Clinical aspects of wound healing Module 1 Principles

- Slides: 13
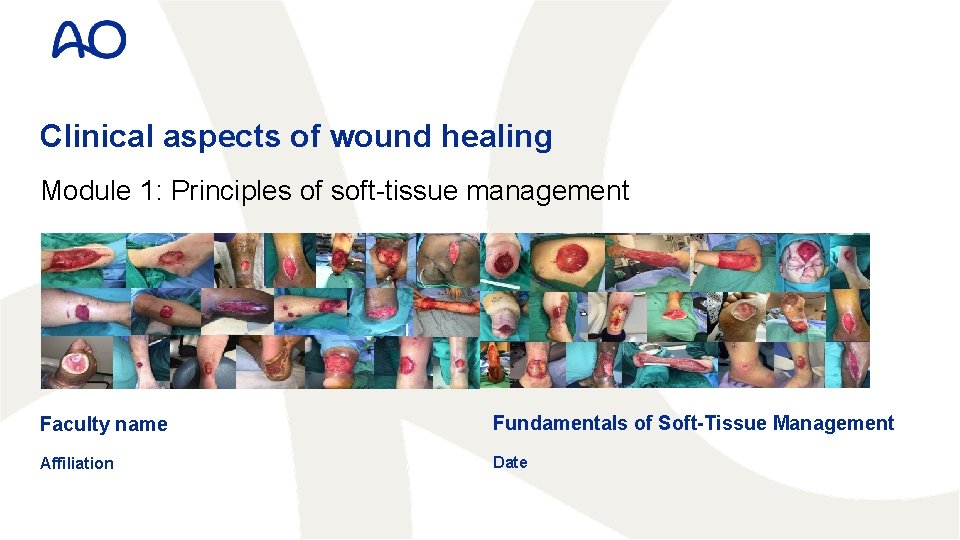
Clinical aspects of wound healing Module 1: Principles of soft-tissue management Faculty name Fundamentals of Soft-Tissue Management Affiliation Date
Disclosures I have no financial relationships with commercial entities that produce health-care related products. OR The commercial entities with which I have a financial relationship do not produce health-care related products or services relevant to the content of my presentation. OR I disclose the following financial relationships with commercial entities that produce health-care related products or services: Consultant for: Advisory Board for: Employee of: Grant/Research support from: Honoraria from: Stockholder in: Speaker/teacher for: 2
Learning objectives • Describe wound healing phases and tensile strength • Describe the vascular anatomy of fascia, subcutaneous tissue & skin • Recognize the value of tissue approximation & reducing dead-space • Apply this knowledge to design and execute wound closure 4

From wound to scar Wounds Sutures Scars 5
Surgical wound classification Class I: Clean 6 Uninfected wounds without inflammation e. g. Operative incisional wounds that follow non-penetrating (blunt) trauma
Surgical wound classification Class I: Clean Class II: Clean contaminated 7 Uninfected wounds without inflammation e. g. Operative incisional wounds that follow non-penetrating (blunt) trauma No unusual wound contamination e. g. Surgery without evidence of infection or major break in sterile technique
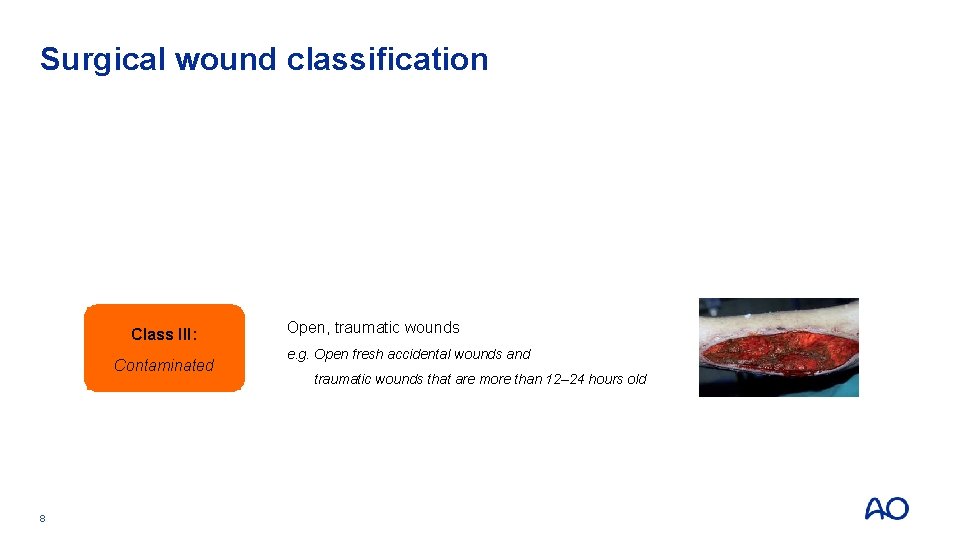
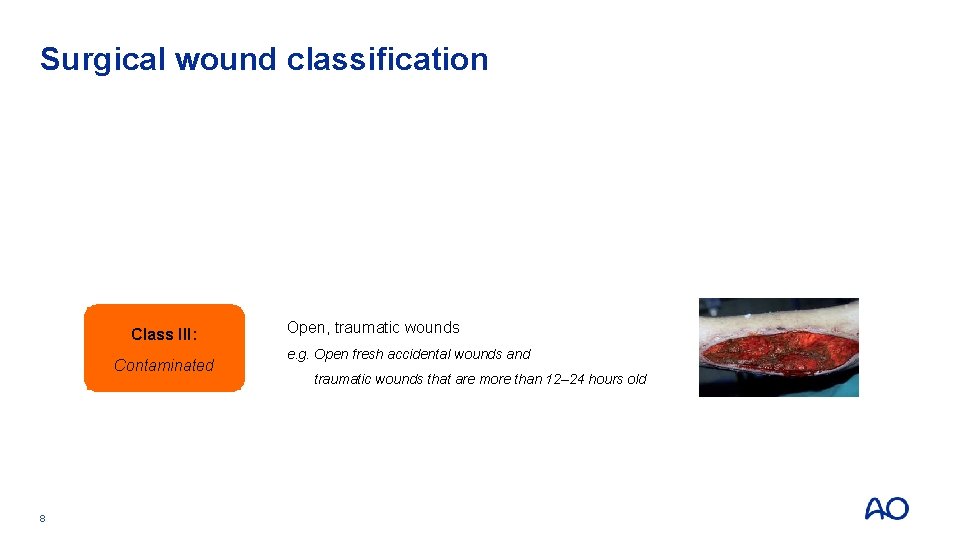
Surgical wound classification Class I: Clean Class II: Clean contaminated Class III: Contaminated 8 Uninfected wounds without inflammation e. g. Operative incisional wounds that follow non-penetrating (blunt) trauma No unusual wound contamination e. g. Surgery without evidence of infection or major break in sterile technique Open, traumatic wounds e. g. Open fresh accidental wounds and traumatic wounds that are more than 12– 24 hours old
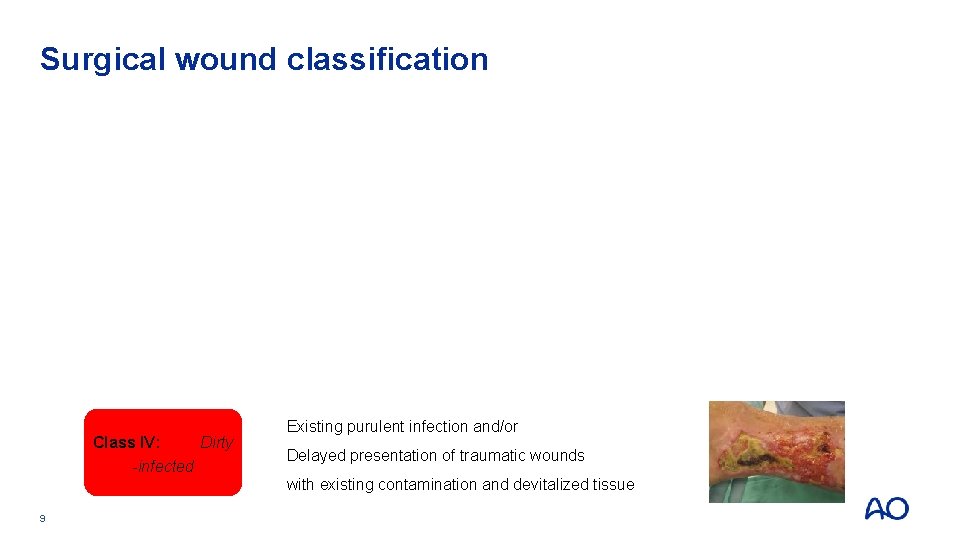
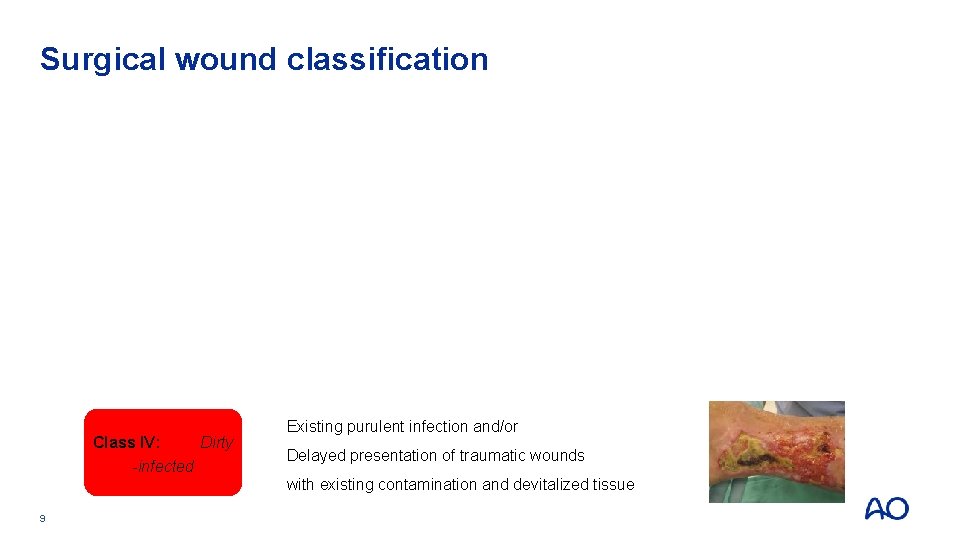
Surgical wound classification Class I: Clean Class II: Clean contaminated Class III: Contaminated Class IV: Dirty -infected Uninfected wounds without inflammation e. g. Operative incisional wounds that follow non-penetrating (blunt) trauma No unusual wound contamination e. g. Surgery without evidence of infection or major break in sterile technique Open, traumatic wounds e. g. Open fresh accidental wounds and traumatic wounds that are more than 12– 24 hours old Existing purulent infection and/or Delayed presentation of traumatic wounds with existing contamination and devitalized tissue 9
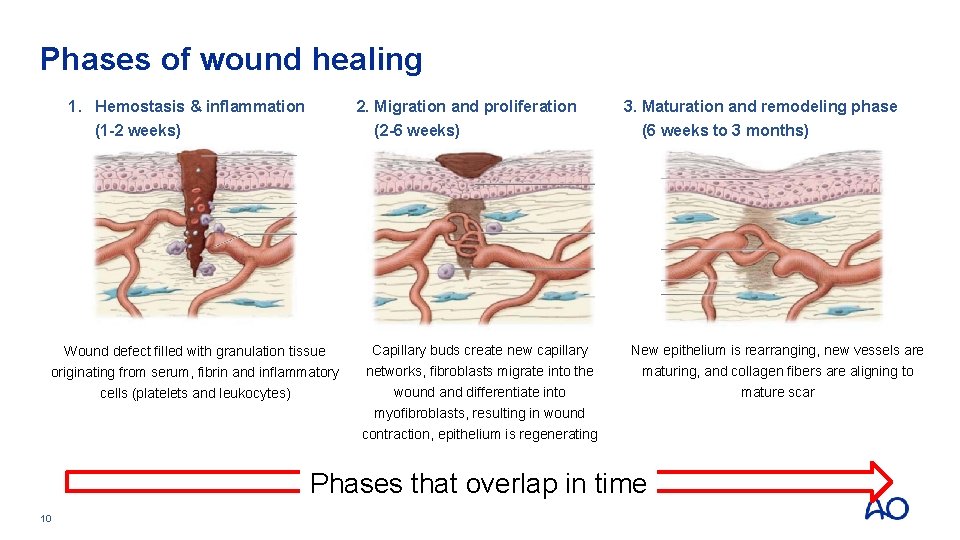
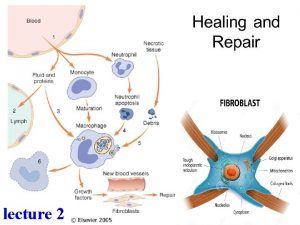
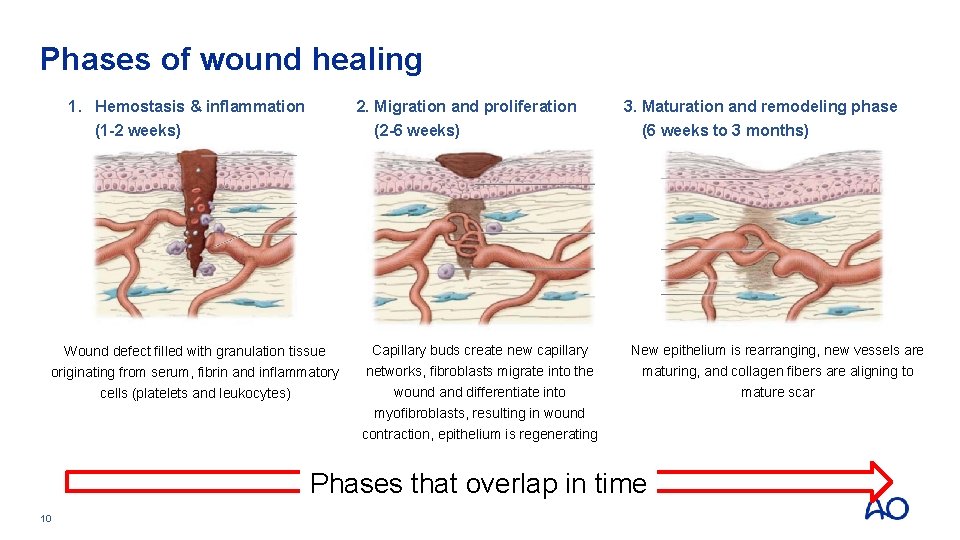
Phases of wound healing 1. Hemostasis & inflammation (1 -2 weeks) 2. Migration and proliferation (2 -6 weeks) 3. Maturation and remodeling phase (6 weeks to 3 months) Wound defect filled with granulation tissue Capillary buds create new capillary New epithelium is rearranging, new vessels are originating from serum, fibrin and inflammatory cells (platelets and leukocytes) networks, fibroblasts migrate into the wound and differentiate into myofibroblasts, resulting in wound contraction, epithelium is regenerating maturing, and collagen fibers are aligning to mature scar Phases that overlap in time 10
Wound healing depends on patient factors • Systemic factors: • Gender, age, diseases (CAOD, vasculitis, diabetes, …), drugs (NSAID, steroids, cytostatic drugs, …), nutrition, smoking, … • Local factors: • Mechanism of injury, hematoma, seroma, infection, tissue viability, irradiated local tissues, … 11
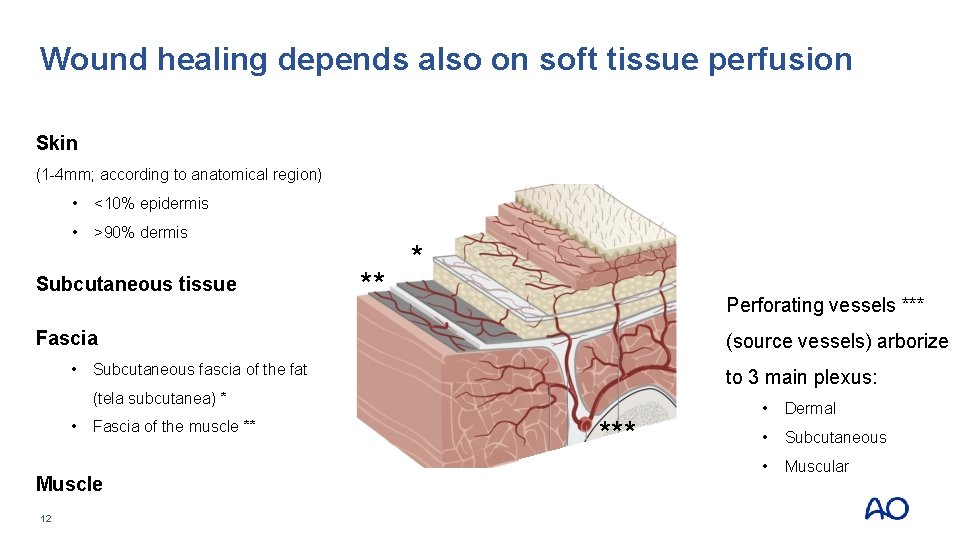
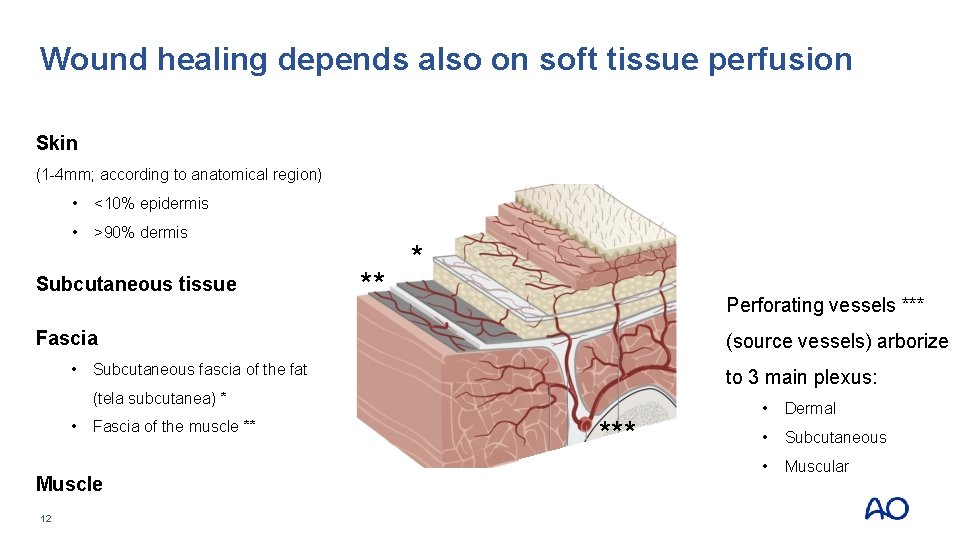
Wound healing depends also on soft tissue perfusion Skin (1 -4 mm; according to anatomical region) • <10% epidermis • >90% dermis Subcutaneous tissue ** * Perforating vessels *** Fascia (source vessels) arborize • Subcutaneous fascia of the fat to 3 main plexus: (tela subcutanea) * • Fascia of the muscle ** Muscle 12 *** • Dermal • Subcutaneous • Muscular
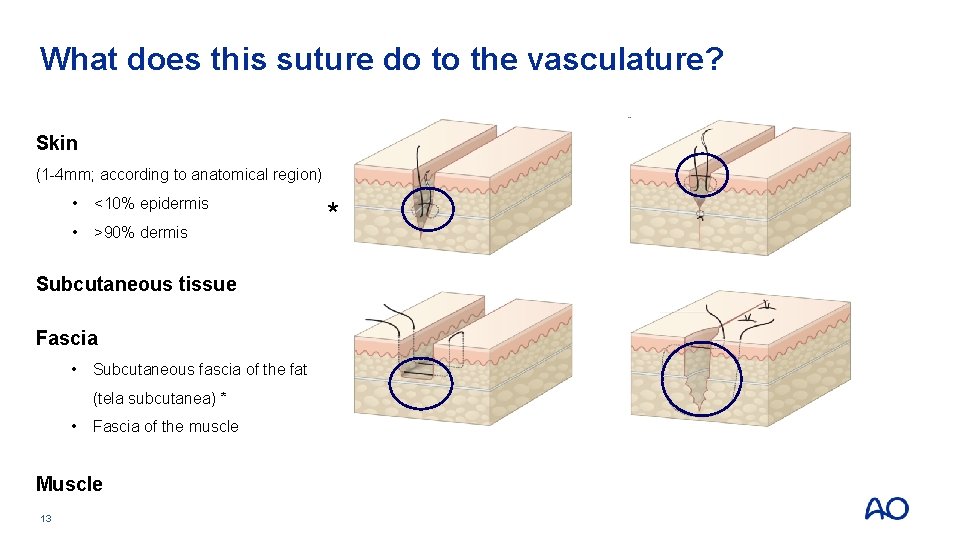
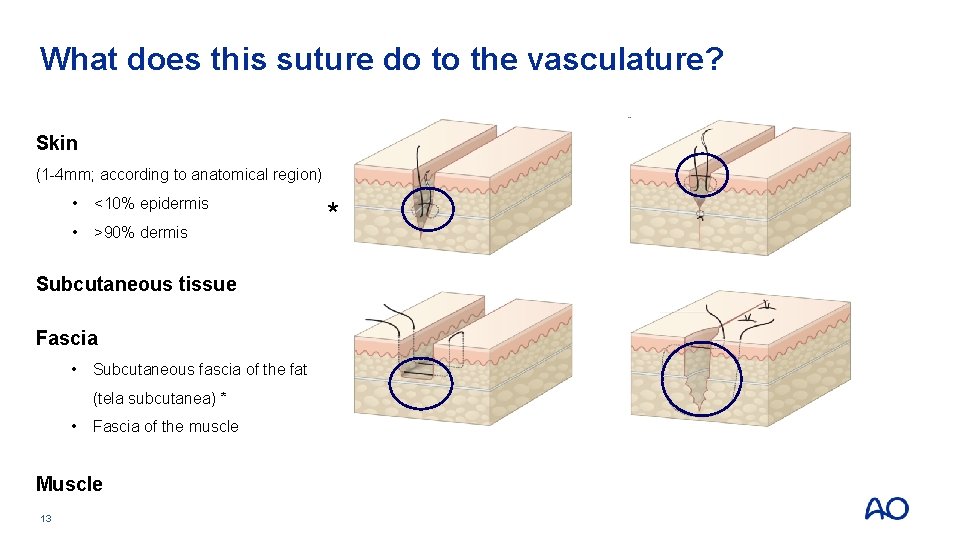
What does this suture do to the vasculature? Skin (1 -4 mm; according to anatomical region) • <10% epidermis • >90% dermis Subcutaneous tissue Fascia • Subcutaneous fascia of the fat (tela subcutanea) * • Fascia of the muscle Muscle 13 *
Take home messages • Systematic wound characterization needed to define treatment • Wound closure matters!!! • Turn a traumatic wound in a surgical wound • Exploit collagen rich tissues for suture repair • Fascia of the muscle, deep fascia of the fat (tela subcutanea), dermis • Approximate epidermis to restore barrier 14
 Systemic factors affecting wound healing
Systemic factors affecting wound healing Wound healing nutrition handout
Wound healing nutrition handout Inflammation fever
Inflammation fever Rank wakefield classification
Rank wakefield classification Factors affecting wound healing ppt
Factors affecting wound healing ppt Gaping earrings puncture
Gaping earrings puncture Primary union wound healing
Primary union wound healing C device module module 1
C device module module 1 What is quantum healing
What is quantum healing Whakatauki about healing
Whakatauki about healing Perkins formula fracture healing
Perkins formula fracture healing Ebers papyrus
Ebers papyrus Marumali
Marumali Male
Male