HUMAN DEFENSE MECHANISMS Categories of Defense Mechanisms Physical


- Slides: 54
HUMAN DEFENSE MECHANISMS

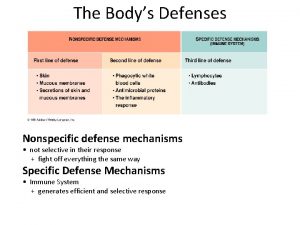
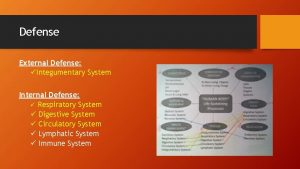
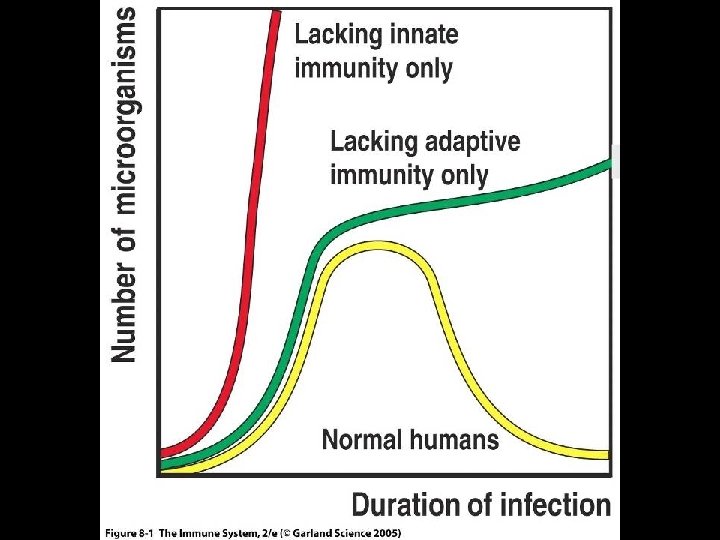
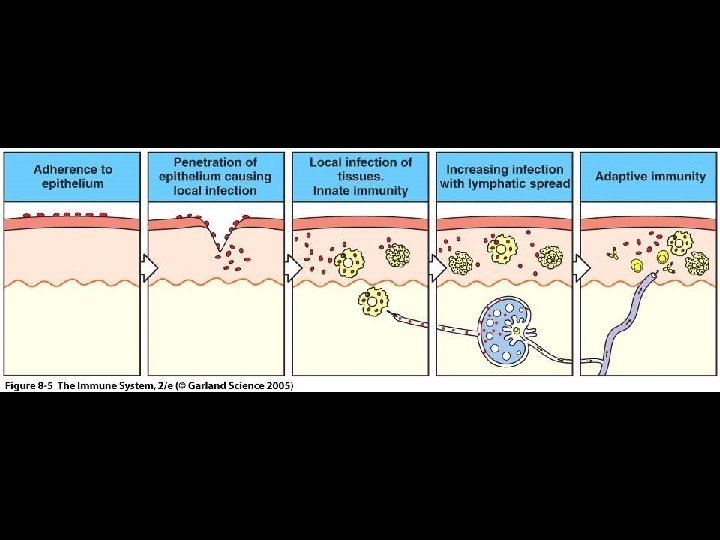
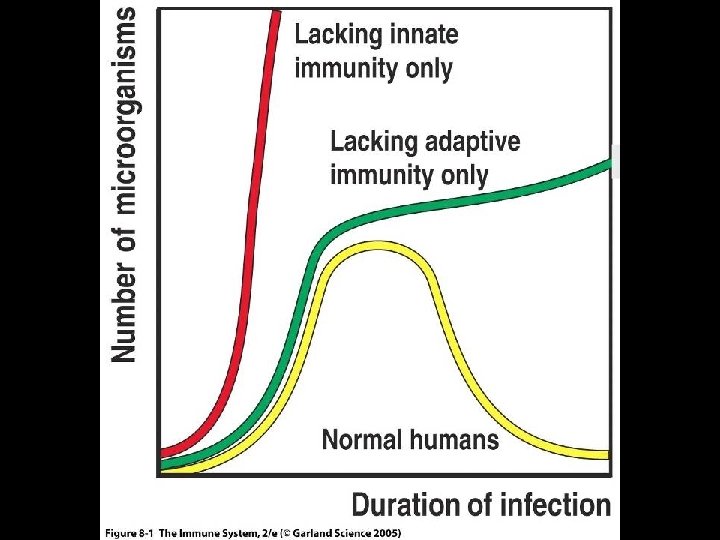
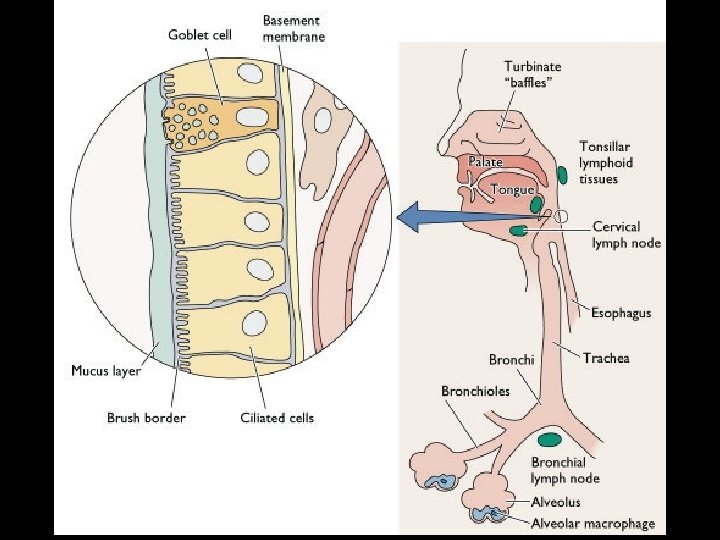
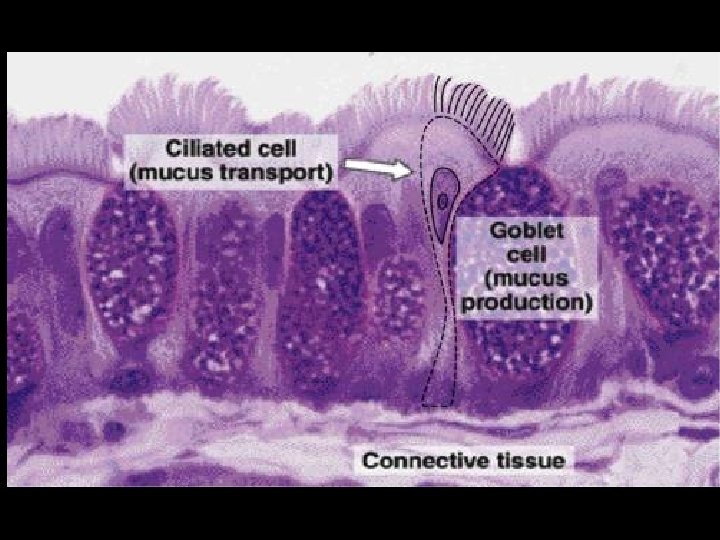
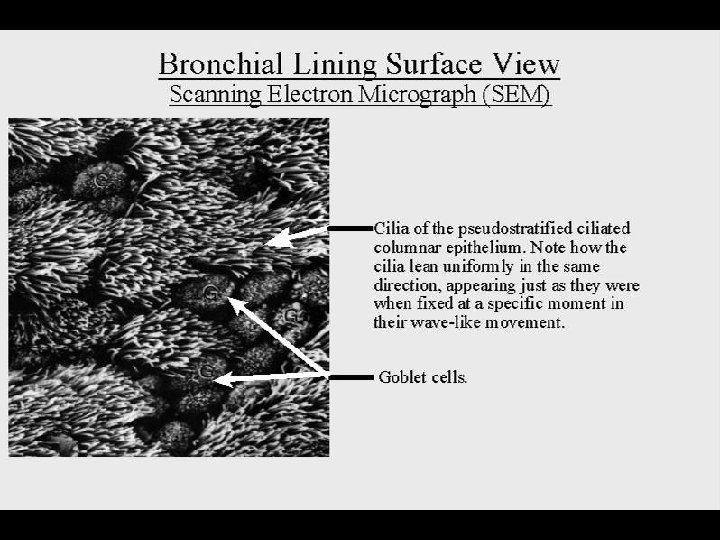
Categories of Defense Mechanisms • Physical barriers > Skin and mucous membranes – Chemical factors – Mechanical factors – Microbiological factors • Innate immunity • Adaptive immunity
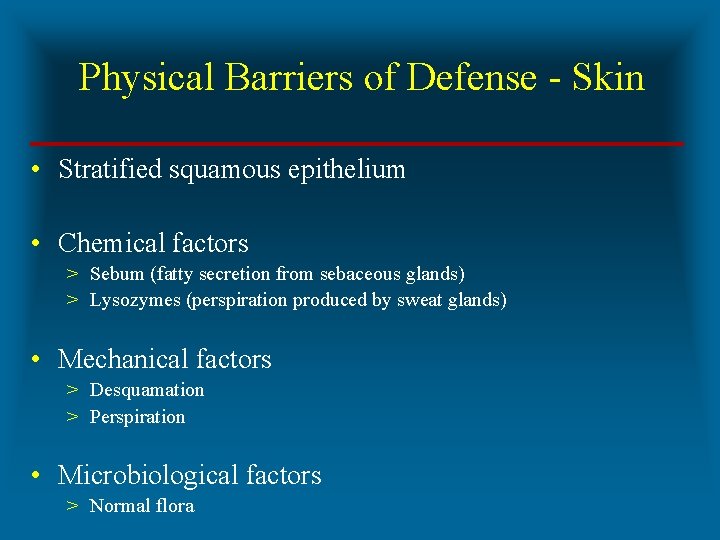
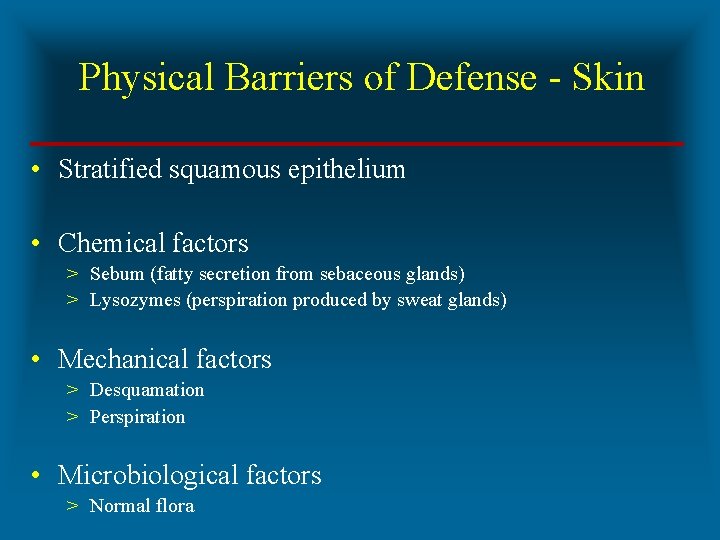
Physical Barriers of Defense - Skin • Stratified squamous epithelium • Chemical factors > Sebum (fatty secretion from sebaceous glands) > Lysozymes (perspiration produced by sweat glands) • Mechanical factors > Desquamation > Perspiration • Microbiological factors > Normal flora
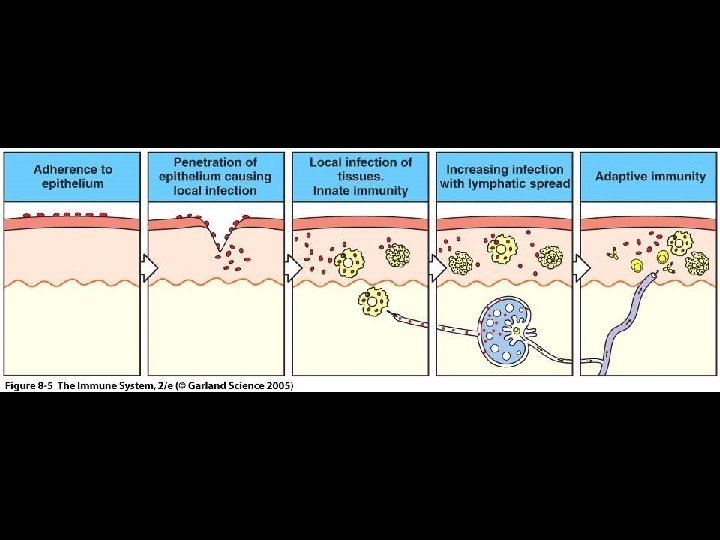
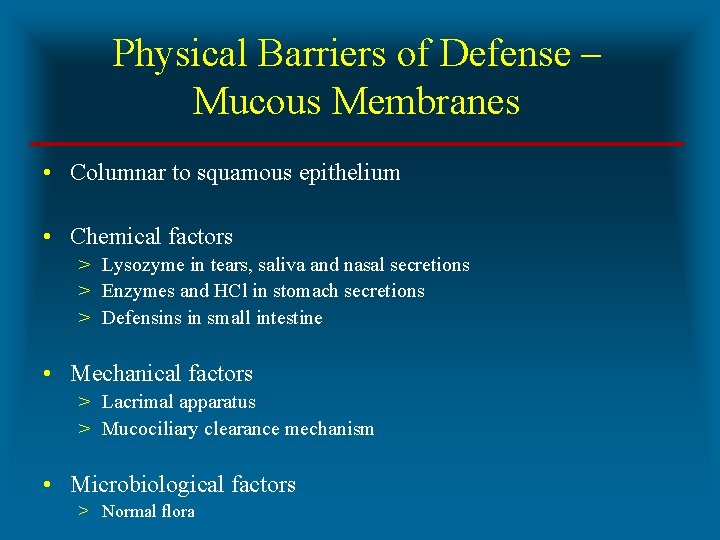
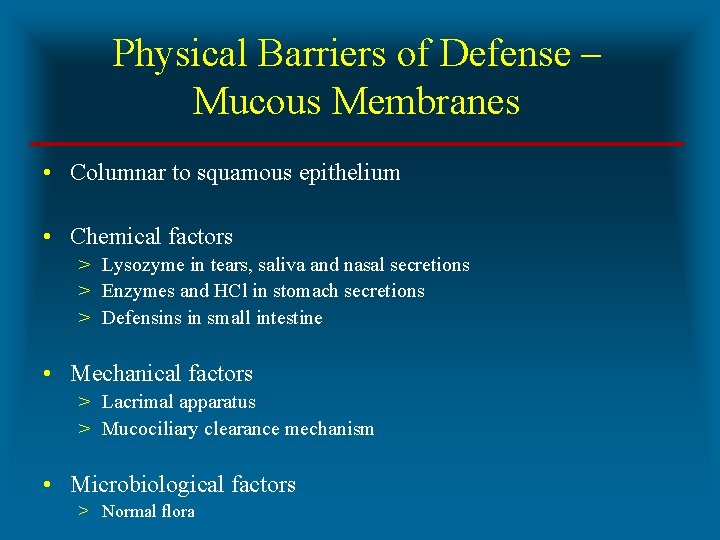
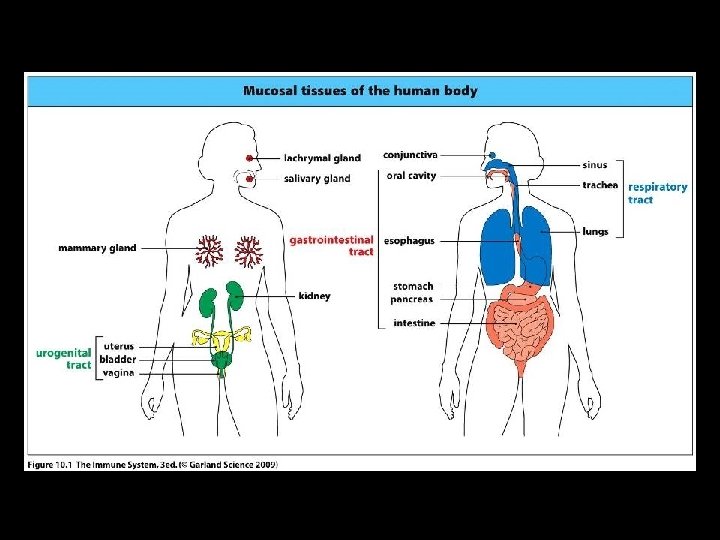
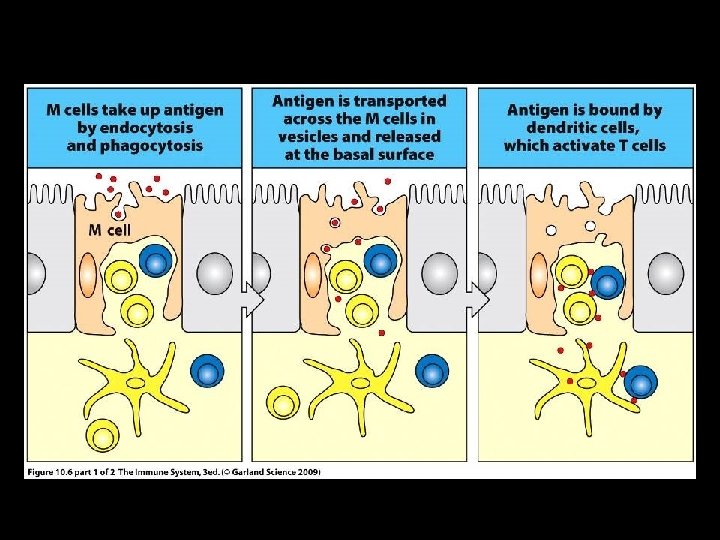
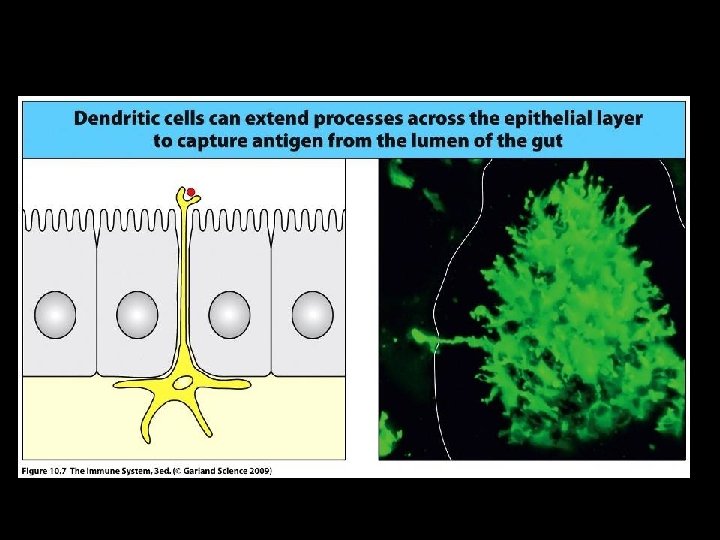
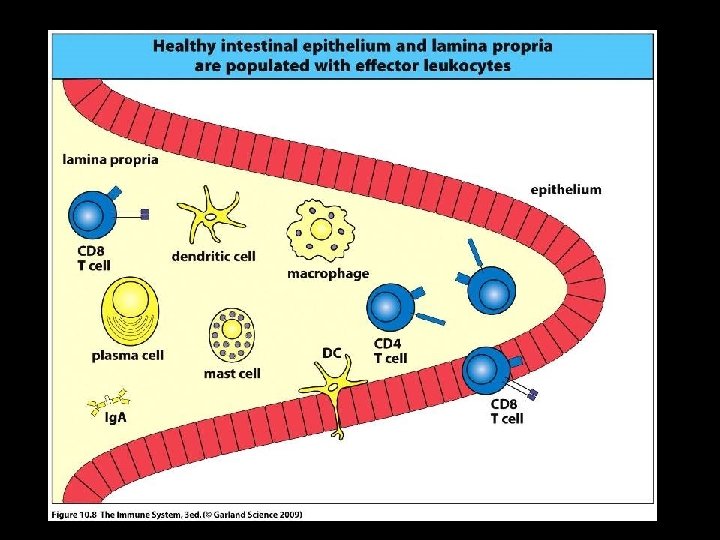
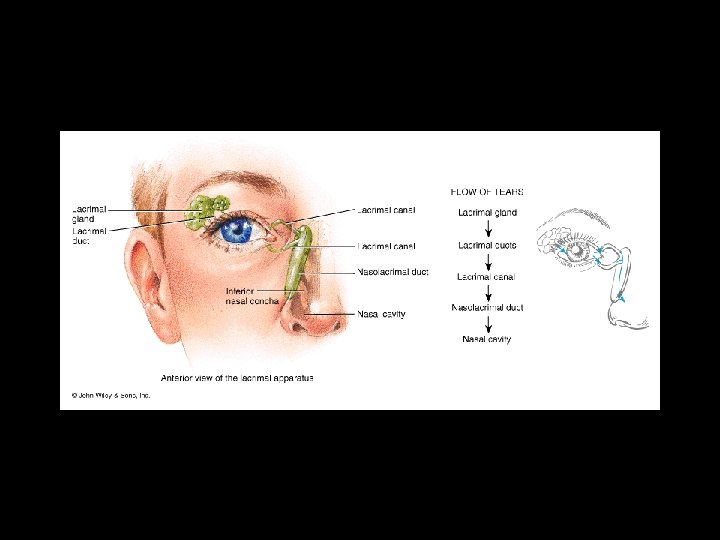
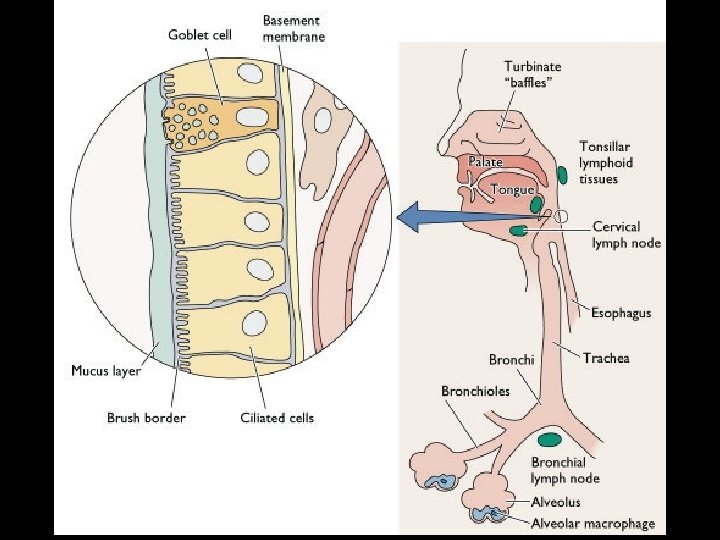
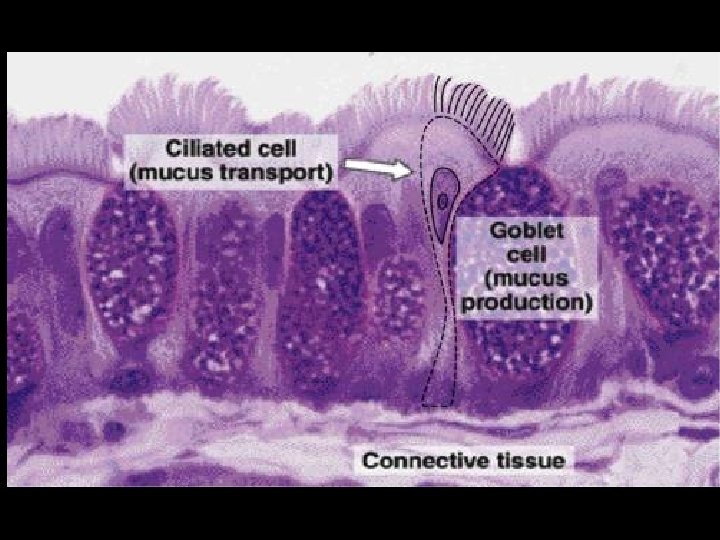
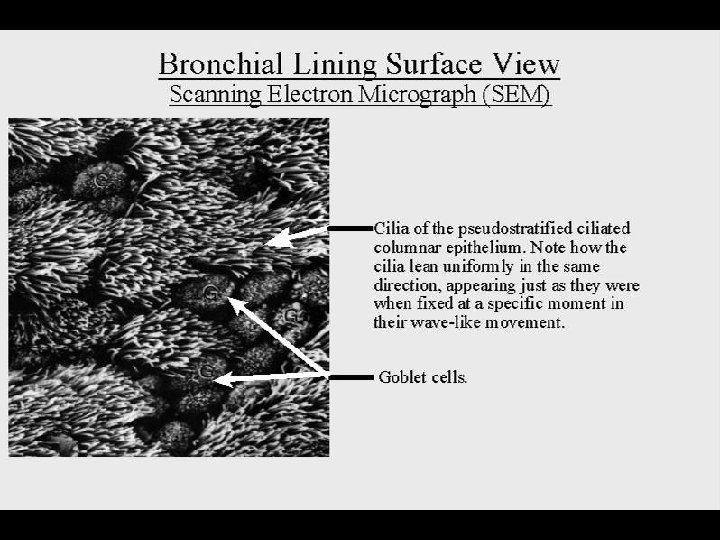
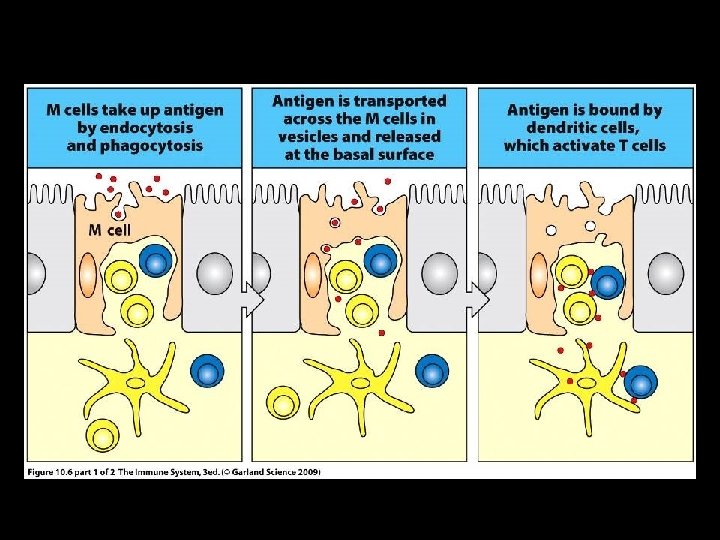
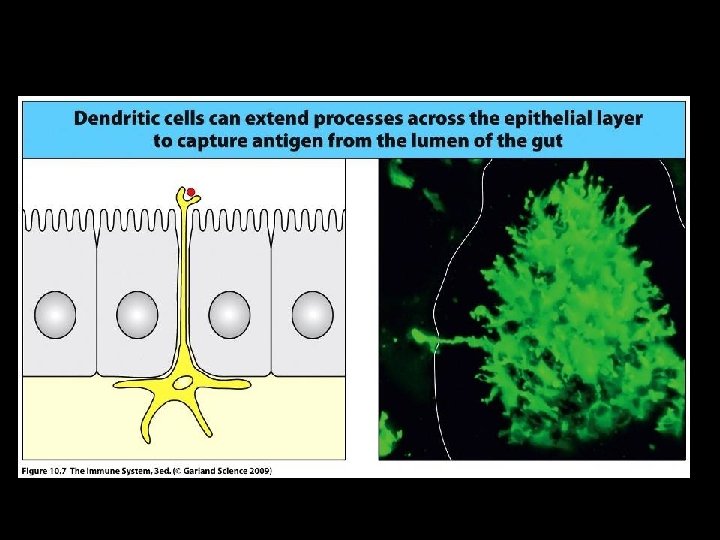
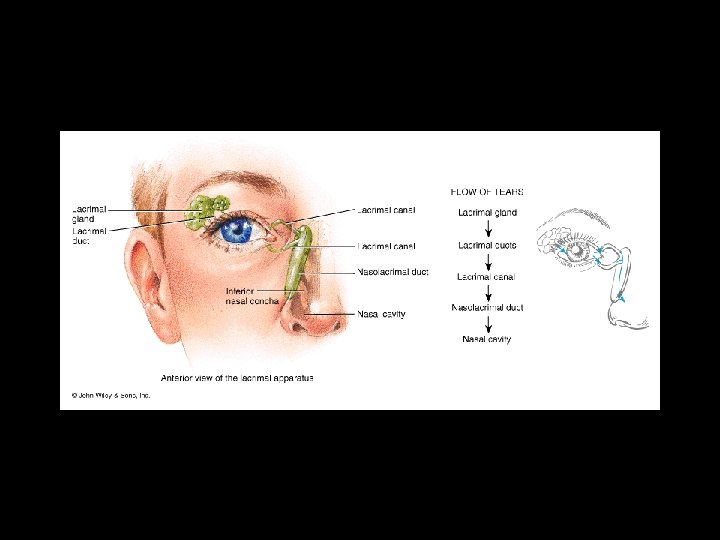
Physical Barriers of Defense – Mucous Membranes • Columnar to squamous epithelium • Chemical factors > Lysozyme in tears, saliva and nasal secretions > Enzymes and HCl in stomach secretions > Defensins in small intestine • Mechanical factors > Lacrimal apparatus > Mucociliary clearance mechanism • Microbiological factors > Normal flora
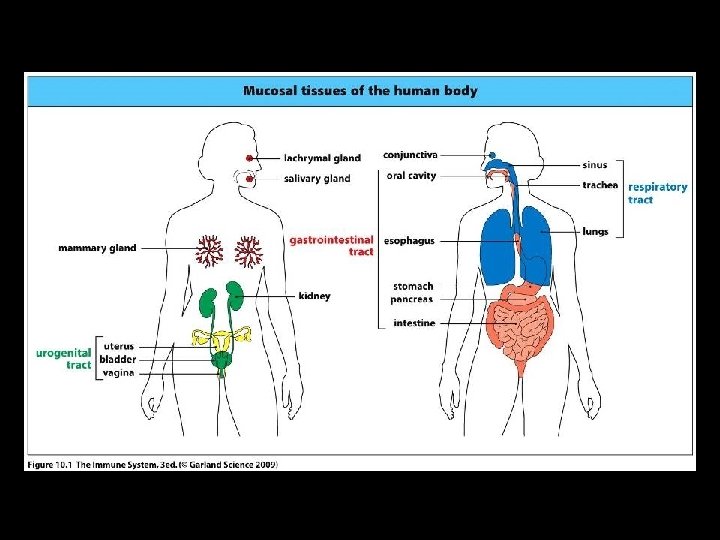
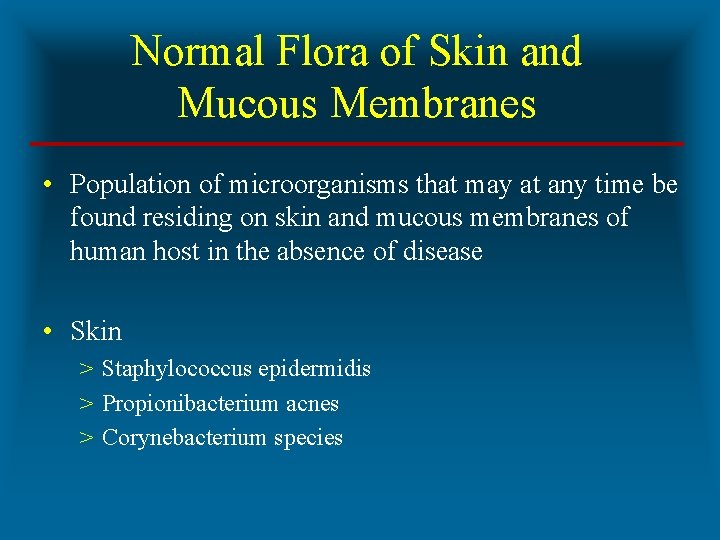
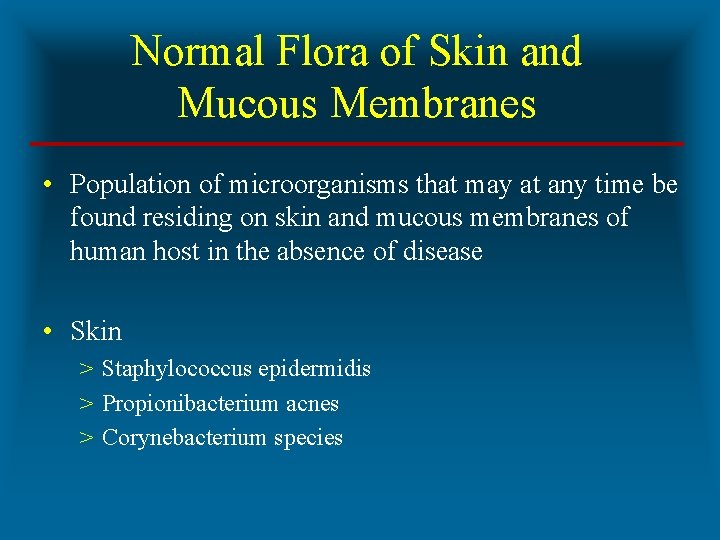
Normal Flora of Skin and Mucous Membranes • Population of microorganisms that may at any time be found residing on skin and mucous membranes of human host in the absence of disease • Skin > Staphylococcus epidermidis > Propionibacterium acnes > Corynebacterium species
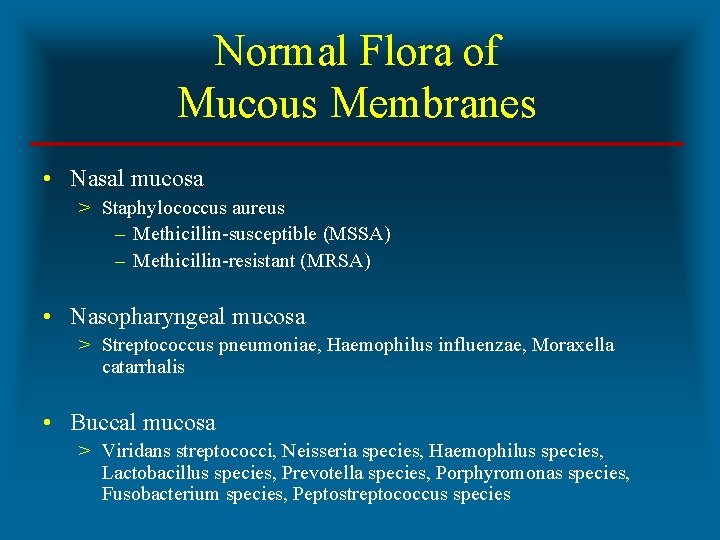
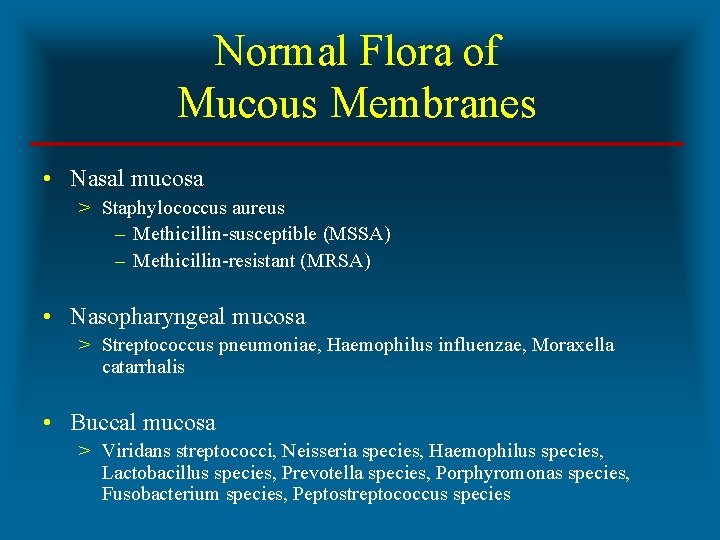
Normal Flora of Mucous Membranes • Nasal mucosa > Staphylococcus aureus – Methicillin-susceptible (MSSA) – Methicillin-resistant (MRSA) • Nasopharyngeal mucosa > Streptococcus pneumoniae, Haemophilus influenzae, Moraxella catarrhalis • Buccal mucosa > Viridans streptococci, Neisseria species, Haemophilus species, Lactobacillus species, Prevotella species, Porphyromonas species, Fusobacterium species, Peptostreptococcus species
Normal Flora of Mucous Membranes • Colon mucosa > Bacteroides fragilis group, Clostridium species, Escherichia coli and other Enterobacteriaceae, Enterococccus species, Lactobacillus species, Candida albicans • Vaginal mucosa > Lactobacillus species, Gardnerella vaginalis, Mobiluncus species, Prevotella species, Porphyromonas species

PROBIOTICS • Definition > Food and Agriculture Organization of UN (FAO) and WHO > ‘live microorganisms which when administered in adequate amounts confer a health benefit on the host’ • Microorganisms > > Bifidobacterium species Lactobacillus bulgaricus Lactobacillus casei Streptococcus thermophilus
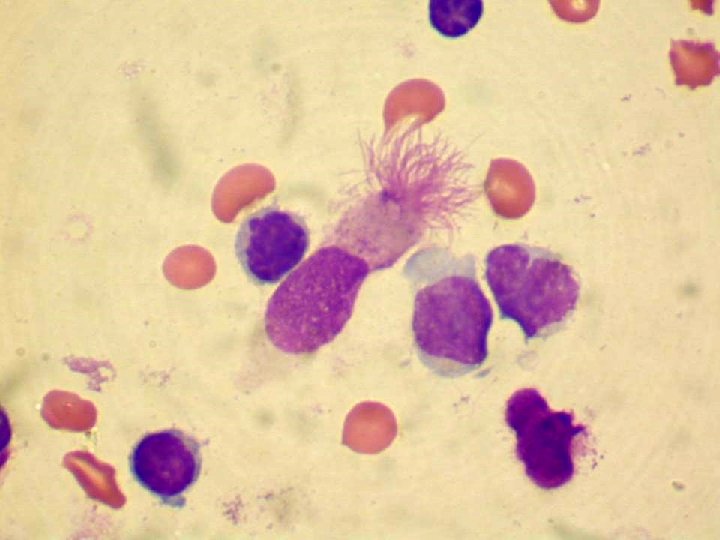
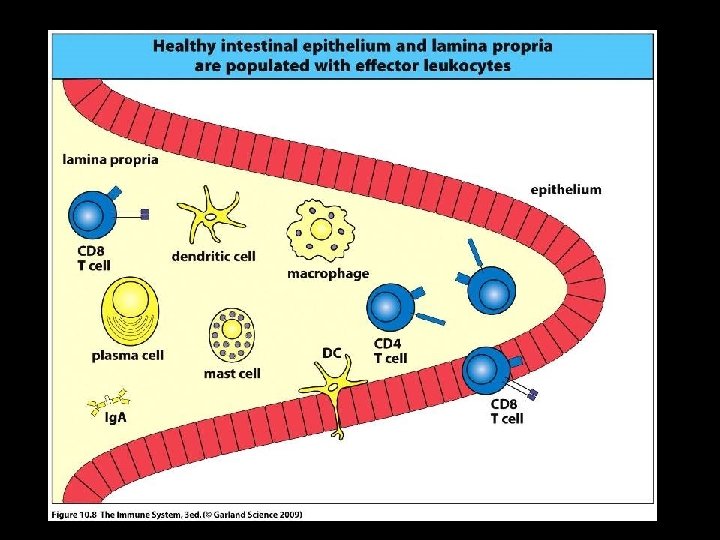
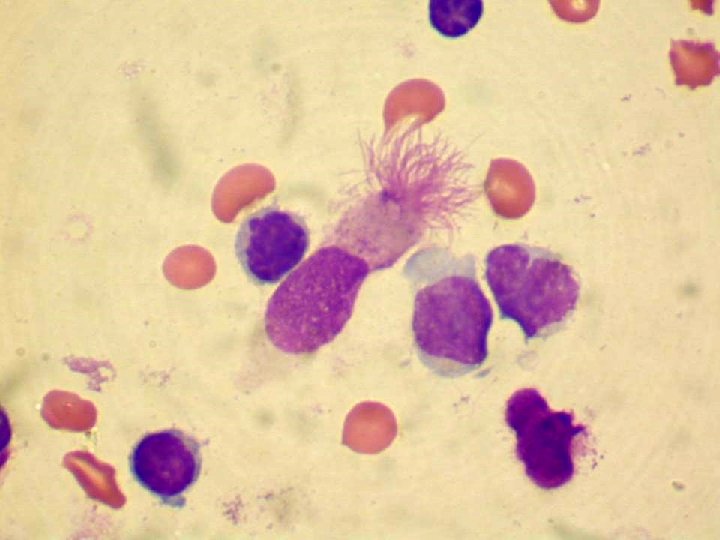
The Innate Response to Bacterial Pathogens • Complement activation via alternative pathway • Phagocytosis of pathogens by > Macrophages – Long-lived cells – Secrete cytokines in innate and adaptive immunity – Function as professional APC’s > Neutrophils – Historically called “microphages” – Enter infected tissues in high numbers – Short-lived cells
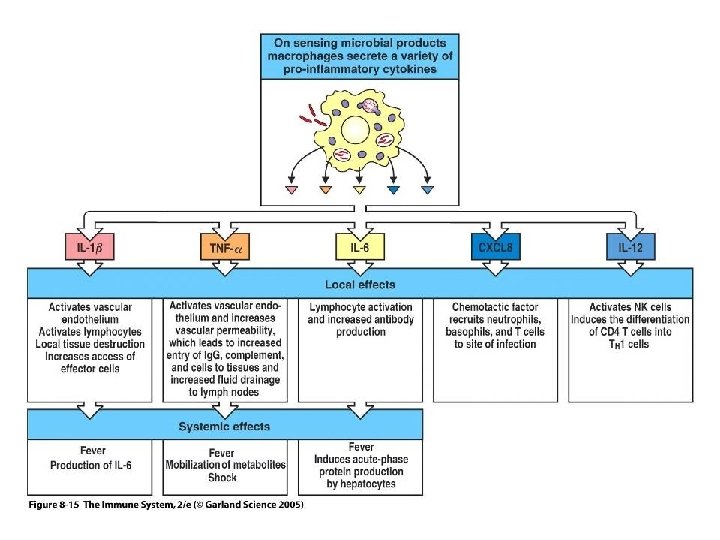
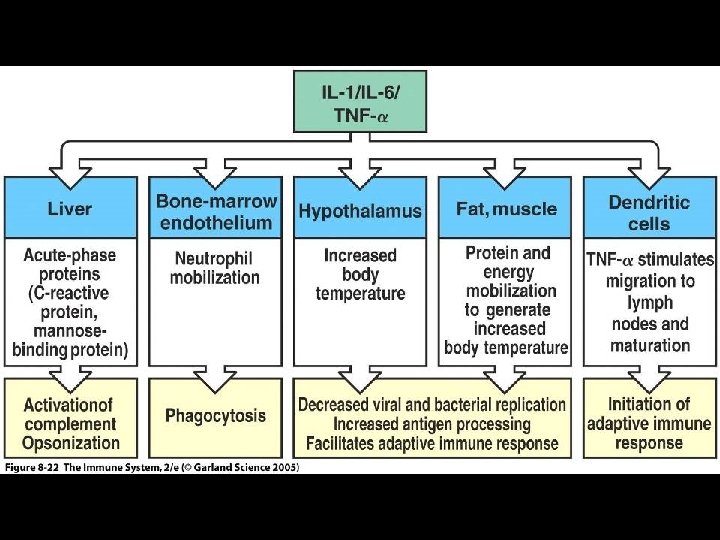
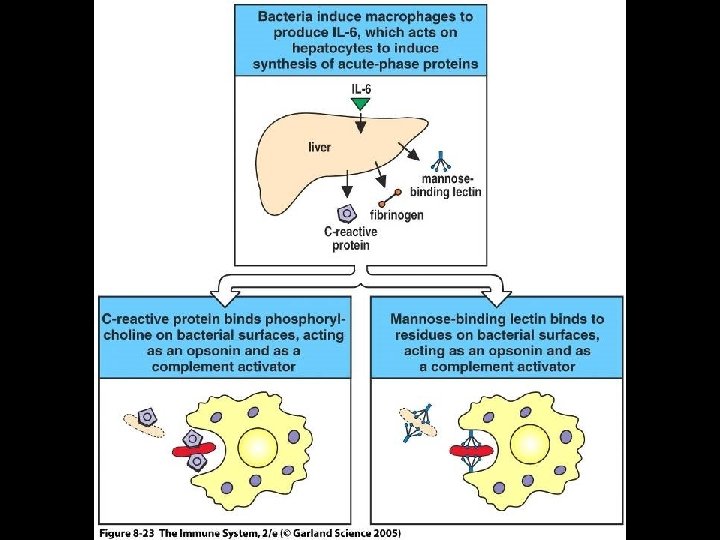
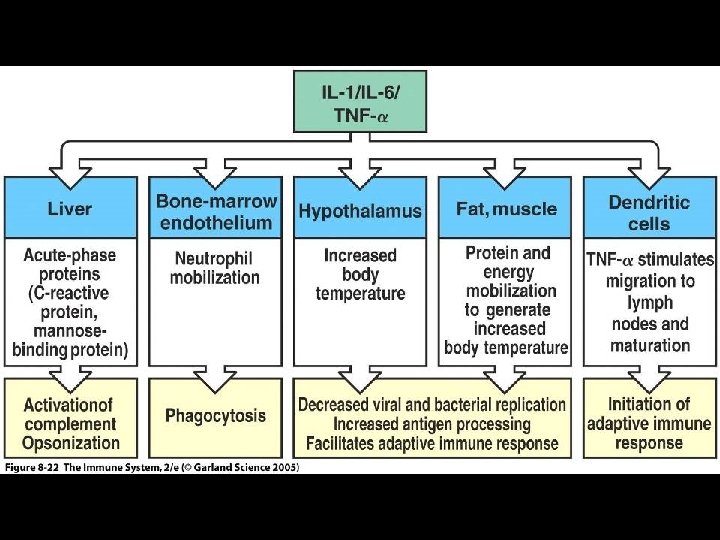
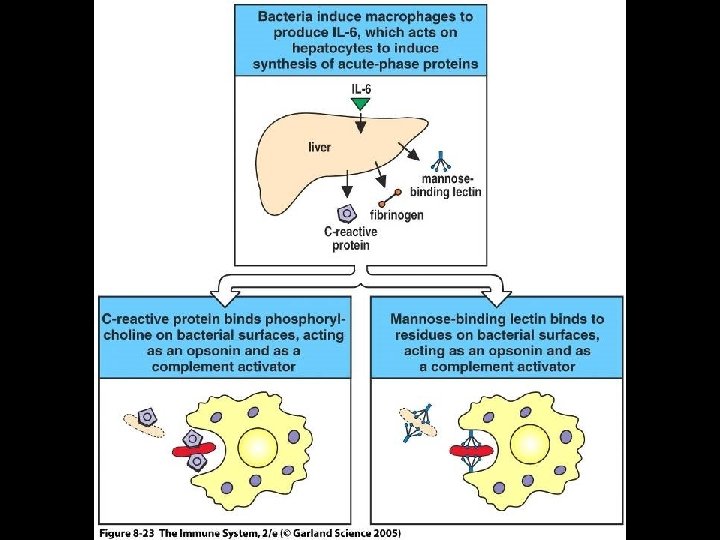
Activation of Tissue Macrophages • Activated macrophages initiate inflammatory response by secreting > Cytokines > Inflammatory mediators • Cytokines (chemoattractant cytokines / chemokines) > IL-1, IL-6, IL-8, IL-12 and TNF-alpha • Inflammatory mediators > Prostaglandins, leukotrienes, plasminogen activator, platelet-activating factor (PAF)
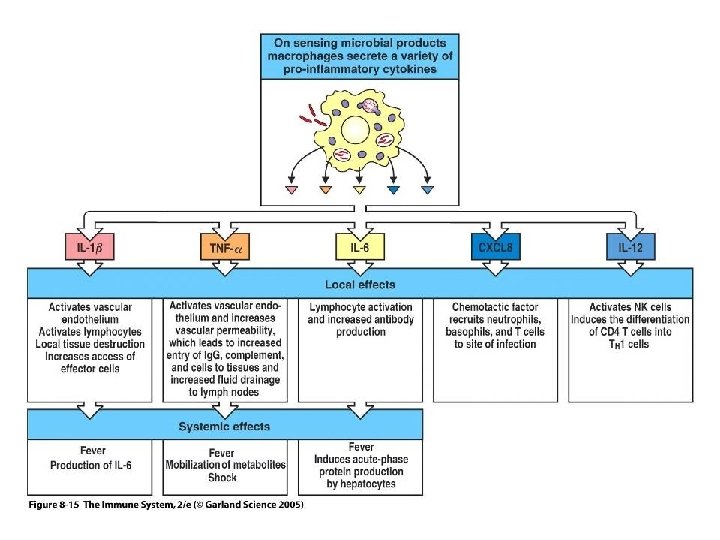
Figure 8 -15
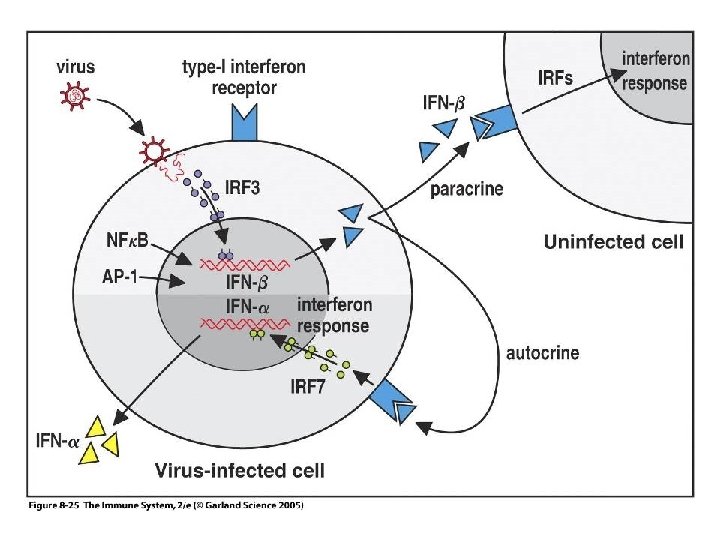
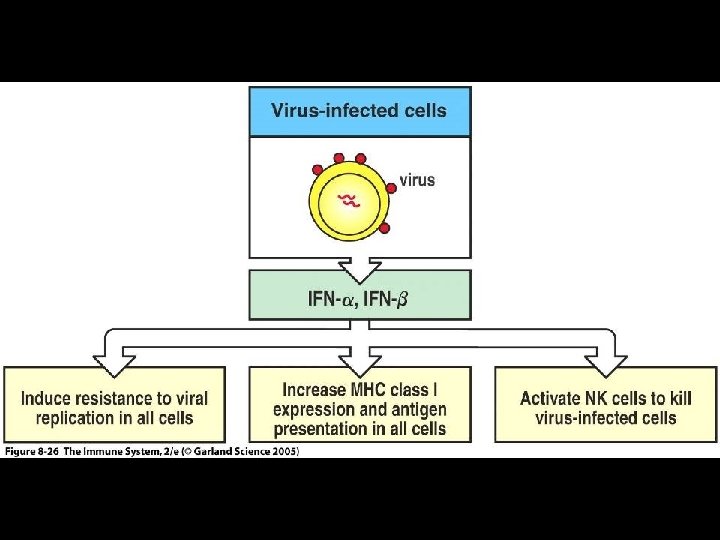
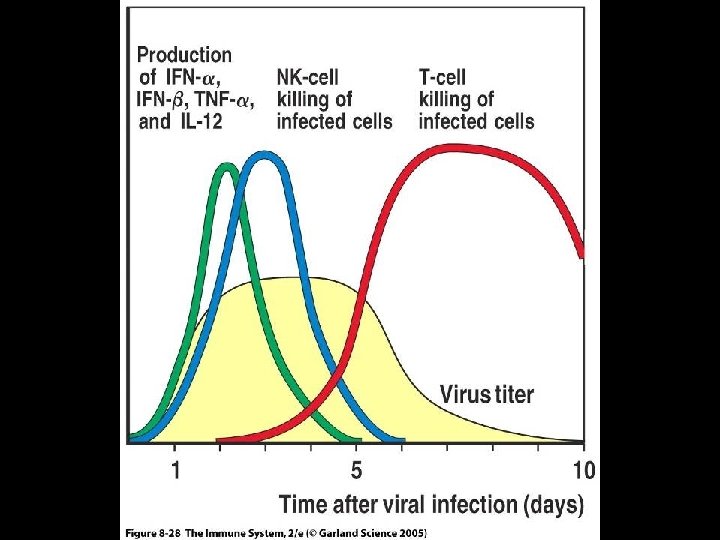
The Innate Response to Viral Pathogens • Virus infection of healthy cells results in production of > Interferon-alpha (IFN-alpha) > Interferon-beta (IFN-beta) • IFN-alpha and IFN-beta are type 1 interferons • Type 1 interferons > Inhibit virus replication > Activate natural killer (NK) cells > Increases expression of MHC-1 molecules
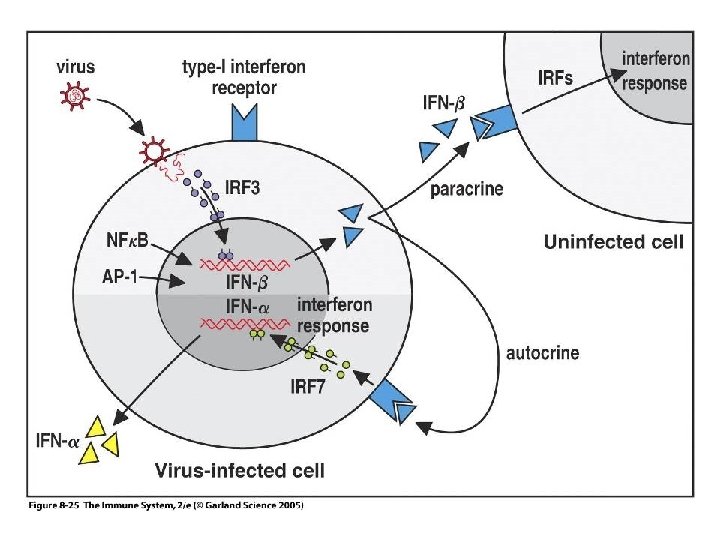
Figure 8 -25
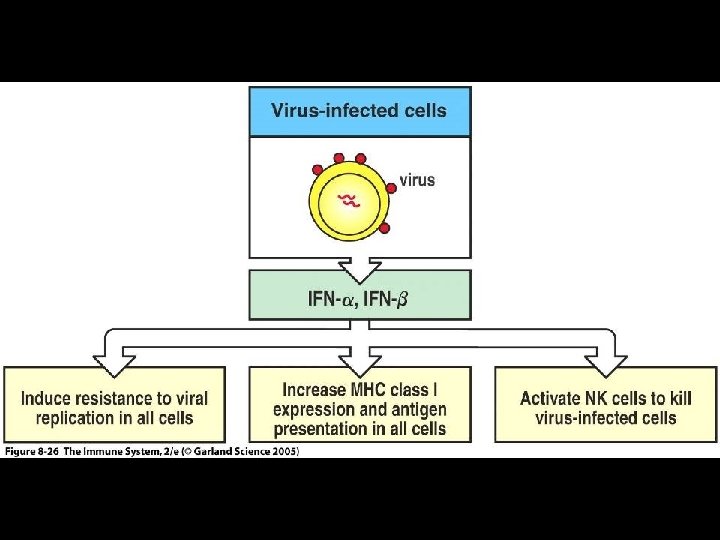
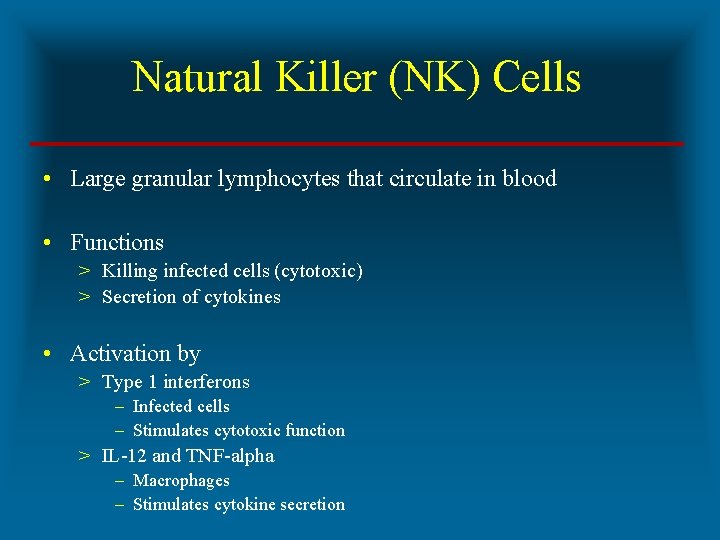
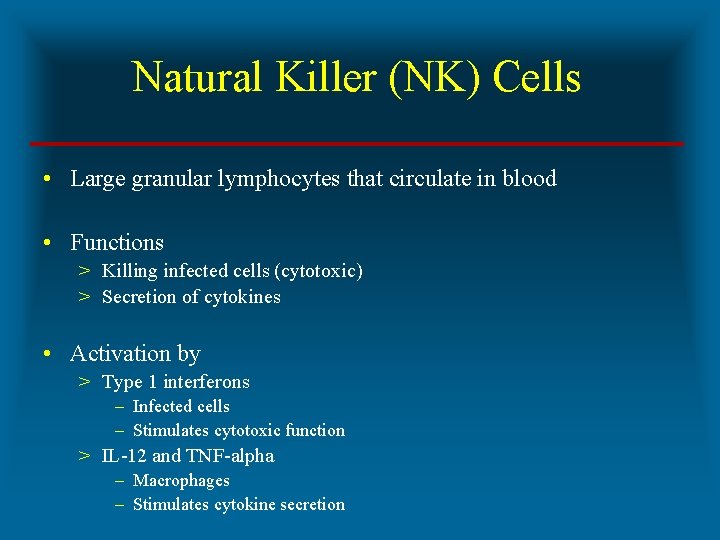
Natural Killer (NK) Cells • Large granular lymphocytes that circulate in blood • Functions > Killing infected cells (cytotoxic) > Secretion of cytokines • Activation by > Type 1 interferons – Infected cells – Stimulates cytotoxic function > IL-12 and TNF-alpha – Macrophages – Stimulates cytokine secretion
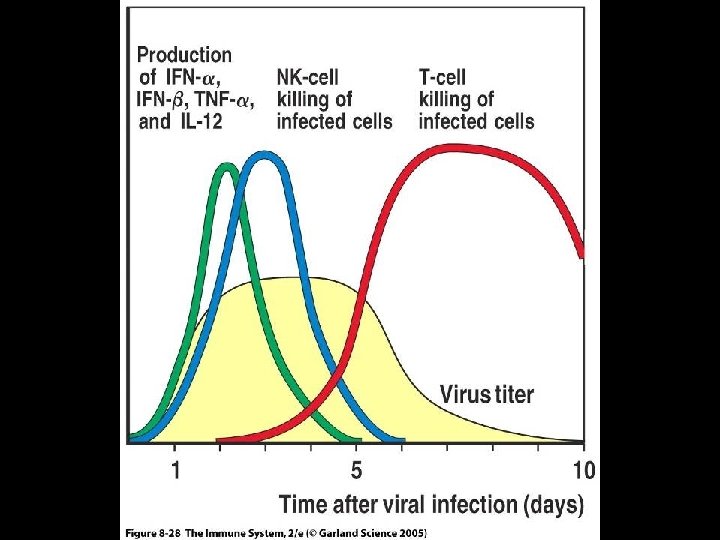
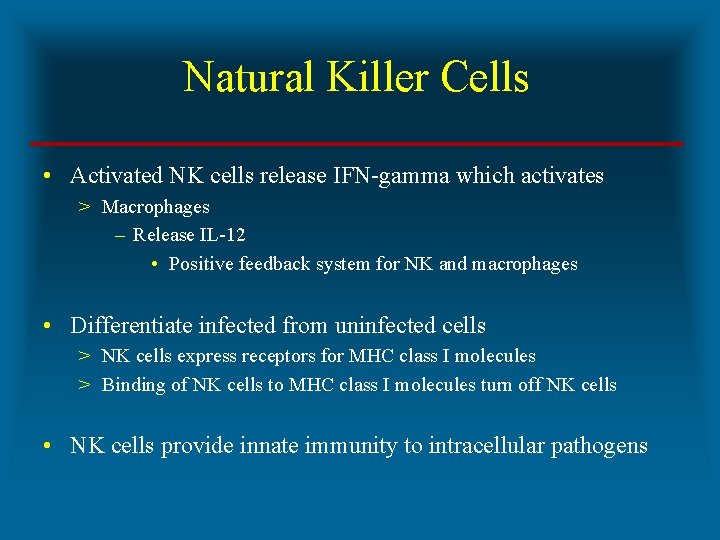
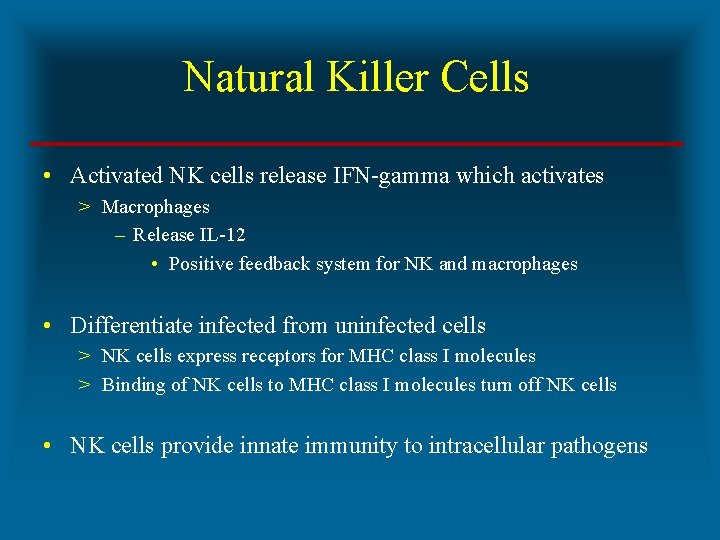
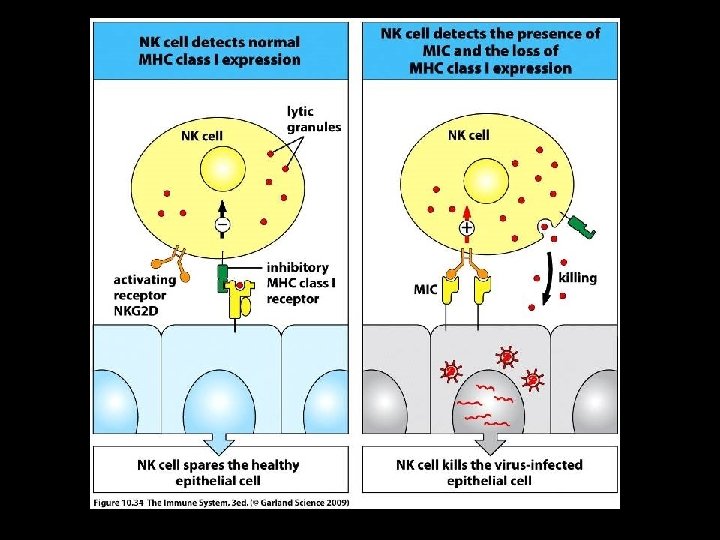
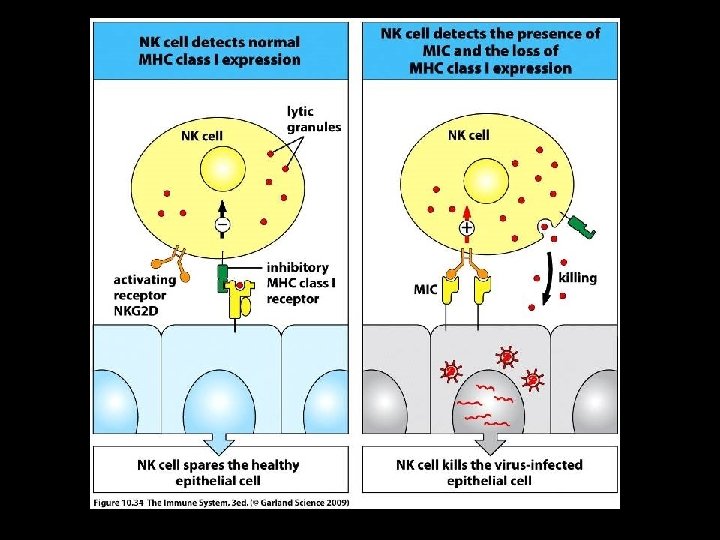
Natural Killer Cells • Activated NK cells release IFN-gamma which activates > Macrophages – Release IL-12 • Positive feedback system for NK and macrophages • Differentiate infected from uninfected cells > NK cells express receptors for MHC class I molecules > Binding of NK cells to MHC class I molecules turn off NK cells • NK cells provide innate immunity to intracellular pathogens
Adaptive Immune Response • Environment for starting provided by innate immune response • Consists of > Primary immune response – Follows initial exposure to antigen – Naive B and T cells – Establishment of memory > Secondary immune response – Follows second exposure to antigen – Memory B and T cells – Utilization of memory
Primary Immune Response • Begins with T cell activation and differentiation in secondary lymphoid tissue > CD 4 TH 1, CD 4 TH 2 and CD 8 – Directed by cytokines • • • IL-12 and IFN-gamma (TH 1) IL-4 and IL-6 (TH 2) Continues with B cell activation in secondary lymphoid tissue > Cognate interaction with CD 4 TH 2 specific for same Ag
Role of T Cells in Primary Immune Response • Effector TH 1 cells > Leave 2 nd lymphoid tissue for infected tissue > Activate destruction of extracellular pathogens by macrophages • Effector CD 8 cells > Leave 2 nd lymphoid tissue for infected tissue > Kill infected cells • Effector TH 2 cells > Remain in 2 nd lymphoid tissue > Stimulates B cell differentiation into plasma cells
Role of B Cells in Primary Immune Response • Differentiation into plasma cells and antibody production • Locations for differentiation following CD 4 TH 2 cognate interaction > Medullary chords of lymph nodes – First wave of antibody secretion > Primary lymphoid follicles – Formation of germinal centers then migration to • Medullary chords of lymph nodes • Bone marrow – Second wave of antibody secretion
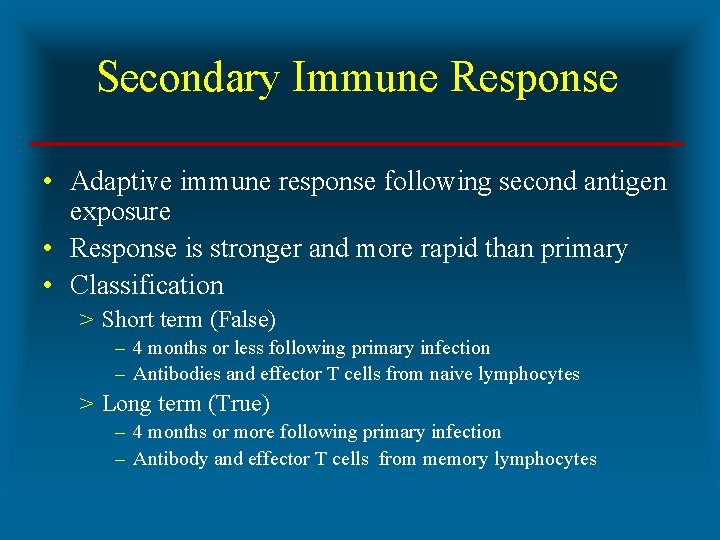
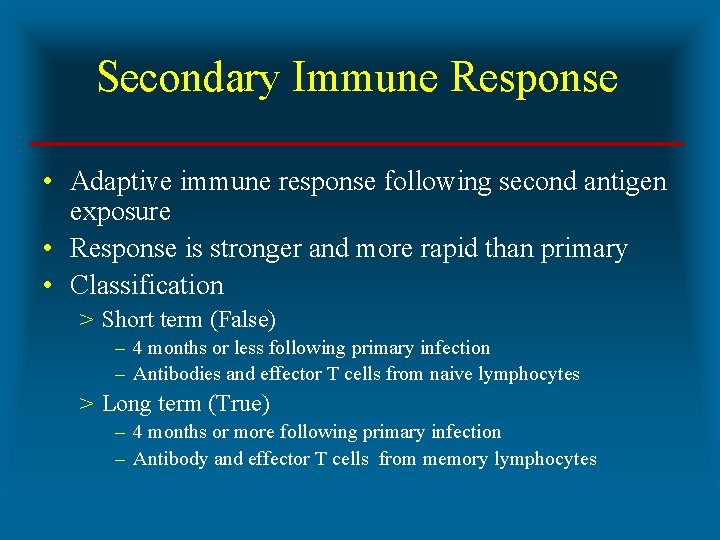
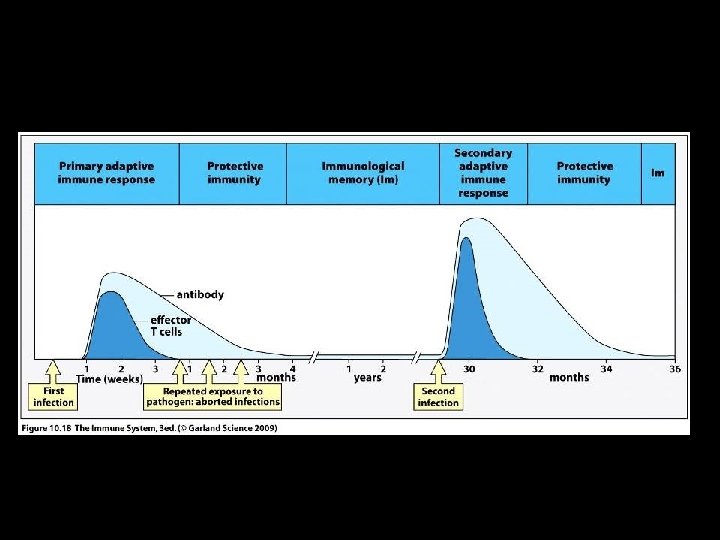
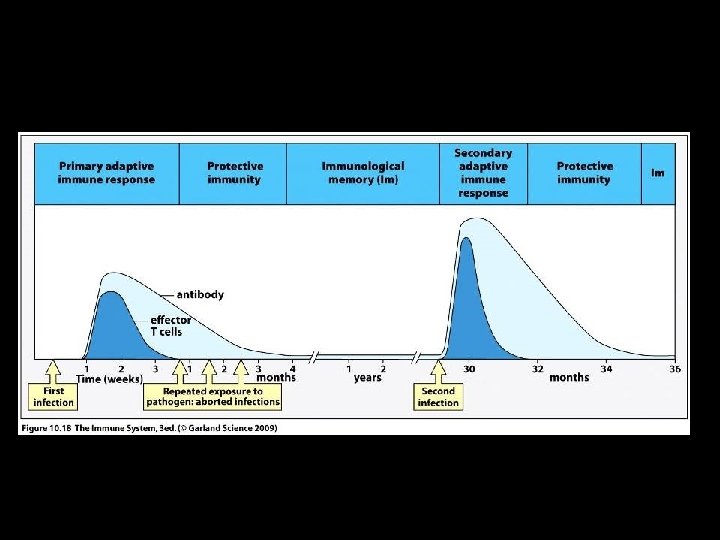
Secondary Immune Response • Adaptive immune response following second antigen exposure • Response is stronger and more rapid than primary • Classification > Short term (False) – 4 months or less following primary infection – Antibodies and effector T cells from naive lymphocytes > Long term (True) – 4 months or more following primary infection – Antibody and effector T cells from memory lymphocytes
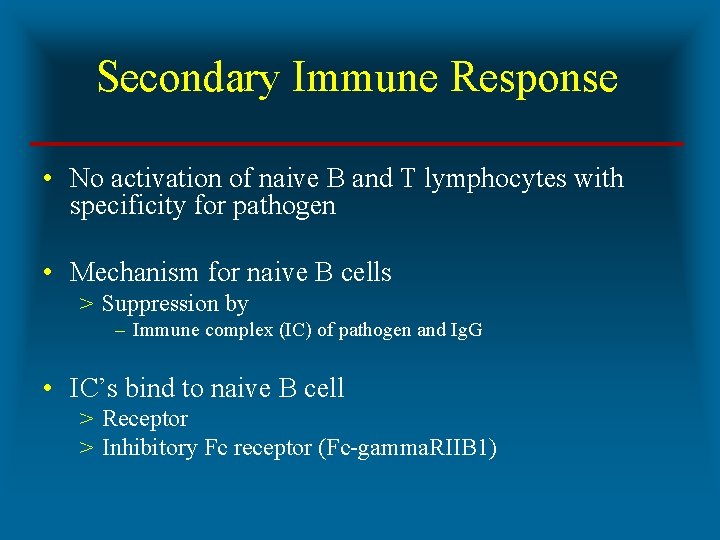
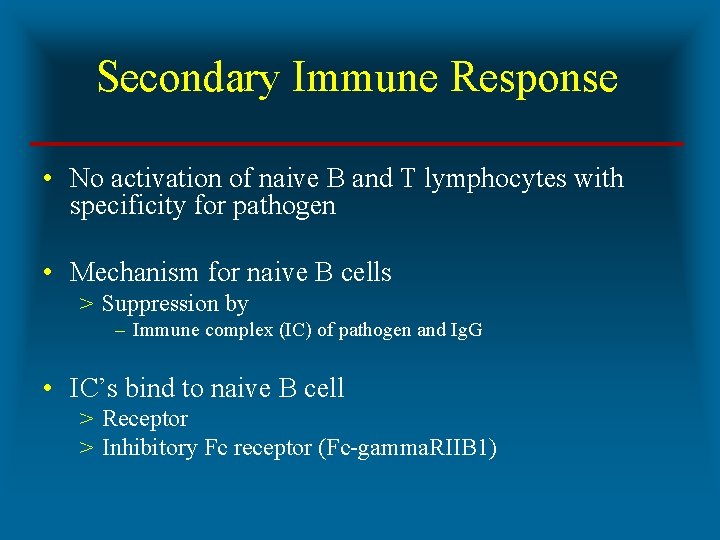
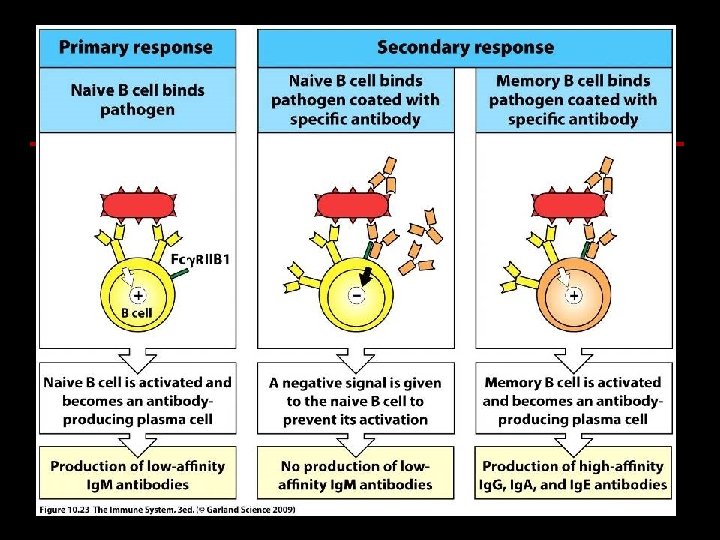
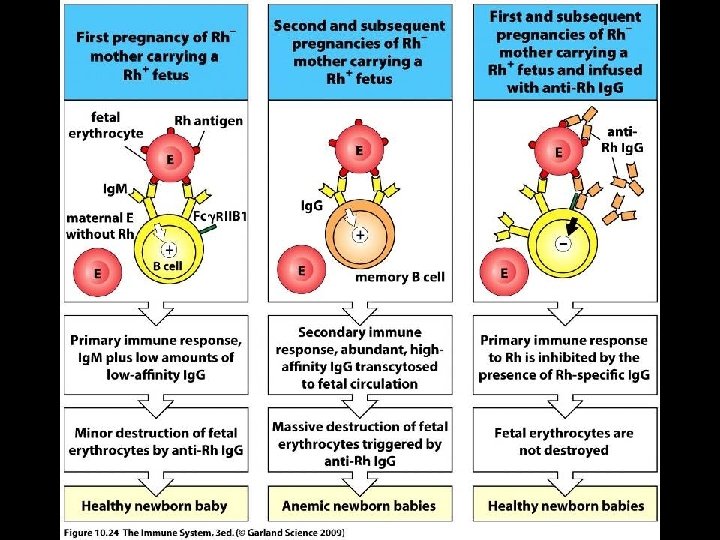
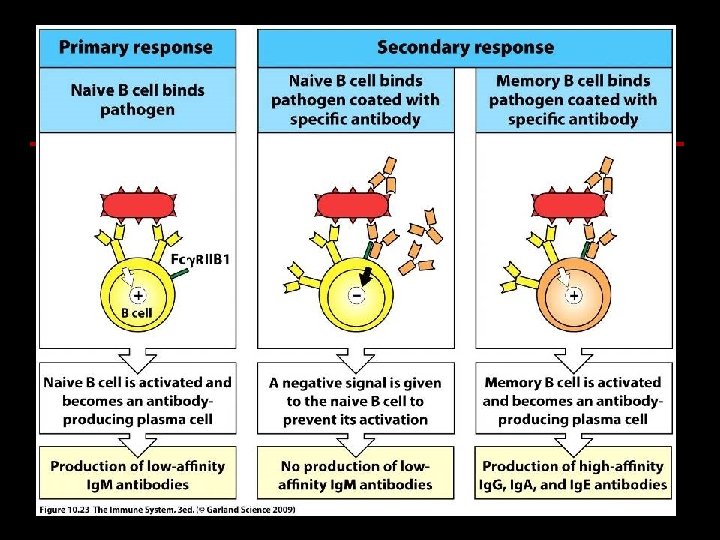
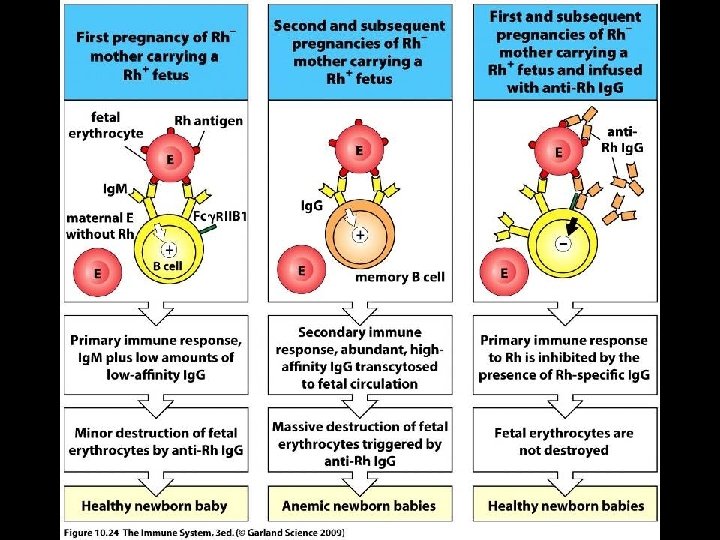
Secondary Immune Response • No activation of naive B and T lymphocytes with specificity for pathogen • Mechanism for naive B cells > Suppression by – Immune complex (IC) of pathogen and Ig. G • IC’s bind to naive B cell > Receptor > Inhibitory Fc receptor (Fc-gamma. RIIB 1)
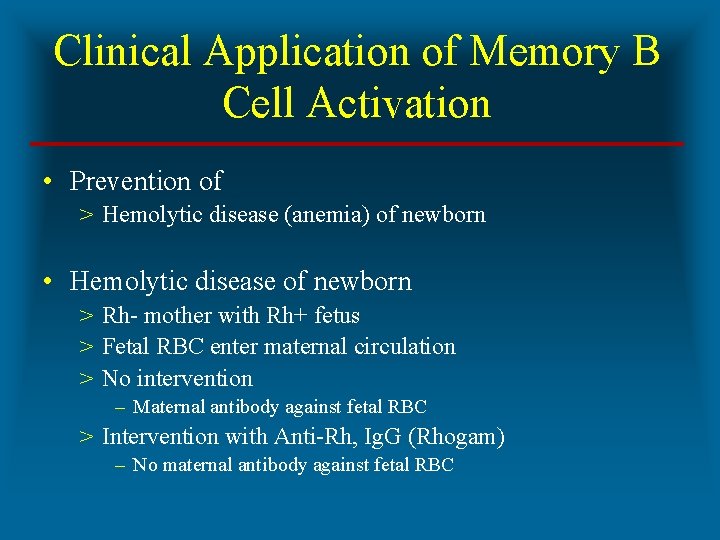
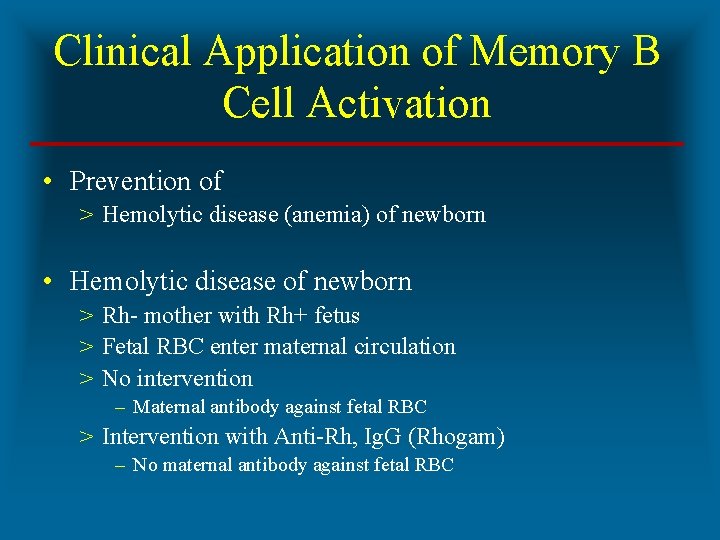
Clinical Application of Memory B Cell Activation • Prevention of > Hemolytic disease (anemia) of newborn • Hemolytic disease of newborn > Rh- mother with Rh+ fetus > Fetal RBC enter maternal circulation > No intervention – Maternal antibody against fetal RBC > Intervention with Anti-Rh, Ig. G (Rhogam) – No maternal antibody against fetal RBC
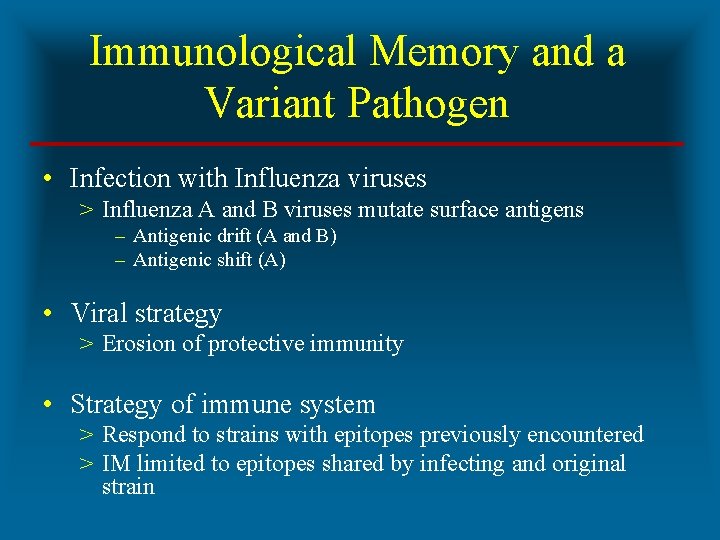
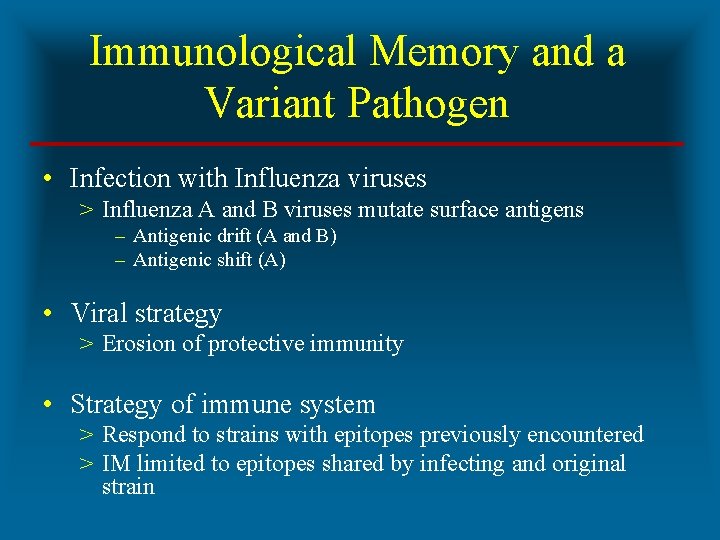
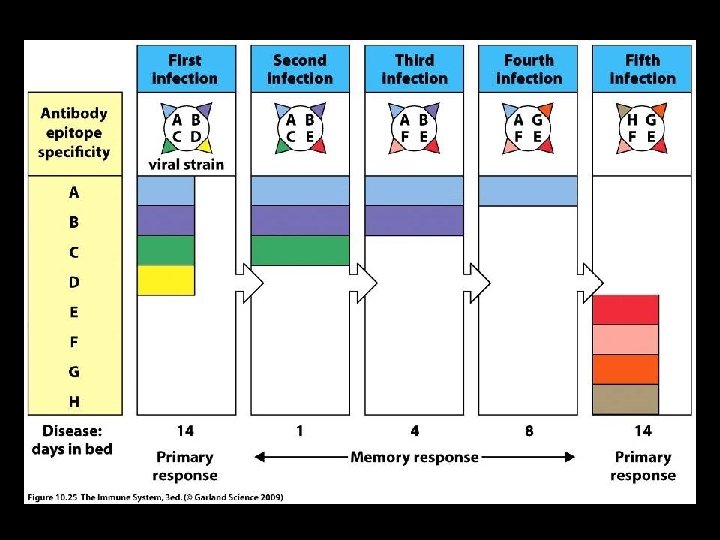
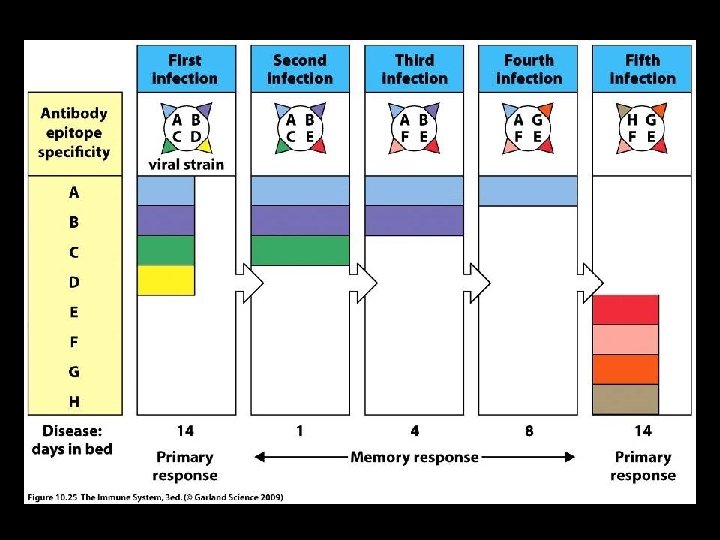
Immunological Memory and a Variant Pathogen • Infection with Influenza viruses > Influenza A and B viruses mutate surface antigens – Antigenic drift (A and B) – Antigenic shift (A) • Viral strategy > Erosion of protective immunity • Strategy of immune system > Respond to strains with epitopes previously encountered > IM limited to epitopes shared by infecting and original strain
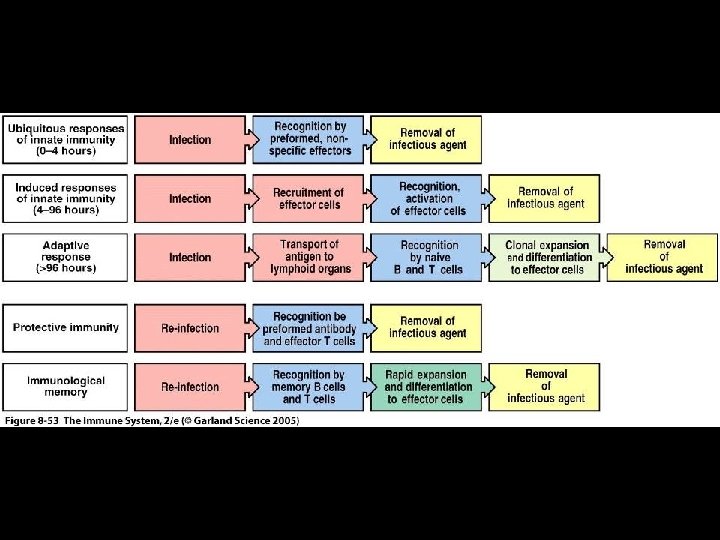
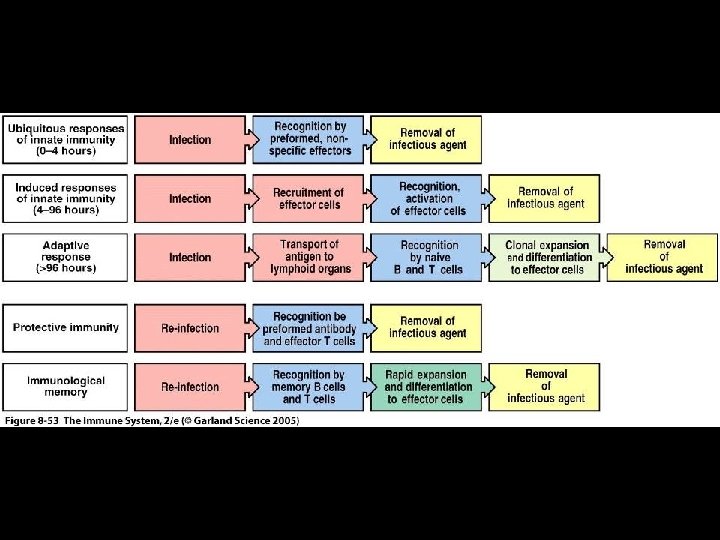
Summary of the Immune Response • Ubiquitous response of innate immunity • Induced response of innate immunity • Adaptive response • Protective immunity • Immunological memory
 Categories of defense mechanisms
Categories of defense mechanisms Chapter 11 health vocabulary
Chapter 11 health vocabulary What are freud's defense mechanisms
What are freud's defense mechanisms Sigmund freud psychodynamic perspective
Sigmund freud psychodynamic perspective Specific defense vs nonspecific defense
Specific defense vs nonspecific defense Projective test example
Projective test example How do sponges protect themselves from predators
How do sponges protect themselves from predators Primitive defense mechanisms
Primitive defense mechanisms Oral fixation examples
Oral fixation examples Freudian defense mechanisms examples
Freudian defense mechanisms examples Ego defense mechanisms
Ego defense mechanisms Psychoanalysis psychology example
Psychoanalysis psychology example The id operates on the ________ principle.
The id operates on the ________ principle. Freuds theories
Freuds theories What are defense mechanisms according to freud?
What are defense mechanisms according to freud? Examples of defence mechanism
Examples of defence mechanism Freud theories
Freud theories Psychoanalytic theory defense mechanisms
Psychoanalytic theory defense mechanisms Female oedipal development klein
Female oedipal development klein Ethical issues in psychiatric nursing
Ethical issues in psychiatric nursing Defense mechanisms nursing
Defense mechanisms nursing Defense mechanisms nursing
Defense mechanisms nursing Freudian analysis
Freudian analysis Anna freud defense mechanisms
Anna freud defense mechanisms Mature defense mechanisms
Mature defense mechanisms Lord of the flies introduction activity
Lord of the flies introduction activity Define human rights
Define human rights Rate fences services marketing
Rate fences services marketing Physical fitness components and tests grade 9
Physical fitness components and tests grade 9 Physical and human characteristics
Physical and human characteristics Compare india and sri lanka on the basis of hdi
Compare india and sri lanka on the basis of hdi Hmsweb
Hmsweb Human made physical systems
Human made physical systems Human vs non human bones
Human vs non human bones 8.3 human needs
8.3 human needs Chapter 8 human needs and human development
Chapter 8 human needs and human development Human development index definition ap human geography
Human development index definition ap human geography Non human nouns
Non human nouns Classes of yeast bread
Classes of yeast bread Hazard statement whmis
Hazard statement whmis Diana lumbrera
Diana lumbrera Macbeth whoosh
Macbeth whoosh Explain the importance of noncompeting labor grades
Explain the importance of noncompeting labor grades Classifications of vegetables
Classifications of vegetables Life roles definition
Life roles definition Iq classification
Iq classification Adultism categories
Adultism categories Unstructured decision
Unstructured decision Cost of quality examples
Cost of quality examples Profit first categories
Profit first categories Eo army
Eo army Mshsl speech categories
Mshsl speech categories Seas application example
Seas application example Two main categories of software
Two main categories of software Six categories of technology
Six categories of technology