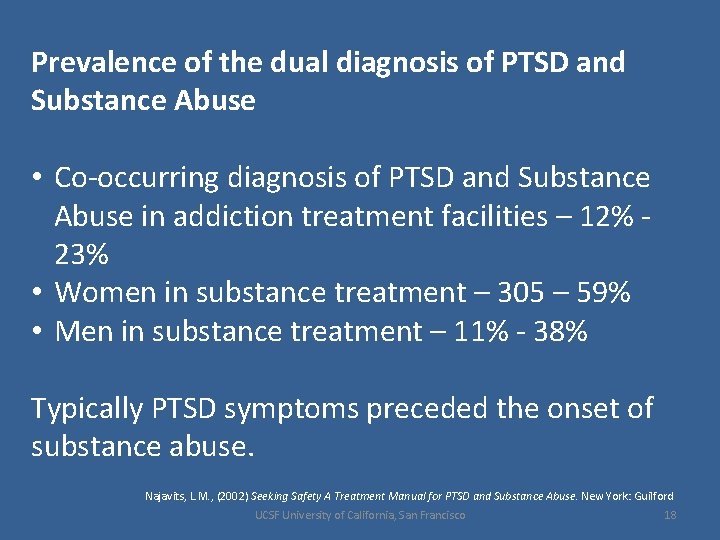
Prevalence of the dual diagnosis of PTSD and Substance Abuse • Co-occurring diagnosis of PTSD and Substance Abuse in addiction treatment facilities – 12% 23% • Women in substance treatment – 305 – 59% • Men in substance treatment – 11% - 38% Typically PTSD symptoms preceded the onset of substance abuse. Najavits, L. M. , (2002) Seeking Safety A Treatment Manual for PTSD and Substance Abuse. New York: Guilford UCSF University of California, San Francisco 18
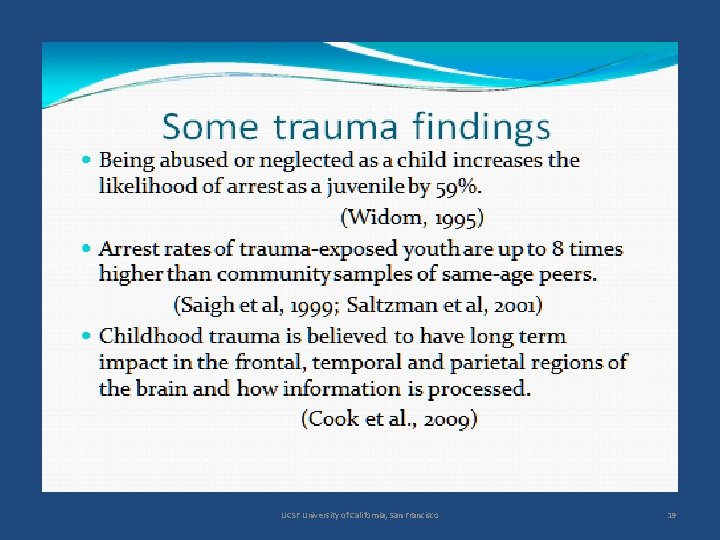
UCSF University of California, San Francisco 19
Taking a Closer Look. . . • Traumatic stress • Vicarious traumatization OVC
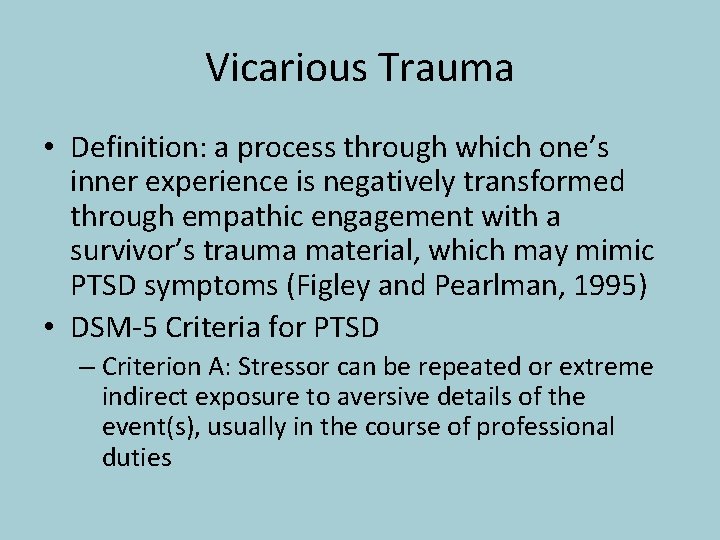
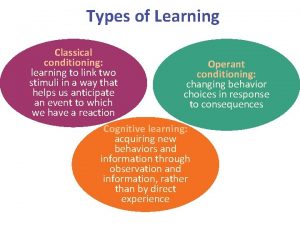
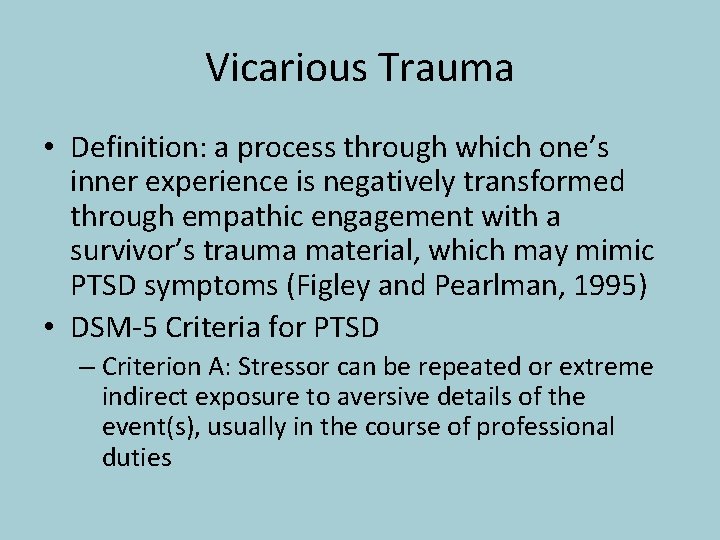
Vicarious Trauma • Definition: a process through which one’s inner experience is negatively transformed through empathic engagement with a survivor’s trauma material, which may mimic PTSD symptoms (Figley and Pearlman, 1995) • DSM-5 Criteria for PTSD – Criterion A: Stressor can be repeated or extreme indirect exposure to aversive details of the event(s), usually in the course of professional duties
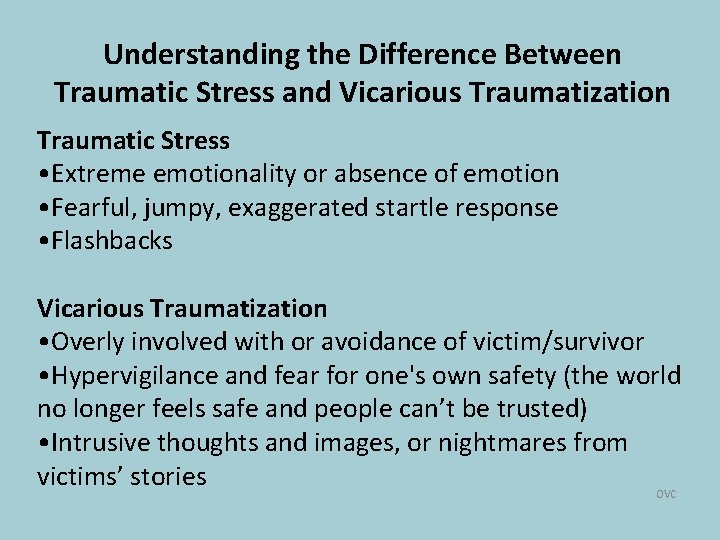
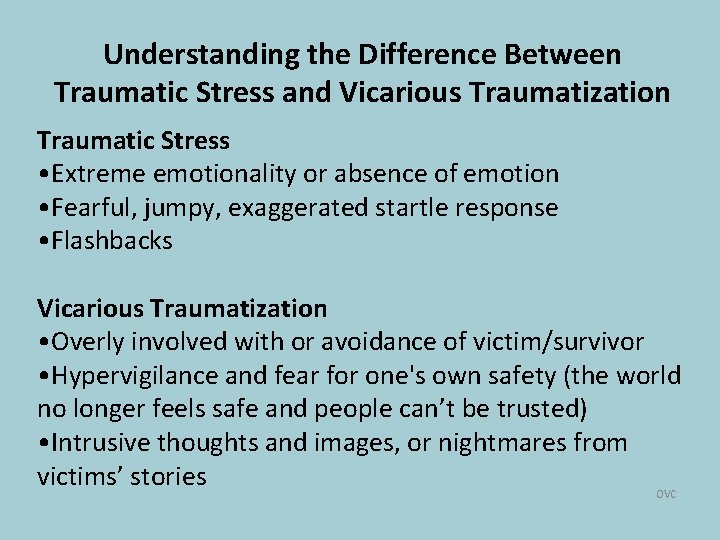
Understanding the Difference Between Traumatic Stress and Vicarious Traumatization Traumatic Stress • Extreme emotionality or absence of emotion • Fearful, jumpy, exaggerated startle response • Flashbacks Vicarious Traumatization • Overly involved with or avoidance of victim/survivor • Hypervigilance and fear for one's own safety (the world no longer feels safe and people can’t be trusted) • Intrusive thoughts and images, or nightmares from victims’ stories OVC
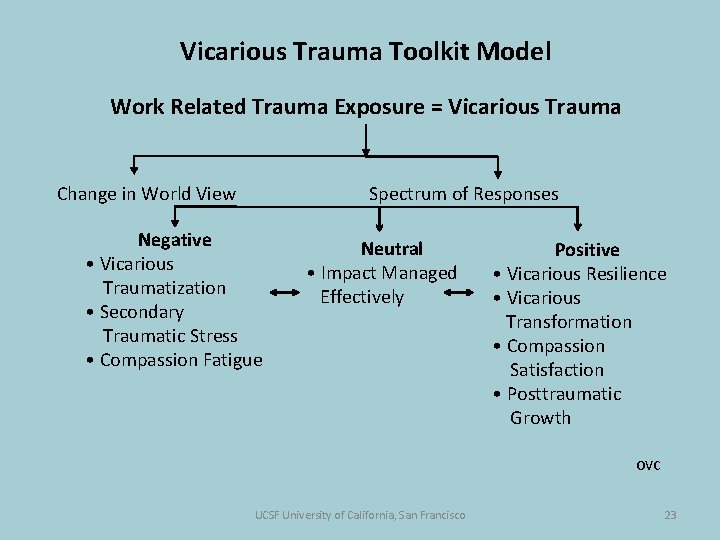
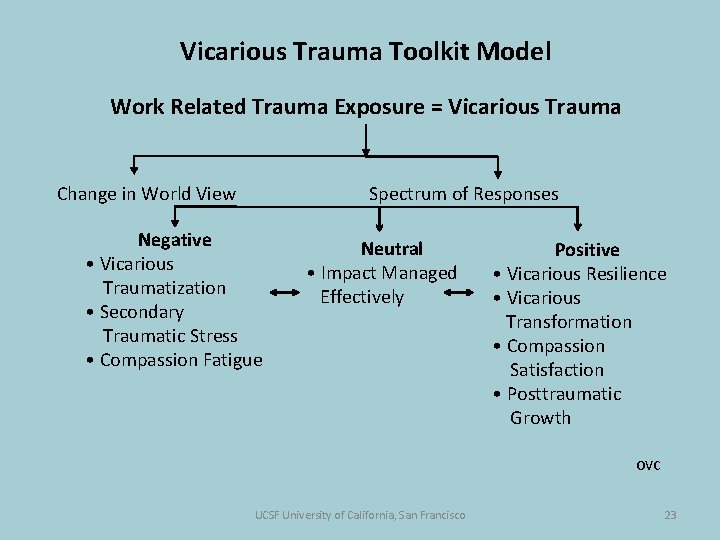
Vicarious Trauma Toolkit Model Work Related Trauma Exposure = Vicarious Trauma Change in World View Spectrum of Responses Negative • Vicarious Traumatization • Secondary Traumatic Stress • Compassion Fatigue Neutral • Impact Managed Effectively Positive • Vicarious Resilience • Vicarious Transformation • Compassion Satisfaction • Posttraumatic Growth OVC UCSF University of California, San Francisco 23
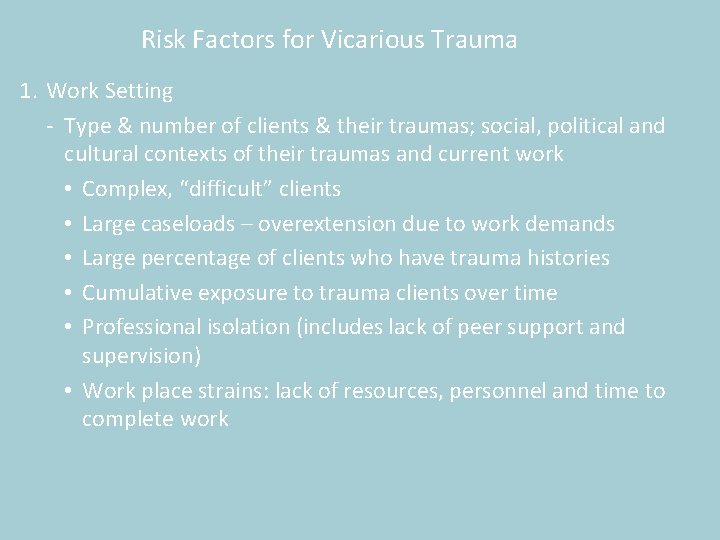
Risk Factors for Vicarious Trauma 1. Work Setting - Type & number of clients & their traumas; social, political and cultural contexts of their traumas and current work • Complex, “difficult” clients • Large caseloads – overextension due to work demands • Large percentage of clients who have trauma histories • Cumulative exposure to trauma clients over time • Professional isolation (includes lack of peer support and supervision) • Work place strains: lack of resources, personnel and time to complete work
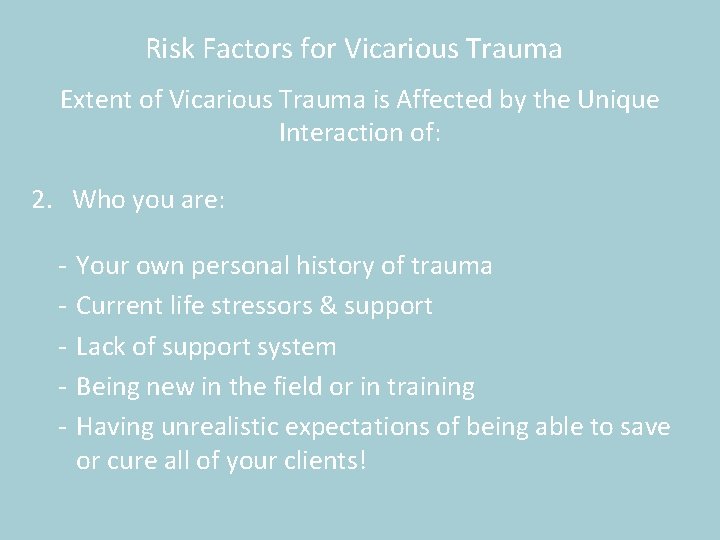
Risk Factors for Vicarious Trauma Extent of Vicarious Trauma is Affected by the Unique Interaction of: 2. Who you are: - Your own personal history of trauma Current life stressors & support Lack of support system Being new in the field or in training Having unrealistic expectations of being able to save or cure all of your clients!
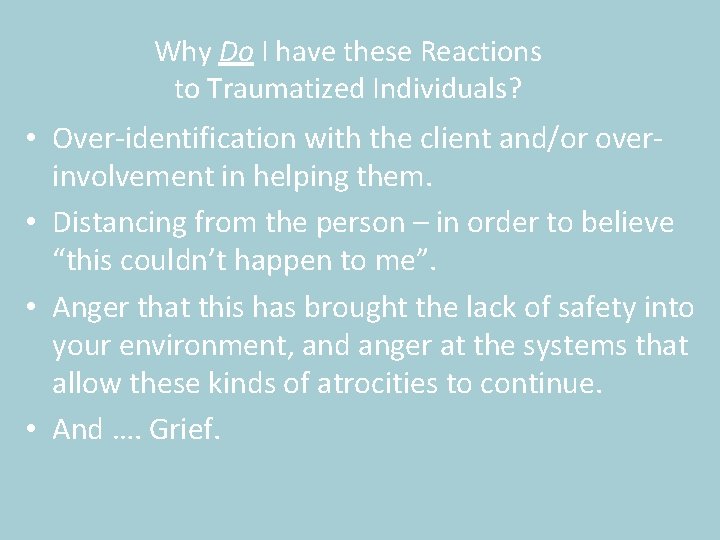
Why Do I have these Reactions to Traumatized Individuals? • Over-identification with the client and/or overinvolvement in helping them. • Distancing from the person – in order to believe “this couldn’t happen to me”. • Anger that this has brought the lack of safety into your environment, and anger at the systems that allow these kinds of atrocities to continue. • And …. Grief.
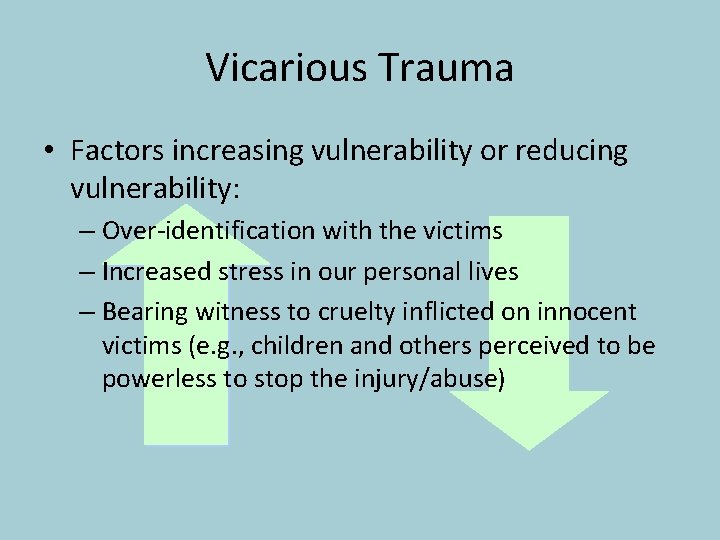
Vicarious Trauma • Factors increasing vulnerability or reducing vulnerability: – Over-identification with the victims – Increased stress in our personal lives – Bearing witness to cruelty inflicted on innocent victims (e. g. , children and others perceived to be powerless to stop the injury/abuse)
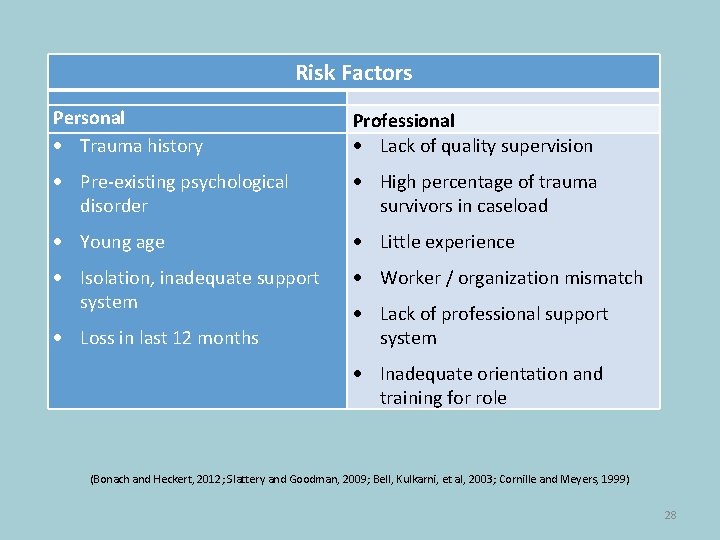
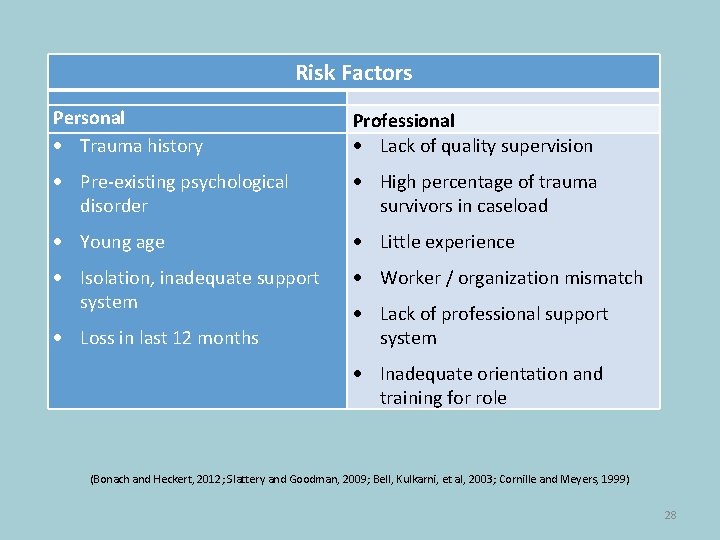
Risk Factors Personal Trauma history Professional Lack of quality supervision Pre-existing psychological disorder High percentage of trauma survivors in caseload Young age Little experience Isolation, inadequate support system Worker / organization mismatch Loss in last 12 months Lack of professional support system Inadequate orientation and training for role (Bonach and Heckert, 2012; Slattery and Goodman, 2009; Bell, Kulkarni, et al, 2003; Cornille and Meyers, 1999) 28
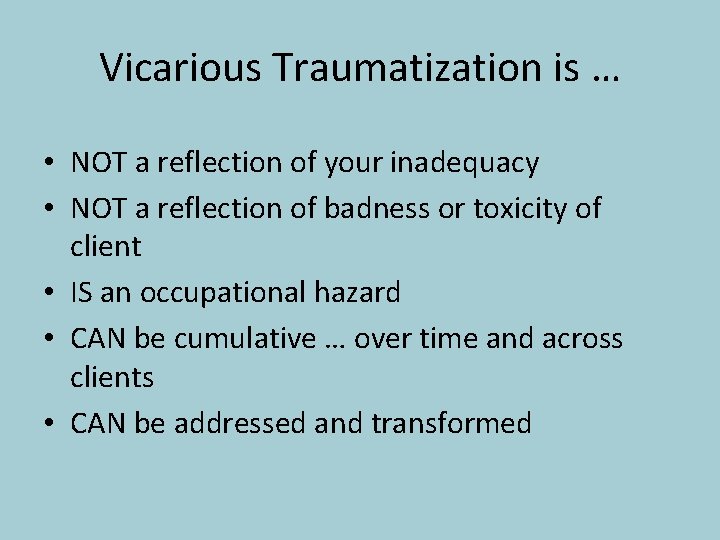
Vicarious Traumatization is … • NOT a reflection of your inadequacy • NOT a reflection of badness or toxicity of client • IS an occupational hazard • CAN be cumulative … over time and across clients • CAN be addressed and transformed
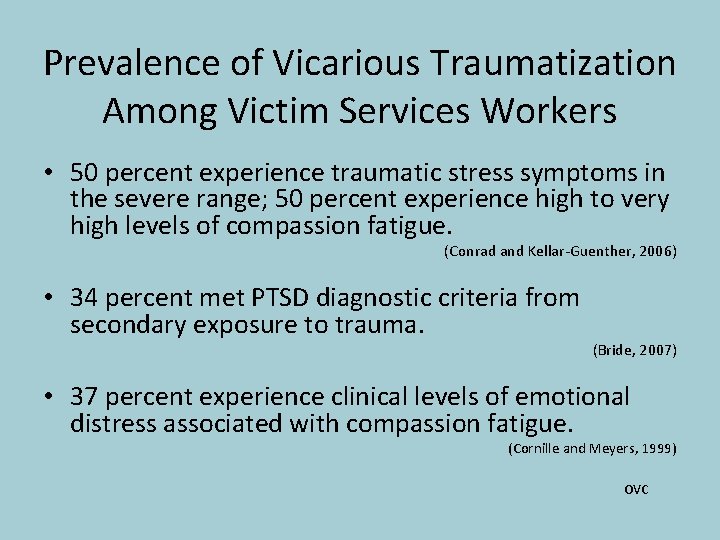
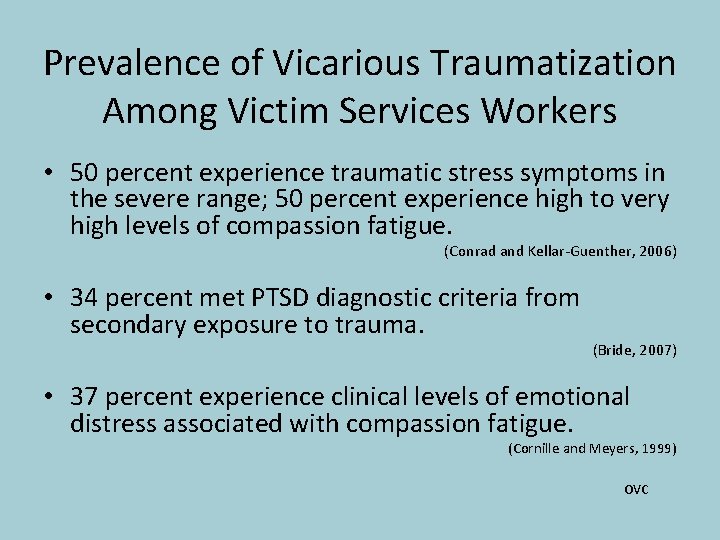
Prevalence of Vicarious Traumatization Among Victim Services Workers • 50 percent experience traumatic stress symptoms in the severe range; 50 percent experience high to very high levels of compassion fatigue. (Conrad and Kellar-Guenther, 2006) • 34 percent met PTSD diagnostic criteria from secondary exposure to trauma. (Bride, 2007) • 37 percent experience clinical levels of emotional distress associated with compassion fatigue. (Cornille and Meyers, 1999) OVC
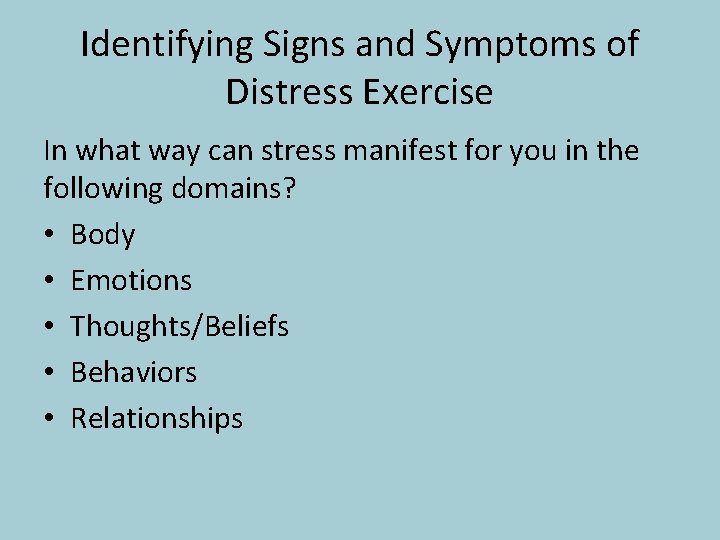
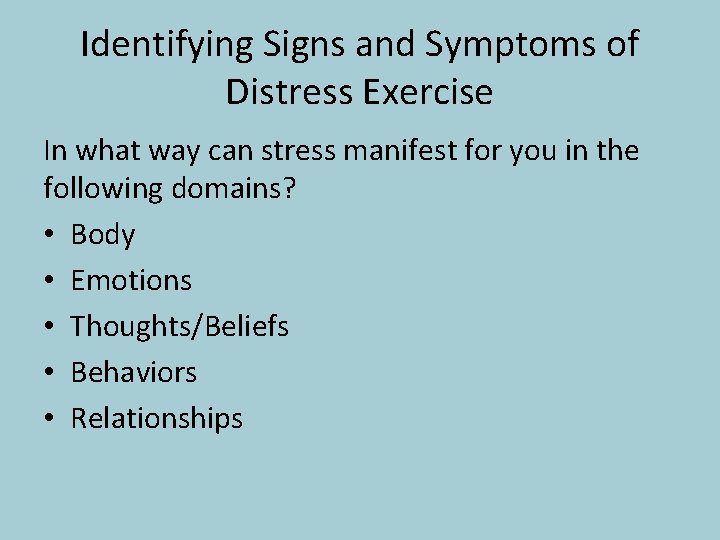
Identifying Signs and Symptoms of Distress Exercise In what way can stress manifest for you in the following domains? • Body • Emotions • Thoughts/Beliefs • Behaviors • Relationships
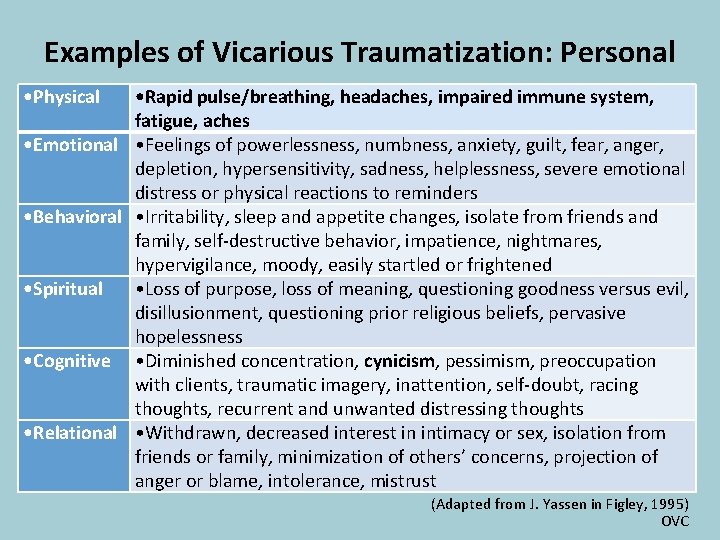
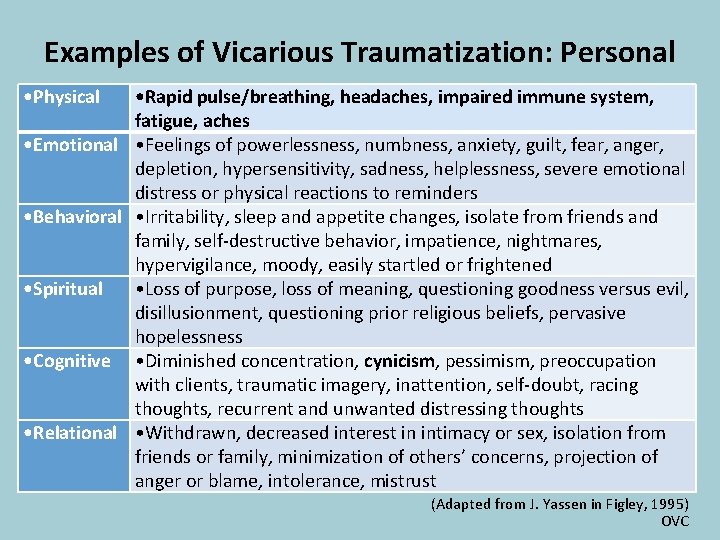
Examples of Vicarious Traumatization: Personal • Physical • Rapid pulse/breathing, headaches, impaired immune system, fatigue, aches • Emotional • Feelings of powerlessness, numbness, anxiety, guilt, fear, anger, depletion, hypersensitivity, sadness, helplessness, severe emotional distress or physical reactions to reminders • Behavioral • Irritability, sleep and appetite changes, isolate from friends and family, self-destructive behavior, impatience, nightmares, hypervigilance, moody, easily startled or frightened • Spiritual • Loss of purpose, loss of meaning, questioning goodness versus evil, disillusionment, questioning prior religious beliefs, pervasive hopelessness • Cognitive • Diminished concentration, cynicism, pessimism, preoccupation with clients, traumatic imagery, inattention, self-doubt, racing thoughts, recurrent and unwanted distressing thoughts • Relational • Withdrawn, decreased interest in intimacy or sex, isolation from friends or family, minimization of others’ concerns, projection of anger or blame, intolerance, mistrust (Adapted from J. Yassen in Figley, 1995) OVC
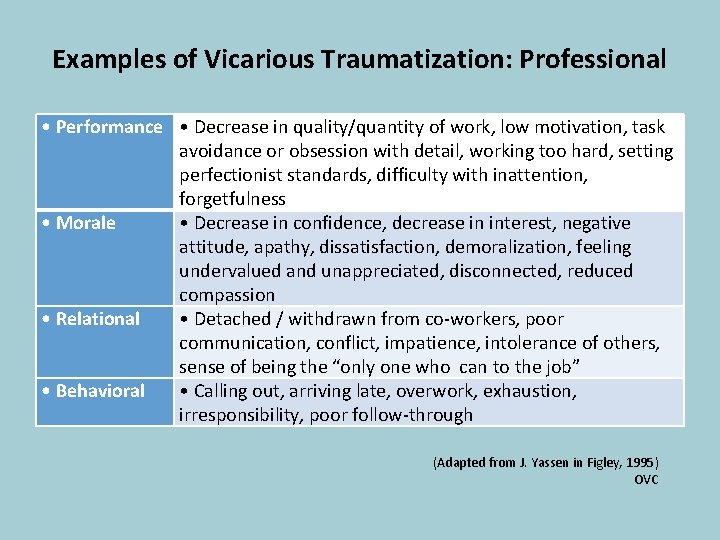
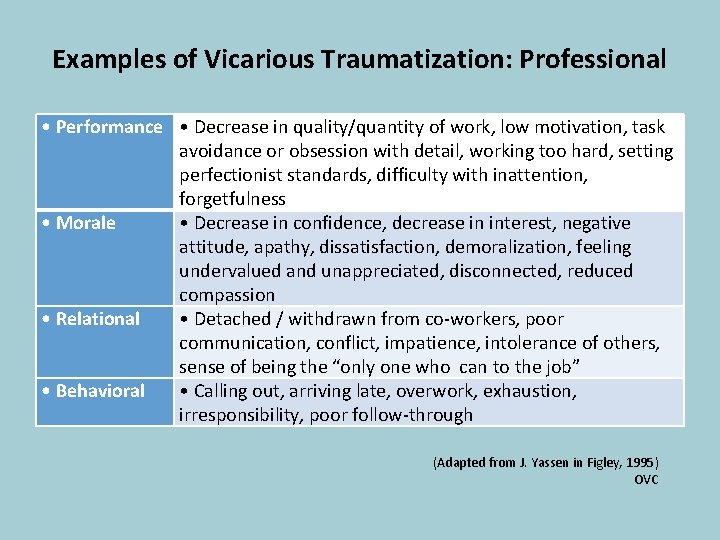
Examples of Vicarious Traumatization: Professional • Performance • Decrease in quality/quantity of work, low motivation, task avoidance or obsession with detail, working too hard, setting perfectionist standards, difficulty with inattention, forgetfulness • Morale • Decrease in confidence, decrease in interest, negative attitude, apathy, dissatisfaction, demoralization, feeling undervalued and unappreciated, disconnected, reduced compassion • Relational • Detached / withdrawn from co-workers, poor communication, conflict, impatience, intolerance of others, sense of being the “only one who can to the job” • Behavioral • Calling out, arriving late, overwork, exhaustion, irresponsibility, poor follow-through (Adapted from J. Yassen in Figley, 1995) OVC

Vignette and Brief Discussion
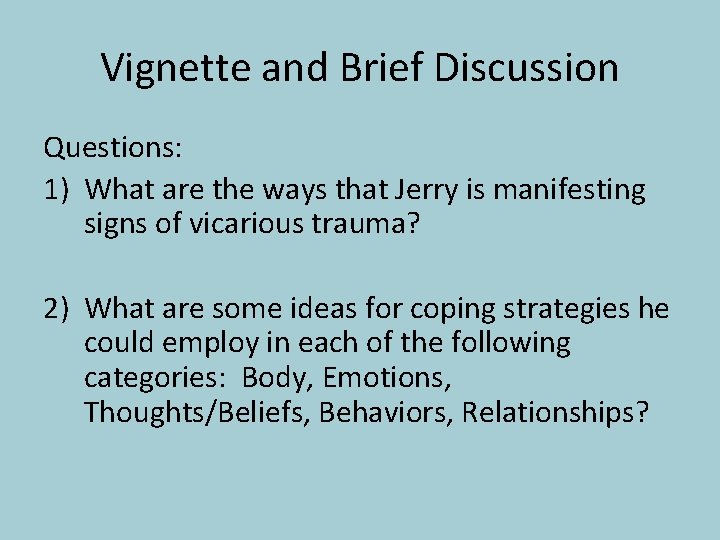
Vignette and Brief Discussion Questions: 1) What are the ways that Jerry is manifesting signs of vicarious trauma? 2) What are some ideas for coping strategies he could employ in each of the following categories: Body, Emotions, Thoughts/Beliefs, Behaviors, Relationships?
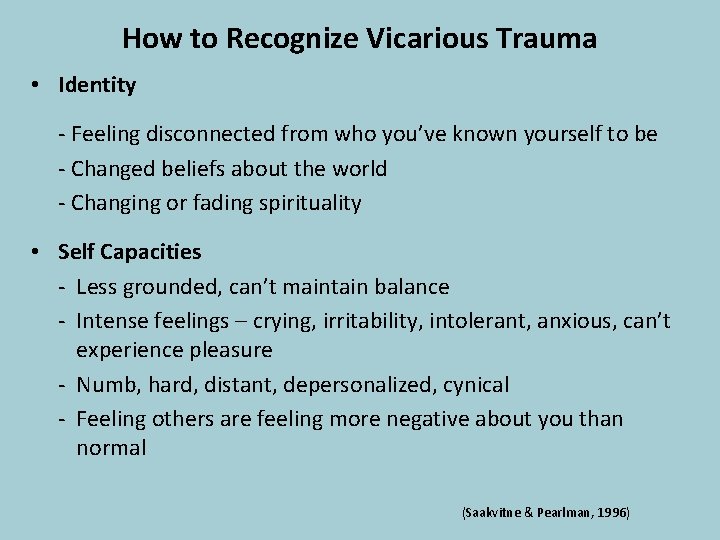
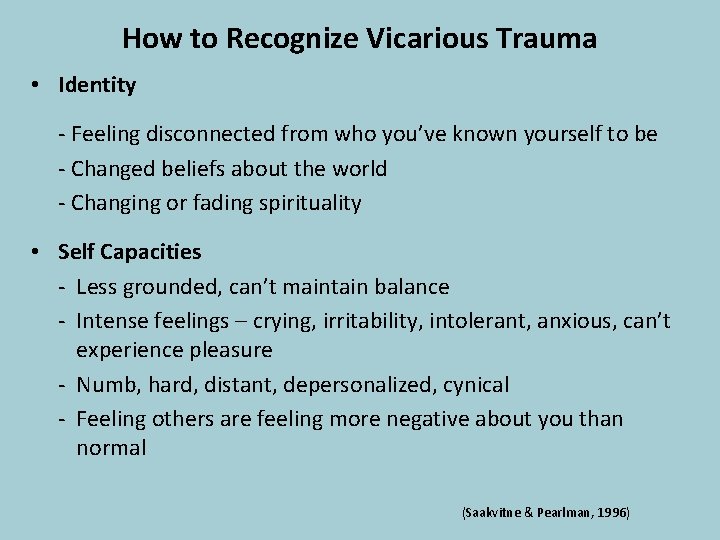
How to Recognize Vicarious Trauma • Identity - Feeling disconnected from who you’ve known yourself to be - Changed beliefs about the world - Changing or fading spirituality • Self Capacities - Less grounded, can’t maintain balance - Intense feelings – crying, irritability, intolerant, anxious, can’t experience pleasure - Numb, hard, distant, depersonalized, cynical - Feeling others are feeling more negative about you than normal (Saakvitne & Pearlman, 1996)
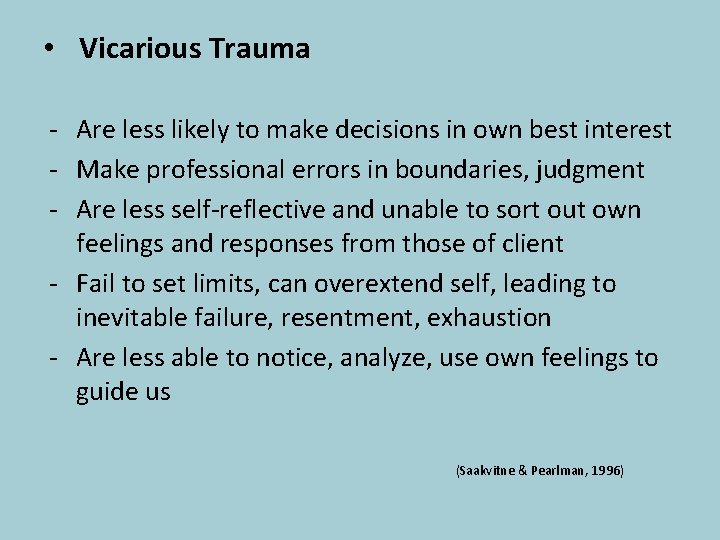
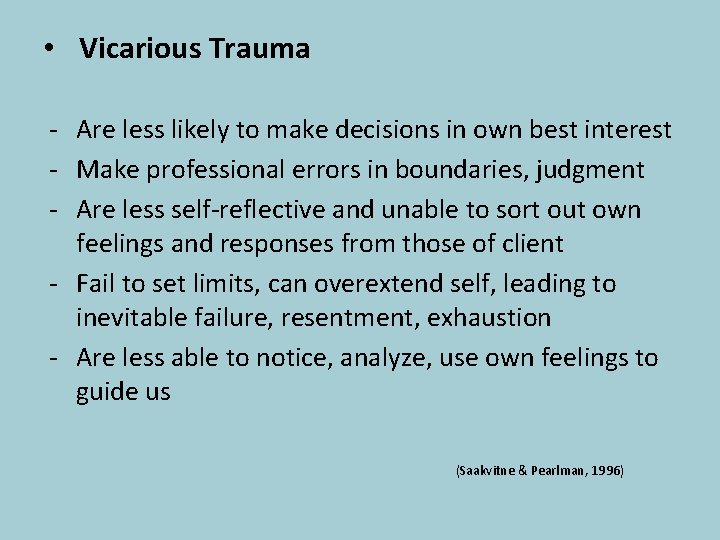
• Vicarious Trauma - Are less likely to make decisions in own best interest - Make professional errors in boundaries, judgment - Are less self-reflective and unable to sort out own feelings and responses from those of client - Fail to set limits, can overextend self, leading to inevitable failure, resentment, exhaustion - Are less able to notice, analyze, use own feelings to guide us (Saakvitne & Pearlman, 1996)
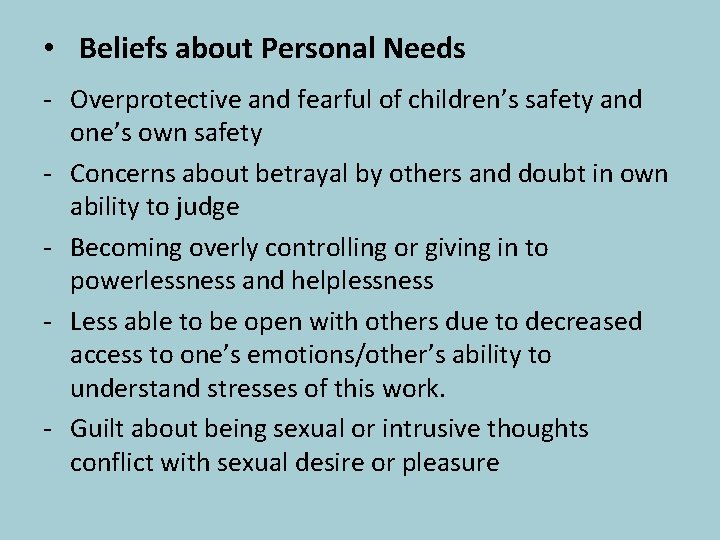
• Beliefs about Personal Needs - Overprotective and fearful of children’s safety and one’s own safety - Concerns about betrayal by others and doubt in own ability to judge - Becoming overly controlling or giving in to powerlessness and helplessness - Less able to be open with others due to decreased access to one’s emotions/other’s ability to understand stresses of this work. - Guilt about being sexual or intrusive thoughts conflict with sexual desire or pleasure
• Memory and Perception - Having intrusive thoughts, images, feelings, somatic experiences - Avoidance of above and their triggers
Interpersonal Responses in VT: Views of self or other can narrow to role of victim, rescuer, perpetrator, uncaring bystander • Feeling others at work or home are intentionally hurtful, malicious, uncaring, or alternatively, weak & less capable • Feeling hurt or disrespected by others • Taking things personally • Feeling weak and less capable • Tending to view others as either a good person or a bad person, forgetting we are all a mixture of both • Observing that you tend to react more strongly with anger, irritability, hurt, or anxiety to things people do • Blaming our clients for being victimized
• Beliefs about Personal Needs - Overprotective and fearful of children’s safety and one’s own safety - Concerns about betrayal by others and doubt in own ability to judge - Becoming overly controlling or giving in to powerlessness and helplessness - Less able to be open with others due to decreased access to one’s emotions/other’s ability to understand stresses of this work. - Guilt about being sexual or intrusive thoughts conflict with sexual desire or pleasure
What is Self-Care? Self-care is what people do for themselves to establish and maintain health, and to prevent and deal with illness. ‘It is a broad concept encompassing hygiene (general and personal), nutrition (type and quality of food eaten), lifestyle (sporting activities, leisure, etc. ), environmental factors (living conditions, social habits, etc. ) socio-economic factors (income level, cultural beliefs, etc. ), and self-medication. ’ (World Health Organization, 1998) (OVC)
Why is Self-Care Important? “To keep the lamp burning we have to keep putting oil in it” - Mother Teresa
Self-Assessment Things I Love to Do How I Spend My Time • How closely does the way I spend my time correspond with the activities I enjoy doing? • If they don’t match exactly, what changes do I need to make so that the correspondence between the two columns is greater? • Which changes can I make right away, and which may require more time and planning? • What steps to I need to take to make these changes?
Domains of Personal Self-Care • • • The Physical self The Nutritious self The Emotional Self The Humorous self The Playful self The Recreational self The Relaxation/stress reduction self The Solitary self The Spiritual self
Nurturing the Physical Self • Get adequate rest and sleep • Physical activity on a regular basis • Fun physical activities • Medical care/preventive health practices • Massage/bodywork/physical therapy • Take time off when you are sick! • Take time to be sexual with self/partner
Nurturing the Nutritious Self • Eat regular, healthy snacks and meals • Never skip breakfast • Your body and brain need water – at least 8 8 oz glasses a day (caffeine doesn’t count) • Be flexible and allow small indulgences for long-term success
Nurturing the Emotional Self • Doing what is comforting to you • Finding things that make you laugh • Praising and loving yourself – giving self affirmations • Allowing yourself to cry • Expressing your outrage in social action, letters • Obtaining your own psychotherapy, support groups, personal growth
Nurturing the Humorous Self • Laughing in a serious environment was the number one strategy listed in one study of clinicians’ coping strategies • It takes time to master the art of laughter at work – look for opportunities
Nurturing the Relaxation Stress-Reduction Self • Stress leads to nervous system over-arousal • Progressive muscle relaxation, breathing • Visualization and imagery • Meditative practices • Yoga • Nature • Massage
Nurturing the Solitary Self • Caring professionals live a life of intense interaction with people who need something • There is a quality to being alone that is incredibly precious once we can move beyond the resistance we sometimes have • Take time away from telephones, the computer too!
Nurturing the Spiritual Self • Identify what is meaningful to you and notice its place in your life • Listen to inspirational music • Include spiritual practices and rituals • Find a spiritual community • Beliefs help to understand painful human realities • Spend time in nature, retreat centers
Nurturing the Spiritual Self • Be open to awe, inspiration, not knowing, not being in charge • Cherish your optimism and hope
Incorporating Self-Care • If you can’t do it all, make some time for what you love • Have faith in yourself, and associate with people who have faith in you. • Operate from confidence, rather than fear and insecurity
Ideas for Interpersonal Self-Care at Work • Take time to give & receive support • Develop a “buddy” system with a co-worker • Catch yourself when perceptions shift or intense feelings arise, and label if VT-related • Engage in “debriefing” around difficult cases • Admit it when you do not know an answer or make a mistake. For helps who have their own trauma history, ask for and accept comfort, counsel
Self-Assessment • Are formal and informal meetings with my peers part of my regular schedule? • If not, how can I build them into it on a regular basis? - Having a weekly breakfast or lunch together - Joining an association of like-minded individuals that meets on a regular basis - Getting regular supervision or consultation, formal or informal - Attending seminars and other opportunities for learning on a regular basis (conferences)
What are some of the barriers or obstacles that may get in your way of self-care?
Examples of Barriers in implementing better selfcare: Don’t have the time Don’t feel I should have to Feelings of shame about having problems or difficult time with the work Afraid others will think I can’t handle it Don’t want to burden others, especially family and friends Change is hard Beliefs that no one will understand or care Feeling negative/defeated at work
Other Barriers in Implementing Better Self-Care: • Lack of consistent supervision • Difficult setting limits/boundaries in your work and with victims • Attitude of “I can do this on my own” – a denial of stress or burnout or your own limits • Blaming others and/or self • Feeling powerless in changing things both with clients, community • Pattern of taking care of others first
How will you go about removing some of these barriers to self-care?
Self-Assessment • Which tasks do I not need to do at all? • Which tasks can be made simpler and less time-consuming? • Am I using the simplest, least complicated way to do my routine activities? (scheduling, billing, note-taking, correspondence, paperwork, other) • If not, how can I simplify those tasks?
Self-Care Strategies at the Organizational / Agency Level
Organizational • • • Creating a healthy work environment/organizational culture Providing supportive leadership Providing quality supervision Debriefing staff Hosting staff/team meetings, retreats, formal and informal opportunities to socialize Encouraging formal and informal peer support Acknowledging stress, STS, and VT as real issues Providing training and education, including orientation to the organization and role Encouraging staff health and wellness (e. g. , practices, programs, policies) VOC

Peer and Supervisor Support • Use effective communication skills • Encourage trusting, mutual relationships • Practice conflict resolution • Emphasize collaboration and teamwork VOC
VOC
Vicarious Resilience and Post Traumatic Growth Involves the process of learning about overcoming adversity from the trauma survivor and the resulting positive transformation and empowerment through their empathy and interaction. (Hernandez, Gangsei, and Engstrom, 2007) (OVC)
Impact of Vicarious Resilience • Greater perspective and appreciation of own problems • More optimistic, motivated, efficacious, and reenergized • Increased sense of hope, understanding, and belief in the possibility of recovery from trauma and other serious challenges • Profound sense of commitment to, and finding (Hernandez, et al, 2007; Engstrom, et al, 2008) meaning from the work (OVC)
Acknowledging the Positive: Compassion Satisfaction Vicarious Transformation (OVC)

Vicarious Posttraumatic Growth • Growth experienced through engagement with trauma survivors. (Allison)
Vicarious Posttraumatic Growth Exercise Find a partner and spent 5 -10 minutes exploring the following questions: • How are you affected by your patients’ stories of resilience and overcoming adversity? • What positive stories stand out to you about patients? • How do you hold onto hope for your patients? • Has working with those who’ve survived trauma made any positive differences in your life? If so, how? (Allison)
BREATHE

MLamb

Contact Information Alicia Boccellari, Ph. D. Director of Special Programs UCSF Trauma Recovery Center 2727 Mariposa Street, Suite 100 San Francisco, CA 94110 e. mail: alicia. boccellari@sfdph. org Phone: 415 -437 -3055 www. traumarecoverycenter. org UCSF University of California, San Francisco
 Vicarious felidae
Vicarious felidae Robyn bradey
Robyn bradey Vicarious trauma
Vicarious trauma Oeasundirect
Oeasundirect Libby whittaker
Libby whittaker Examples of self care
Examples of self care Uni due cm
Uni due cm Vicarius significado
Vicarius significado Vicarious transformation
Vicarious transformation Vicariously sentence
Vicariously sentence Yewen v noakes
Yewen v noakes When was the little albert experiment
When was the little albert experiment Vicarious liability means
Vicarious liability means Vicarious reinforcement
Vicarious reinforcement What is social learning theory
What is social learning theory Vicarious reinforcement
Vicarious reinforcement Vicarious reinforcement
Vicarious reinforcement Vicarious reinforcement
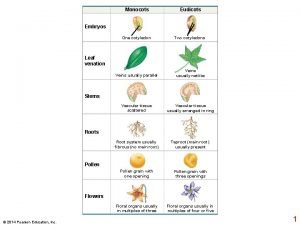
Vicarious reinforcement Plant growth definition
Plant growth definition Pith
Pith Primary growth and secondary growth in plants
Primary growth and secondary growth in plants Chapter 35 plant structure growth and development
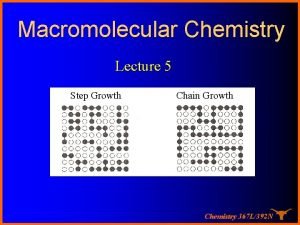
Chapter 35 plant structure growth and development Growthchain
Growthchain Geometric growth vs exponential growth
Geometric growth vs exponential growth Neoclassical growth theory vs. endogenous growth theory
Neoclassical growth theory vs. endogenous growth theory Organic vs inorganic growth
Organic vs inorganic growth Nc resilience and learning project
Nc resilience and learning project Social emotional assets and resilience scales pdf
Social emotional assets and resilience scales pdf National risk and resilience unit
National risk and resilience unit Firefighter pqa example answers
Firefighter pqa example answers Building grit and resilience
Building grit and resilience Resilience index measurement and analysis
Resilience index measurement and analysis Johannes volkelt empathy theory
Johannes volkelt empathy theory Types of resilience
Types of resilience Boing boing resilience
Boing boing resilience Meaning of resilience
Meaning of resilience Resilience in a box
Resilience in a box Resilience assembly
Resilience assembly Network resilience a systematic approach
Network resilience a systematic approach Mechanical properties of materials
Mechanical properties of materials Modulus of toughness
Modulus of toughness Assembly on resilience
Assembly on resilience Resilience aesthetic
Resilience aesthetic Family resilience framework
Family resilience framework I have resilience
I have resilience Emotional resilience in nursing
Emotional resilience in nursing Master resilience training modules
Master resilience training modules I have resilience
I have resilience Kent resilience forum
Kent resilience forum Uk climate resilience programme
Uk climate resilience programme Emotional resilience in social work
Emotional resilience in social work Resilience vs fault tolerance
Resilience vs fault tolerance Resilience in the classroom
Resilience in the classroom I have resilience
I have resilience Emotional resilience lds manual
Emotional resilience lds manual Mershon center
Mershon center Resilience pyramid
Resilience pyramid 10 guideposts for wholehearted living poster
10 guideposts for wholehearted living poster Resilience direct
Resilience direct Colour for resilience
Colour for resilience National resilience strategy
National resilience strategy Resilience in the classroom
Resilience in the classroom Resilience
Resilience Resilience
Resilience Azure resilience patterns
Azure resilience patterns Compassion resilience toolkit
Compassion resilience toolkit Receliance
Receliance Resilience meaning
Resilience meaning What is psychological first aid
What is psychological first aid Pilot programme for climate resilience
Pilot programme for climate resilience 5 pillars of resilience
5 pillars of resilience Leading age colorado
Leading age colorado Resilience examples
Resilience examples Bonnie benard resilience
Bonnie benard resilience Acrostic poem for resilience
Acrostic poem for resilience Resistance vs resilience
Resistance vs resilience