Catherine Hayhurst MCA AND MHA IN THE ED

- Slides: 24
Catherine Hayhurst MCA AND MHA IN THE ED
Definitions � To have mental capacity is the ability to make an informed decision. � Capacity is decision specific. � To have capacity, a person has to be able to: �Understand the information around the decision �Retain that information �Weigh that information �Communicate the decision
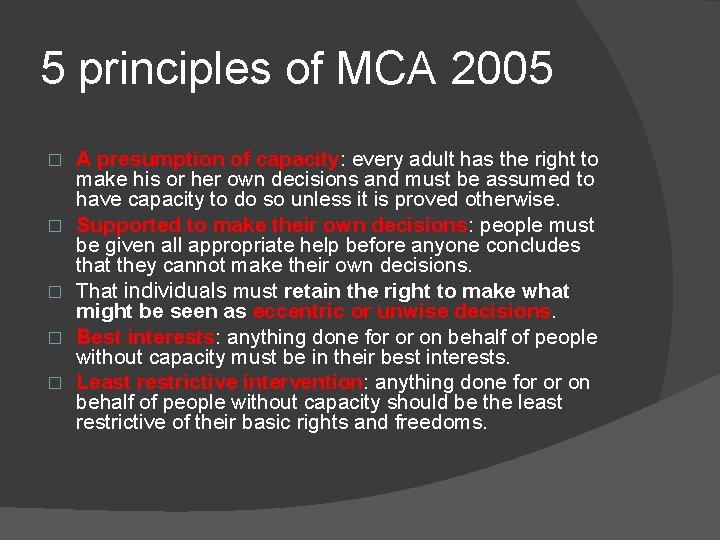
5 principles of MCA 2005 � � � A presumption of capacity: every adult has the right to make his or her own decisions and must be assumed to have capacity to do so unless it is proved otherwise. Supported to make their own decisions: people must be given all appropriate help before anyone concludes that they cannot make their own decisions. That individuals must retain the right to make what might be seen as eccentric or unwise decisions. Best interests: anything done for or on behalf of people without capacity must be in their best interests. Least restrictive intervention: anything done for or on behalf of people without capacity should be the least restrictive of their basic rights and freedoms.
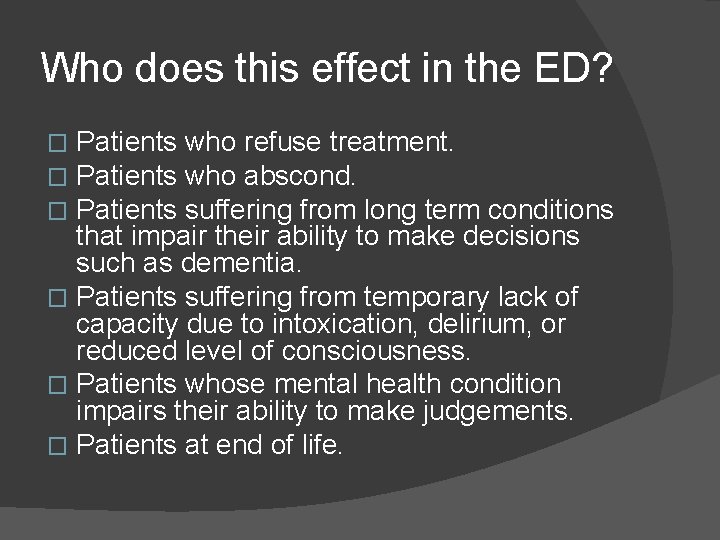
Who does this effect in the ED? Patients who refuse treatment. Patients who abscond. Patients suffering from long term conditions that impair their ability to make decisions such as dementia. � Patients suffering from temporary lack of capacity due to intoxication, delirium, or reduced level of consciousness. � Patients whose mental health condition impairs their ability to make judgements. � Patients at end of life. � � �
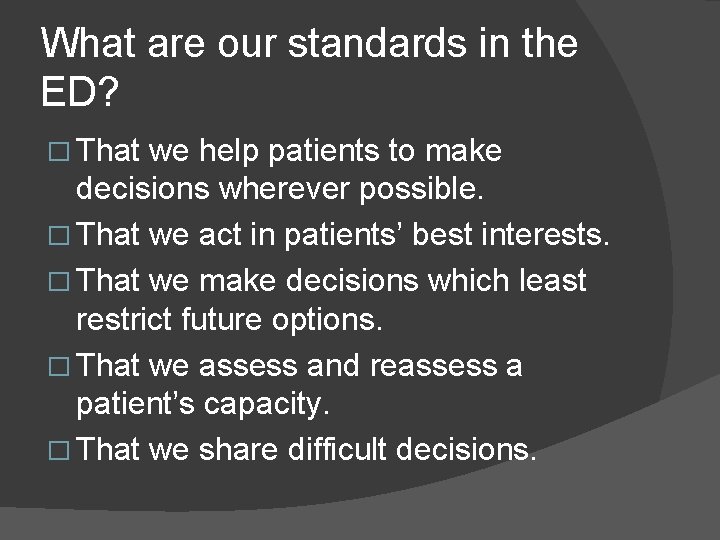
What are our standards in the ED? � That we help patients to make decisions wherever possible. � That we act in patients’ best interests. � That we make decisions which least restrict future options. � That we assess and reassess a patient’s capacity. � That we share difficult decisions.
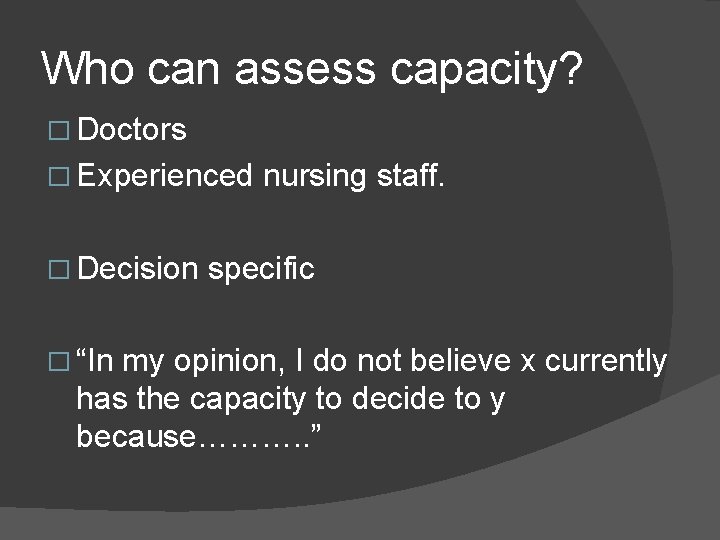
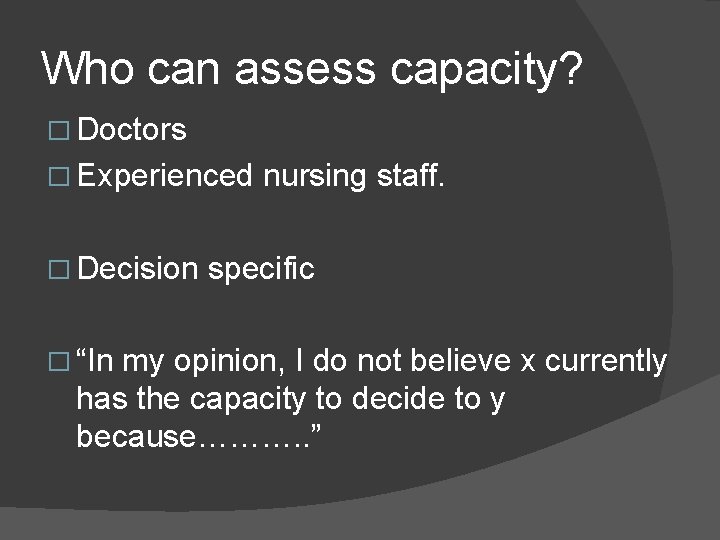
Who can assess capacity? � Doctors � Experienced � Decision � “In nursing staff. specific my opinion, I do not believe x currently has the capacity to decide to y because………. . ”
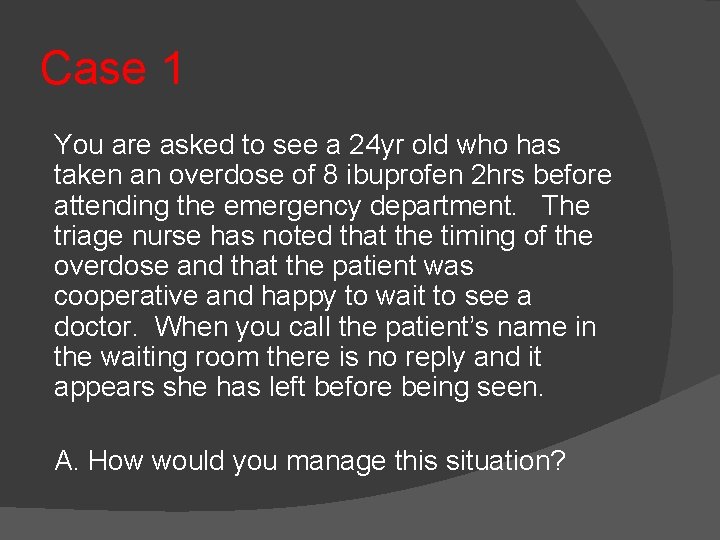
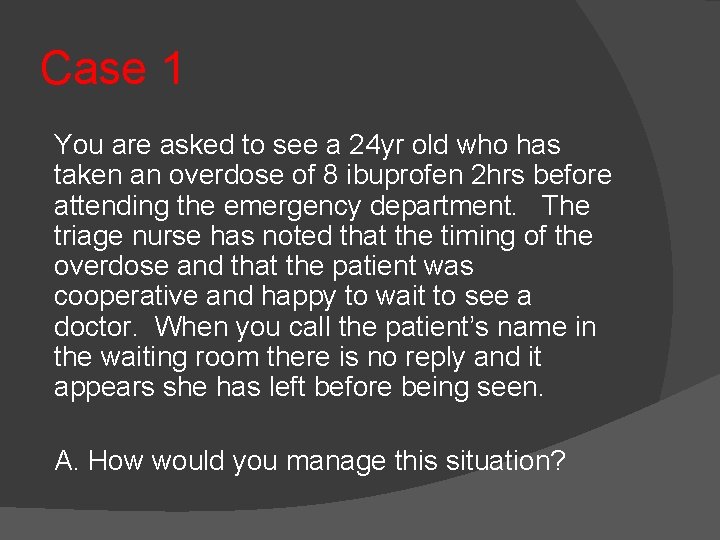
Case 1 You are asked to see a 24 yr old who has taken an overdose of 8 ibuprofen 2 hrs before attending the emergency department. The triage nurse has noted that the timing of the overdose and that the patient was cooperative and happy to wait to see a doctor. When you call the patient’s name in the waiting room there is no reply and it appears she has left before being seen. A. How would you manage this situation?
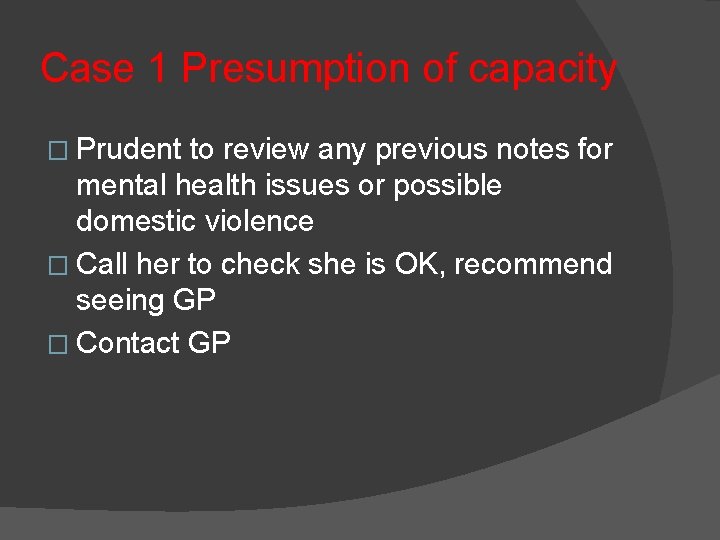
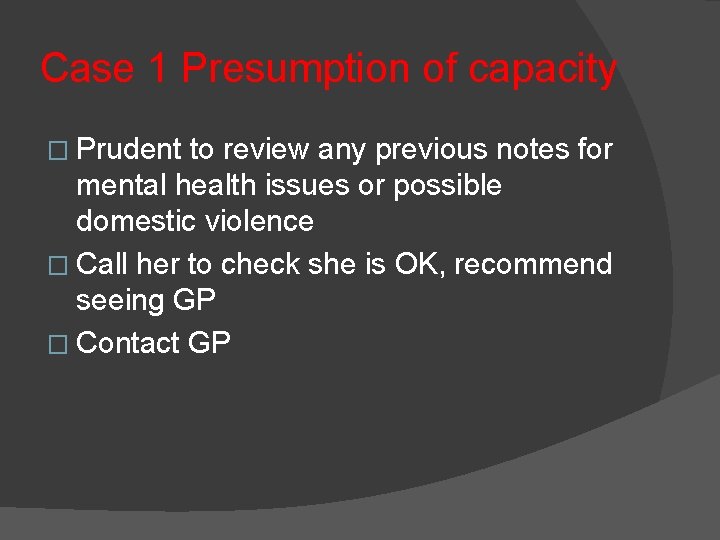
Case 1 Presumption of capacity � Prudent to review any previous notes for mental health issues or possible domestic violence � Call her to check she is OK, recommend seeing GP � Contact GP
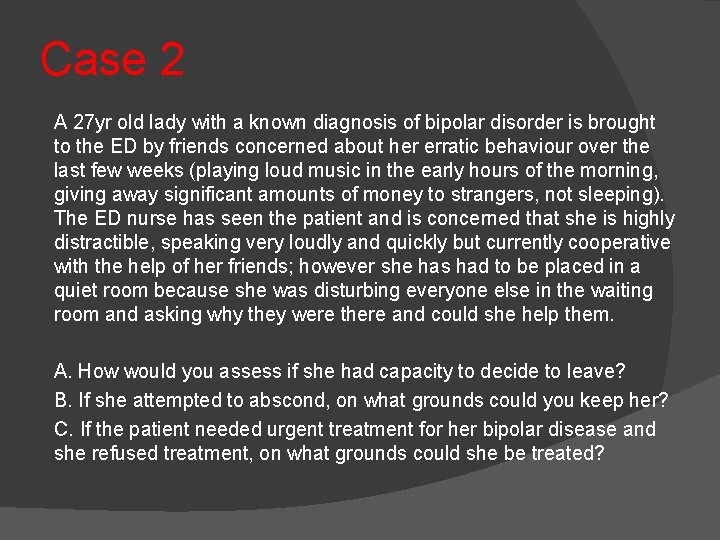
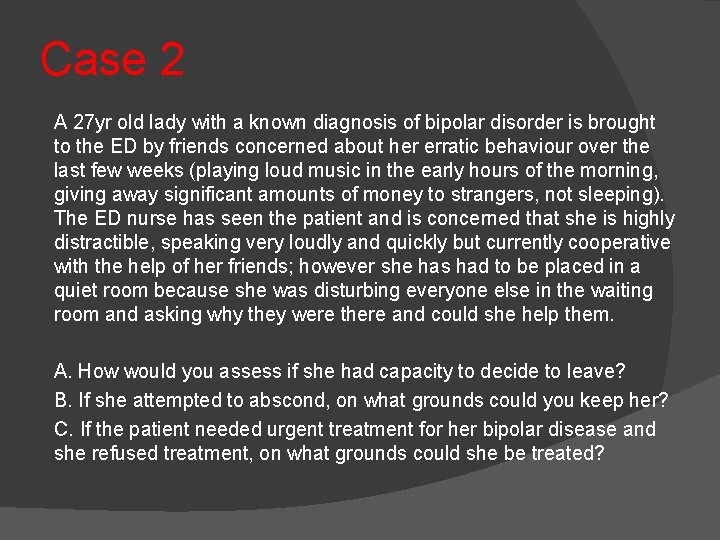
Case 2 A 27 yr old lady with a known diagnosis of bipolar disorder is brought to the ED by friends concerned about her erratic behaviour over the last few weeks (playing loud music in the early hours of the morning, giving away significant amounts of money to strangers, not sleeping). The ED nurse has seen the patient and is concerned that she is highly distractible, speaking very loudly and quickly but currently cooperative with the help of her friends; however she has had to be placed in a quiet room because she was disturbing everyone else in the waiting room and asking why they were there and could she help them. A. How would you assess if she had capacity to decide to leave? B. If she attempted to abscond, on what grounds could you keep her? C. If the patient needed urgent treatment for her bipolar disease and she refused treatment, on what grounds could she be treated?
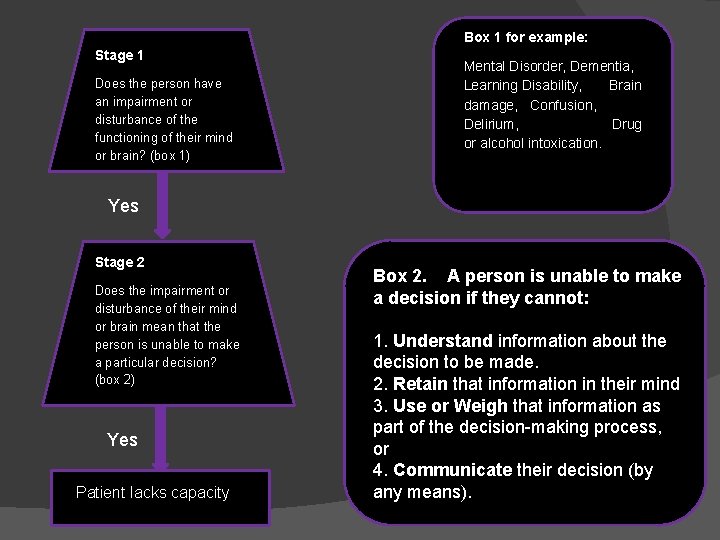
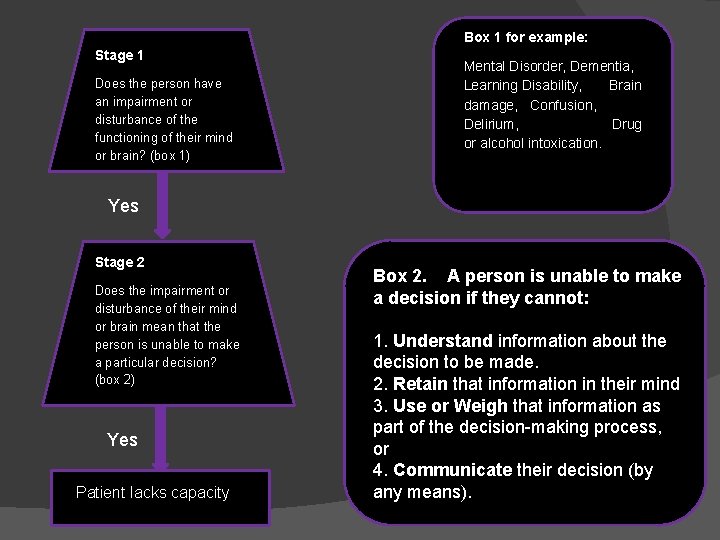
Box 1 for example: Stage 1 Does the person have an impairment or disturbance of the functioning of their mind or brain? (box 1) Mental Disorder, Dementia, Learning Disability, Brain damage, Confusion, Delirium, Drug or alcohol intoxication. Yes Stage 2 Does the impairment or disturbance of their mind or brain mean that the person is unable to make a particular decision? (box 2) Yes Patient lacks capacity Box 2. A person is unable to make a decision if they cannot: 1. Understand information about the decision to be made. 2. Retain that information in their mind 3. Use or Weigh that information as part of the decision-making process, or 4. Communicate their decision (by any means).
� MCA – grounds for keeping her, but not for treating her. � Ideally do not use MCA for too long for MH patients. Ask for MHA assessment as this provides a detailed assessment with the patient’s welfare in mind. � Section 5. 2 of MHA used to hold patients for assessment for 72 hours – can only be used on a ward. � Full MHA assessment – section 2 or 3 can be used for Rx.
Case 3 An 18 yr old man has been found wandering semi-naked on a busy road having tried to cut his arm. The police have brought him to the ED because they are concerned about his wound and his welfare. He is clearly highly agitated and the triage nurse has requested that a doctor assess him immediately. He is generally uncooperative and in-attentive and he has not allowed the nurse to obtain any baseline observations and is not responding to direct questioning. A quick search of the ED computer system has shown that he has a past history of schizophrenia and a few attendances related to drug ingestion. A. B. C. D. E. F. What would you ask the police officers? When can the police officers leave? If he tries to leave, on what grounds can you restrain him? In terms of the restraint, what options are open to you? What if a patient like this had tried to leave saying he planned to hurt someone? What if a patient like this had tried to leave before you had a chance to assess his capacity or mental state?
What is a section 136?
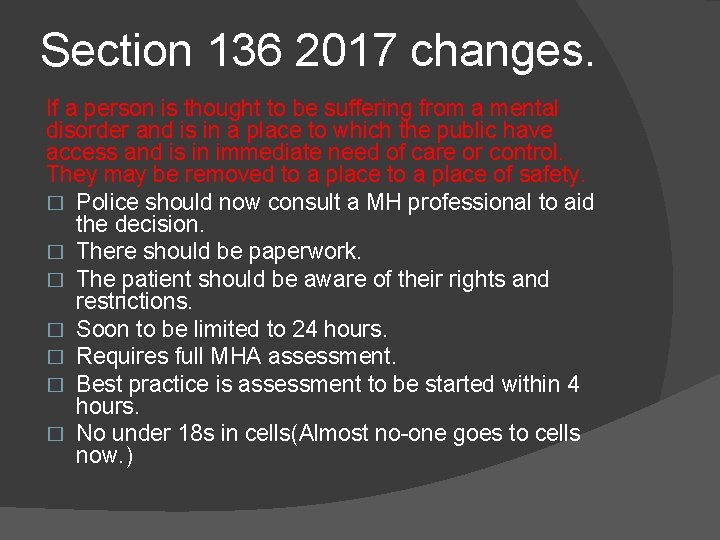
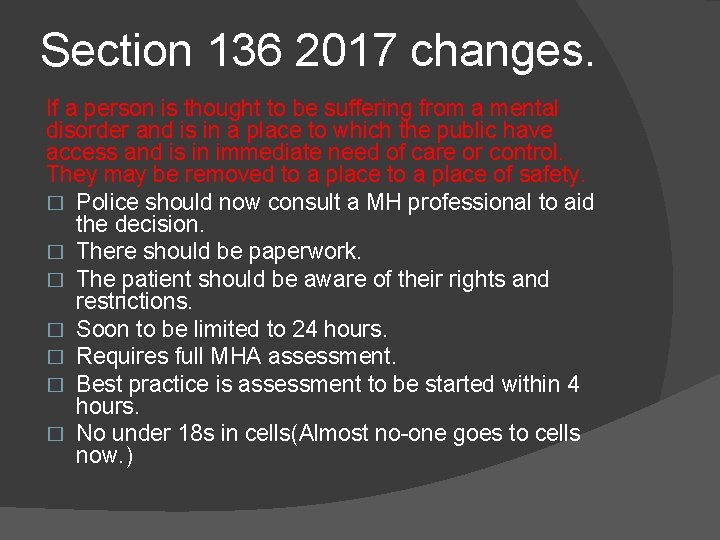
Section 136 2017 changes. If a person is thought to be suffering from a mental disorder and is in a place to which the public have access and is in immediate need of care or control. They may be removed to a place of safety. � Police should now consult a MH professional to aid the decision. � There should be paperwork. � The patient should be aware of their rights and restrictions. � Soon to be limited to 24 hours. � Requires full MHA assessment. � Best practice is assessment to be started within 4 hours. � No under 18 s in cells(Almost no-one goes to cells now. )
Section 136 � Police bringing in a patient from the community with mental health problems should be using a 136 unless… �They have truly come voluntarily (rare). �They have brought the patient as they lack capacity. (potentially tricky as 136 may be more appropriate. ) �The ambulance crew have merely asked police to follow behind for back up
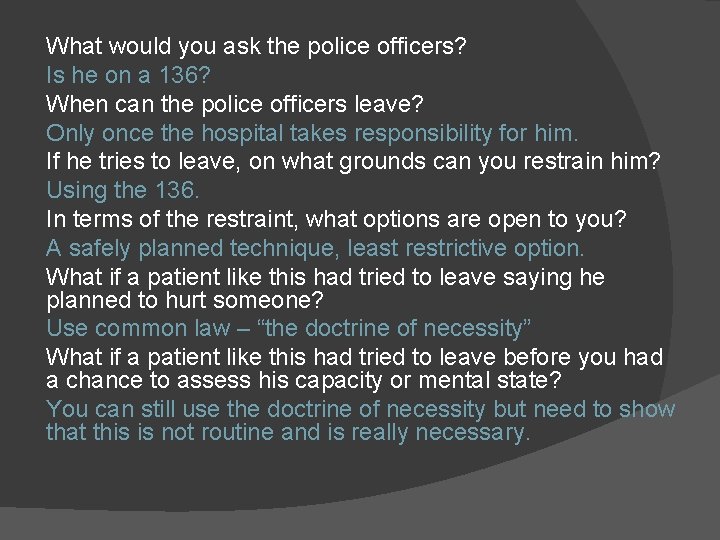
What would you ask the police officers? Is he on a 136? When can the police officers leave? Only once the hospital takes responsibility for him. If he tries to leave, on what grounds can you restrain him? Using the 136. In terms of the restraint, what options are open to you? A safely planned technique, least restrictive option. What if a patient like this had tried to leave saying he planned to hurt someone? Use common law – “the doctrine of necessity” What if a patient like this had tried to leave before you had a chance to assess his capacity or mental state? You can still use the doctrine of necessity but need to show that this is not routine and is really necessary.
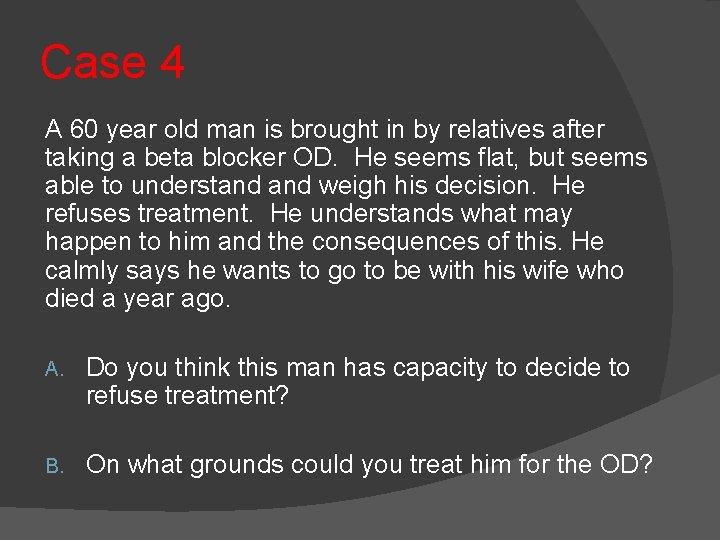
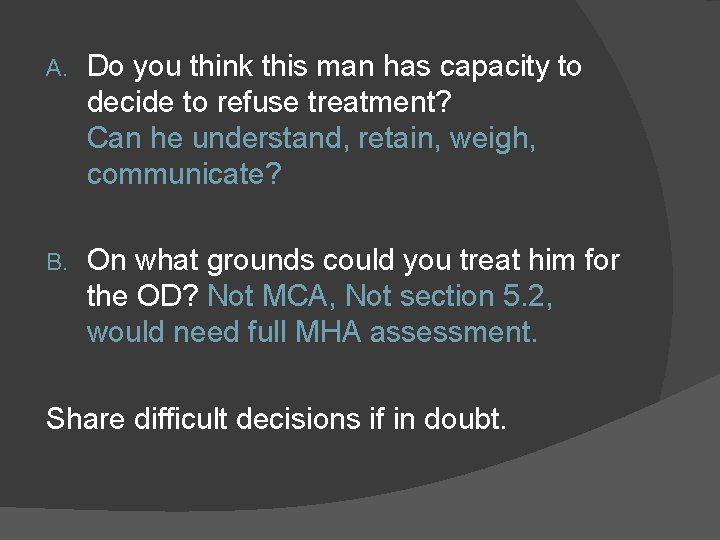
Case 4 A 60 year old man is brought in by relatives after taking a beta blocker OD. He seems flat, but seems able to understand weigh his decision. He refuses treatment. He understands what may happen to him and the consequences of this. He calmly says he wants to go to be with his wife who died a year ago. A. Do you think this man has capacity to decide to refuse treatment? B. On what grounds could you treat him for the OD?
A. Do you think this man has capacity to decide to refuse treatment? Can he understand, retain, weigh, communicate? B. On what grounds could you treat him for the OD? Not MCA, Not section 5. 2, would need full MHA assessment. Share difficult decisions if in doubt.
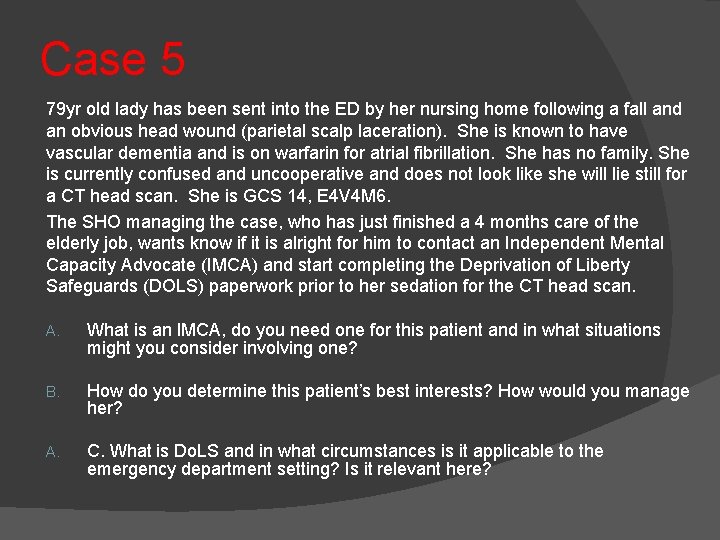
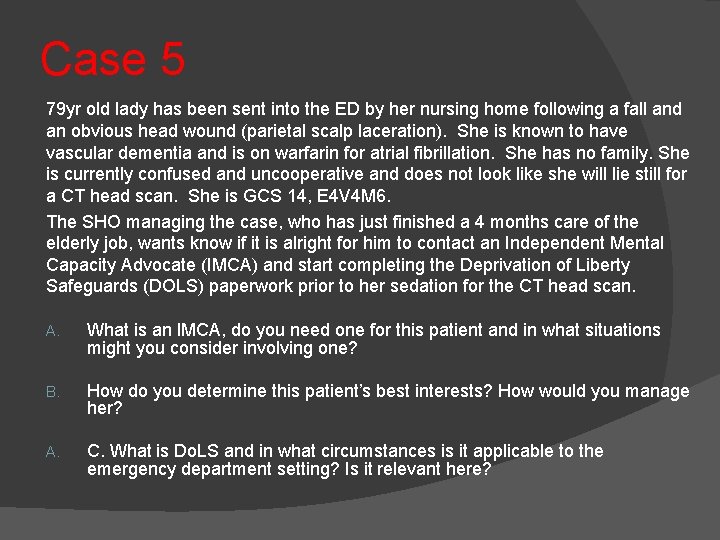
Case 5 79 yr old lady has been sent into the ED by her nursing home following a fall and an obvious head wound (parietal scalp laceration). She is known to have vascular dementia and is on warfarin for atrial fibrillation. She has no family. She is currently confused and uncooperative and does not look like she will lie still for a CT head scan. She is GCS 14, E 4 V 4 M 6. The SHO managing the case, who has just finished a 4 months care of the elderly job, wants know if it is alright for him to contact an Independent Mental Capacity Advocate (IMCA) and start completing the Deprivation of Liberty Safeguards (DOLS) paperwork prior to her sedation for the CT head scan. A. What is an IMCA, do you need one for this patient and in what situations might you consider involving one? B. How do you determine this patient’s best interests? How would you manage her? A. C. What is Do. LS and in what circumstances is it applicable to the emergency department setting? Is it relevant here?
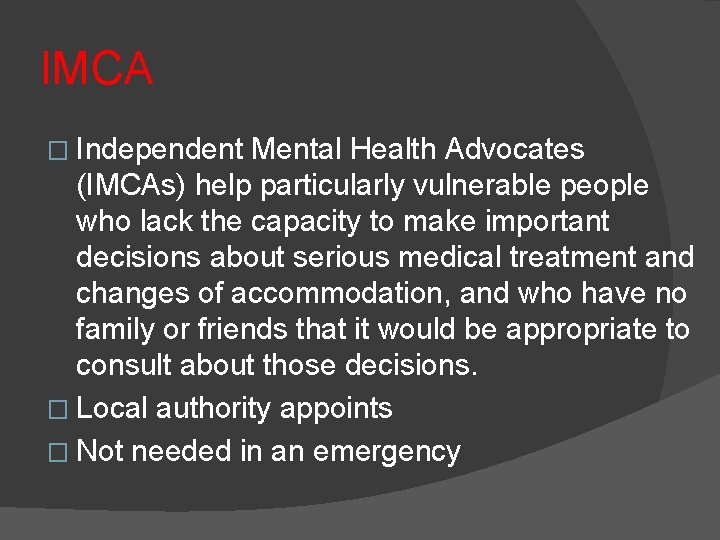
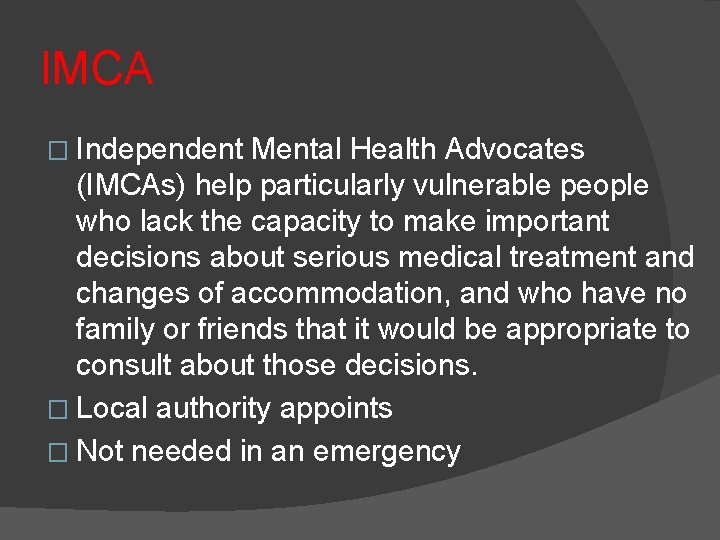
IMCA � Independent Mental Health Advocates (IMCAs) help particularly vulnerable people who lack the capacity to make important decisions about serious medical treatment and changes of accommodation, and who have no family or friends that it would be appropriate to consult about those decisions. � Local authority appoints � Not needed in an emergency
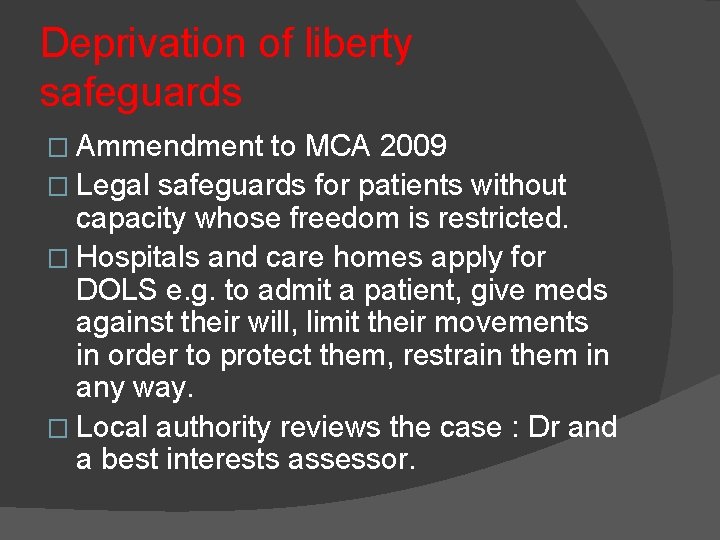
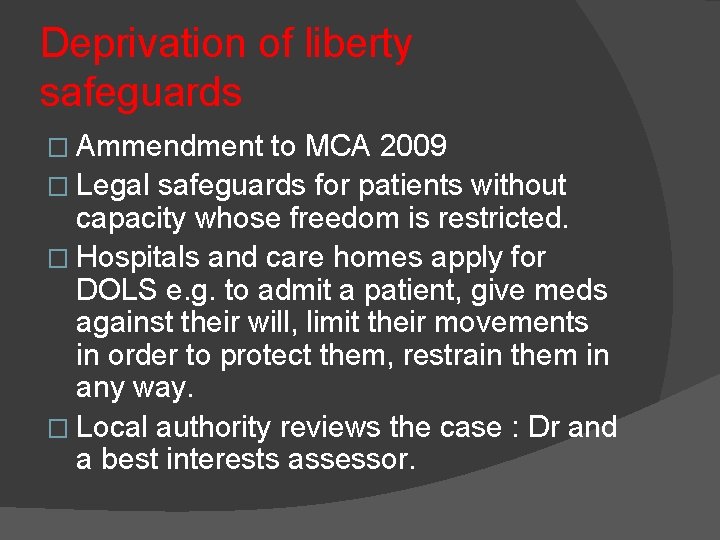
Deprivation of liberty safeguards � Ammendment to MCA 2009 � Legal safeguards for patients without capacity whose freedom is restricted. � Hospitals and care homes apply for DOLS e. g. to admit a patient, give meds against their will, limit their movements in order to protect them, restrain them in any way. � Local authority reviews the case : Dr and a best interests assessor.
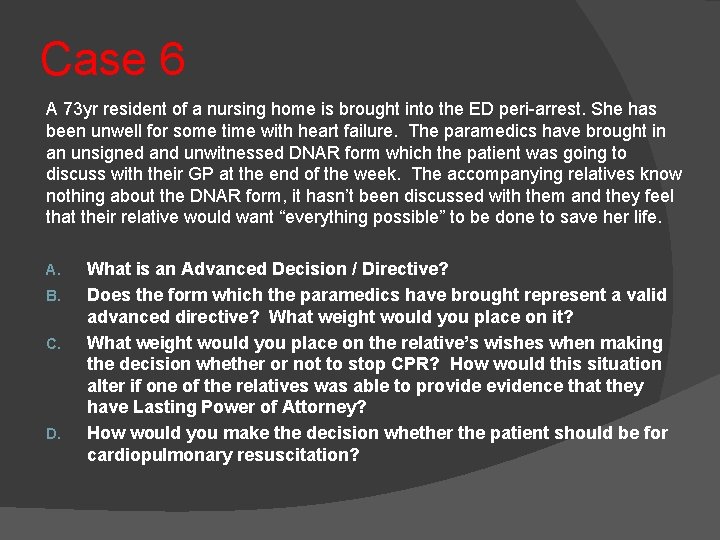
Case 6 A 73 yr resident of a nursing home is brought into the ED peri-arrest. She has been unwell for some time with heart failure. The paramedics have brought in an unsigned and unwitnessed DNAR form which the patient was going to discuss with their GP at the end of the week. The accompanying relatives know nothing about the DNAR form, it hasn’t been discussed with them and they feel that their relative would want “everything possible” to be done to save her life. A. B. C. D. What is an Advanced Decision / Directive? Does the form which the paramedics have brought represent a valid advanced directive? What weight would you place on it? What weight would you place on the relative’s wishes when making the decision whether or not to stop CPR? How would this situation alter if one of the relatives was able to provide evidence that they have Lasting Power of Attorney? How would you make the decision whether the patient should be for cardiopulmonary resuscitation?

Summary � Early assessment � Share difficult decisions � Document well � Be clear when you are using MCA and when MHA.
 Catherine hayhurst
Catherine hayhurst Mca and dols
Mca and dols Mha patrilineal
Mha patrilineal Gmu health informatics
Gmu health informatics Maria ha
Maria ha Mrrn
Mrrn Mha equipment
Mha equipment Carrie bradford
Carrie bradford Tonya mha
Tonya mha Sue mha
Sue mha Mha discussion
Mha discussion Mha kaç cilt
Mha kaç cilt Statutory principles of the mca
Statutory principles of the mca Statutory principles of the mca
Statutory principles of the mca Mca software engineering
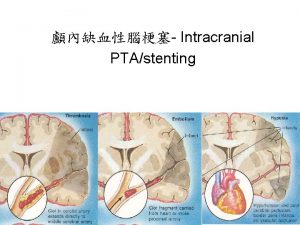
Mca software engineering Medial striate artery
Medial striate artery Emav-mca
Emav-mca Master 500 gt near coastal
Master 500 gt near coastal Mca court
Mca court Dr martin mca
Dr martin mca Sah subarachnoid hemorrhage
Sah subarachnoid hemorrhage Hyperdense mca
Hyperdense mca Aka.ms/mca マイクロソフト
Aka.ms/mca マイクロソフト 5 principles of the mental capacity act
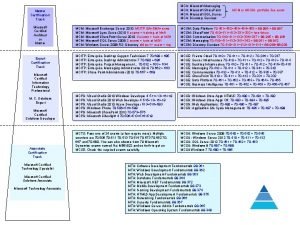
5 principles of the mental capacity act Mca diagram
Mca diagram