COMMON GYNECOLOGIC PROCEDURES AZZA Al YAMANI Department of












- Slides: 45
COMMON GYNECOLOGIC PROCEDURES AZZA Al. YAMANI Department of Obestetrics and Gynecology
Common Gynecologic Procedures Aim of this presentation is : 1. students become aware of the basic principles of common gynecologic surgical procedures. 2. become familial with the instruments that used in these procedures. 3. and be aware of the indications and complications of each procedure.
{1} Endometrial Sampling ( Dilatation & Curettage) D & C * it is the most common minor gynecologic surgical procedure , it is used as diagnostic or therapeutic tool. * in spite of the advances in office – based evaluation of the endometrium as US or hysteroscopy , a thorough fractional curettage is the best procedure if endometrial or cervical cancer is suspected.
Indications Diagnostic: 1. abnormal uterine bleeding. 2. postmenopausal bleeding , end. ca. 3. irregularities of the endometrial cavity either congenital ( uterine septum) or acquired (submucous fibroids or polyp)can be determined during the operation.
Therapeutic: 1. endometrial hyperplasia with heavy bleeding. 2. removal of endometrial polyps or small pedunculated myomas. 3. dilatation & evacuation in inevitable and missed abortion. 4. removal of missed intrauterine IUCD.

Technique instruments

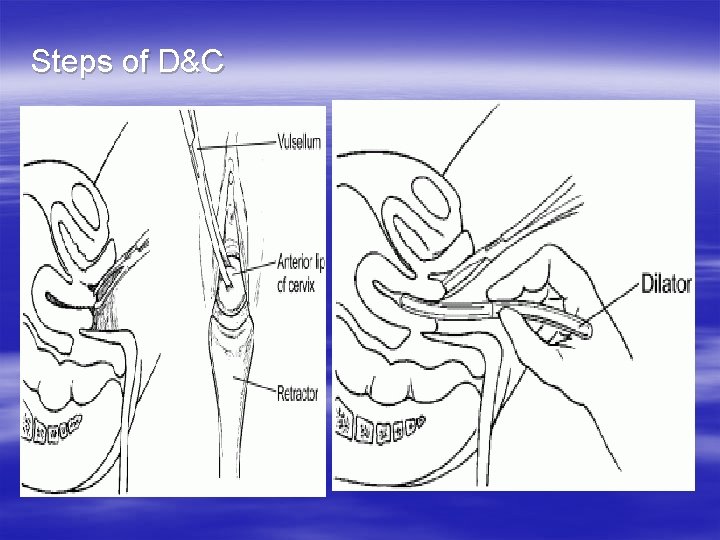
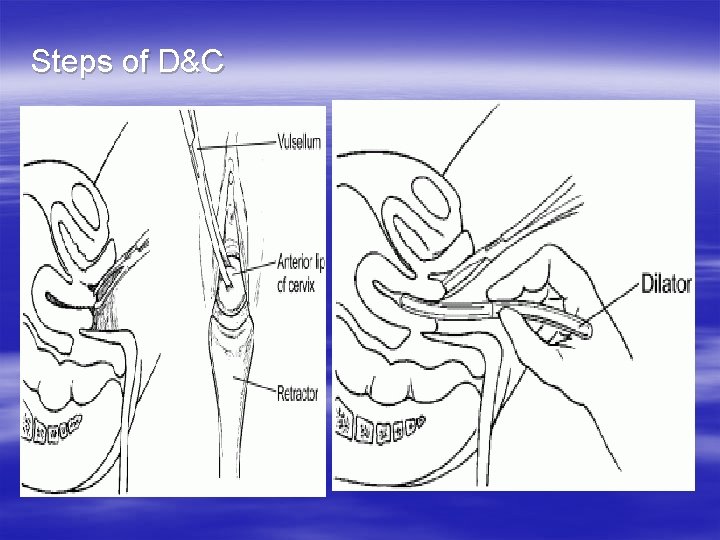
Steps of D&C


Complications: 1. Perforation of the uterus. it is not uncommon complication , it occurs in : * RVF uterus. * pregnancy. * postmenopausal è endometrial carcinoma. 2. Cervical laceration. 3. Infection. 4. Haemorrahge.
Endometrial Ablation it is the complete destruction of the endometrium down to the basal layer , resulting in fibrosis of the uterine cavity and amenorrhoea ( 30% ) , however , patient satisfaction rates are over 70%. Ia It indicated in women who have heavy menstrual bleeding that is impacting her life and do not have other problems that require hysterectomy. Endometrial ablation is now well established as day case or outpatient procedure.
Endometrial Ablation is performed using the resectoscope which is : a hysteroscpe with a build in wire loop(or other shape device ) that uses high frequency electrical current to cut or coagulate tissue. Indications: 1. abnormal uterine bleeding. 2. benign lesions as small submucus myomas or endometrial polyps.
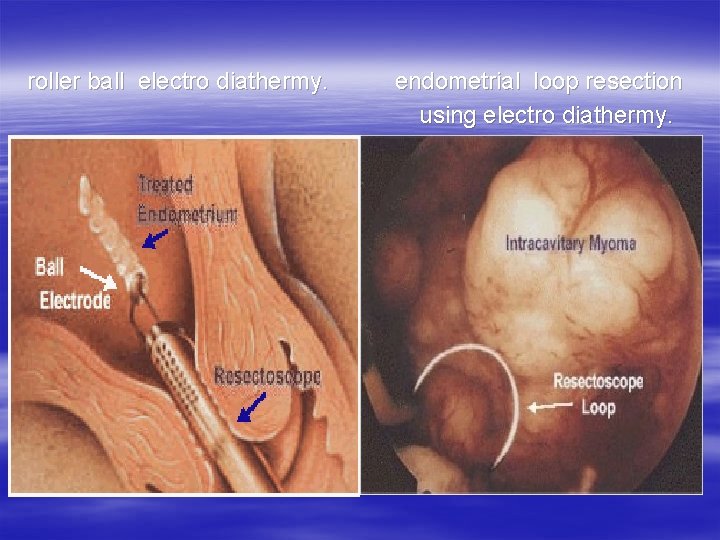
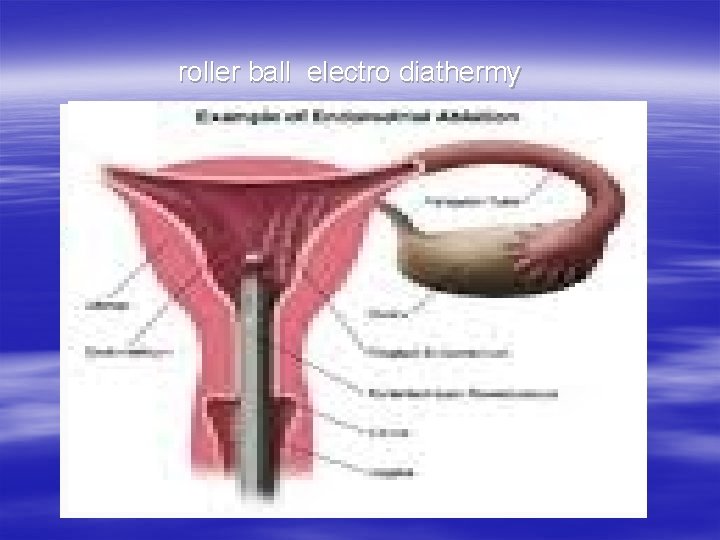
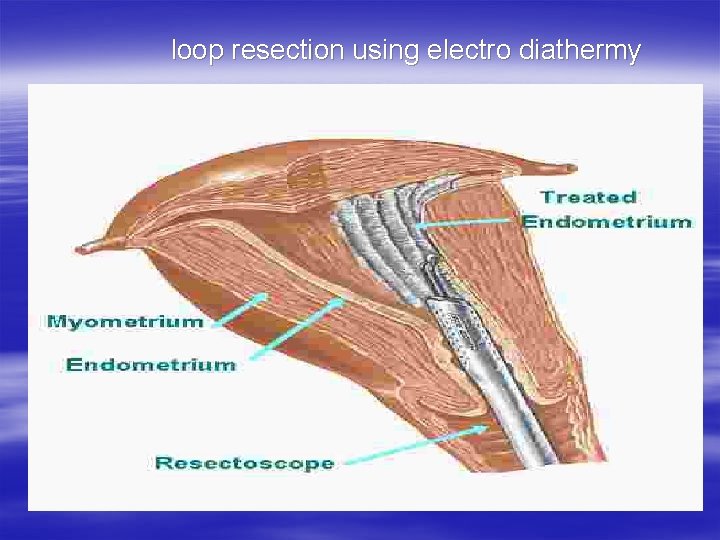
Technique Established techniques carried out under direct hysteroscopic vision involve the use of fluid for distention and irrigation. These techniques are : * laser ablation. * endometrial loop resection using electro diathermy. * roller ball electro diathermy.

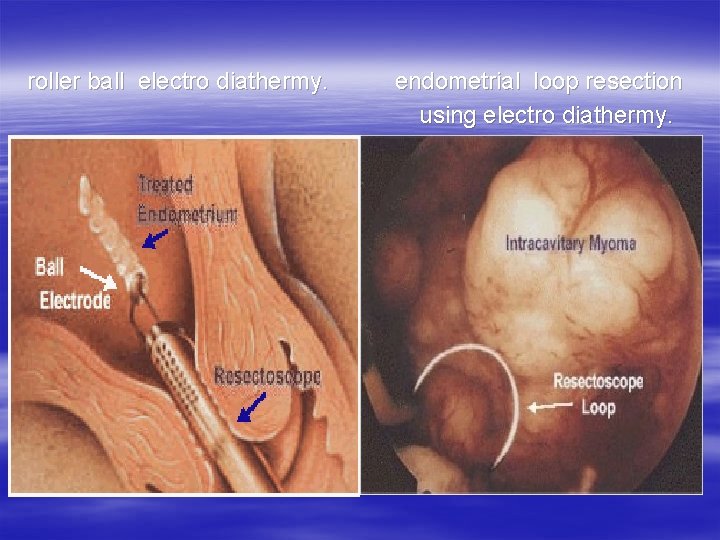
roller ball electro diathermy. endometrial loop resection using electro diathermy.
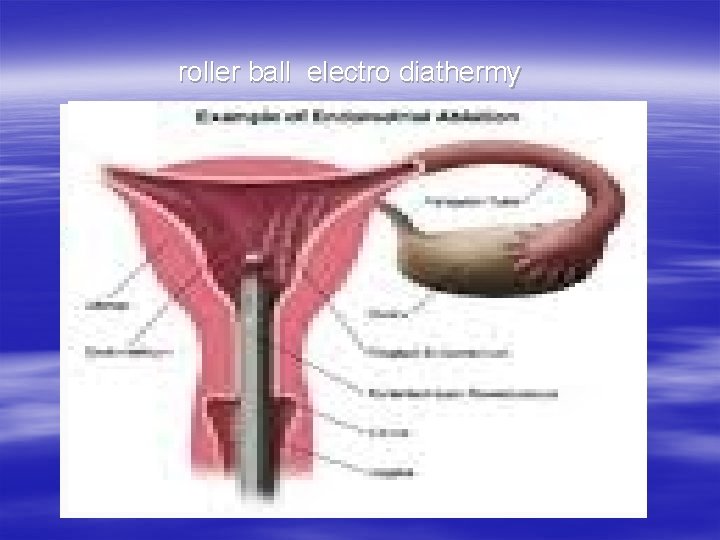
roller ball electro diathermy
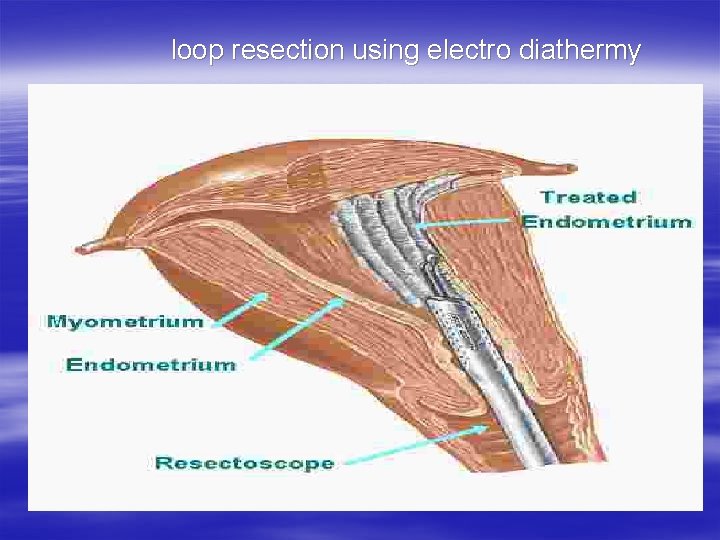
loop resection using electro diathermy
Complications : 2% 1. uterine perforation. 2. hemorrhage. 3. infections as endometritis & PID. 4. bowel or urinary tract injury. 5. cervical lacerations & stenosis. 5. distention medium hazards as: * gas embolism. * fluid overload. * anaphylactic shock.
Although the resectoscope provides excellent results in experienced hands, the technique is difficult to master. because all the previous techniques are: * operator dependent. * time consuming. * carry risk of systemic fluid absorption. * hemorrhage. * uterine perforation è heat damage to adjacent structures.
Other methods of ablation Newer techniques have been developed with the aim of reducing operator dependency and minimizing risk. Of these , the best evaluated to date are : * microwave ablation. * thermal balloon ablation. They have equivalent short-term efficacy with the advantage of shorter operating times and fewer complications.
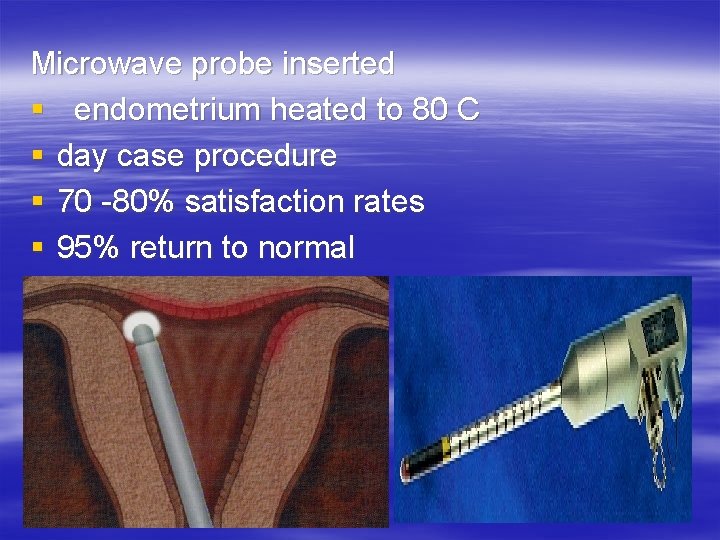
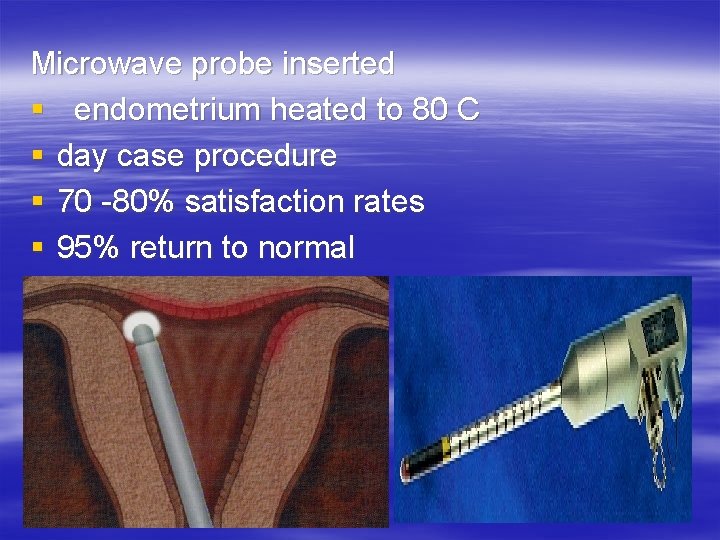
Microwave probe inserted § endometrium heated to 80 C § day case procedure § 70 -80% satisfaction rates § 95% return to normal
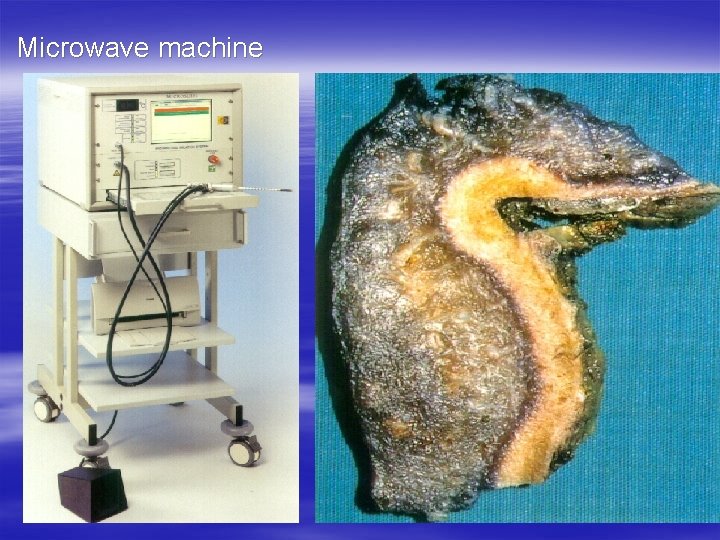
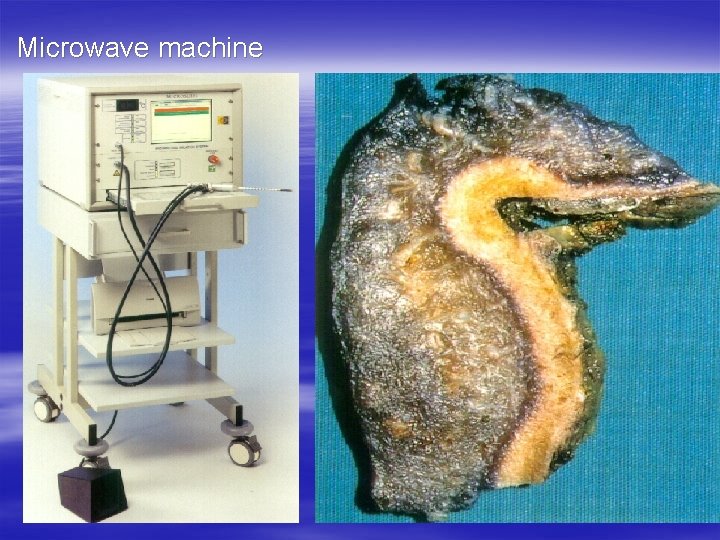
Microwave machine
Thermachoice ballon This uses a balloon placed in the uterine cavity through the cervix. Hot water is circulated inside the balloon to destroy the endometrium. Thermachoice Balloon Ablation Central element heats liquid circulated in balloon 87 degrees C for 8 minutes. Limitations: * uterine cavity size 6 -10 cm; * can’t treat submucous myomas.


Thermachoice ballon Fig. The 3 - Thermachoice The Caveterm System
Hysterectomy it is the most commonly performed major gynecologic operation , it can be performed either Abdominally , vaginally or laparoscopically. although some indications remain controversial , high patient satisfaction levels and increasing safety for the procedure have been reported.
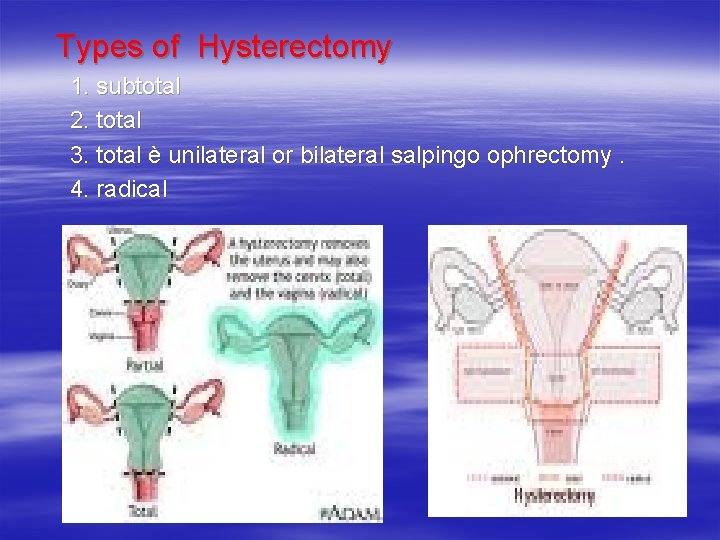
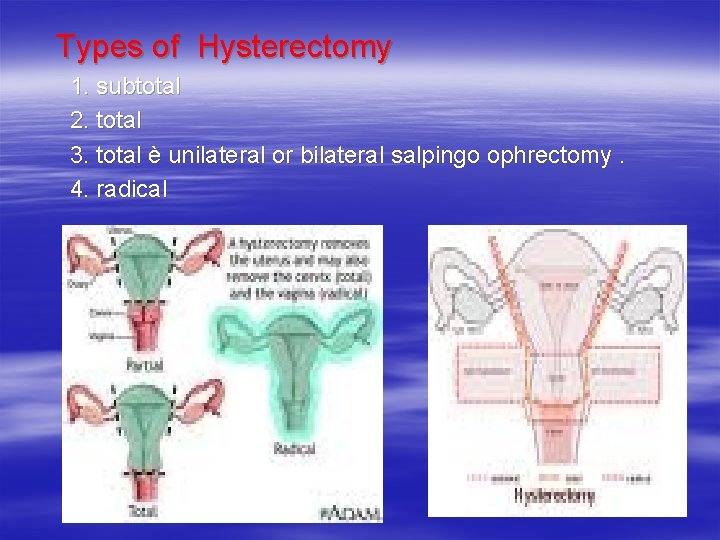
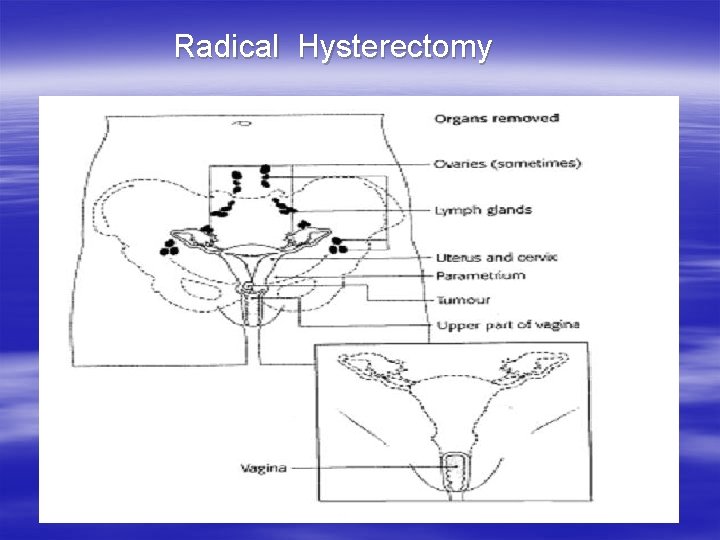
Types of Hysterectomy 1. subtotal 2. total 3. total è unilateral or bilateral salpingo ophrectomy. 4. radical
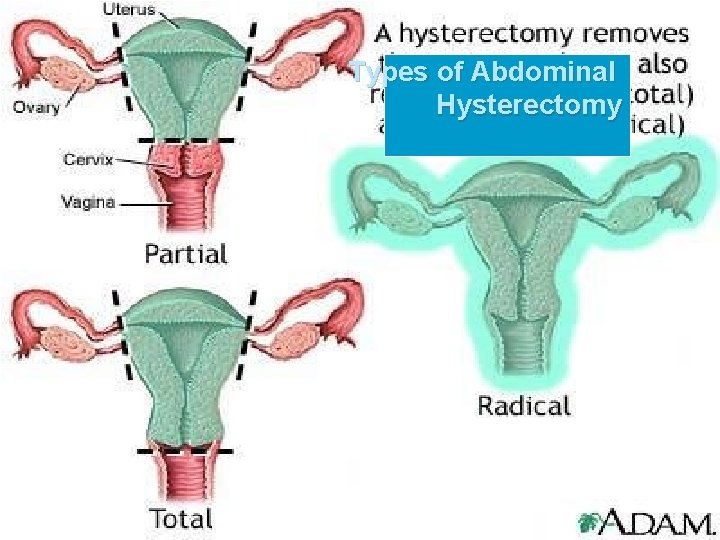
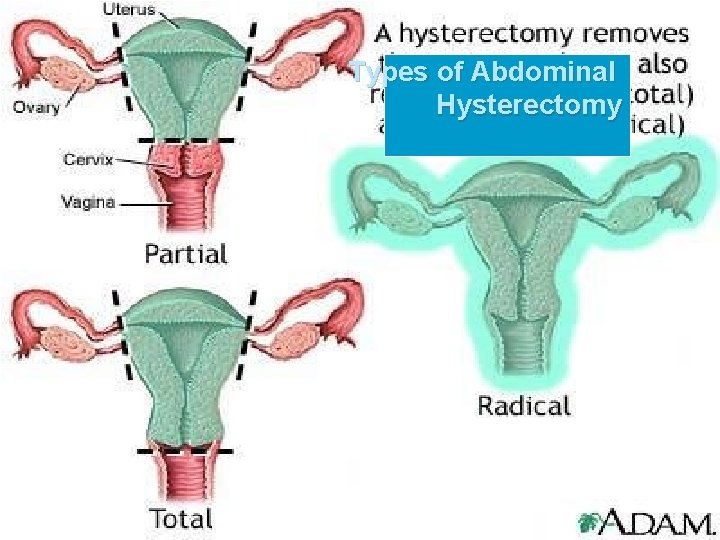
Types of Abdominal Hysterectomy
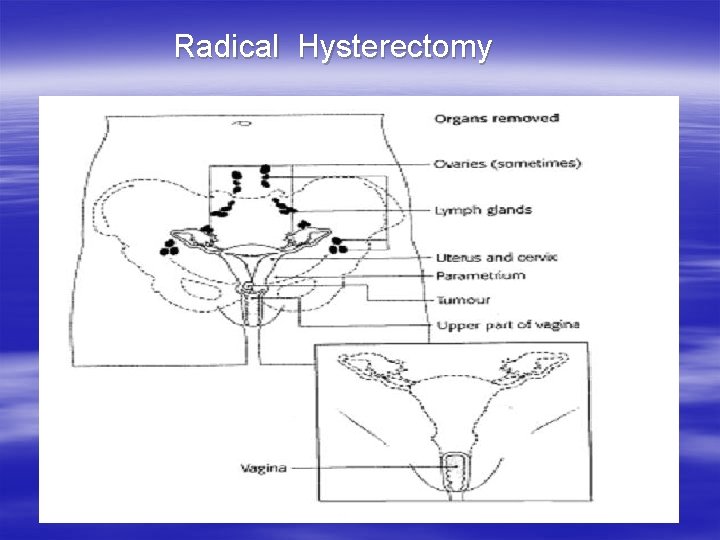
Radical Hysterectomy
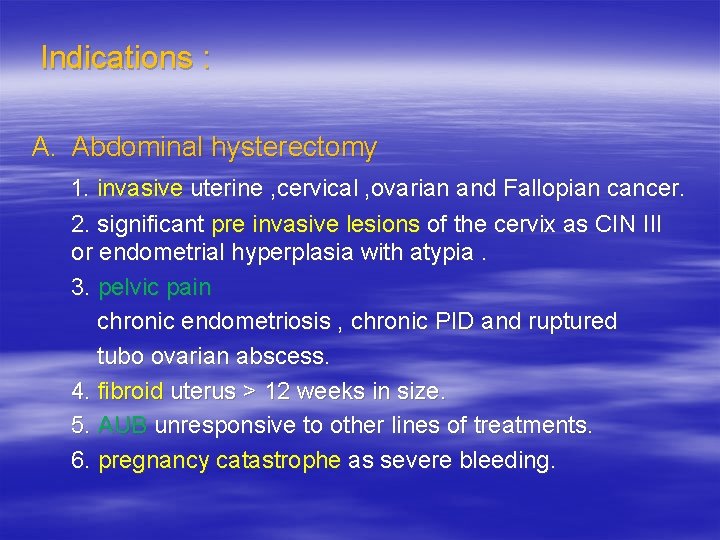
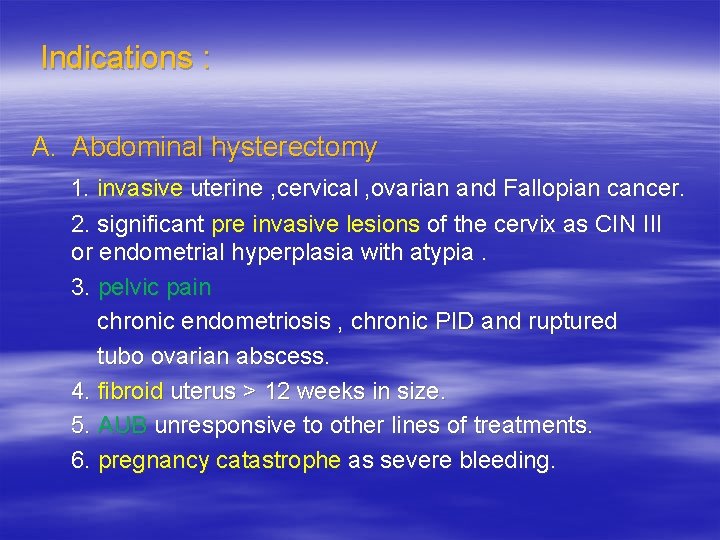
Indications : A. Abdominal hysterectomy 1. invasive uterine , cervical , ovarian and Fallopian cancer. 2. significant pre invasive lesions of the cervix as CIN III or endometrial hyperplasia with atypia. 3. pelvic pain chronic endometriosis , chronic PID and ruptured tubo ovarian abscess. 4. fibroid uterus > 12 weeks in size. 5. AUB unresponsive to other lines of treatments. 6. pregnancy catastrophe as severe bleeding.
B. vaginal hysterectomy 1. utero vaginal prolapse. 2. AUB with small uterus. pre requesits to vaginal hysterectomy : * benign disease. * uterus is mobile with some pelvic relaxation & no pelvic adhesions. * uterus is < 12 weeks in size.
C. Laparoscopic hysterectomy * < 10% of hysterectomies performed with the use of laparoscopy. * it is used to assist in vaginal hysterectomy or to convert an abdominal to a vaginal hysterectomy.
Technique 1. supine position. 2. general anaesthesia. 3. a careful abdominal & pelvic exam. under anaesthesia is carried out. 4. incision * vertical in obese , if endometriosis is anticipated and patients who have had several prior abdominal operations. * transverse in restricted benign disease.

5. exploration of the upper abdominal organs especially the liver , spleen and para-aortic lymph nodes. 6. the abdominal viscera are packed up with towels. 7. round ligament. each is clamped incised and ligated. 8. the vesico-uterine fold of peritoneum is incised transversely between the incised round lig. and the bladder is reflected inferiorly. 9. the two layers of the broad ligam. are separated and the ureters are explored and identified.
10. the infundibulo pelvic ligs. with the ovarian vessels are clamped , cut and ligated. if the adnexa are to be removed. 11. the broad lig. is then incised towards the uterus exposing the uterine vessels (skeletonized). 12. the uterine vessels are clamped at the level of internal cervical os , incised and ligated on each side. 13. medial to the ligated uterine vessels , the cardinal lig. on each side is clamped , incised and ligated.


14. posteriorlly , the peritoneum between the uterosacral lig. is incised transversely and the rectum is freed from the posterior aspect of the cervix & upper vagina after the uterosacral lig. are clamped , incised & ligated. 15. the total uterus is removed by cutting across the vagina just below the cervix. 16. the vaginal cuff is closed è absorbable sutures , incorporating the cardinal & uterosacral ligs. into each lateral angle to avoid latter development of vault prolapse.
Sites of ureteric injures : 1. at clamping & incising the infundibulo pelvic ligaments. 2. at ligating the uterine vessels. 3. at clamping & incising the cardinal ligs. if the urinary bladder is not sufficiently reflected inferiorly.
Complications : A. Intra operative 1. hemorrhage. 2. ureteric injuries. 3. bladder and bowel injury. 4. anesthetic complications. B. Post operative 1. wound infection ( 5 days postoperatively). 2. UTI. 3. thrombophlebitis and pulmonary embolism, ( 7 – 12 days ). 4. uretero vaginal fistula ( 5 – 21 days ).

Thank you

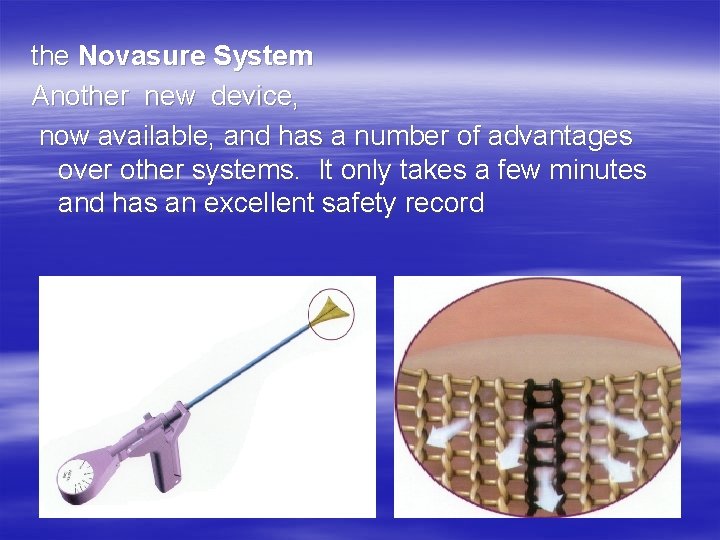
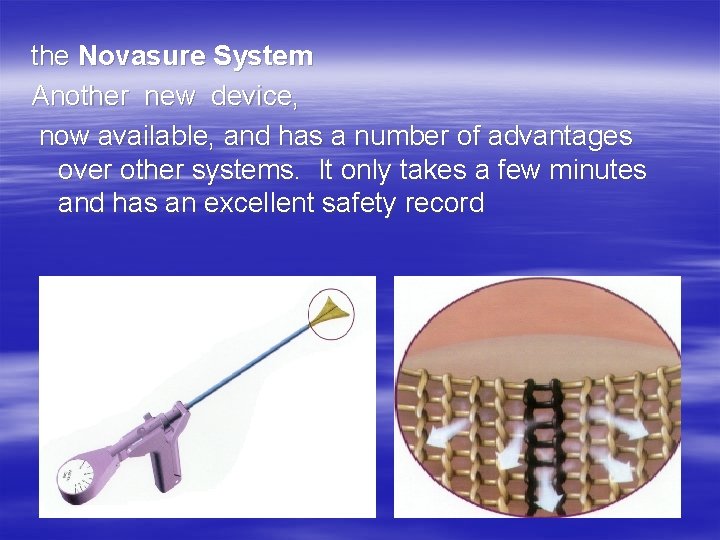
the Novasure System Another new device, now available, and has a number of advantages over other systems. It only takes a few minutes and has an excellent safety record
 Azza ouled zaid
Azza ouled zaid Azza spectra
Azza spectra Zain yamani
Zain yamani Niat tawaf sunat
Niat tawaf sunat Chapter 23 gynecologic emergencies
Chapter 23 gynecologic emergencies Cent kfupm
Cent kfupm Hcf 60 and 72
Hcf 60 and 72 Lowest common factor
Lowest common factor Factors to 18
Factors to 18 Lcm of 48 and 60
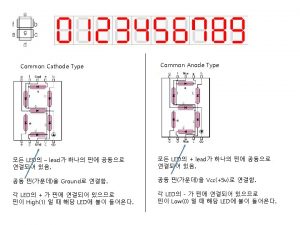
Lcm of 48 and 60 Common anode and common cathode
Common anode and common cathode Highest common factors and lowest common multiples
Highest common factors and lowest common multiples Family medicine fellowship
Family medicine fellowship Substantive audit procedures for payroll
Substantive audit procedures for payroll Hospital patient room cleaning procedures
Hospital patient room cleaning procedures Procedural fluency examples
Procedural fluency examples Basic kitchen procedures
Basic kitchen procedures Mechanical dishwashing procedures
Mechanical dishwashing procedures Preliminary audit
Preliminary audit How do auditing standards differ from auditing procedures
How do auditing standards differ from auditing procedures Advantages and disadvantages of projective tests
Advantages and disadvantages of projective tests Audit procedures
Audit procedures Reperformance audit
Reperformance audit Designing accurate data entry procedures
Designing accurate data entry procedures Chain of custody procedures
Chain of custody procedures Functional check
Functional check Audit planning and analytical procedures
Audit planning and analytical procedures Anatomic form impression
Anatomic form impression Hospital patient room cleaning procedures
Hospital patient room cleaning procedures Database policy and procedures
Database policy and procedures Quality control in hematology wikipedia
Quality control in hematology wikipedia Multiple opportunity method aba
Multiple opportunity method aba Instructional procedures examples
Instructional procedures examples National planning procedures handbook
National planning procedures handbook Procedures in python
Procedures in python Types of enema
Types of enema Bsbhrm506 assessment answers
Bsbhrm506 assessment answers Work study examines *
Work study examines * Troop leading procedures army
Troop leading procedures army Food objectives
Food objectives Lte nas procedures
Lte nas procedures Mutually exclusive procedures
Mutually exclusive procedures Evacuation procedures
Evacuation procedures Designing accurate data entry procedures
Designing accurate data entry procedures Chapter 8 sanitation procedures
Chapter 8 sanitation procedures Data gathering procedure in research example
Data gathering procedure in research example