CHILD HEALTH STRATEGY RCH IINRHM National goals MDG







- Slides: 35

CHILD HEALTH STRATEGY RCH II/NRHM
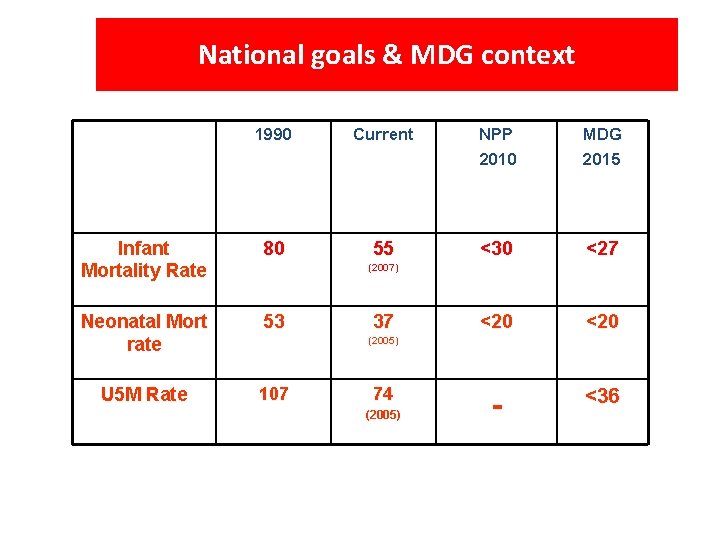
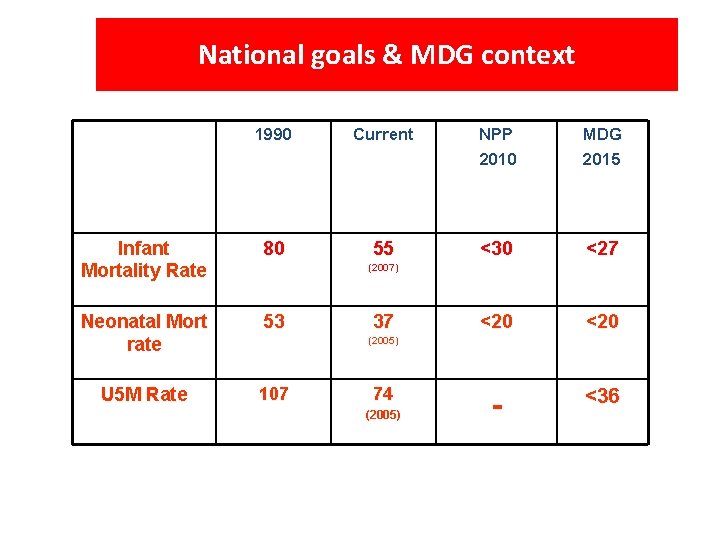
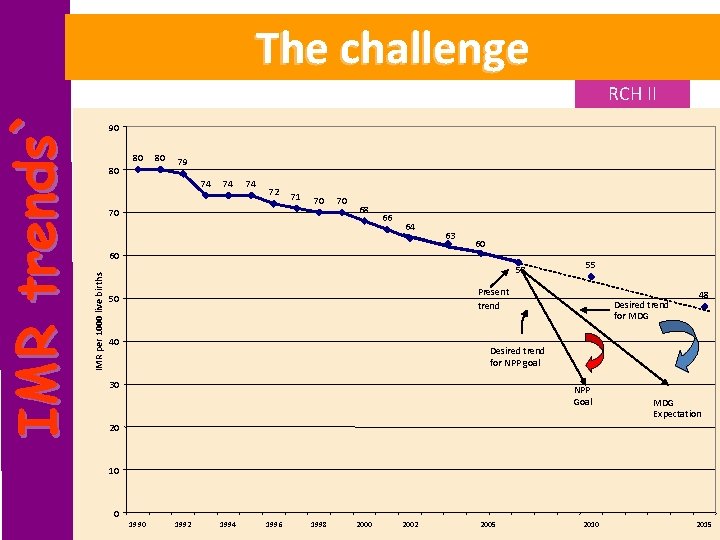
National goals & MDG context 1990 Current NPP 2010 MDG 2015 Infant Mortality Rate 80 55 <30 <27 Neonatal Mort rate 53 <20 U 5 M Rate 107 - <36 (2007) 37 (2005) 74 (2005)
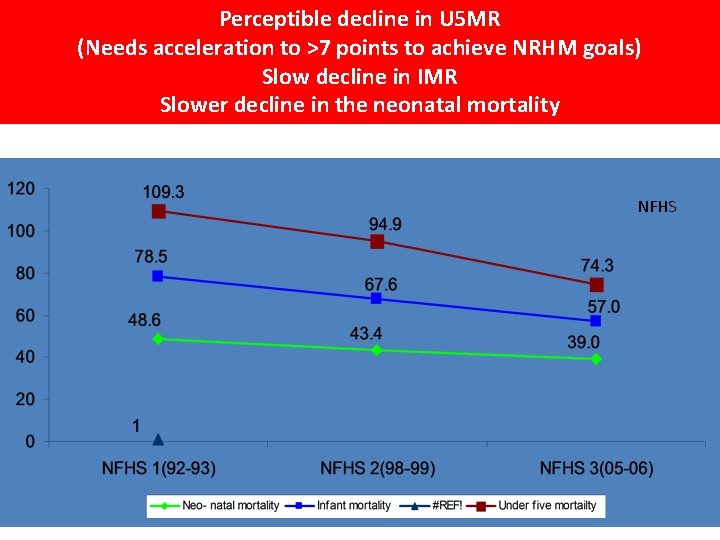
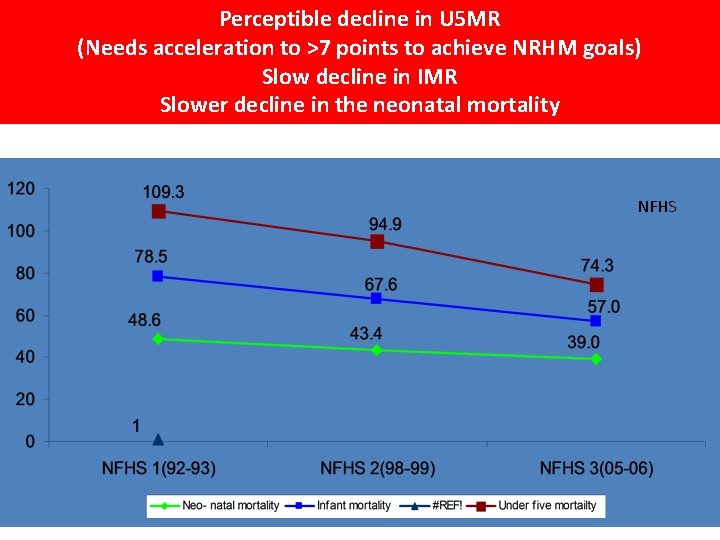
Perceptible decline in U 5 MR (Needs acceleration to >7 points to achieve NRHM goals) Slow decline in IMR Slower decline in the neonatal mortality NFHS
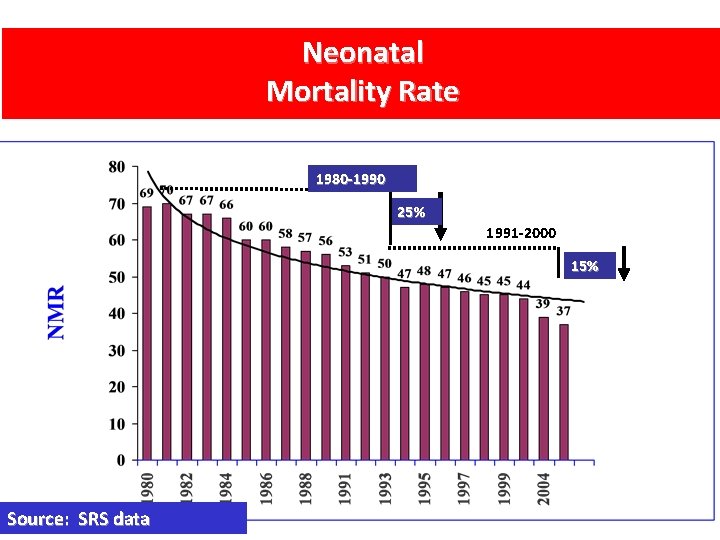
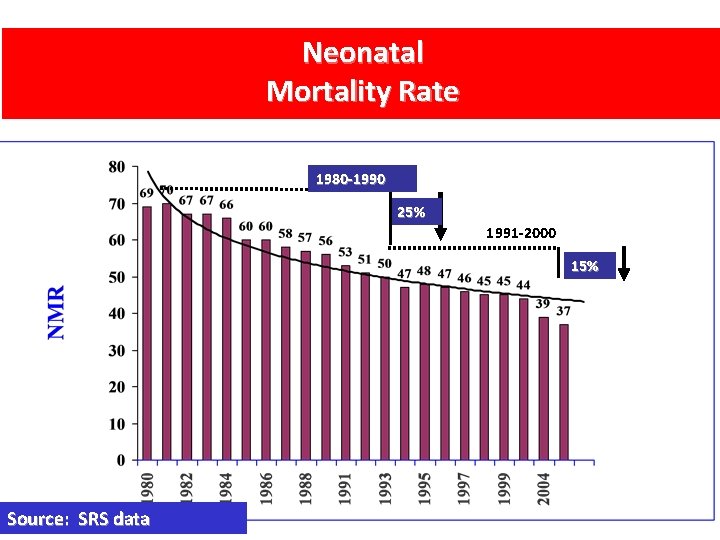
Neonatal Mortality Rate 1980 -1990 25% 1991 -2000 15% Source: SRS data
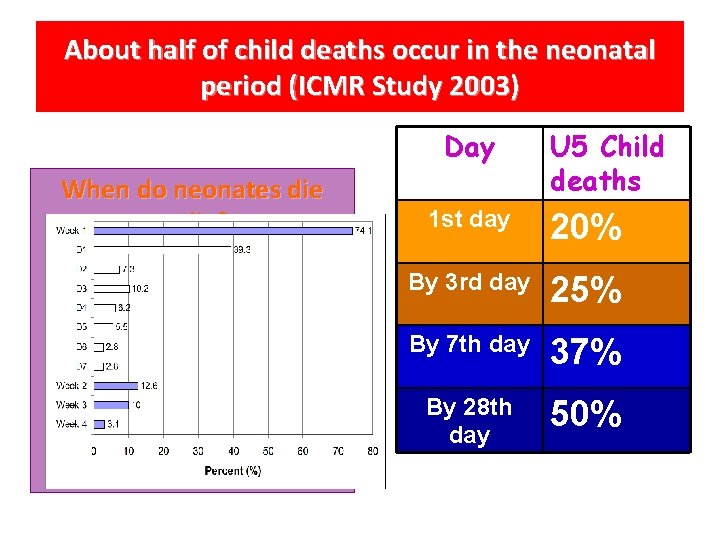
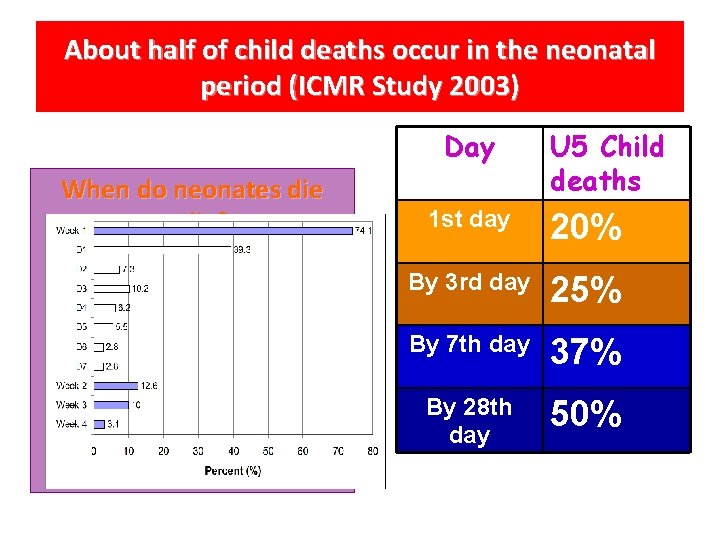
About half of child deaths occur in the neonatal period (ICMR Study 2003) Day When do neonates die? U 5 Child deaths 1 st day 20% By 3 rd day 25% By 7 th day 37% By 28 th day 50%
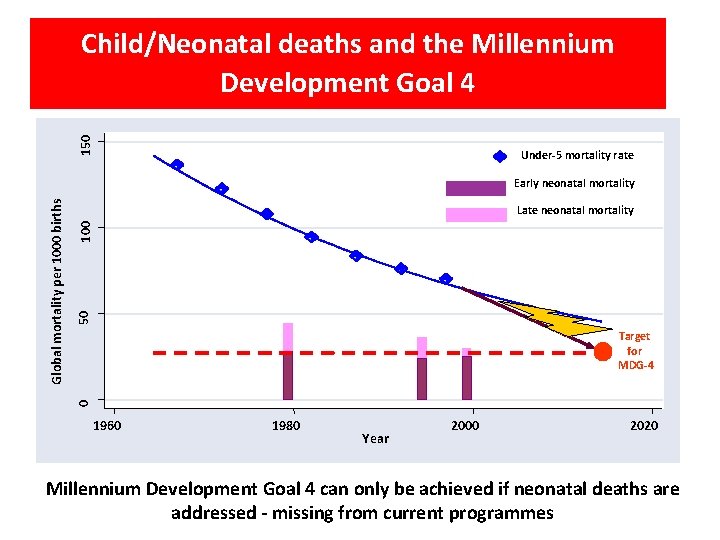
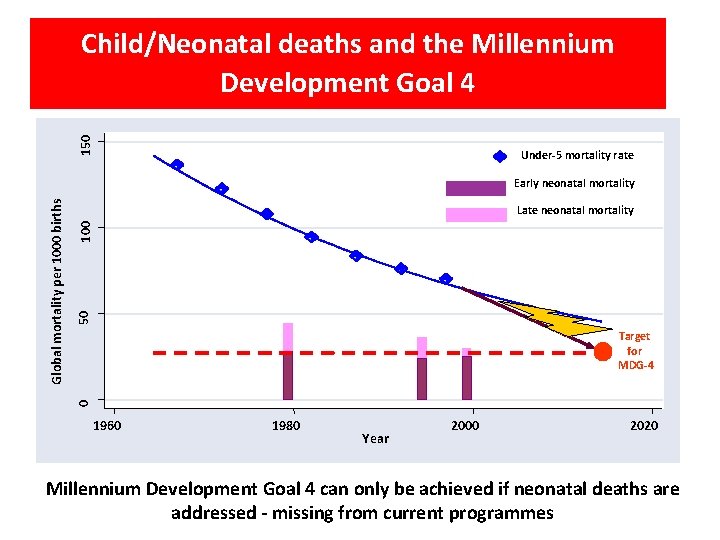
150 Child/Neonatal deaths and the Millennium Development Goal 4 Under-5 mortality rate 50 100 Late neonatal mortality Target for MDG-4 0 Global mortality per 1000 births Early neonatal mortality 1960 1980 Year 2000 2020 Millennium Development Goal 4 can only be achieved if neonatal deaths are addressed - missing from current programmes
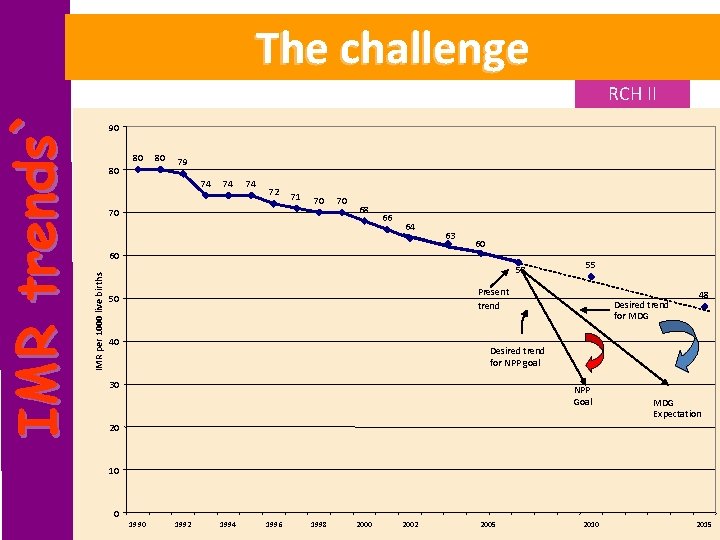
RCH II 90 80 80 80 79 74 74 74 72 71 70 70 70 68 66 64 63 60 60 IMR per 1000 live births IM R trends` The challenge 58 55 Present trend 50 40 Desired trend for MDG 48 Desired trend for NPP goal 30 NPP Goal MDG Expectation 20 10 0 1992 1994 1996 1998 2000 2002 2005 2010 2015

State-wise burden of neonatal deaths TN As Hr UP Pb Kn WB Gj Or MP Mh AP Rj Bi Estimation based on data from National Human Development Report 20017 & SRS 2001
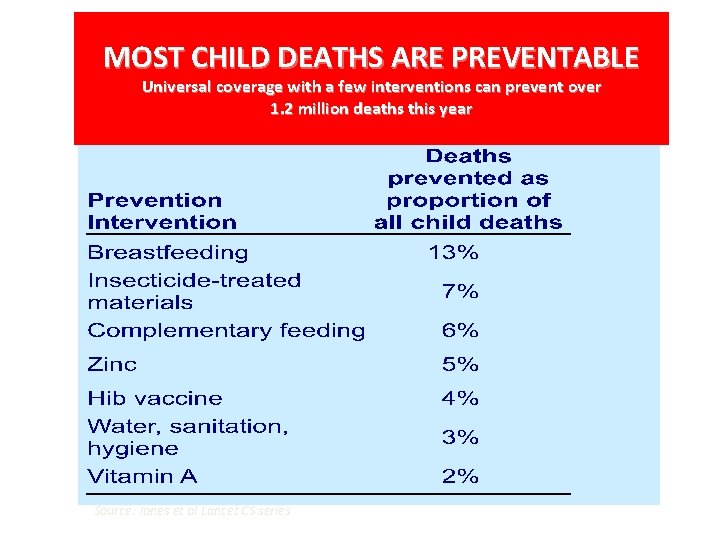
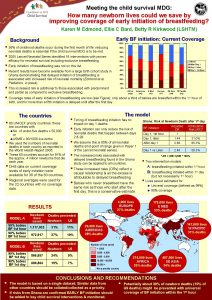
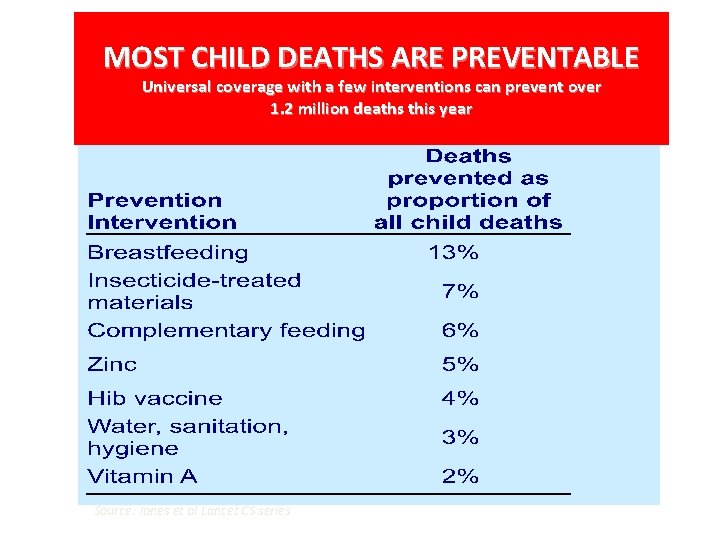
MOST CHILD DEATHS ARE PREVENTABLE Universal coverage with a few interventions can prevent over 1. 2 million deaths this year Source: Jones et al Lancet CS series

MOST CHILD DEATHS ARE PREVENTABLE Universal coverage with a few interventions can prevent over 1. 2 million deaths this year Source: Jones et al Lancet CS series

New Born & Child Health Key Strategies 1. Increase coverage of skilled care at birth for newborns in conjunction with maternal care 2. Implement, by 2010, a newborn and child health package of preventive, promotive and curative interventions using a comprehensive IMNCI approach
New Born & Child Health Key Strategies under RCH II/NRHM 3. Strengthen and augment existing services (care at birth/Essential New born /care, ARI and diarrhea control) in areas where IMNCI is yet to be implemented. 4. Implement the multi year strategic plan for the UIP (Universal Immunization Program)
CHILD HEALTH INTERVENTIONS • Essential new born Care • Integrated management of neonatal and Child hood Illness • Exclusive Breast Feeding and Timely introduction of complimentary Feeding • Immunization
CHILD HEALTH INTERVENTIONS • Vitamin A and Iron and folic acid supplementation • Early detection and management of ARI/ diarrhoea and other infections • referral care • pre service training
CHILD HEALTH Interventions Essential New born Care • Initiation of early breast feeding. • Rooming/ keeping baby warm • Resuscitation. • Infection prevention • Immunization
CHILD HEALTH Interventions- Breast Feeding • Early Initiation • Excusive feeding till 6 months • Starting Complementary feeding at 6 months
CHILD HEALTH Interventions - Diarrhoeal disease • Increase ORS Use rate /addition of Zinc • Prevention of diarrhea (Safe Water, Contd. feeding) • Rational drug usage
CHILD HEALTH Interventions - ARI Management • Early recognition of fast breathing • Cotrimoxazole administration for Pneumonia • Rational drug usage
CHILD HEALTH Interventions - Immunizations • Complete Immunization schedule in first year • Supplementation of Vitamin A and Iron
CHILD HEALTH Interventions – Integrated Management of Neonatal and childhood Illness • Appropriate care of sick new born and sick child. • Recognition of Danger Signs • Counseling on Breast Feeding and Nutrition
CHILD HEALTH Interventions – Referral / Facility Care • Care of Sick New born /Child • Emergency Assessment /Care. • Management of Malnutrition. Pilot in MP
Interventions – Home Based Care • Care of Sick New born at Home • Based on Gadchiroli Model. • Pilot in UP, Bihar, Orissa, Rajasthan and MP
Child health Indicators 1. Infant Mortality Rate/Under five mortality Rate. 2. % of children visited within 24 hrs of and on 3 rd and the 7 th day of delivery by a trained provider. 3. % of children who were breast fed within 1 hr of delivery and exclusively for 6 months. 4. % of children fully immunized.
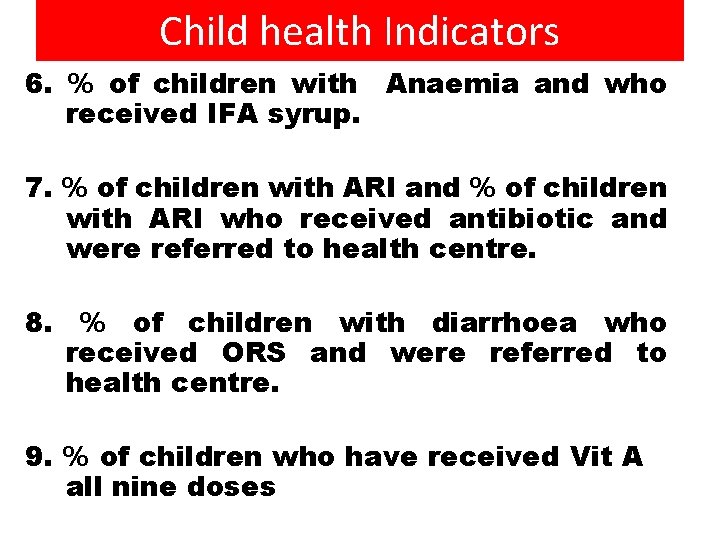
Child health Indicators 6. % of children with Anaemia and who received IFA syrup. 7. % of children with ARI and % of children with ARI who received antibiotic and were referred to health centre. 8. % of children with diarrhoea who received ORS and were referred to health centre. 9. % of children who have received Vit A all nine doses
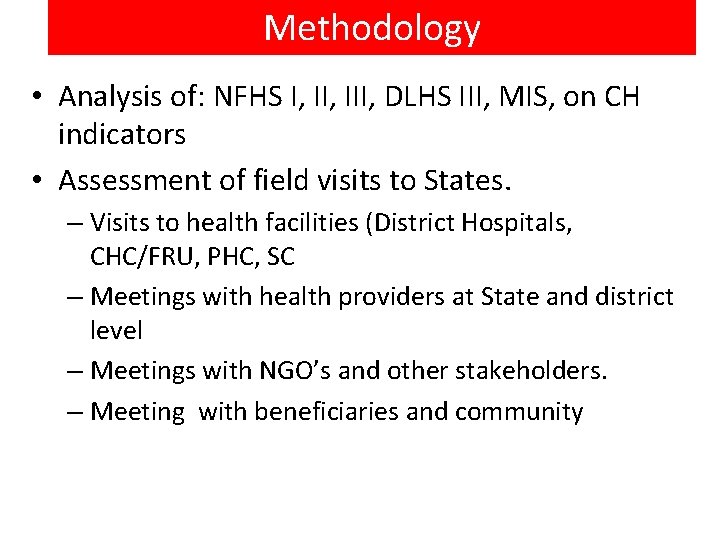
Methodology • Analysis of: NFHS I, III, DLHS III, MIS, on CH indicators • Assessment of field visits to States. – Visits to health facilities (District Hospitals, CHC/FRU, PHC, SC – Meetings with health providers at State and district level – Meetings with NGO’s and other stakeholders. – Meeting with beneficiaries and community

TRENDS IN CHILD HEALTH
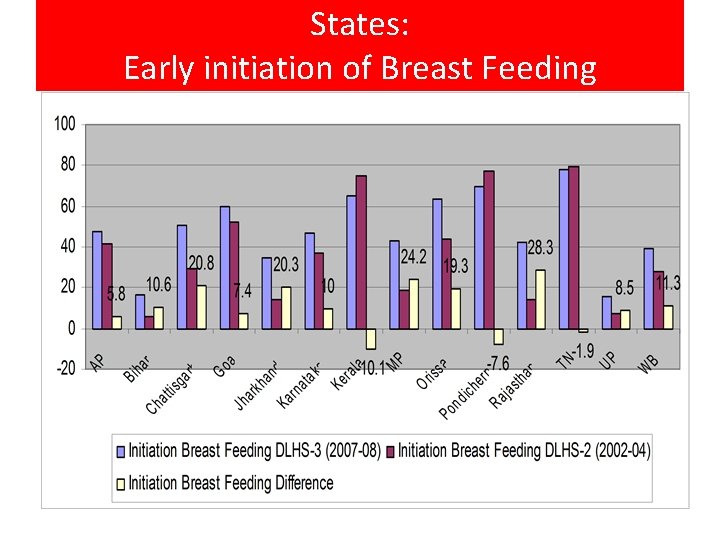
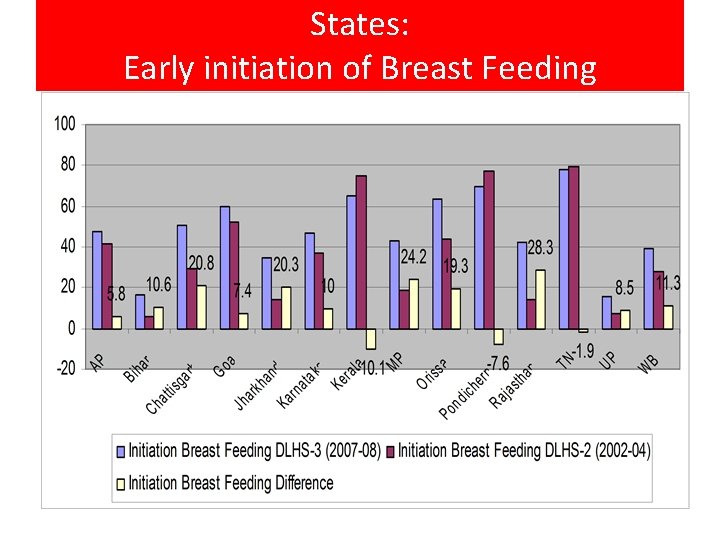
States: Early initiation of Breast Feeding
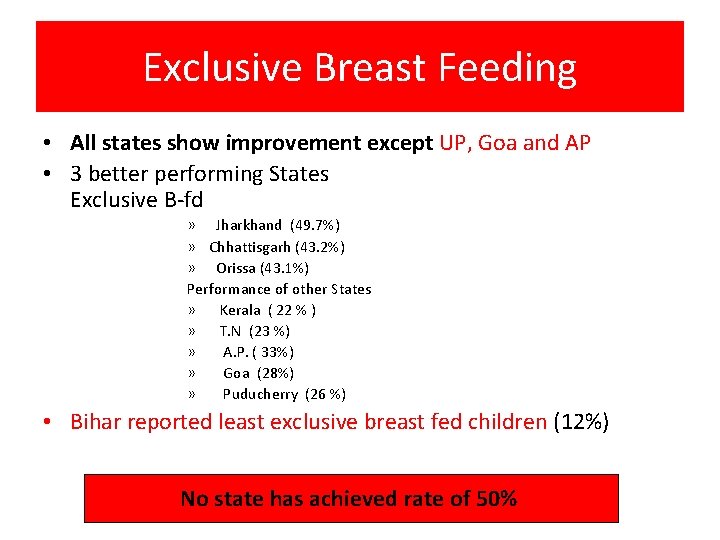
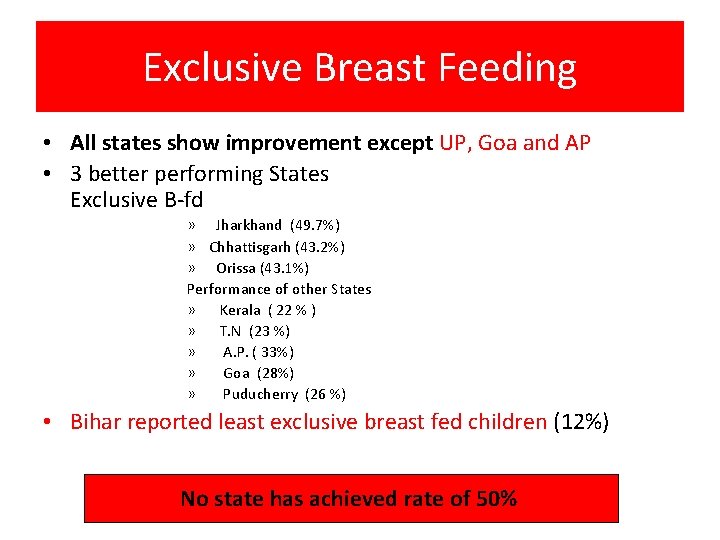
Exclusive Breast Feeding • All states show improvement except UP, Goa and AP • 3 better performing States Exclusive B-fd » Jharkhand (49. 7%) » Chhattisgarh (43. 2%) » Orissa (43. 1%) Performance of other States » Kerala ( 22 % ) » T. N (23 %) » A. P. ( 33%) » Goa (28%) » Puducherry (26 %) • Bihar reported least exclusive breast fed children (12%) No state has achieved rate of 50%
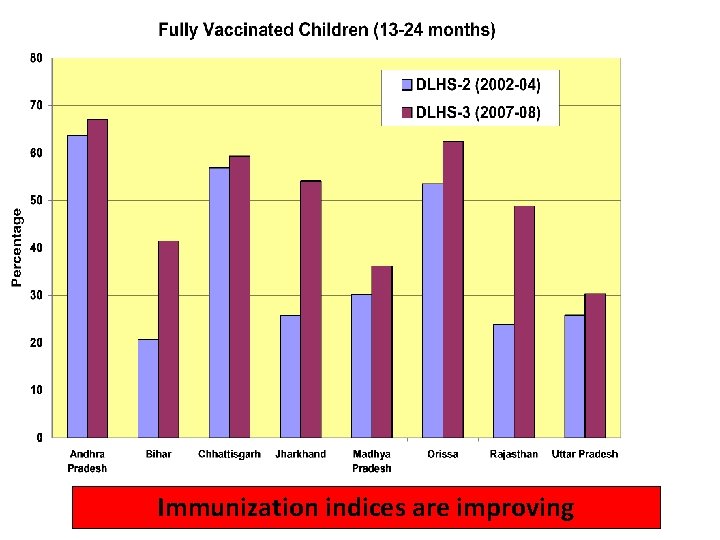
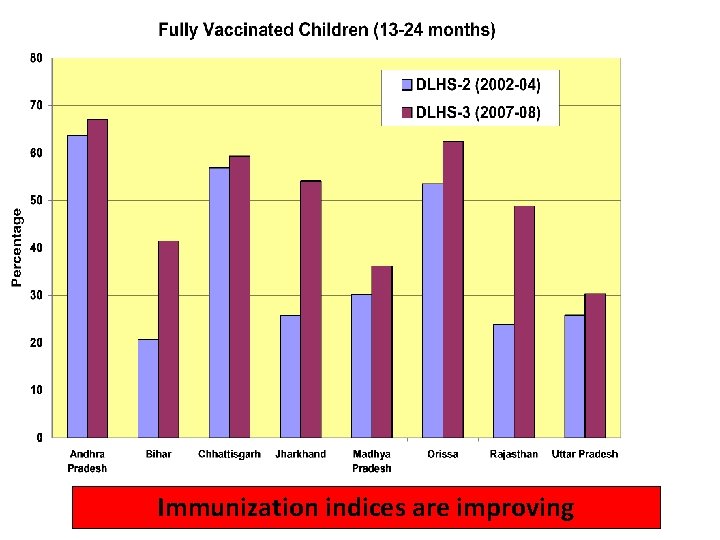
Immunization indices are improving
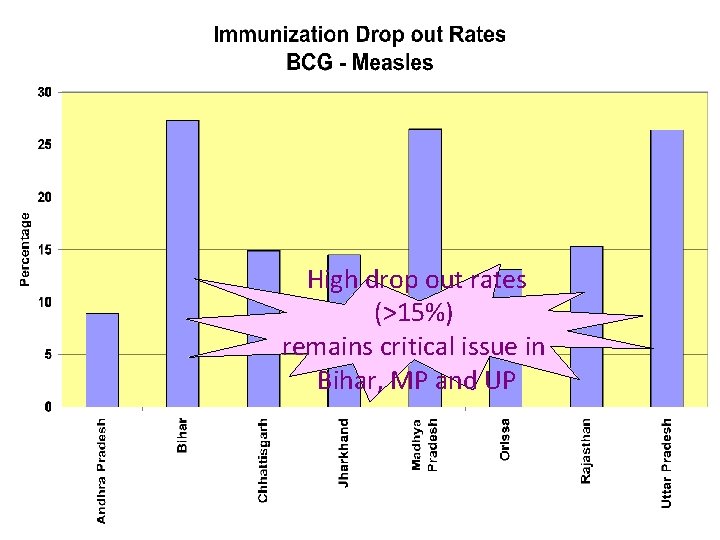
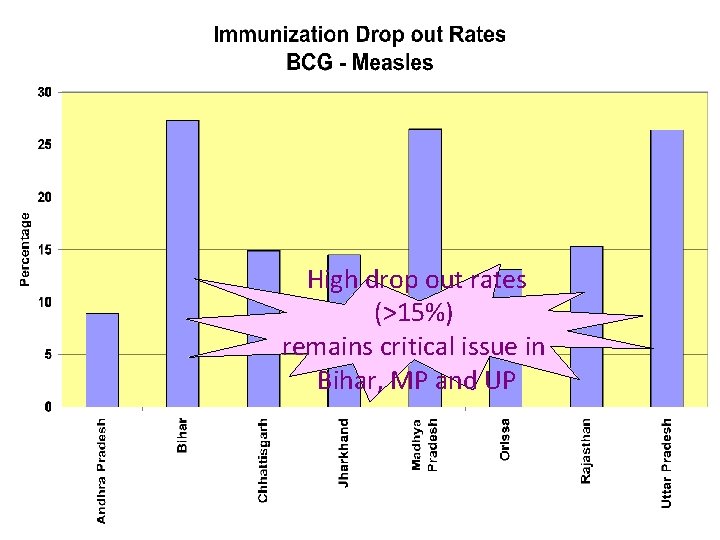
High drop out rates (>15%) remains critical issue in Bihar, MP and UP

Training - Child health TRAINING SATES DISTRICTS NO. TRAINED IMNCI 28 145 135000 PRE SERVICE IMNCI 6 STATES-60 MEDICAL COLLEGES 4000
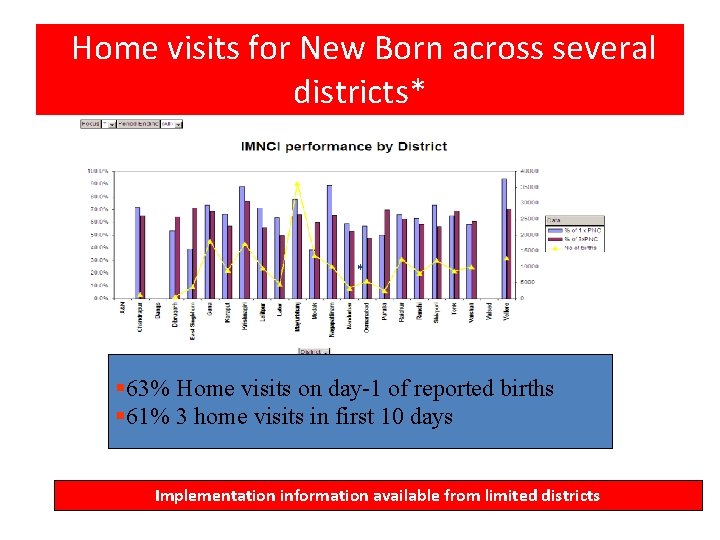
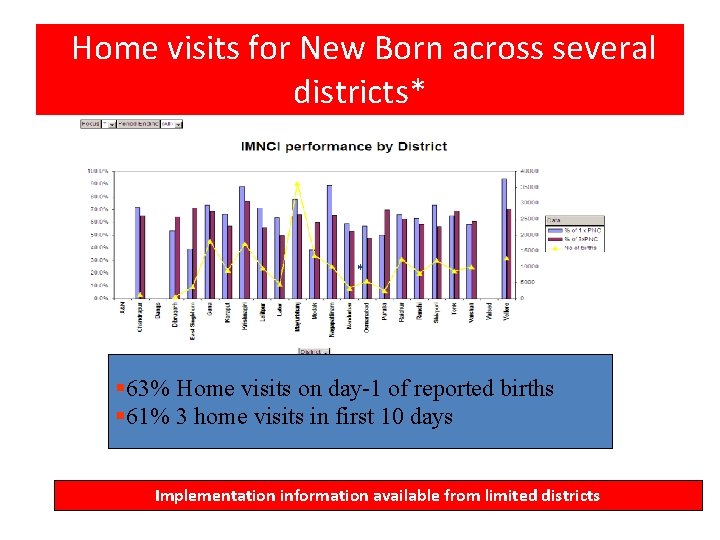
Home visits for New Born across several districts* * § 63% Home visits on day-1 of reported births § 61% 3 home visits in first 10 days Implementation information available from limited districts
Initiatives in Pipeline • F-IMNCI (IMNCI and Facility based care in the process of finalization) • Newborn Health Care strategy on the anvil • School Health Programme • Pentavalent Vaccine

Innovative Schemes • District Child Health Co-ordinator (Rajasthan, MP, Orissa) • ISO certification of District Hospitals. Standard Protocols for New Born and Sick New Born at District Hospitals (Gujarat) • New Born Care Kits (2 Baby Mattresses; 4 Baby Jackets; 3 Baby Caps; 3 pairs of Gloves; 12 Baby Diapers and 8 Baby Blankets) (AP) • Health information help line
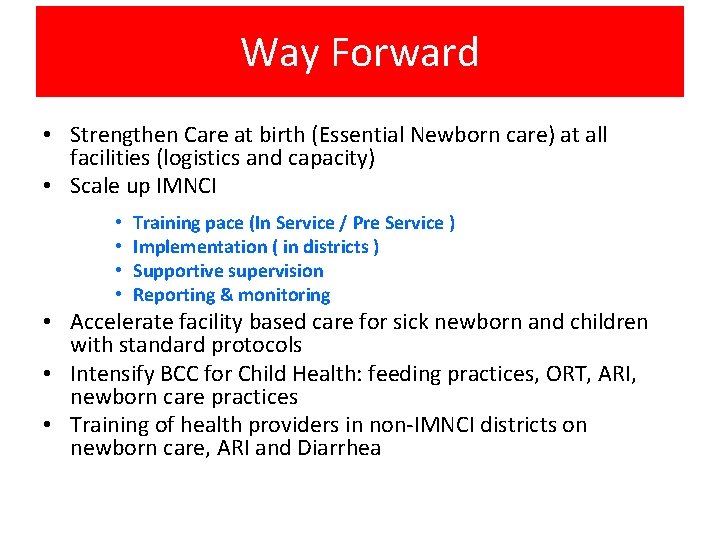
Way Forward • Strengthen Care at birth (Essential Newborn care) at all facilities (logistics and capacity) • Scale up IMNCI • • Training pace (In Service / Pre Service ) Implementation ( in districts ) Supportive supervision Reporting & monitoring • Accelerate facility based care for sick newborn and children with standard protocols • Intensify BCC for Child Health: feeding practices, ORT, ARI, newborn care practices • Training of health providers in non-IMNCI districts on newborn care, ARI and Diarrhea
 Strategic goals tactical goals operational goals
Strategic goals tactical goals operational goals Strategic goals tactical goals operational goals
Strategic goals tactical goals operational goals National health intervention programme for mother and child
National health intervention programme for mother and child Rch programme conclusion
Rch programme conclusion Why shift from mdg to sdg
Why shift from mdg to sdg Mdg
Mdg National policy and legislation
National policy and legislation National health strategy zimbabwe
National health strategy zimbabwe National health security strategy
National health security strategy General goals and specific goals
General goals and specific goals Examples of generic goals and product-specific goals
Examples of generic goals and product-specific goals Treatment plan for adhd
Treatment plan for adhd 전위 순회
전위 순회 A multistep strategy to achieve your goals
A multistep strategy to achieve your goals National patient safety goals 2012
National patient safety goals 2012 The national patient safety goal 6
The national patient safety goal 6 2018 national patient safety goals
2018 national patient safety goals National patient safety goals 2017
National patient safety goals 2017 2013 hospital national patient safety goals
2013 hospital national patient safety goals National patient safety goal 6
National patient safety goal 6 Tenue type 1 rch
Tenue type 1 rch Reproductive and child health programme phase 1
Reproductive and child health programme phase 1 Rch programme
Rch programme How to change lmp date in rch portal
How to change lmp date in rch portal Rch phase 2
Rch phase 2 Anmol app data entry
Anmol app data entry Role of nurse in rch phase 2
Role of nurse in rch phase 2 Epilepsy
Epilepsy Rch portal
Rch portal Roseola infantum rch
Roseola infantum rch Rch supracondylar fracture
Rch supracondylar fracture Agencies related to child welfare
Agencies related to child welfare National agencies related to child welfare
National agencies related to child welfare Pediprn
Pediprn National network of child psychiatry access programs
National network of child psychiatry access programs National tribal child support association
National tribal child support association