CRT 2019 Renal Denervation with Ultrasound Felix Mahfoud


- Slides: 16
CRT 2019 Renal Denervation with Ultrasound Felix Mahfoud Saarland University Hospital, Homburg, Germany
Potential Conflicts of Interest I have the following potential conflicts of interest to report: Research grants: • Deutsche Hochdruckliga • Deutsche Gesellschaft für Kardiologie • Saarländisches Ministerium für Wissenschaft und Forschung • Medtronic, St. Jude Consultant/Lecture fee: • Medtronic, Recor
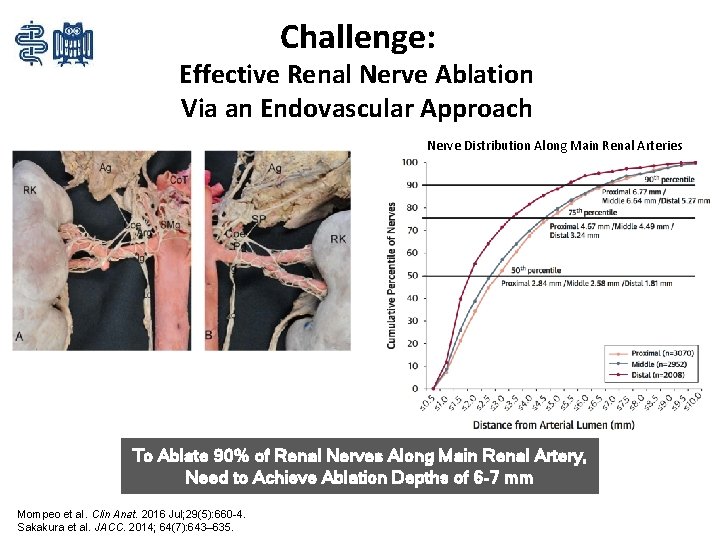
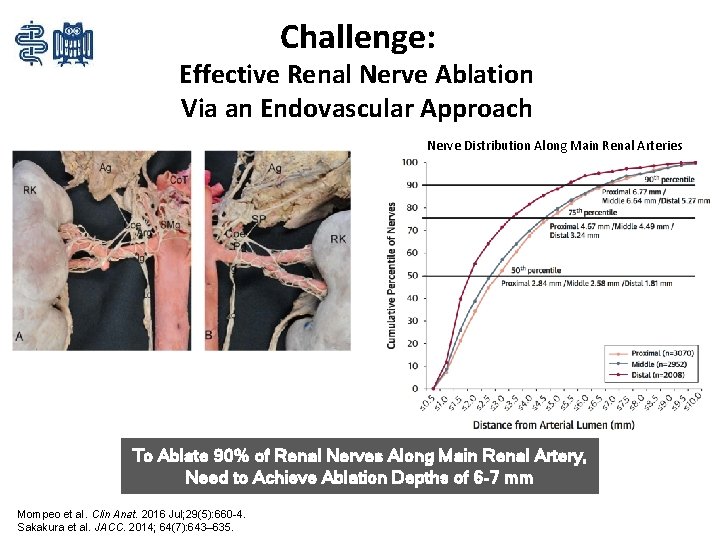
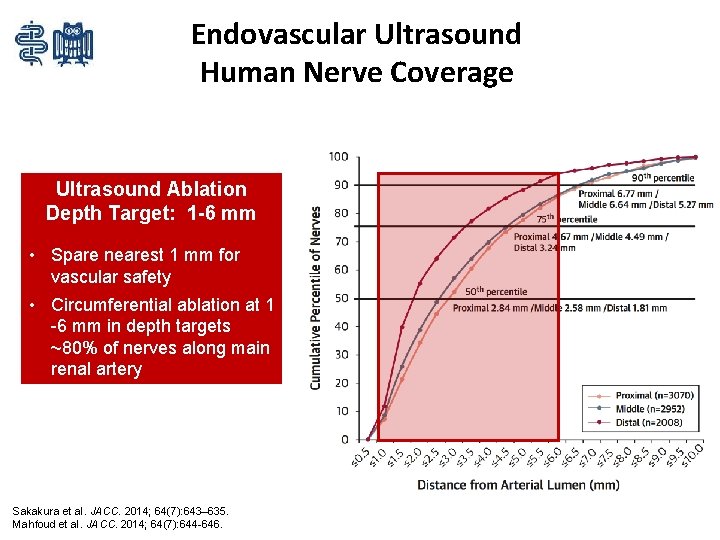
Challenge: Effective Renal Nerve Ablation Via an Endovascular Approach Nerve Distribution Along Main Renal Arteries To Ablate 90% of Renal Nerves Along Main Renal Artery, Need to Achieve Ablation Depths of 6 -7 mm Mompeo et al. Clin Anat. 2016 Jul; 29(5): 660 -4. Sakakura et al. JACC. 2014; 64(7): 643– 635.
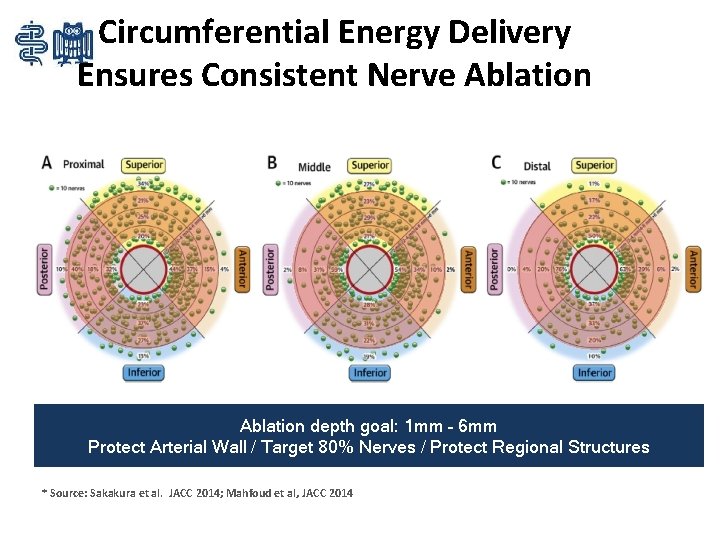
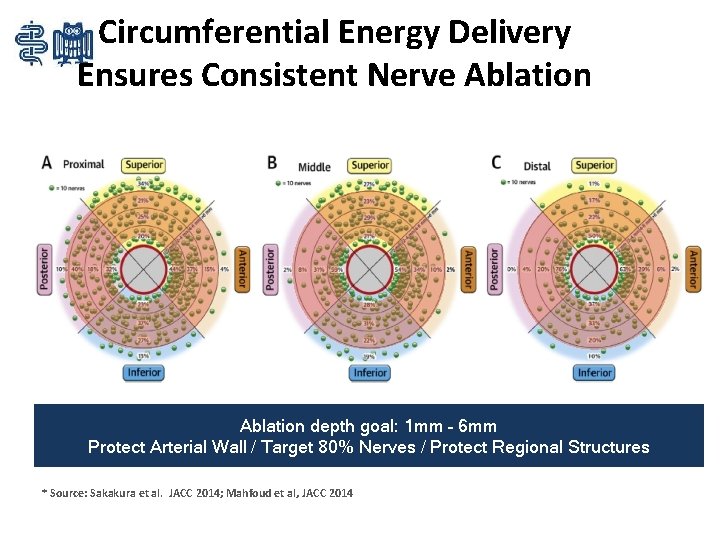
Circumferential Energy Delivery Ensures Consistent Nerve Ablation depth goal: 1 mm – 6 mm Protect Arterial Wall / Target 80% Nerves / Protect Regional Structures * Source: Sakakura et al. JACC 2014; Mahfoud et al, JACC 2014
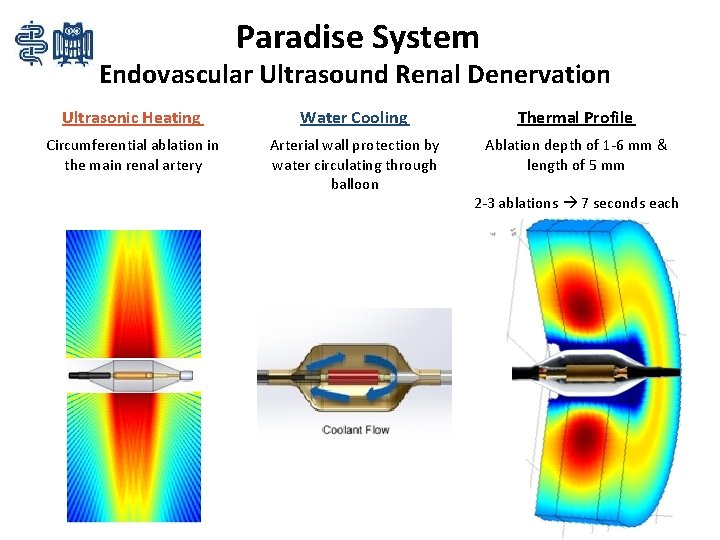
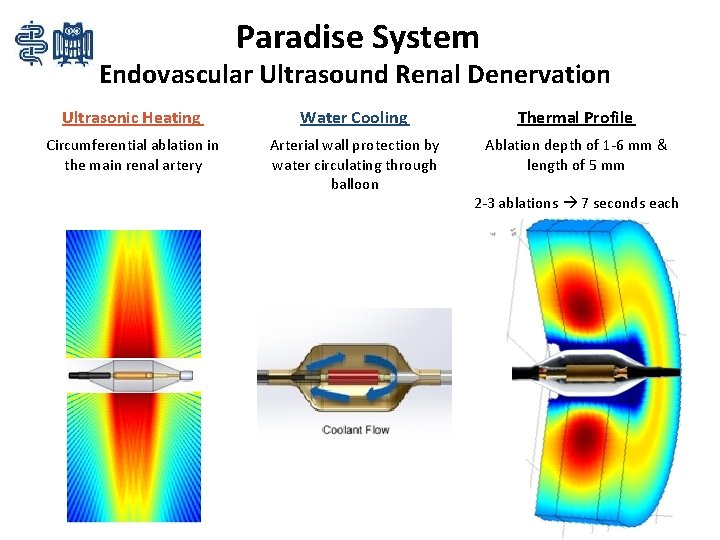
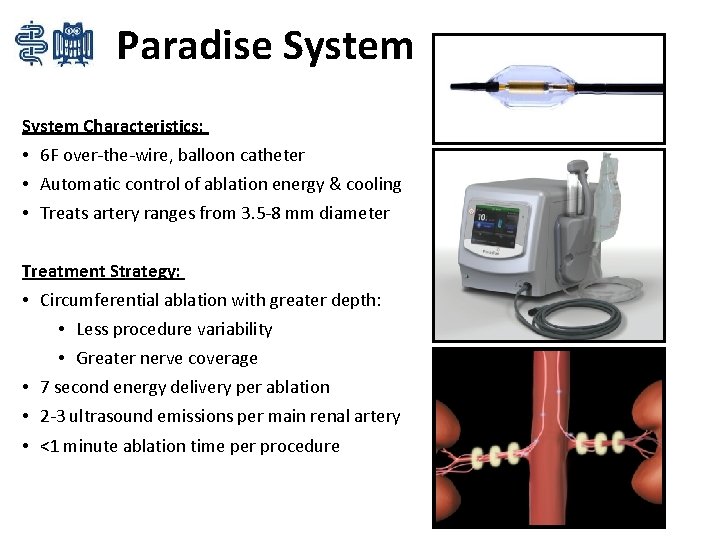
Paradise System Endovascular Ultrasound Renal Denervation Ultrasonic Heating Water Cooling Thermal Profile Circumferential ablation in the main renal artery Arterial wall protection by water circulating through balloon Ablation depth of 1 -6 mm & length of 5 mm 2 -3 ablations 7 seconds each
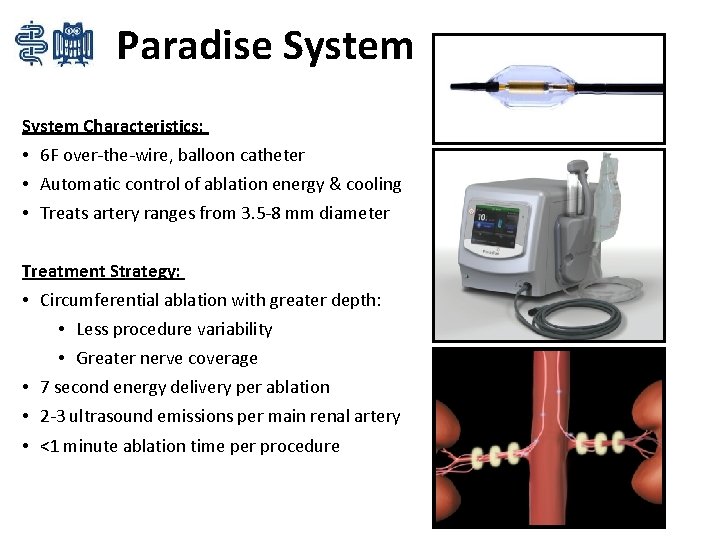
Paradise System Characteristics: • 6 F over-the-wire, balloon catheter • Automatic control of ablation energy & cooling • Treats artery ranges from 3. 5 -8 mm diameter Treatment Strategy: • Circumferential ablation with greater depth: • Less procedure variability • Greater nerve coverage • 7 second energy delivery per ablation • 2 -3 ultrasound emissions per main renal artery • <1 minute ablation time per procedure

Ablation Creation: Gel Becomes Opaque at Ablative Temperatures
Procedural Angiogram
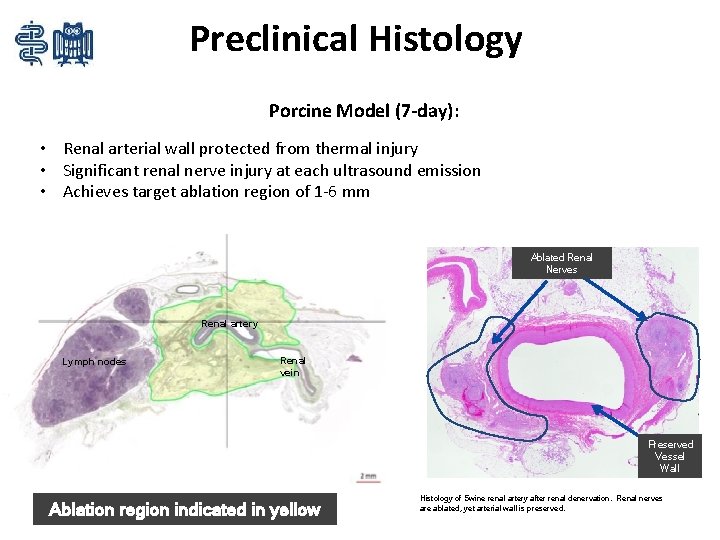
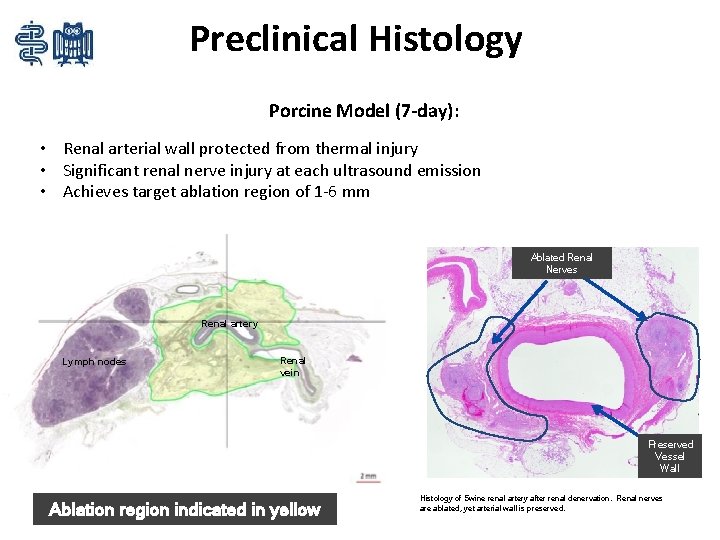
Preclinical Histology Porcine Model (7 -day): • Renal arterial wall protected from thermal injury • Significant renal nerve injury at each ultrasound emission • Achieves target ablation region of 1 -6 mm Ablated Renal Nerves Renal artery Lymph nodes Renal vein Preserved Vessel Wall Ablation region indicated in yellow Histology of Swine renal artery after renal denervation. Renal nerves are ablated, yet arterial wall is preserved.
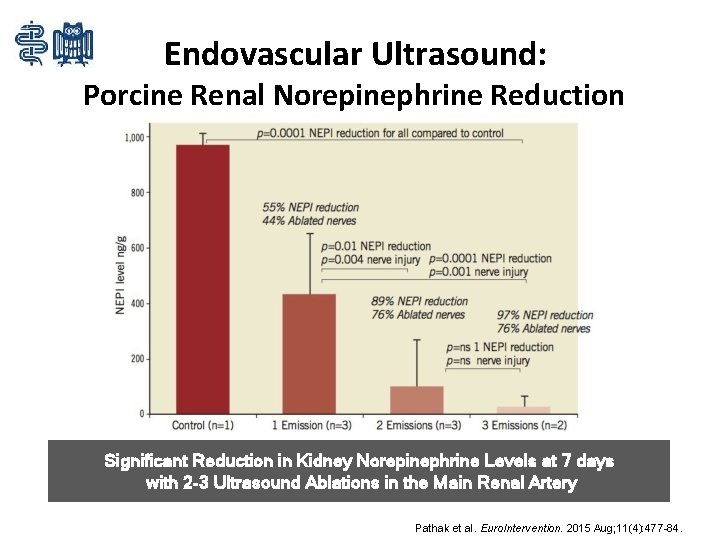
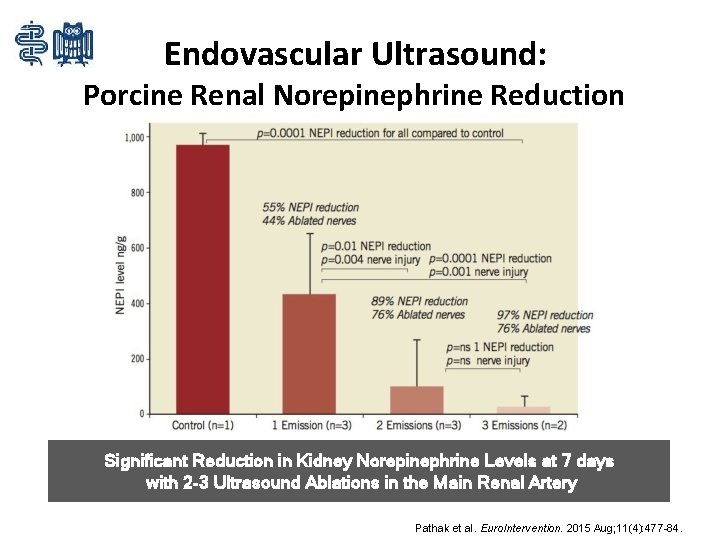
Endovascular Ultrasound: Porcine Renal Norepinephrine Reduction Significant Reduction in Kidney Norepinephrine Levels at 7 days with 2 -3 Ultrasound Ablations in the Main Renal Artery Pathak et al. Euro. Intervention. 2015 Aug; 11(4): 477 -84.
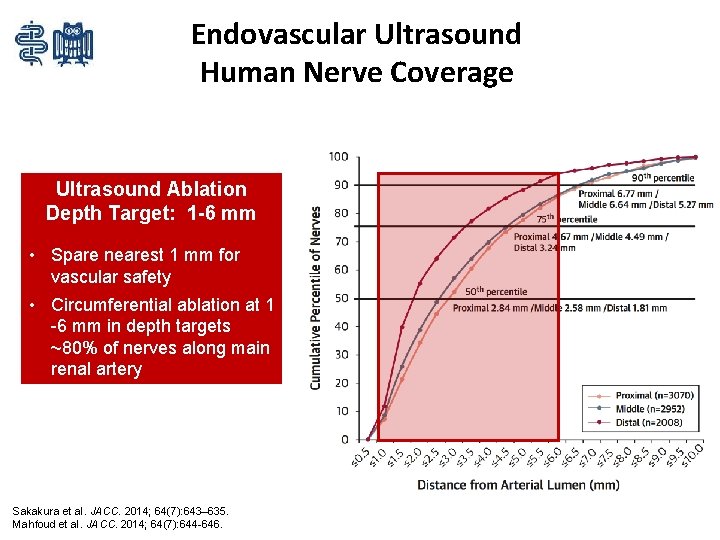
Endovascular Ultrasound Human Nerve Coverage Ultrasound Ablation Depth Target: 1 -6 mm • Spare nearest 1 mm for vascular safety • Circumferential ablation at 1 -6 mm in depth targets ~80% of nerves along main renal artery Sakakura et al. JACC. 2014; 64(7): 643– 635. Mahfoud et al. JACC. 2014; 64(7): 644 -646.
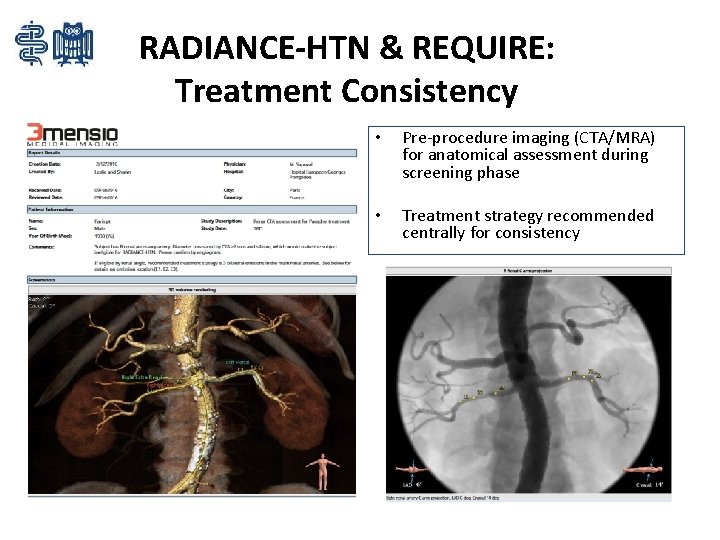
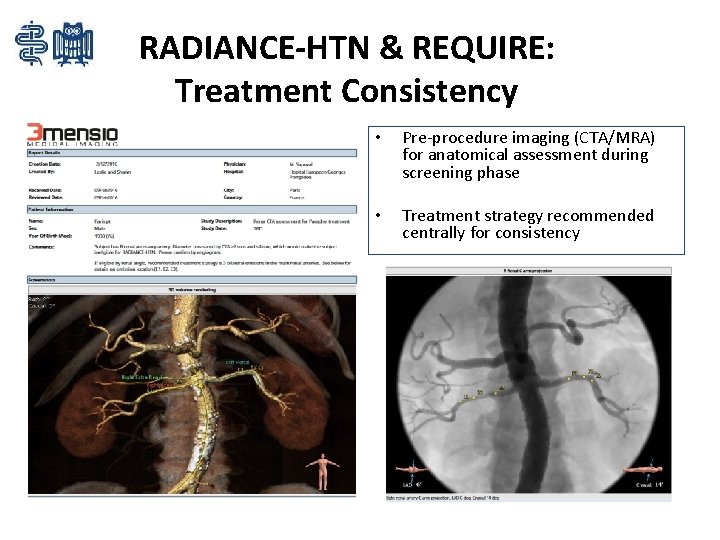
RADIANCE-HTN & REQUIRE: Treatment Consistency • Pre-procedure imaging (CTA/MRA) for anatomical assessment during screening phase • Treatment strategy recommended centrally for consistency
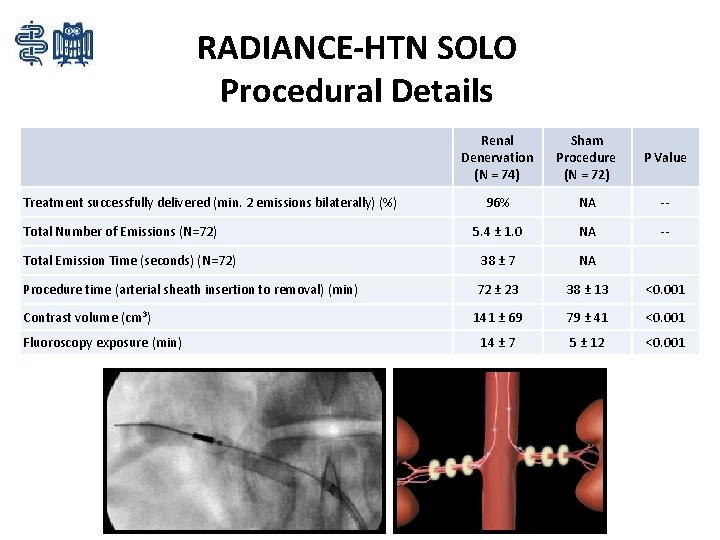
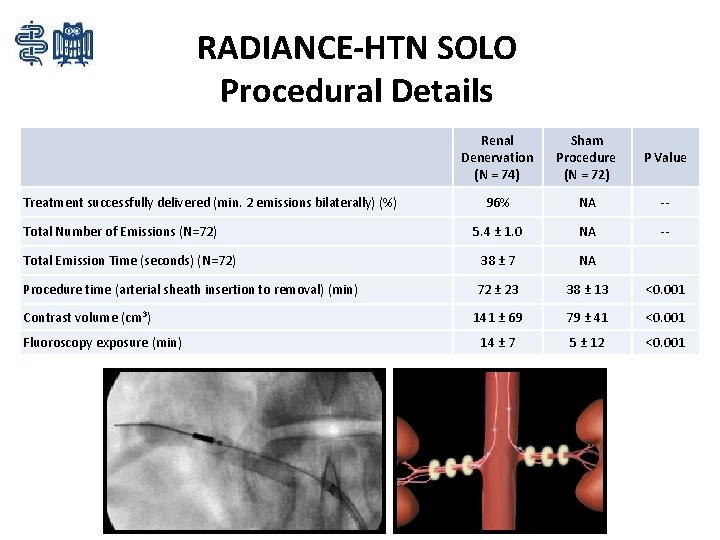
RADIANCE-HTN SOLO Procedural Details Renal Denervation (N = 74) Sham Procedure (N = 72) P Value 96% NA -- 5. 4 ± 1. 0 NA -- Total Emission Time (seconds) (N=72) 38 ± 7 NA Procedure time (arterial sheath insertion to removal) (min) 72 ± 23 38 ± 13 <0. 001 Contrast volume (cm 3) 141 ± 69 79 ± 41 <0. 001 14 ± 7 5 ± 12 <0. 001 Treatment successfully delivered (min. 2 emissions bilaterally) (%) Total Number of Emissions (N=72) Fluoroscopy exposure (min)
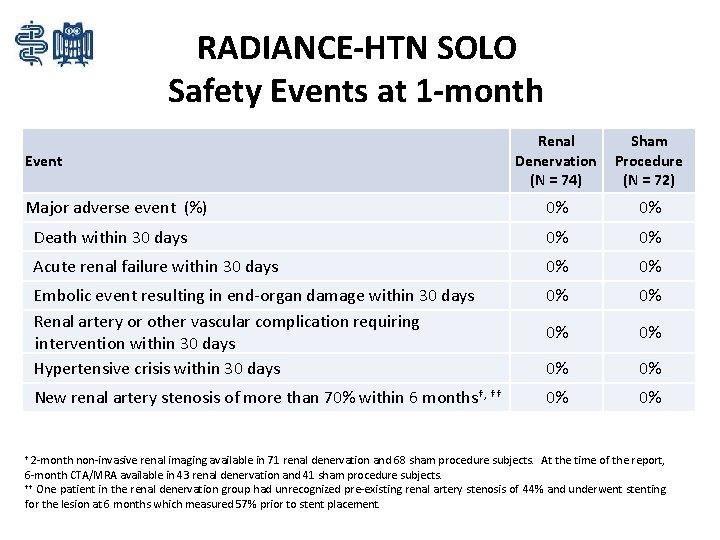
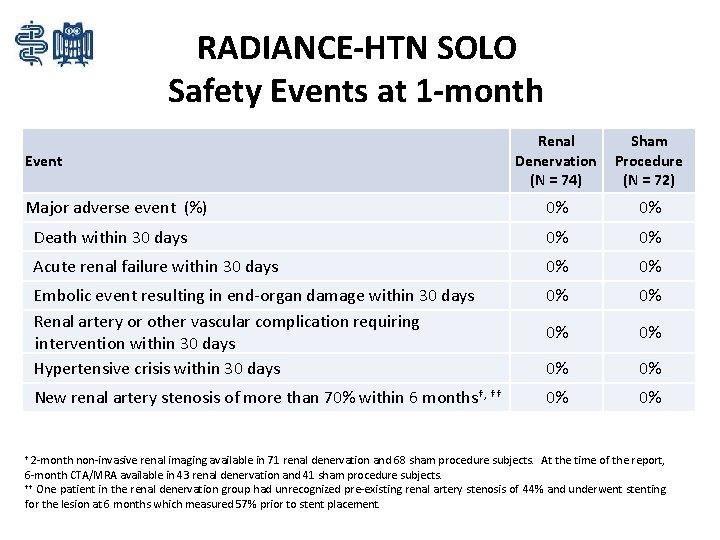
RADIANCE-HTN SOLO Safety Events at 1 -month Renal Denervation (N = 74) Sham Procedure (N = 72) 0% 0% Death within 30 days 0% 0% Acute renal failure within 30 days 0% 0% Embolic event resulting in end-organ damage within 30 days Renal artery or other vascular complication requiring intervention within 30 days Hypertensive crisis within 30 days 0% 0% 0% New renal artery stenosis of more than 70% within 6 months†, †† 0% 0% Event Major adverse event (%) † 2 -month non-invasive renal imaging available in 71 renal denervation and 68 sham procedure subjects. At the time of the report, 6 -month CTA/MRA available in 43 renal denervation and 41 sham procedure subjects. †† One patient in the renal denervation group had unrecognized pre-existing renal artery stenosis of 44% and underwent stenting for the lesion at 6 months which measured 57% prior to stent placement.
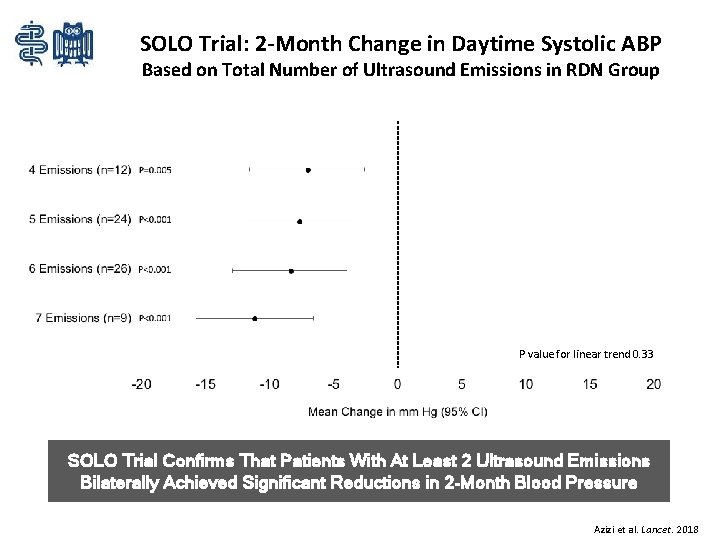
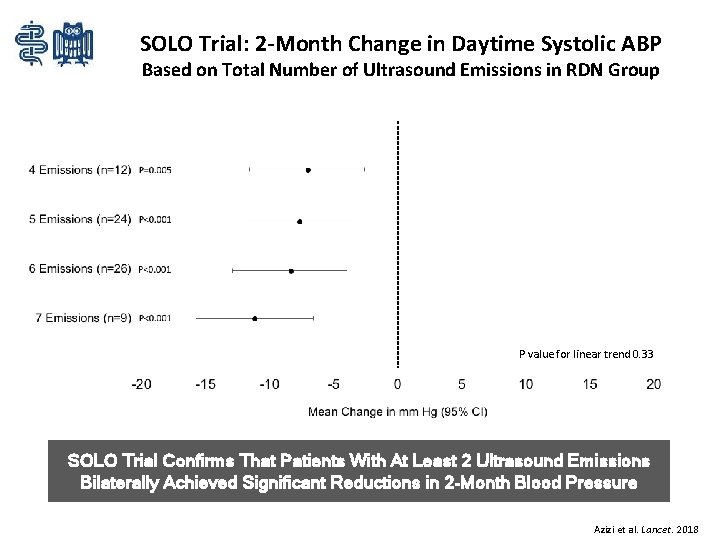
SOLO Trial: 2 -Month Change in Daytime Systolic ABP Based on Total Number of Ultrasound Emissions in RDN Group P value for linear trend 0. 33 SOLO Trial Confirms That Patients With At Least 2 Ultrasound Emissions Bilaterally Achieved Significant Reductions in 2 -Month Blood Pressure Azizi et al. Lancet. 2018

Thank you! Felix Mahfoud, MD FESC Klinik für Innere Medizin III Kardiologie, Angiologie und Intern. Intensivmedizin Universitätsklinikum des Saarlandes Homburg/Saar felix. mahfoud@uks. eu
 Renal denervation
Renal denervation Wholey wire cardiac
Wholey wire cardiac Res extra commercium
Res extra commercium Diagnostico etiologico
Diagnostico etiologico Ferriman–gallwey score
Ferriman–gallwey score Cortical and juxtamedullary nephrons difference
Cortical and juxtamedullary nephrons difference Crt
Crt Glass envelope in crt
Glass envelope in crt Monitor crt partes
Monitor crt partes Rsa crt calculator
Rsa crt calculator Pokupka
Pokupka Crt 2010
Crt 2010 Critical race theory curriculum examples
Critical race theory curriculum examples Monitory crt
Monitory crt Crt display technology
Crt display technology Fosdick test
Fosdick test Schemat monitora crt
Schemat monitora crt