Chapter 3 Inflammation and Repair Defense Mechanisms Defense
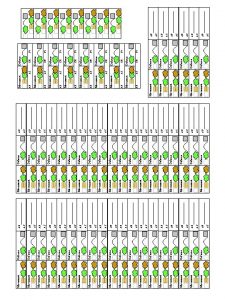
- Slides: 27
Chapter 3 Inflammation and Repair
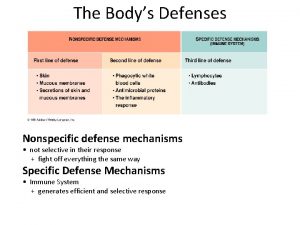
Defense Mechanisms • Defense mechanisms can be – Nonspecific: • Protecting against all invaders – Specific: • Identifies specific invader before neutralizing it • Three lines of defense protect body against foreign invasion: 1. Physical or surface barriers (nonspecific) 2. Inflammation (nonspecific) 3. Immune response (specific)
Defense Mechanisms: Physical or Surface Barriers • Skin – Body’s first line of defense – Covered with “good” bacteria • Normal flora • Prevents growth of “bad” bacteria – Glands • Secrete antibacterial substances onto surface – Mucus membranes • Secrete mucus that traps invaders
Defense Mechanisms: Inflammation • Nonspecific response to anything causing cell injury – Causes can be: • Goal – Isolate & destroy invader, clean up debris, & promote healing • Characteristic signs of inflammation are:
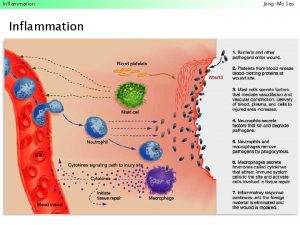
Inflammatory Process • Chemical agents are formed & released when tissue is damaged – Called: • Cell Derived Mediators come from two sources: – Mast cells – Injured cells
Inflammatory Process: Cell derived Mediators • Mast cells – Specialized cells found in: – Release histamine in response to trauma • Histamine – Leads to:
Inflammatory Process: Cell derived Mediators • Injured cells – Plasma membranes release two mediators in response to injury: – Effect:
Inflammatory Process: plasma derived Mediators • Blood plasma contains proteins that circulate as inactive compounds • With tissue damage they leak into injured area and are activated – Called: – Leads to:
Inflammatory Process • Hyperemia: – Vasodilation: increases blood flow to the area • Causes increased redness and heat • Bring increased numbers of leukocytes (WBC’s) to the area
Inflammatory Process • Leaky blood vessels – Fluid leaks from dilated & more permeable blood vessels into tissues • Called: – Fluid containing: • Leads to: – Neutrophils escape from blood into tissues
Inflammatory Process • Neutrophils – A type of white blood cell – Use phagocytosis – Drawn to injured area by chemotaxis • Chemicals released by injured tissue or bacteria tell neutrophils where to go • Monocytes show up 3 -4 days later
Inflammatory Process • Monocytes – A type of white blood cell – Are called a macrophage after entering tissue – Use phagocytosis • Other leukocytes of inflammation release chemicals – Basophils: histamine – Eosinophils: allergic response
Defense Mechanisms: Immune response – Occurs if inflammation persists beyond 7 days – Lymphocytes will be used • A type of WBC • Specific killers • ID invaders & make antibodies that neutralize/kill – Remember invader for later
Types of Inflammation • Hard to determine exactly when acute inflammation becomes chronic • In general: – Acute: lasts less than 10 days – Chronic: lasts longer than 10 days • Will see a larger # of macrophages & less neutrophils • Can see damage to tissue • If damage is severe scar tissue may form which can disturb normal function
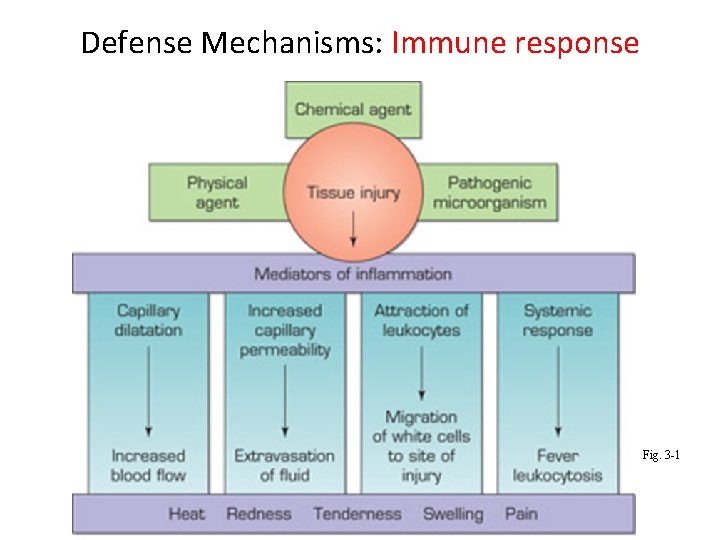
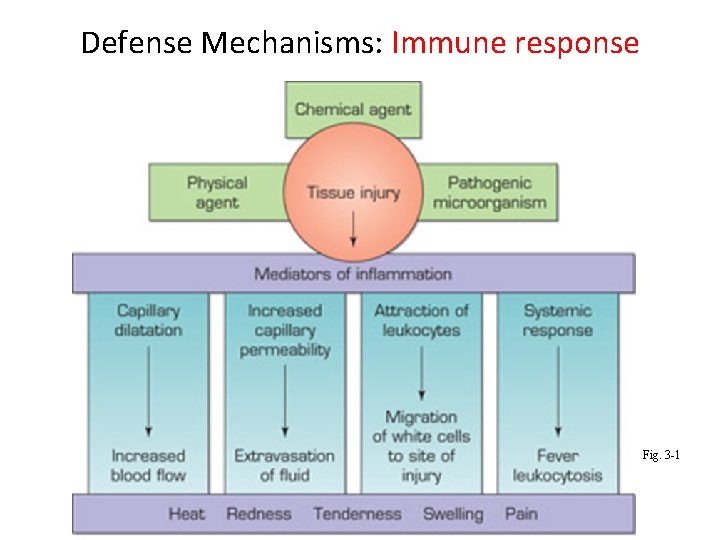
Defense Mechanisms: Immune response Fig. 3 -1
Tissue Repair and Healing • Final phase of inflammation – Macrophages clean up the area & stimulate the repair process – Body repairs tissue in 2 ways: • Regeneration – Damaged tissue replaced by cell division of healthy tissue – Ex. Skin tissue replaced by epithelial cell division • Fibrous connective tissue repair – Same results no matter location – A tough fibrous tissue is formed (scar) – Doesn’t restore function – Nerve, brain, & heart muscle don’t regenerate only use fibrous repair
Inflammatory Exudates • Appearance of exudate can vary • Types: – Serous – Fibrinous – Purulent – Hemorrhagic
Inflammatory Exudates • Serous exudate – E. g. • Fibrinous exudate – Coagulates to form a mesh-like lesion • On surface called: – Can cause 2 areas to stick together • Called an:
Inflammatory Exudates • Purulent exudate – Commonly called: • Hemorrhagic exudate
Lesions • Any abnormality of tissue due to physical or pathologic injury • Lesions caused by inflammation include: – Abscesses – Cellulitis
Lesions • Abscess • Usually caused by bacterial infection – Will see common signs of inflammation – Draining an abscess can help speed healing – Ex.
Lesions • Cellulitis – Characterized by: – Cause:
Infection • Invasion of pathogenic organisms causing cell or tissue injury & leading to the inflammatory response – Pathogenic • 3 conditions needed for infection to occur
Conditions Needed for Infection to Occur 1. Pathogens must successfully enter the body – Common points of entry
Conditions Needed for Infection to Occur 2. Pathogen needs to be able to survive the hosts defenses – Virulence: • High virulence: • High number of invading microorganisms • Vulnerable condition of individual or host
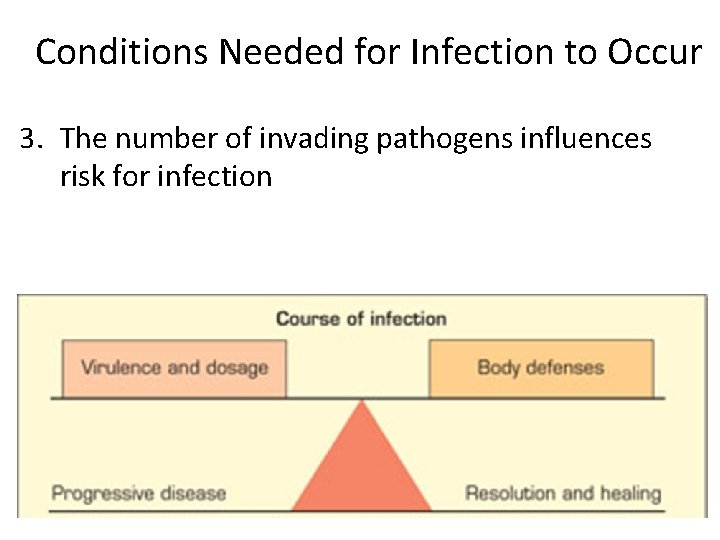
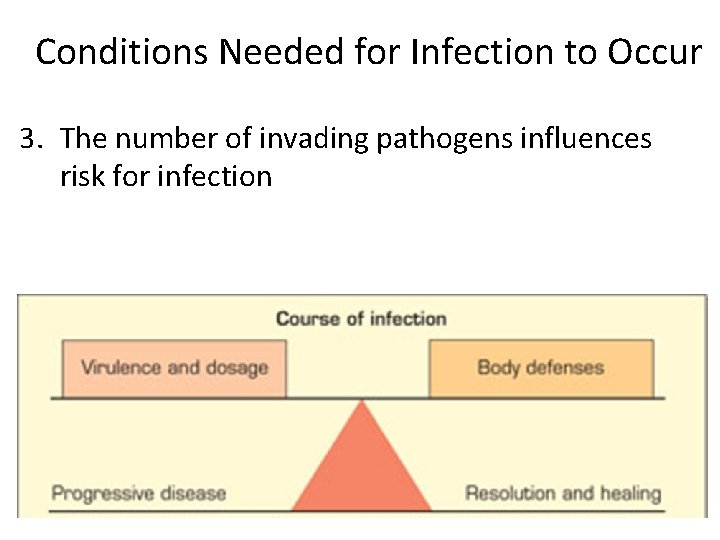
Conditions Needed for Infection to Occur 3. The number of invading pathogens influences risk for infection
? ? QUESTIONS? ? 27
 Dna repair mechanism notes
Dna repair mechanism notes Base excision repair
Base excision repair Mom boy
Mom boy Freud defense mechanism examples
Freud defense mechanism examples Specific defense vs nonspecific defense
Specific defense vs nonspecific defense Reciprocal determinism
Reciprocal determinism How do sponges protect themselves
How do sponges protect themselves Ego defenses
Ego defenses Oral fixation examples
Oral fixation examples Sublimation defence mechanism
Sublimation defence mechanism Superego definition psychology
Superego definition psychology Free association psychology
Free association psychology The id operates on the ________ principle.
The id operates on the ________ principle. Psychodynamic personality theory
Psychodynamic personality theory The real reason dinosaurs became extinct
The real reason dinosaurs became extinct What are defense mechanisms according to freud?
What are defense mechanisms according to freud? Sour graping defense mechanism
Sour graping defense mechanism Freud's theory
Freud's theory Psychoanalytic theory defense mechanisms
Psychoanalytic theory defense mechanisms Female oedipal development klein
Female oedipal development klein Defense mechanisms nursing
Defense mechanisms nursing Defense mechanisms nursing
Defense mechanisms nursing Defense mechanisms nursing
Defense mechanisms nursing Freudian analysis
Freudian analysis Anna freud defense mechanisms
Anna freud defense mechanisms Hublov
Hublov Ego defense mechanisms in lord of the flies
Ego defense mechanisms in lord of the flies Power brake system
Power brake system