Diseases of the Vulva Azza Alyamani Department of







- Slides: 48
Diseases of the Vulva Azza Alyamani Department of Obstet. & Gynecol.
Vulvo-vaginal problems are among 10 leading disorders encountered by primary care clinicians. * Benign lesions of the vulva are mentioned in three categories : 1. Epithelial conditions. 2. Benign neoplastic disorders. 3. Dermatologic disorders. * VIN * Cancer vulva
Benign Conditions of the Vulva
(1) Epithelial Conditions 1) Lichen simplex. 2) Lichen sclerosis. 3) Lichen planus, erosive lichen planus.
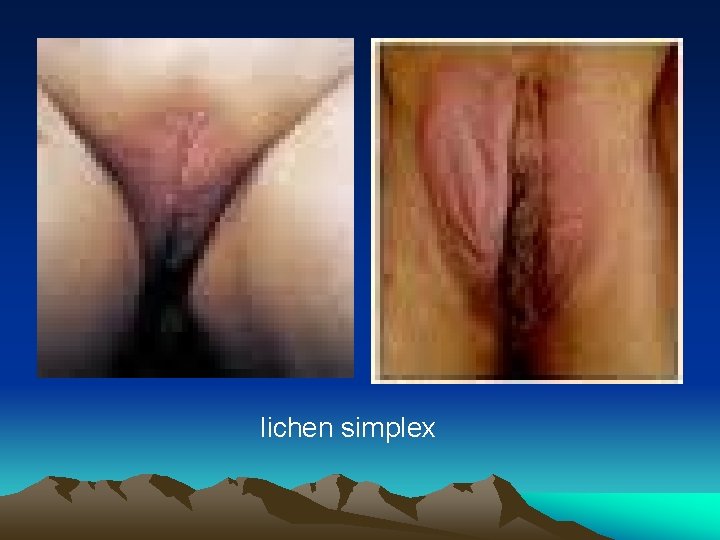
1) Lichen Simplex “ squamous cell hyperplasia “ * it is a local thickening of the epithelium resulting from a prolonged itching. * symptoms : pruritus and pain. * signs : white or reddish thickened , leathery , raised surface. usually discrete lesion but may be multiple. * treatment : • moderate-strength steroid ointment. • antipruritic agent.
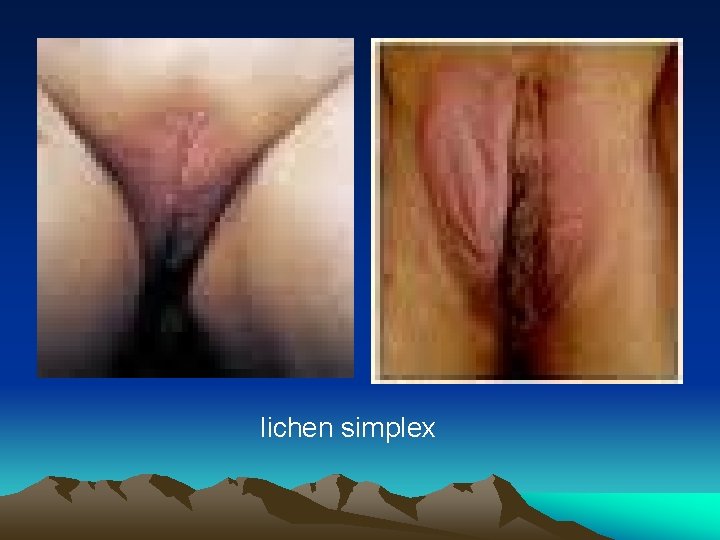
lichen simplex
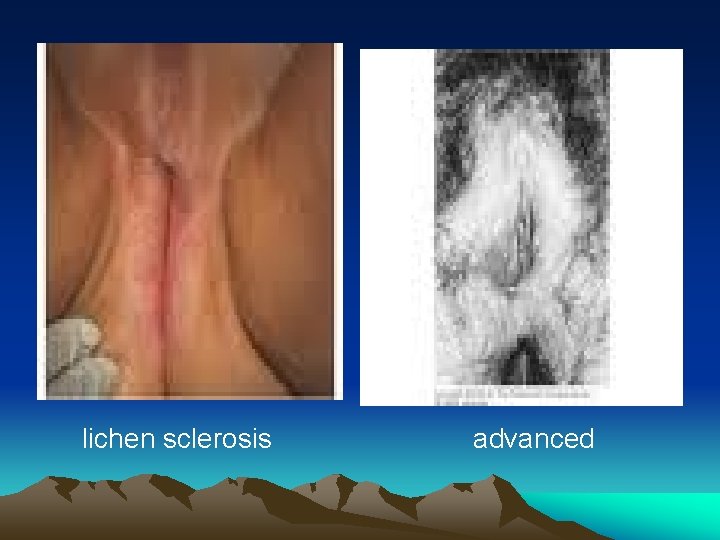
2) Lichen Sclerosis * it is a chronic progressive disease which constrict and destroy the normal genital anatomy. In the long term , labia minora are lost , labia majora flatten , clitoris becomes inverted. * frequently found on the vulva of postmenopausal women & can involve all the genital area from mons to the anal area.
* combinations of lichen sclerosis & epithleal hyperplasia or carcinoma are possible. * symptoms: intense pruritus , dyspareunia and burning pain. * signs: thin inelastic atrophic skin , white with a crinkled , tissue paper appearance.
* diagnosis: multiple biopsies is necessary. it reveals a thin atrophic epithelium with inflammatory cells lining the basement membrane. * treatment: ● potent topical steroids. 80% of lesions respond. long term therapy with low potent steroids may be necessary. ● other local treatments are: esrtogen cream and anaesthetics.
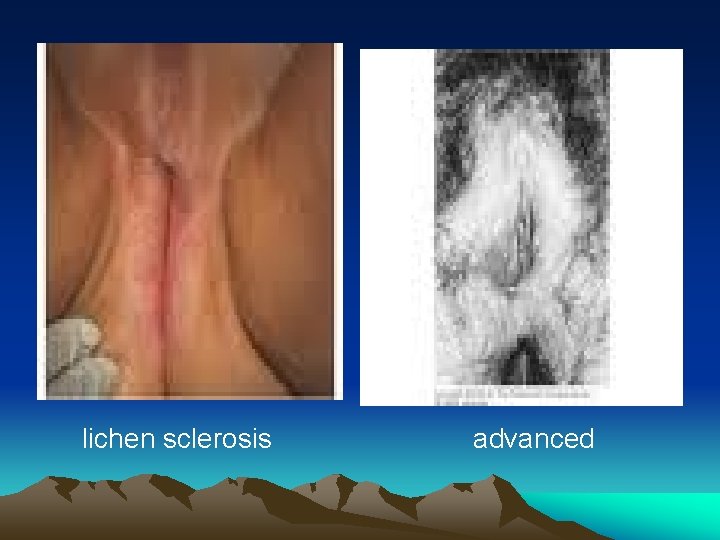
lichen sclerosis advanced
3) Lichen planus * it is a purplish , polygonal papules that may appear in their erosive form. * it involve the vulva , the vagina and the mouth ( vulval – vaginal –gingival syndrome ). * symptoms: vulval burning , severe dyspareunia when vaginal stenosis develop in advanced stages. * treatment: topical and systemic steroids.

erosive lichen planus of vulva & vagina lichen planus
(2) Benign Neoplastic condions 1) epidermal inclusion and sebaceous cysts. 2) vulvar varicosities. 3) fibromas and lipomas. 4) clitoromegaly.
1) epidermal inclusion & sebaceous cysts * they are nontender , mobile , spherical , slow growing cysts located below the epidermis. * sebaceous cysts are firmer bec. they are filled with dry caseous material. * treatment : most of inclusion cysts require no ttt. if they are asymptomatic, or surgical excision.
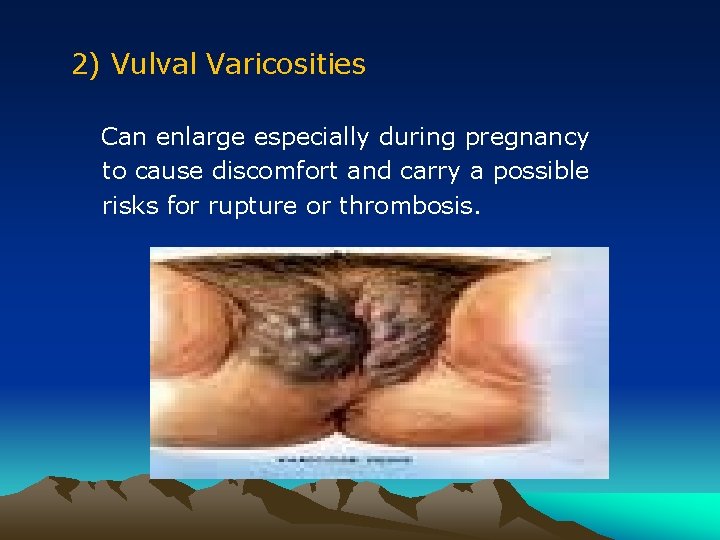
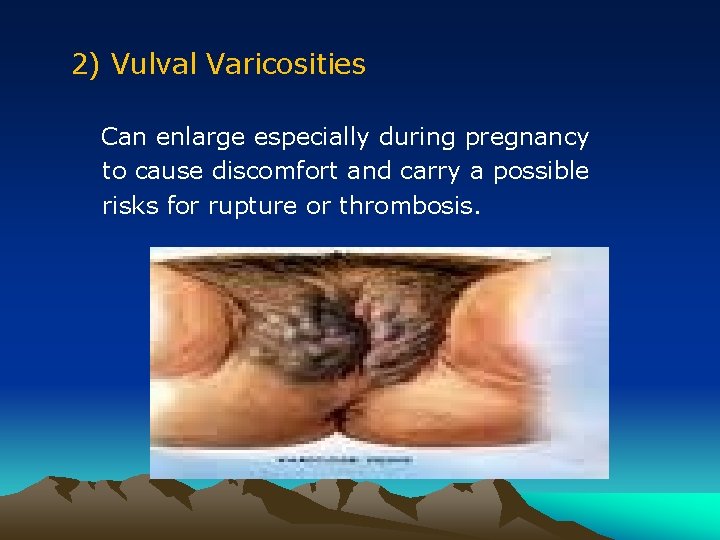
2) Vulval Varicosities Can enlarge especially during pregnancy to cause discomfort and carry a possible risks for rupture or thrombosis.
3) Fibromas and Lipomas Fibromas: * are the most common benign solid tumors that arise in the deeper connective tissue of the vulva. * they are slow growing 1– 10 cm in diameter, but may become huge. Lipomas: * slow growing tumors composed of adipose cells.
Vulval Fibroma
4) Clitoromegaly * may develop after birth in response to excessive androgen exposure. It is a sign virillization. * diagnosed when the clitorial length exceeds 30 mm or the width at the base exceeds 10 mm.

clitoromegaly
( 3) Dermatologic Disorders 1) Psoriasis. 2) Behcet ′s syndrome. 3) Crohn ΄s disease. 4) Acanthosis nigricans.
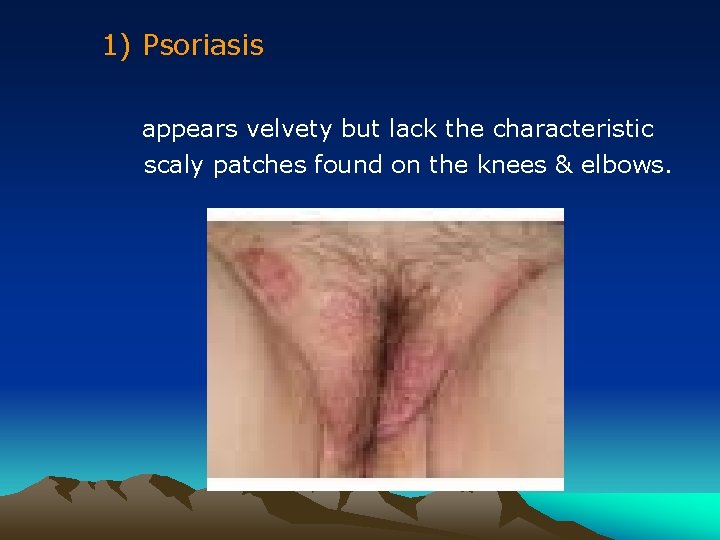
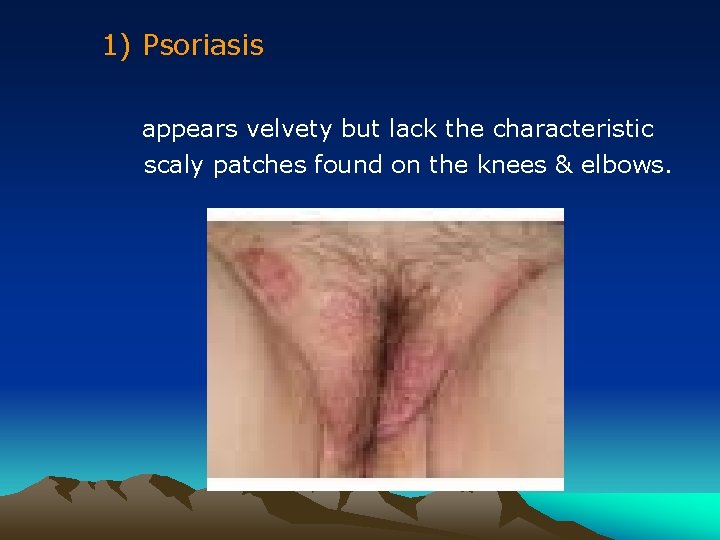
1) Psoriasis appears velvety but lack the characteristic scaly patches found on the knees & elbows.
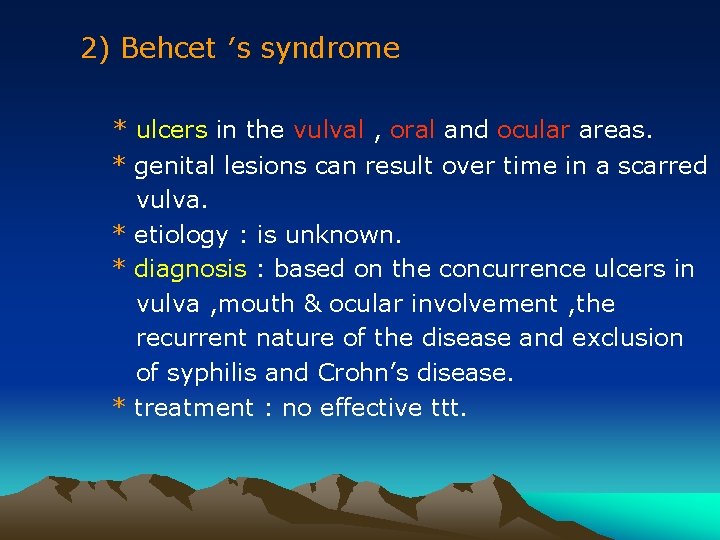
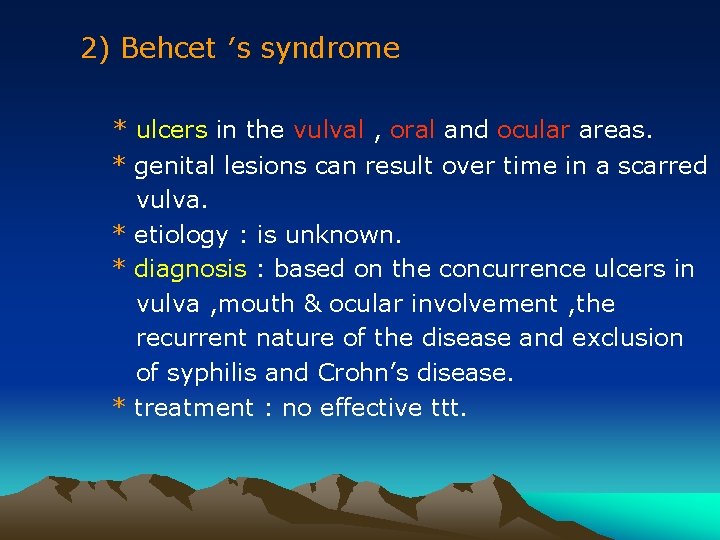
2) Behcet ′s syndrome * ulcers in the vulval , oral and ocular areas. * genital lesions can result over time in a scarred vulva. * etiology : is unknown. * diagnosis : based on the concurrence ulcers in vulva , mouth & ocular involvement , the recurrent nature of the disease and exclusion of syphilis and Crohn’s disease. * treatment : no effective ttt.

oral ulcer vulvar ulcer Behcet′ s disease
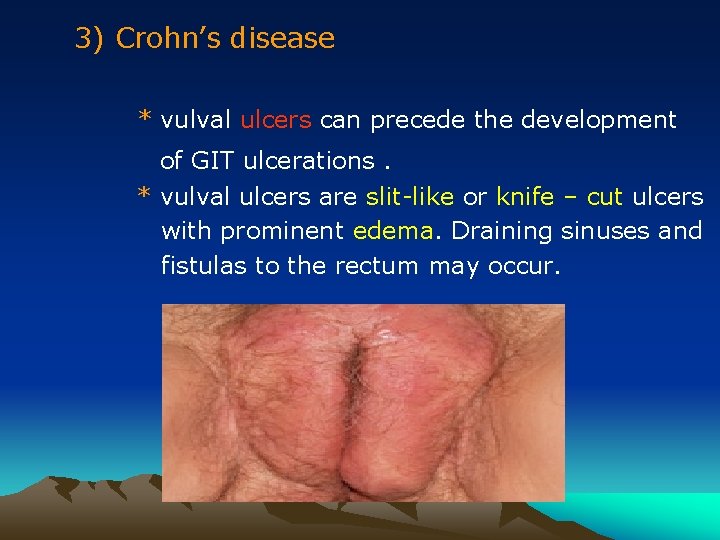
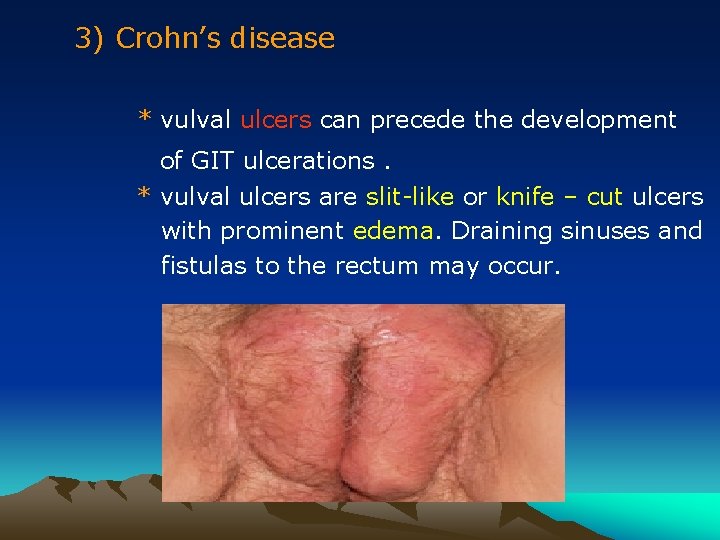
3) Crohn’s disease * vulval ulcers can precede the development of GIT ulcerations. * vulval ulcers are slit-like or knife – cut ulcers with prominent edema. Draining sinuses and fistulas to the rectum may occur.
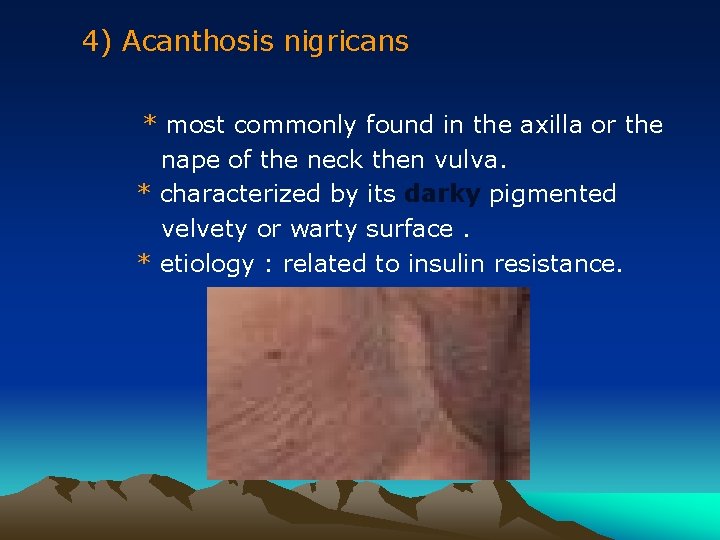
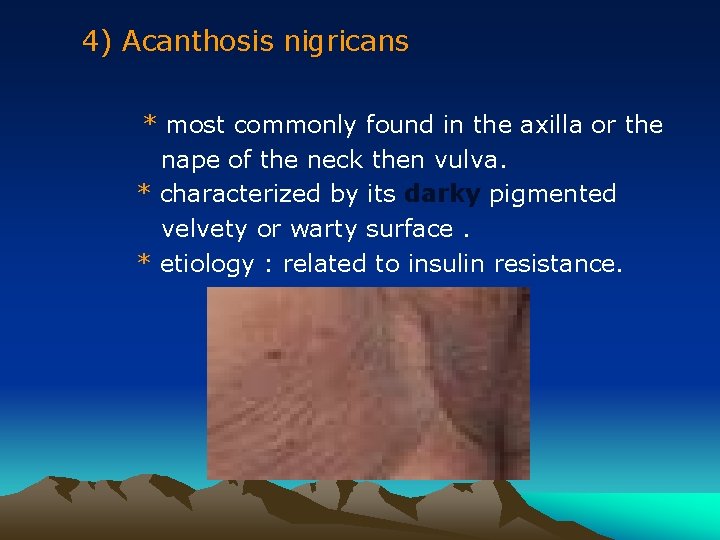
4) Acanthosis nigricans * most commonly found in the axilla or the nape of the neck then vulva. * characterized by its darky pigmented velvety or warty surface. * etiology : related to insulin resistance.
Vulval Neoplasms Introduction * uncommon 5 % of female genital tract malign. most tumors are squamous cell carcinomas , may be melanomas , adenocarcinomas and sarcomas. * postmenopausal women , mean age 65 years. * a history of chronic vulval itching is common.
Epidemiology Two different etiologic types of vulval cancers : 1. A less common type: * in younger women. * related to HPV infection and smoking. * commonly associated with VIN.
2. The more common type: * * in old women. unrelated to HPV infection or smoking. concurrent VIN is uncommon. long standing lichen sclerosis is common. 5% of patients have +ve serologic tests for syphilis , lymphogranuloma venereum and granuloma inguinale.
Vulval Intraepithelial Neoplasia (VIN) 2 types of VIN : 1. squamous cell carcinoma in situ VIN III or Bowen’s disease. 2. Adenocarcinoma in situ VIN III or Paget’s disease.
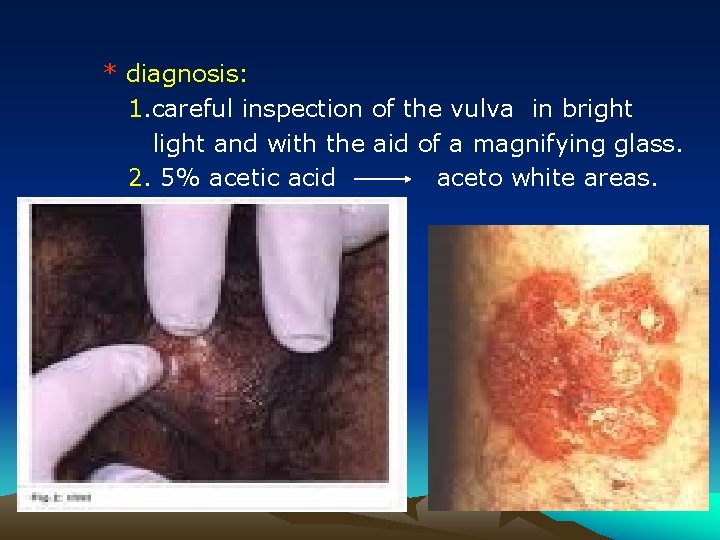
Squamous cell carcinoma in situ: VIN III ( Bowen′s disease ) * mean age 45 years. * symptoms: 50% asymptomatic. itching is the most common symptom. * signs: most lesions are elevated , white , red , pink , brown or grey in color. 20% of lesions are warty in appearance.
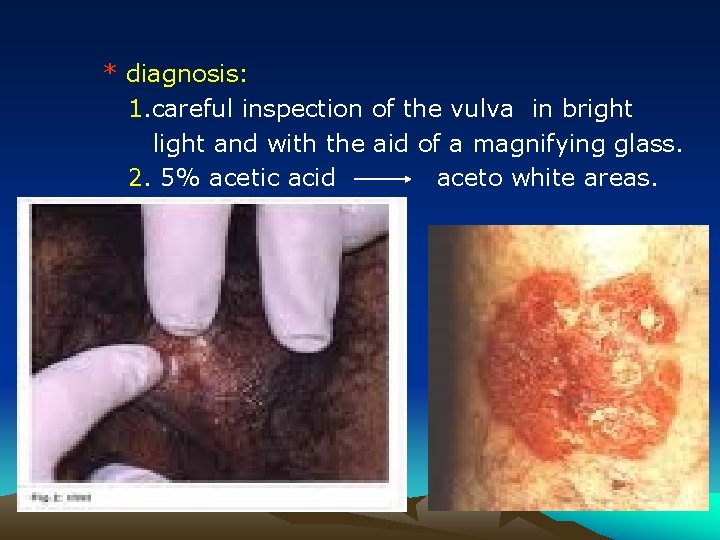
* diagnosis: 1. careful inspection of the vulva in bright light and with the aid of a magnifying glass. 2. 5% acetic acid aceto white areas.
* treatment : 1. local superficial excision. with margins of 5 mm are adequate. 2. skinning vulvectomy in extensive lesions. 3. laser therapy if lesions involves the clitoris , labia minora or perineal area.
Adenocarcinoma in situ VIN III ( Paget′ s disease ) * occurs in white postmenopausal elderly women. also occurs in the nipple area of the breast. * 20% is associated with adenocarcinoma. * symptoms: itching and tenderness are common. * signs: well demarcated and eczematus with white plaque like lesions. * growth may progresses beyond the vulva to the mons pubis , buttocks & thighs.
* diagnosis histologically: adenocarcinoma in situ characterized by large , pale , pathognomonic Paget’ s cells, typically located both in the epidermic and in the adnexal structures. * treatment: 1. local superficial excision. with margins 5 -10 mm. 2. laser therapy in recurrences which are common.

Paget′ s disease
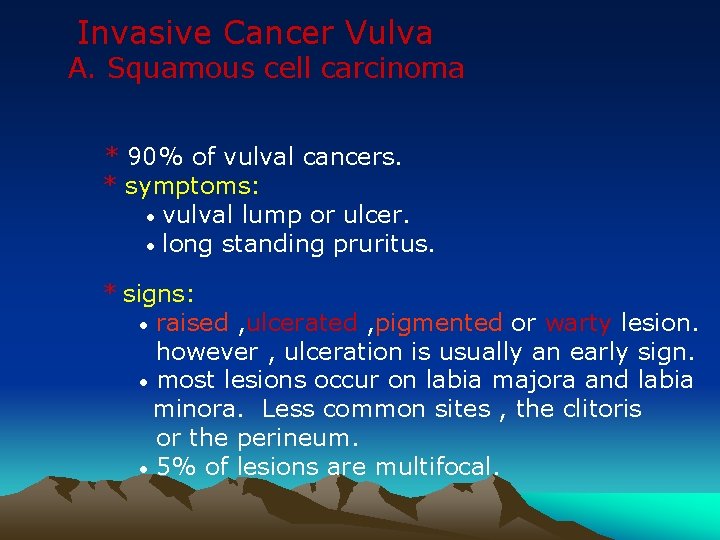
Invasive Cancer Vulva A. Squamous cell carcinoma * 90% of vulval cancers. * symptoms: • vulval lump or ulcer. • long standing pruritus. * signs: • raised , ulcerated , pigmented or warty lesion. however , ulceration is usually an early sign. • most lesions occur on labia majora and labia minora. Less common sites , the clitoris or the perineum. • 5% of lesions are multifocal.

squamous cell carcinoma of vulva
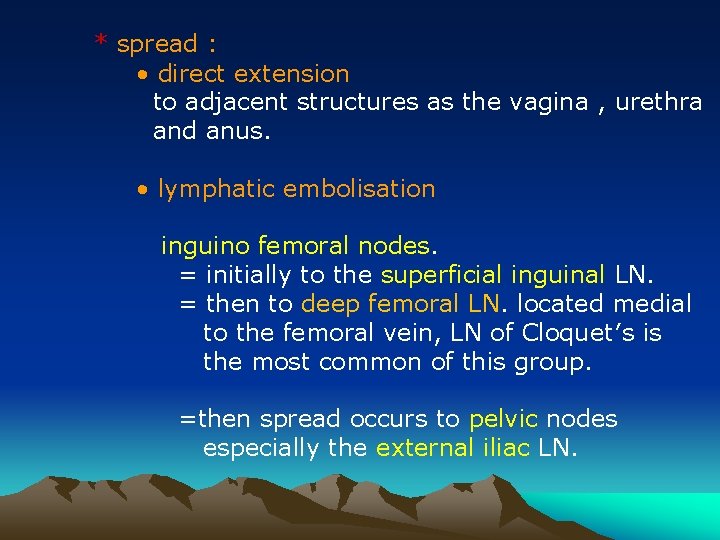
* spread : • direct extension to adjacent structures as the vagina , urethra and anus. • lymphatic embolisation inguino femoral nodes. = initially to the superficial inguinal LN. = then to deep femoral LN. located medial to the femoral vein, LN of Cloquet′s is the most common of this group. =then spread occurs to pelvic nodes especially the external iliac LN.
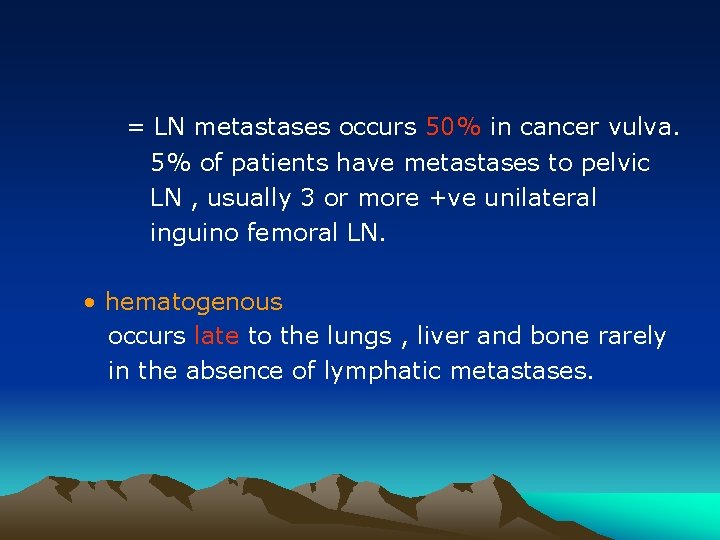
= LN metastases occurs 50% in cancer vulva. 5% of patients have metastases to pelvic LN , usually 3 or more +ve unilateral inguino femoral LN. • hematogenous occurs late to the lungs , liver and bone rarely in the absence of lymphatic metastases.
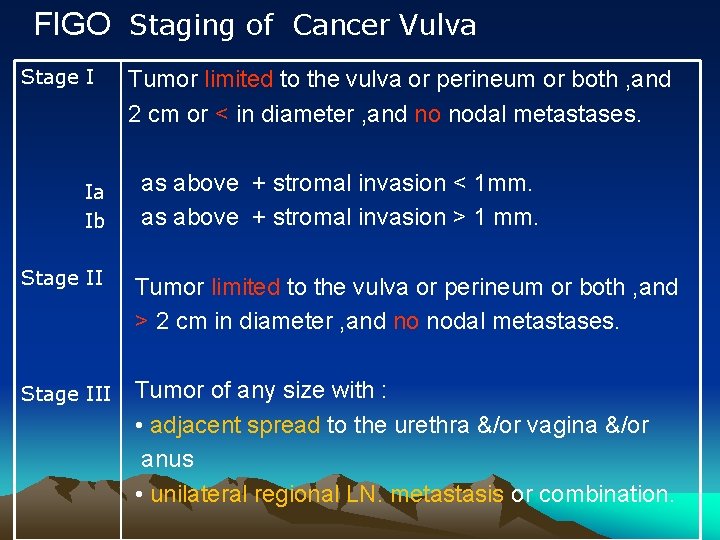
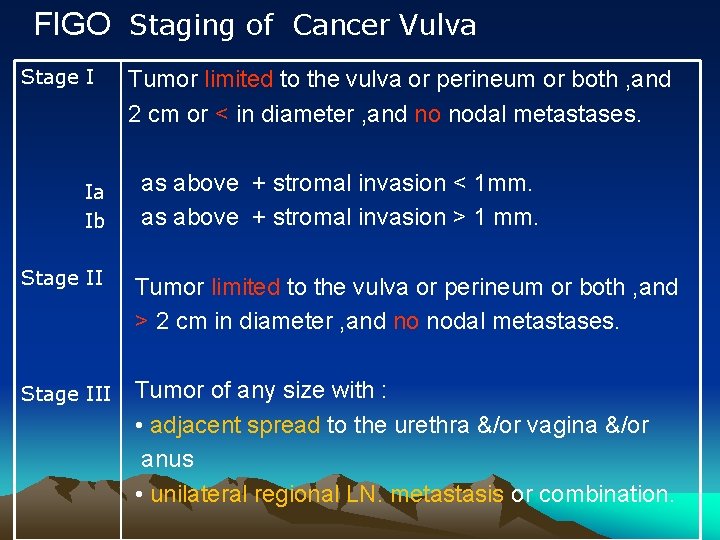
FIGO Staging of Cancer Vulva Stage I Ia Ib Tumor limited to the vulva or perineum or both , and 2 cm or < in diameter , and no nodal metastases. as above + stromal invasion < 1 mm. as above + stromal invasion > 1 mm. Stage II Tumor limited to the vulva or perineum or both , and > 2 cm in diameter , and no nodal metastases. Stage III Tumor of any size with : • adjacent spread to the urethra &/or vagina &/or anus • unilateral regional LN. metastasis or combination.
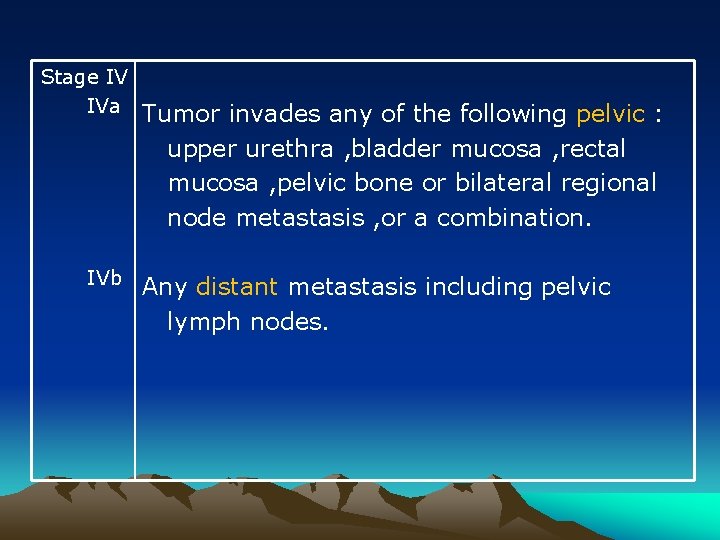
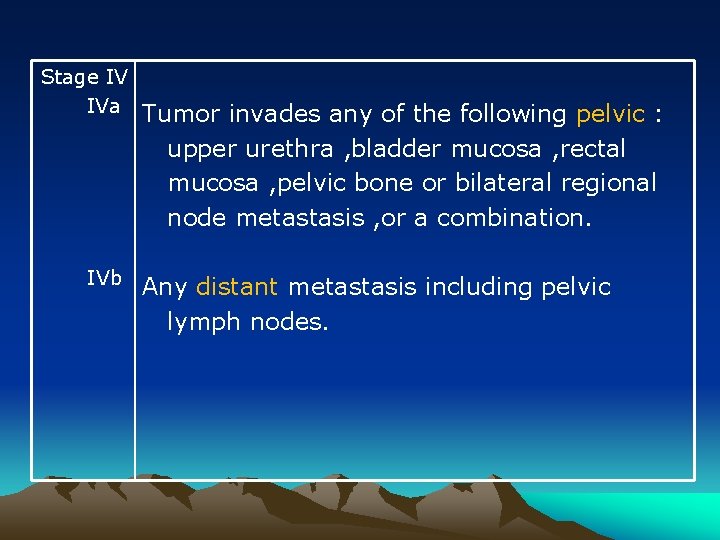
Stage IV IVa IVb Tumor invades any of the following pelvic : upper urethra , bladder mucosa , rectal mucosa , pelvic bone or bilateral regional node metastasis , or a combination. Any distant metastasis including pelvic lymph nodes.
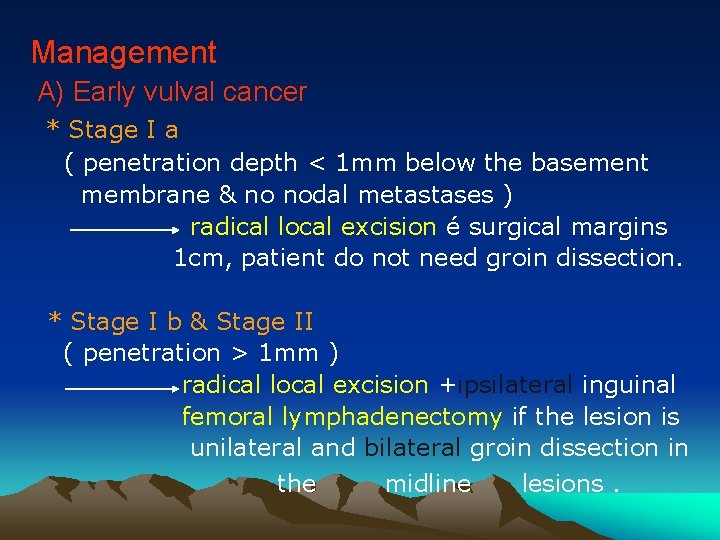
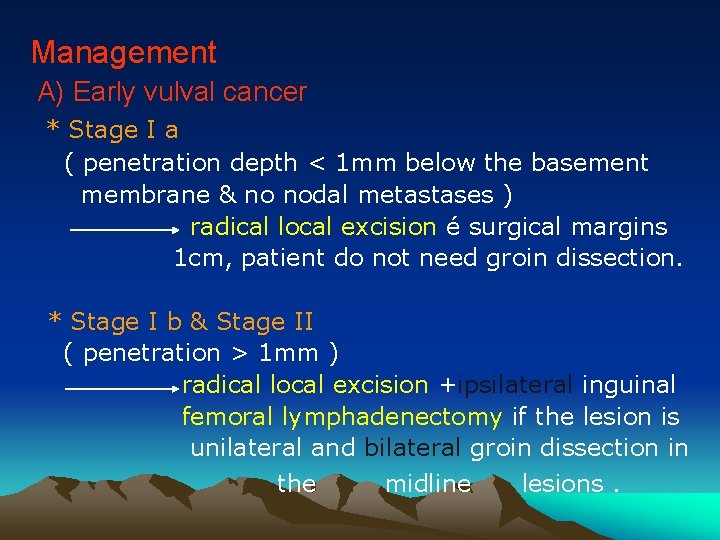
Management A) Early vulval cancer * Stage I a ( penetration depth < 1 mm below the basement membrane & no nodal metastases ) radical local excision é surgical margins 1 cm, patient do not need groin dissection. * Stage I b & Stage II ( penetration > 1 mm ) radical local excision +ipsilateral inguinal femoral lymphadenectomy if the lesion is unilateral and bilateral groin dissection in the midline lesions.
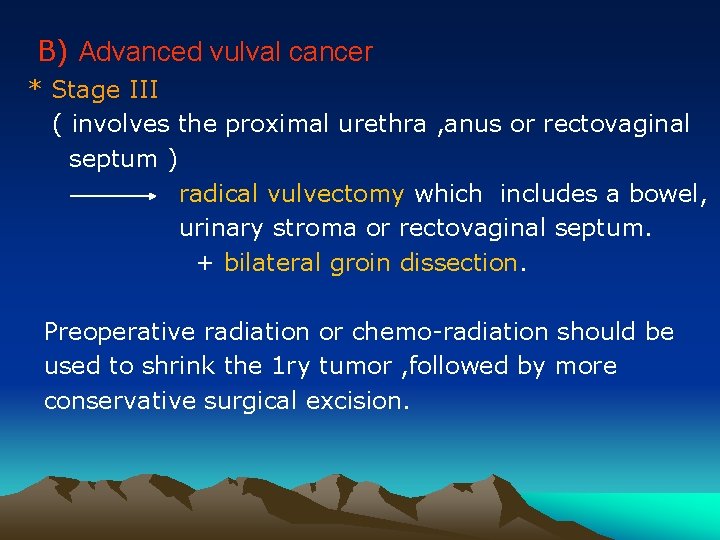
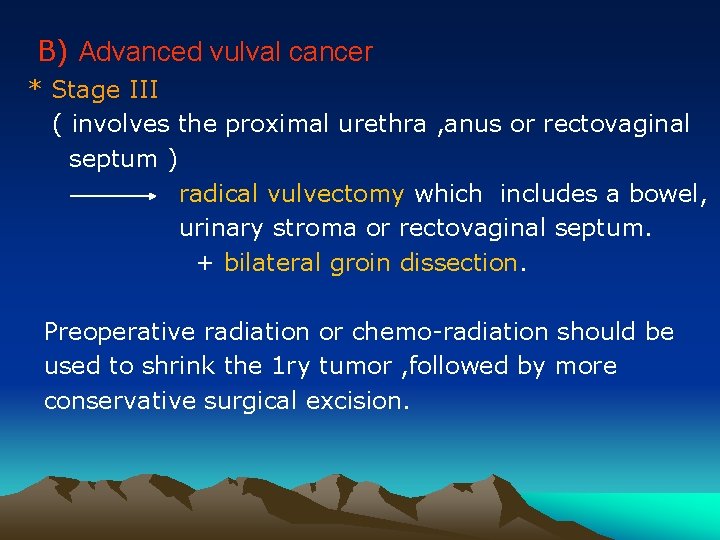
B) Advanced vulval cancer * Stage III ( involves the proximal urethra , anus or rectovaginal septum ) radical vulvectomy which includes a bowel, urinary stroma or rectovaginal septum. + bilateral groin dissection. Preoperative radiation or chemo-radiation should be used to shrink the 1 ry tumor , followed by more conservative surgical excision.
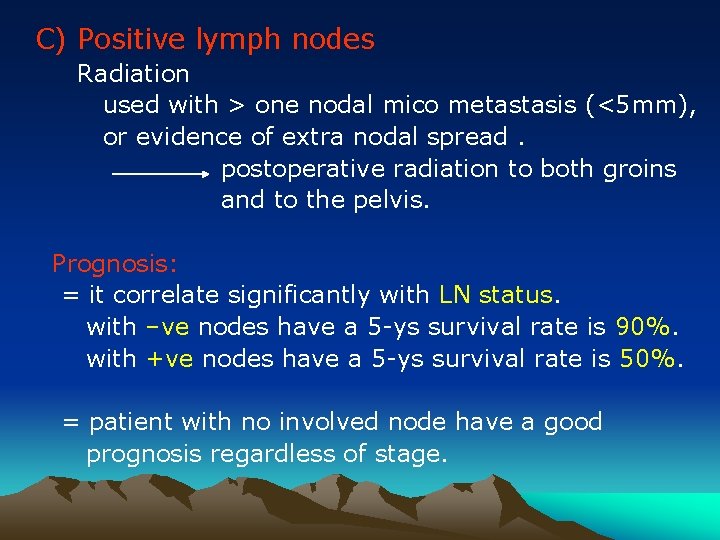
C) Positive lymph nodes Radiation used with > one nodal mico metastasis (<5 mm), or evidence of extra nodal spread. postoperative radiation to both groins and to the pelvis. Prognosis: = it correlate significantly with LN status. with –ve nodes have a 5 -ys survival rate is 90%. with +ve nodes have a 5 -ys survival rate is 50%. = patient with no involved node have a good prognosis regardless of stage.

Malignant Melanoma * the 2 nd most common vulvar cancer. * may arise de novo or from a preexisting nevus. commonly involve labia minora or clitoris. * occurs in postmenopausal white women. * diagnosis : any pigmented lesion of the vulva requires excisional biopsy for histopathology. * usually smaller lesions and tend to metastasized early.

malignant melanoma of the vulva
* prognosis: correlates to the depth of penetration into the dermis. The 5 -ys survival rate is 30%. * superficial lesion radical local excision alone with margins of 1 cm, is adequate. * deeper lesions 1 mm or > radical local excision + ipsilateral inguinal femoral lymphadenectomy. * adjuvant therapy: = nonspecific immuno stimulants. = chemotherapy. = vaccines.
Thank You
 Azza ouled zaid
Azza ouled zaid Azza spectra
Azza spectra S
S Lesiones vulvares benignas
Lesiones vulvares benignas Dr ashley fuller swedish
Dr ashley fuller swedish Que es una neoplasia
Que es una neoplasia Vulva
Vulva Cecilia gomez melendez
Cecilia gomez melendez Altura uterina normal
Altura uterina normal Innervation of ovary
Innervation of ovary Vulva
Vulva Vulva
Vulva Cortonen adalah
Cortonen adalah Kerozis
Kerozis Vulva
Vulva Vulva caracteristicas
Vulva caracteristicas Vulva
Vulva Lymphatic drainage of vulva
Lymphatic drainage of vulva Female body parts name in tamil with picture
Female body parts name in tamil with picture Anterior rhinoscopy structures
Anterior rhinoscopy structures Septo intercavernoso
Septo intercavernoso útero em anteversão
útero em anteversão Uterus avf position
Uterus avf position Eluryng
Eluryng Thơ thất ngôn tứ tuyệt đường luật
Thơ thất ngôn tứ tuyệt đường luật Các châu lục và đại dương trên thế giới
Các châu lục và đại dương trên thế giới Từ ngữ thể hiện lòng nhân hậu
Từ ngữ thể hiện lòng nhân hậu Diễn thế sinh thái là
Diễn thế sinh thái là Ví dụ giọng cùng tên
Ví dụ giọng cùng tên Vẽ hình chiếu vuông góc của vật thể sau
Vẽ hình chiếu vuông góc của vật thể sau Làm thế nào để 102-1=99
Làm thế nào để 102-1=99 Tỉ lệ cơ thể trẻ em
Tỉ lệ cơ thể trẻ em Hát lên người ơi
Hát lên người ơi Sự nuôi và dạy con của hươu
Sự nuôi và dạy con của hươu Lời thề hippocrates
Lời thề hippocrates đại từ thay thế
đại từ thay thế Quá trình desamine hóa có thể tạo ra
Quá trình desamine hóa có thể tạo ra Công thức tiính động năng
Công thức tiính động năng Hát kết hợp bộ gõ cơ thể
Hát kết hợp bộ gõ cơ thể Thế nào là mạng điện lắp đặt kiểu nổi
Thế nào là mạng điện lắp đặt kiểu nổi Dạng đột biến một nhiễm là
Dạng đột biến một nhiễm là Vẽ hình chiếu đứng bằng cạnh của vật thể
Vẽ hình chiếu đứng bằng cạnh của vật thể Phản ứng thế ankan
Phản ứng thế ankan Voi kéo gỗ như thế nào
Voi kéo gỗ như thế nào Môn thể thao bắt đầu bằng chữ đua
Môn thể thao bắt đầu bằng chữ đua Khi nào hổ mẹ dạy hổ con săn mồi
Khi nào hổ mẹ dạy hổ con săn mồi Thiếu nhi thế giới liên hoan
Thiếu nhi thế giới liên hoan điện thế nghỉ
điện thế nghỉ Một số thể thơ truyền thống
Một số thể thơ truyền thống