MCA DOLs Consent Dr Martin Curtice Consultant in



![Incapacitatedly autonomous Wye Valley NHS Trust v B [2015] EWCOP 60 • 28 th Incapacitatedly autonomous Wye Valley NHS Trust v B [2015] EWCOP 60 • 28 th](https://slidetodoc.com/presentation_image/275d772ac839eb5af713bdfcd44abb1f/image-20.jpg)
![Montgomery v Lanarkshire [2015] • Diabetic mother – shoulder dystocia during birth • Mother Montgomery v Lanarkshire [2015] • Diabetic mother – shoulder dystocia during birth • Mother](https://slidetodoc.com/presentation_image/275d772ac839eb5af713bdfcd44abb1f/image-28.jpg)
![Montgomery v Lanarkshire [2015] • What is a material risk? • It is a Montgomery v Lanarkshire [2015] • What is a material risk? • It is a](https://slidetodoc.com/presentation_image/275d772ac839eb5af713bdfcd44abb1f/image-29.jpg)
![Montgomery v Lanarkshire [2015] • A pro forma ‘scripted’ approach to consent is a Montgomery v Lanarkshire [2015] • A pro forma ‘scripted’ approach to consent is a](https://slidetodoc.com/presentation_image/275d772ac839eb5af713bdfcd44abb1f/image-30.jpg)
![Montgomery v Lanarkshire [2015] Exceptions to disclosure 1. The patient might tell the doctor Montgomery v Lanarkshire [2015] Exceptions to disclosure 1. The patient might tell the doctor](https://slidetodoc.com/presentation_image/275d772ac839eb5af713bdfcd44abb1f/image-31.jpg)
![Montgomery v Lanarkshire [2015] So for capacitous & consenting patients 1. Does the patient Montgomery v Lanarkshire [2015] So for capacitous & consenting patients 1. Does the patient](https://slidetodoc.com/presentation_image/275d772ac839eb5af713bdfcd44abb1f/image-32.jpg)
![Do. LS and covert administration of medication AG v BMBC & Anor [2016] EWCOP Do. LS and covert administration of medication AG v BMBC & Anor [2016] EWCOP](https://slidetodoc.com/presentation_image/275d772ac839eb5af713bdfcd44abb1f/image-33.jpg)

- Slides: 36

MCA & DOLs & Consent Dr Martin Curtice Consultant in old age psychiatry MBCh. B LLM FRCPsych
Brief Bio • • Consultant 2003 BSMHFT HACW 2013 DGM Examiner LLM Mental Health Law Research: Mental Health Law; EOLC Human Rights Act 1998/ECHR 80+ publications 2
Introduction • Case examples • MCA 2005 – main principles • DOLs – current principles • Montgomery v Lanarkshire [2015] UKSC • Wye Valley NHS Trust v B [2015] • Do. LS and covert medication 3
Oh no not lawyery stuff…. 4
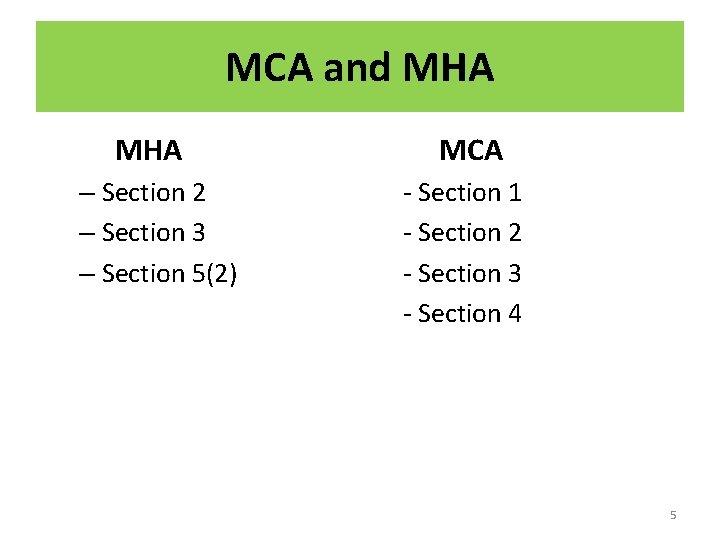
MCA and MHA – Section 2 – Section 3 – Section 5(2) MCA - Section 1 - Section 2 - Section 3 - Section 4 5
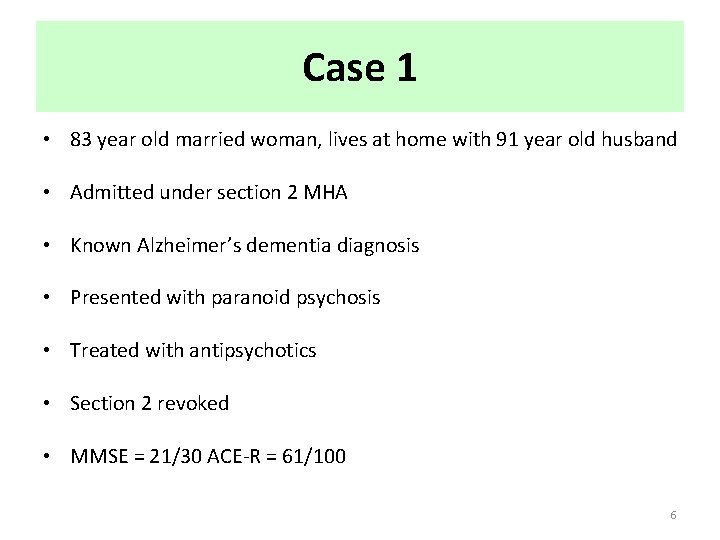
Case 1 • 83 year old married woman, lives at home with 91 year old husband • Admitted under section 2 MHA • Known Alzheimer’s dementia diagnosis • Presented with paranoid psychosis • Treated with antipsychotics • Section 2 revoked • MMSE = 21/30 ACE-R = 61/100 6

Case 1 • Husband was in respite care due to physical illness and there were safeguarding issues around the family input (finances) • Prior to admission significant neglect of the home over several months (cat died) – needed deep clean • Family disharmony over welfare issues • How would you go about assessing her capacity to make welfare decisions to be discharged from the ward? 7
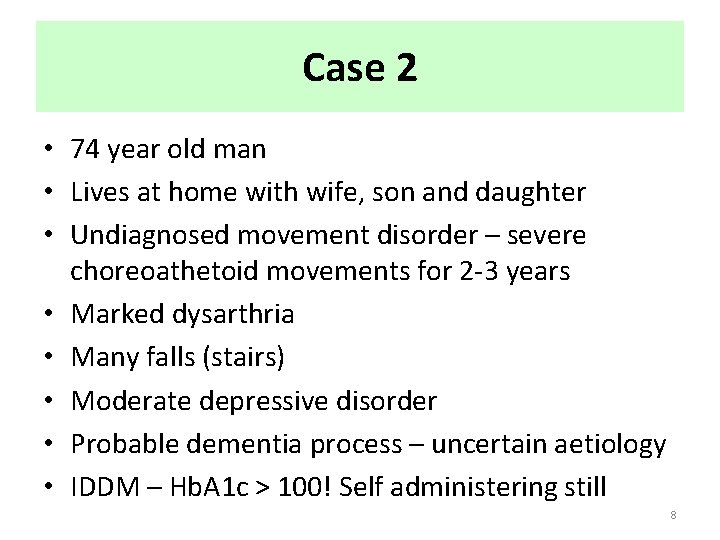
Case 2 • 74 year old man • Lives at home with wife, son and daughter • Undiagnosed movement disorder – severe choreoathetoid movements for 2 -3 years • Marked dysarthria • Many falls (stairs) • Moderate depressive disorder • Probable dementia process – uncertain aetiology • IDDM – Hb. A 1 c > 100! Self administering still 8
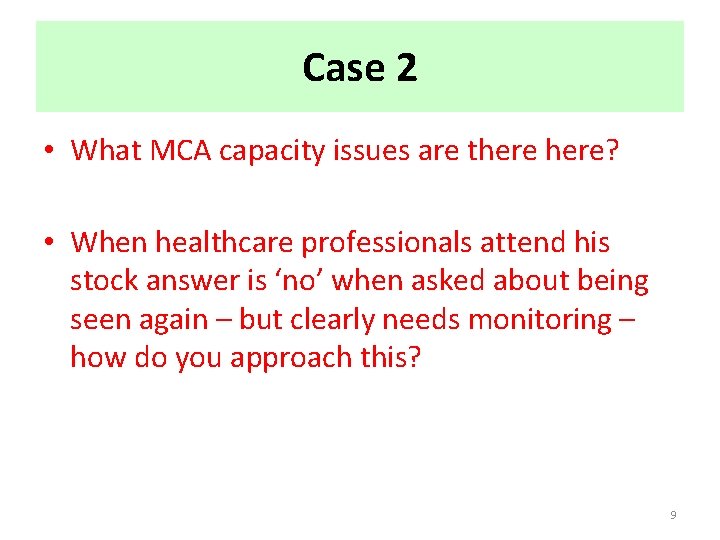
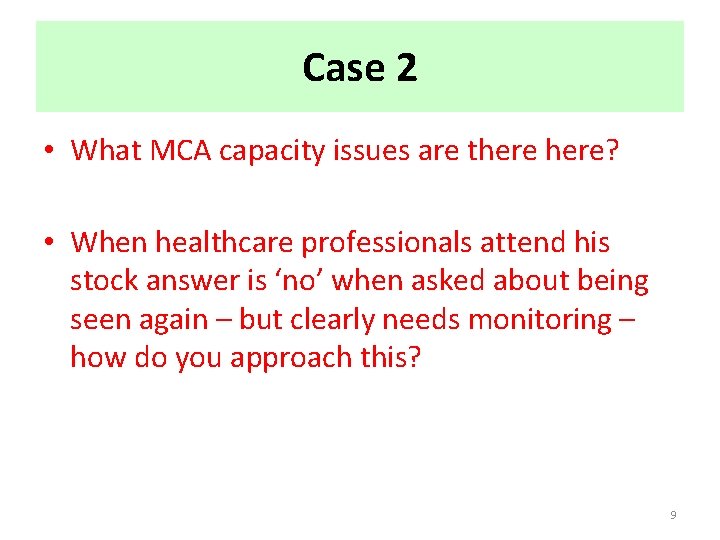
Case 2 • What MCA capacity issues are there? • When healthcare professionals attend his stock answer is ‘no’ when asked about being seen again – but clearly needs monitoring – how do you approach this? 9
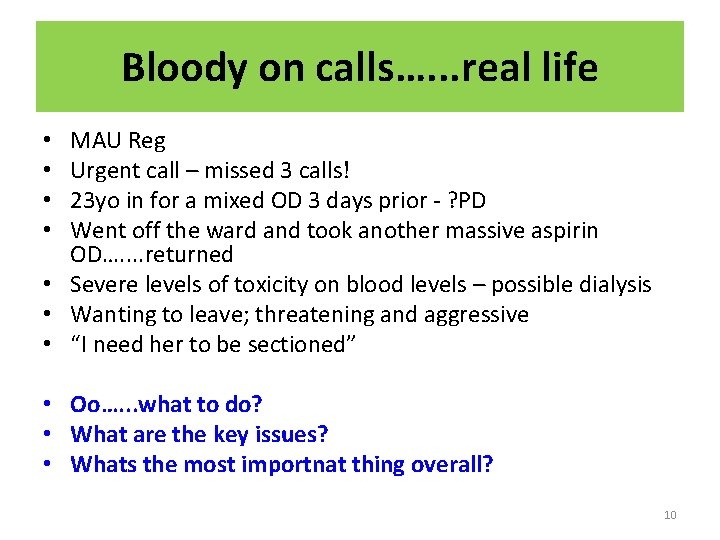
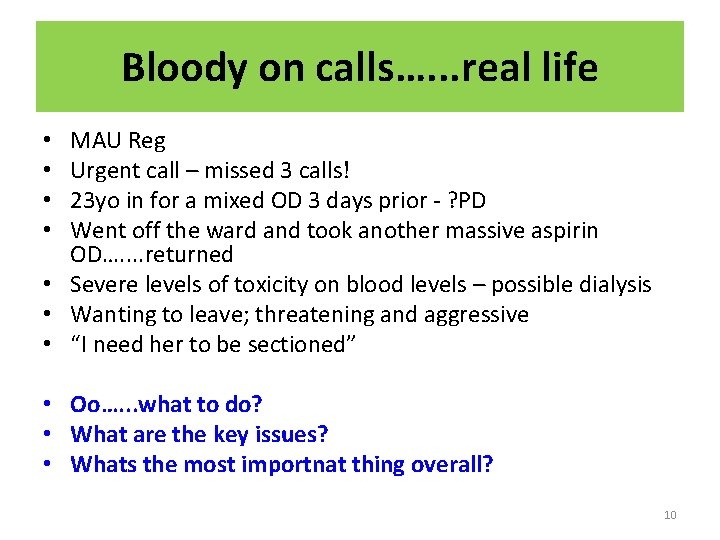
Bloody on calls…. . . real life MAU Reg Urgent call – missed 3 calls! 23 yo in for a mixed OD 3 days prior - ? PD Went off the ward and took another massive aspirin OD…. . returned • Severe levels of toxicity on blood levels – possible dialysis • Wanting to leave; threatening and aggressive • “I need her to be sectioned” • • • Oo…. . . what to do? • What are the key issues? • Whats the most importnat thing overall? 10
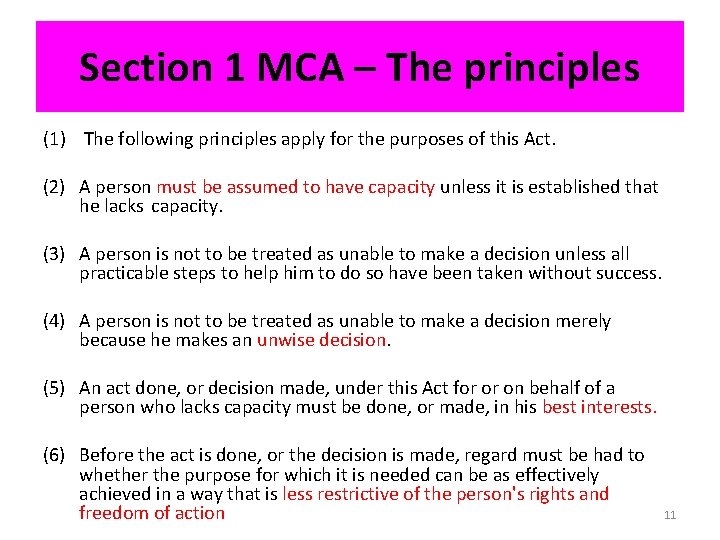
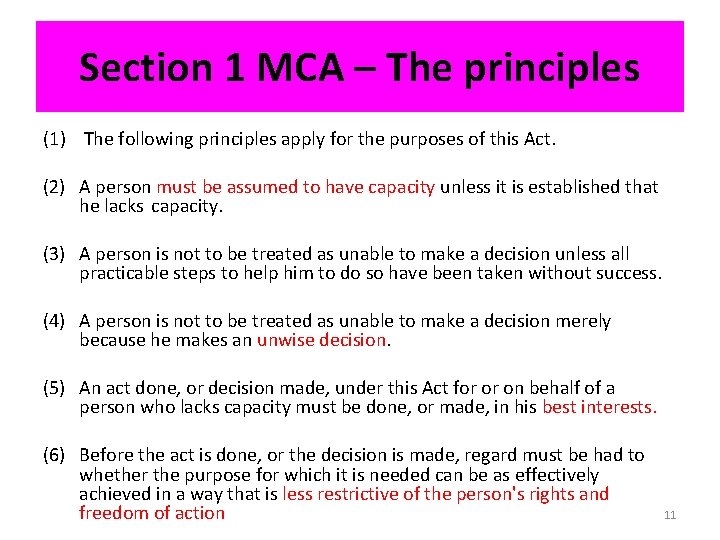
Section 1 MCA – The principles (1) The following principles apply for the purposes of this Act. (2) A person must be assumed to have capacity unless it is established that he lacks capacity. (3) A person is not to be treated as unable to make a decision unless all practicable steps to help him to do so have been taken without success. (4) A person is not to be treated as unable to make a decision merely because he makes an unwise decision. (5) An act done, or decision made, under this Act for or on behalf of a person who lacks capacity must be done, or made, in his best interests. (6) Before the act is done, or the decision is made, regard must be had to whether the purpose for which it is needed can be as effectively achieved in a way that is less restrictive of the person's rights and freedom of action 11
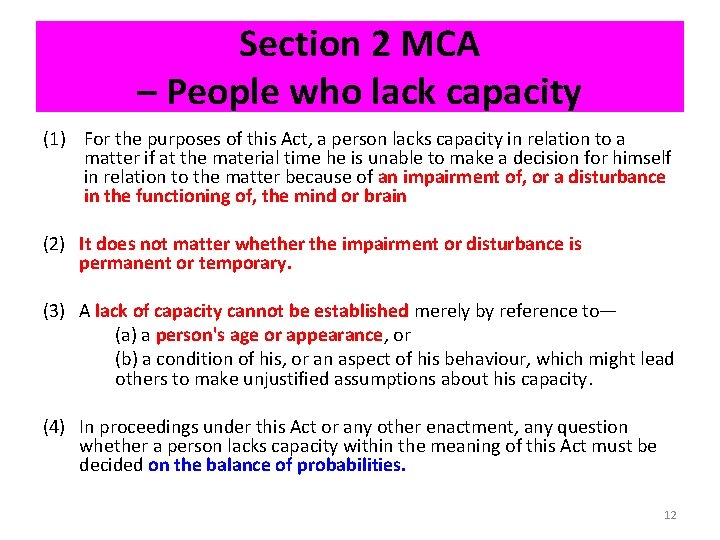
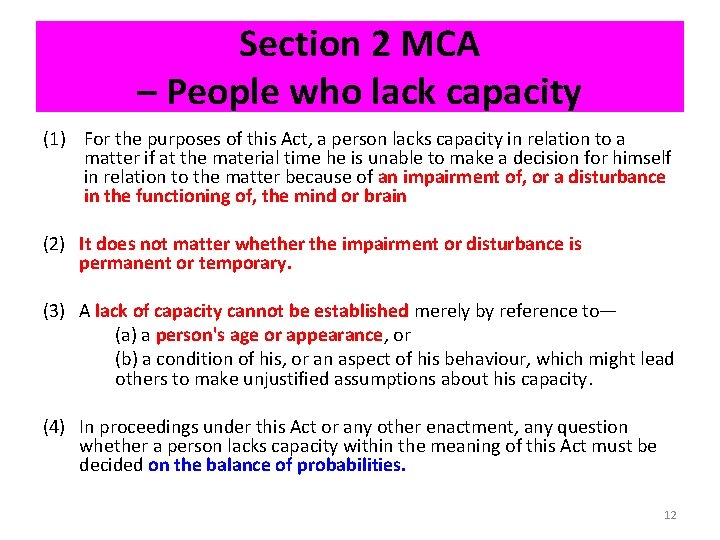
Section 2 MCA – People who lack capacity (1) For the purposes of this Act, a person lacks capacity in relation to a matter if at the material time he is unable to make a decision for himself in relation to the matter because of an impairment of, or a disturbance in the functioning of, the mind or brain (2) It does not matter whether the impairment or disturbance is permanent or temporary. (3) A lack of capacity cannot be established merely by reference to— (a) a person's age or appearance, or (b) a condition of his, or an aspect of his behaviour, which might lead others to make unjustified assumptions about his capacity. (4) In proceedings under this Act or any other enactment, any question whether a person lacks capacity within the meaning of this Act must be decided on the balance of probabilities. 12
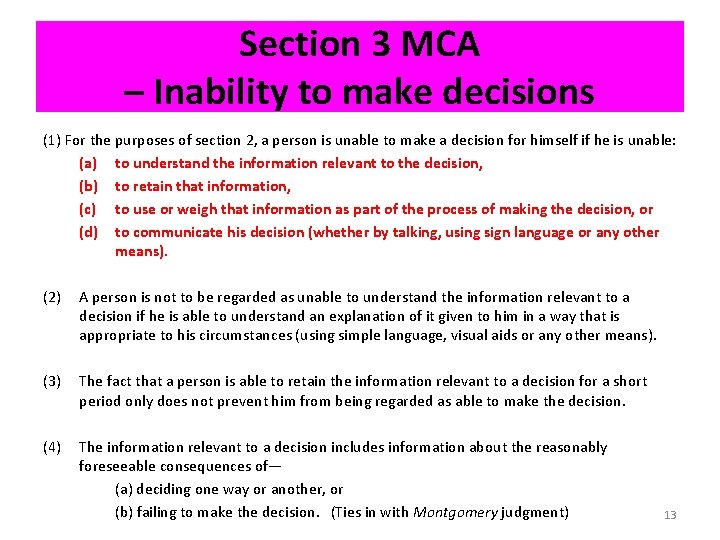
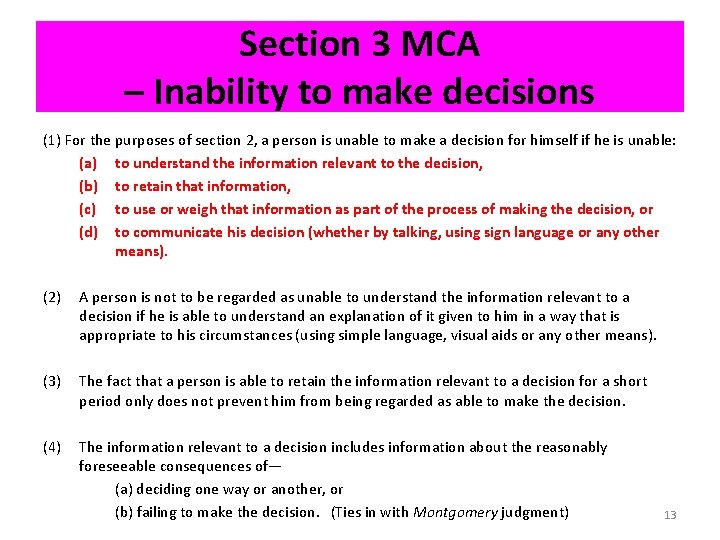
Section 3 MCA – Inability to make decisions (1) For the purposes of section 2, a person is unable to make a decision for himself if he is unable: (a) to understand the information relevant to the decision, (b) to retain that information, (c) to use or weigh that information as part of the process of making the decision, or (d) to communicate his decision (whether by talking, using sign language or any other means). (2) A person is not to be regarded as unable to understand the information relevant to a decision if he is able to understand an explanation of it given to him in a way that is appropriate to his circumstances (using simple language, visual aids or any other means). (3) The fact that a person is able to retain the information relevant to a decision for a short period only does not prevent him from being regarded as able to make the decision. (4) The information relevant to a decision includes information about the reasonably foreseeable consequences of— (a) deciding one way or another, or (b) failing to make the decision. (Ties in with Montgomery judgment) 13

Section 4 MCA – Best interests 1) In determining for the purposes of this Act what is in a person's best interests, the person making the determination must not make it merely on the basis of: (a) the person's age or appearance, or (b) a condition of his, or an aspect of his behaviour, which might lead others to make unjustified assumptions about what might be in his best interests. (2) The person making the determination must consider all the relevant circumstances and, in particular, take the following steps. (3) He must consider: (a) whether it is likely that the person will at some time have capacity in relation to the matter in question, and (b) if it appears likely that he will, when that is likely to be. 14
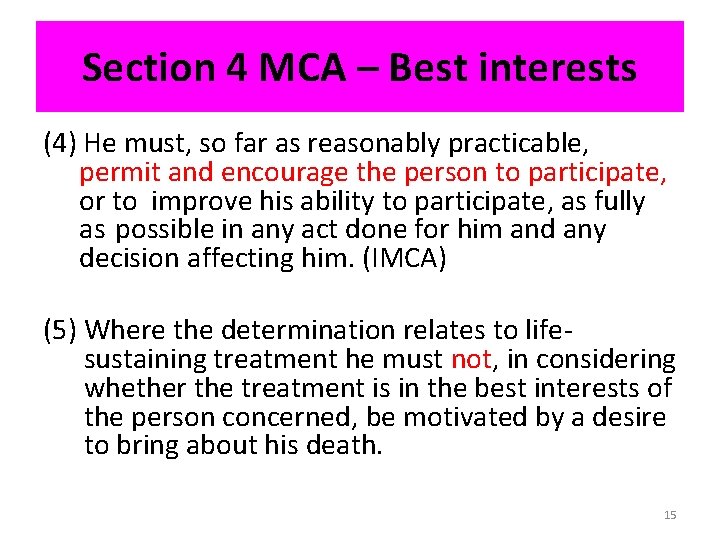
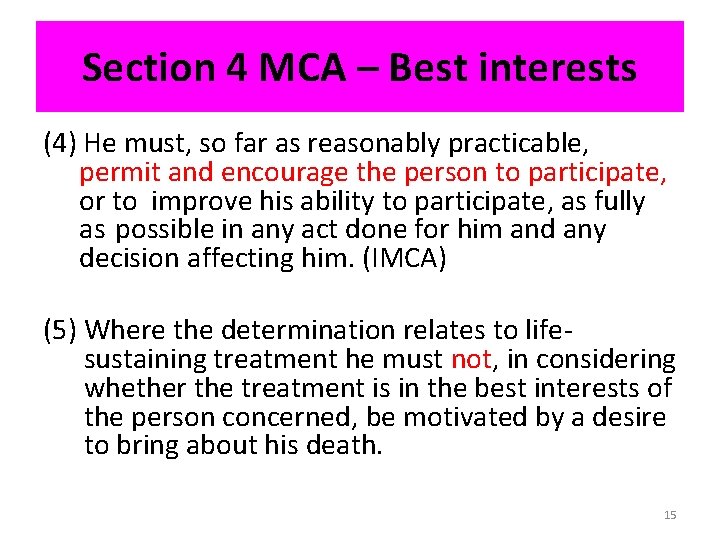
Section 4 MCA – Best interests (4) He must, so far as reasonably practicable, permit and encourage the person to participate, or to improve his ability to participate, as fully as possible in any act done for him and any decision affecting him. (IMCA) (5) Where the determination relates to lifesustaining treatment he must not, in considering whether the treatment is in the best interests of the person concerned, be motivated by a desire to bring about his death. 15
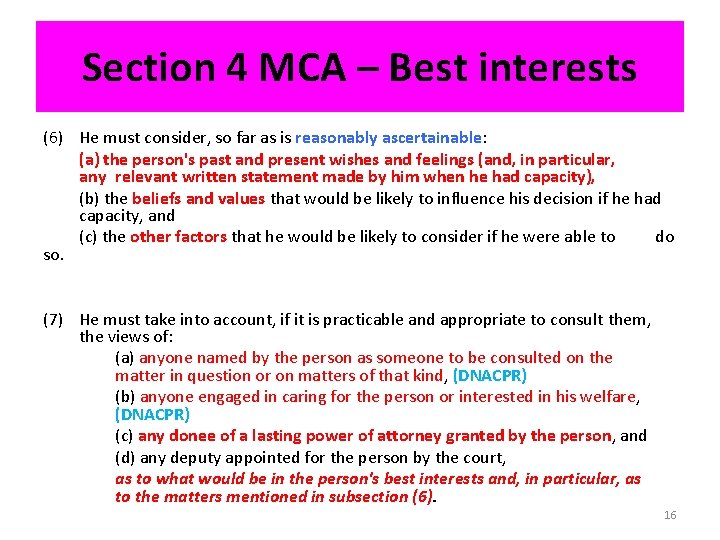
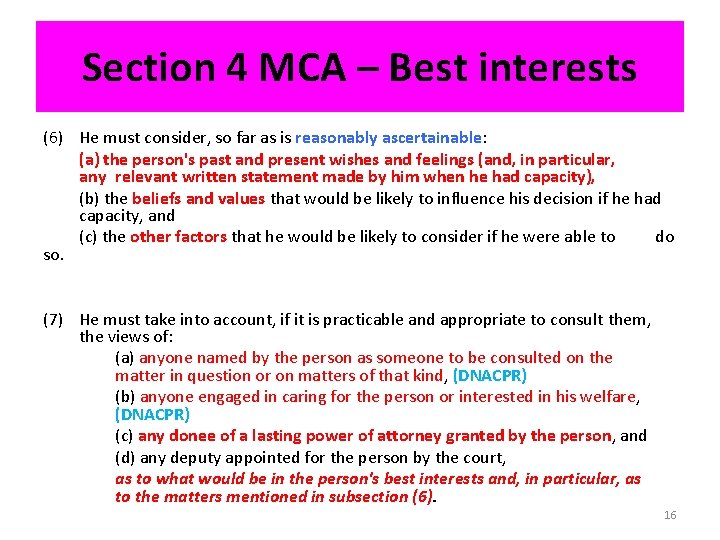
Section 4 MCA – Best interests (6) He must consider, so far as is reasonably ascertainable: (a) the person's past and present wishes and feelings (and, in particular, any relevant written statement made by him when he had capacity), (b) the beliefs and values that would be likely to influence his decision if he had capacity, and (c) the other factors that he would be likely to consider if he were able to do so. (7) He must take into account, if it is practicable and appropriate to consult them, the views of: (a) anyone named by the person as someone to be consulted on the matter in question or on matters of that kind, (DNACPR) (b) anyone engaged in caring for the person or interested in his welfare, (DNACPR) (c) any donee of a lasting power of attorney granted by the person, and (d) any deputy appointed for the person by the court, as to what would be in the person's best interests and, in particular, as to the matters mentioned in subsection (6). 16
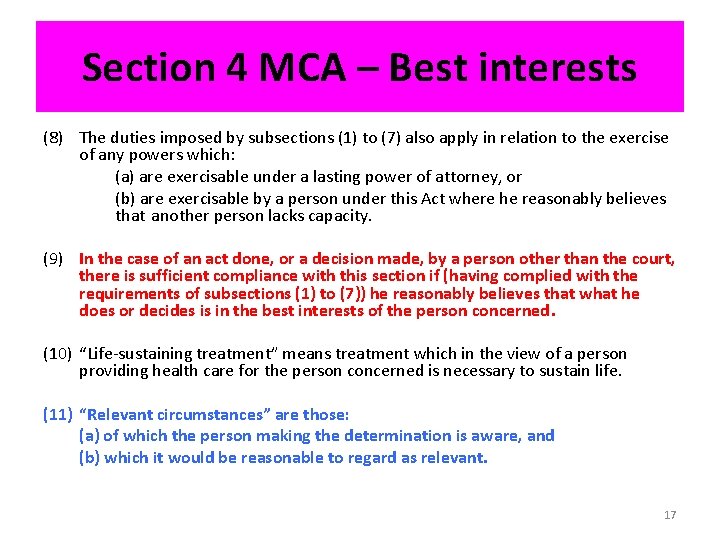
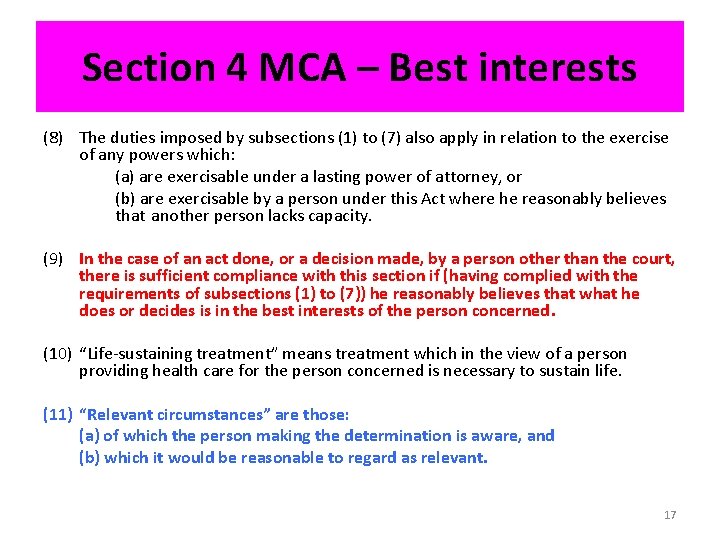
Section 4 MCA – Best interests (8) The duties imposed by subsections (1) to (7) also apply in relation to the exercise of any powers which: (a) are exercisable under a lasting power of attorney, or (b) are exercisable by a person under this Act where he reasonably believes that another person lacks capacity. (9) In the case of an act done, or a decision made, by a person other than the court, there is sufficient compliance with this section if (having complied with the requirements of subsections (1) to (7)) he reasonably believes that what he does or decides is in the best interests of the person concerned. (10) “Life-sustaining treatment” means treatment which in the view of a person providing health care for the person concerned is necessary to sustain life. (11) “Relevant circumstances” are those: (a) of which the person making the determination is aware, and (b) which it would be reasonable to regard as relevant. 17
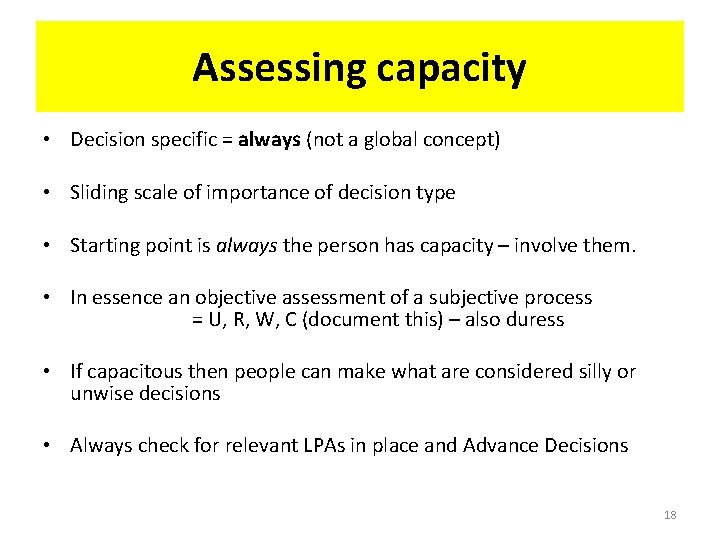
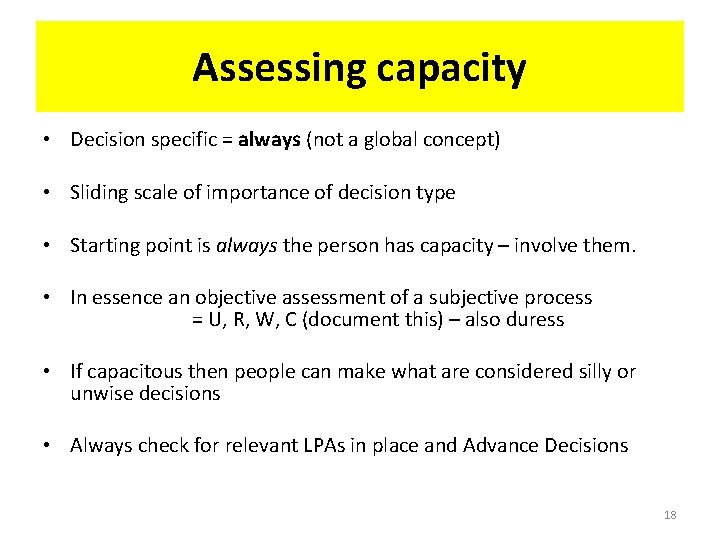
Assessing capacity • Decision specific = always (not a global concept) • Sliding scale of importance of decision type • Starting point is always the person has capacity – involve them. • In essence an objective assessment of a subjective process = U, R, W, C (document this) – also duress • If capacitous then people can make what are considered silly or unwise decisions • Always check for relevant LPAs in place and Advance Decisions 18
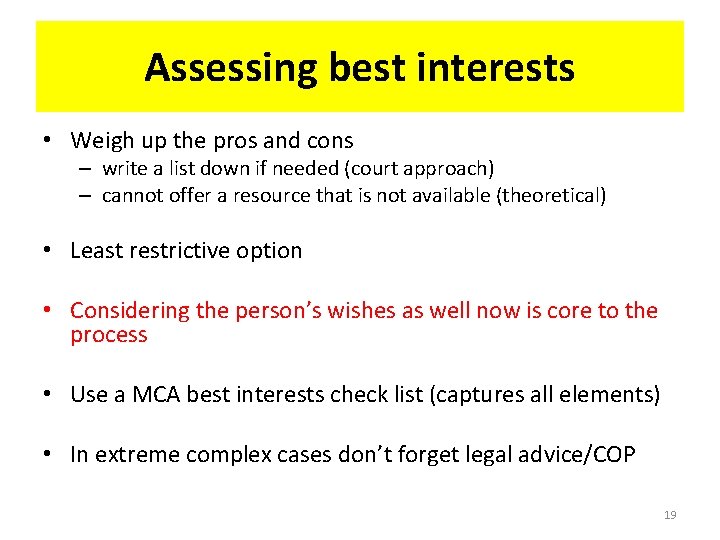
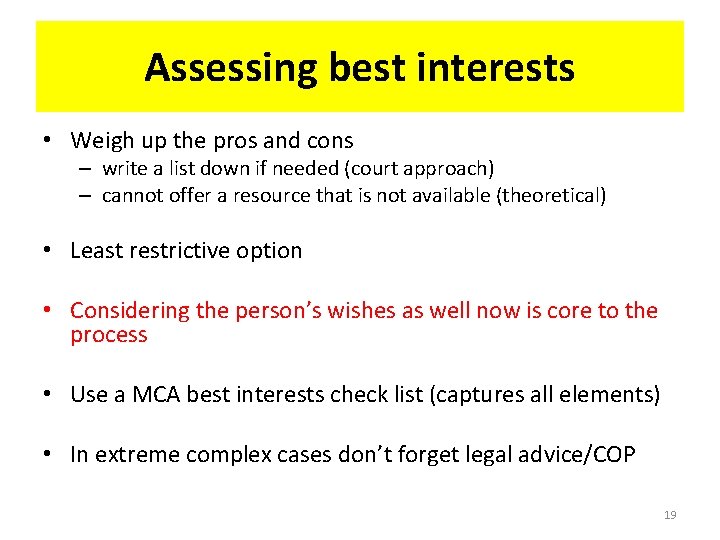
Assessing best interests • Weigh up the pros and cons – write a list down if needed (court approach) – cannot offer a resource that is not available (theoretical) • Least restrictive option • Considering the person’s wishes as well now is core to the process • Use a MCA best interests check list (captures all elements) • In extreme complex cases don’t forget legal advice/COP 19
![Incapacitatedly autonomous Wye Valley NHS Trust v B 2015 EWCOP 60 28 th Incapacitatedly autonomous Wye Valley NHS Trust v B [2015] EWCOP 60 • 28 th](https://slidetodoc.com/presentation_image/275d772ac839eb5af713bdfcd44abb1f/image-20.jpg)
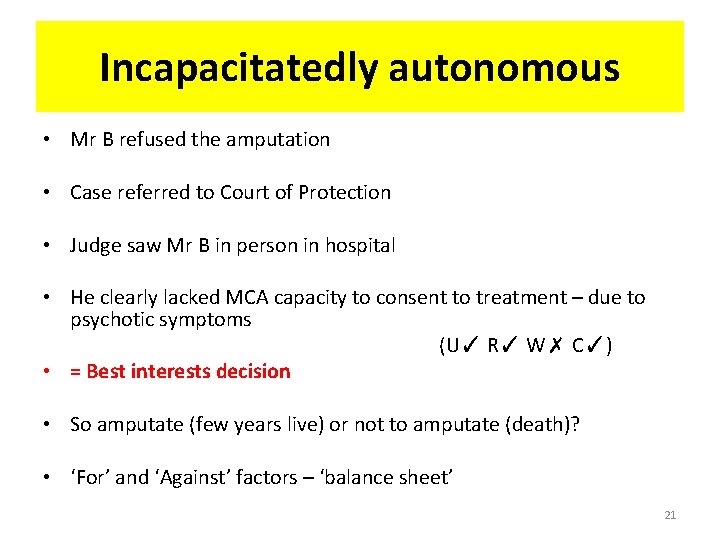
Incapacitatedly autonomous Wye Valley NHS Trust v B [2015] EWCOP 60 • 28 th September 2015 • 73 -year-old man Mr B; no NOK (IMCA); no visitors • Chronic schizophrenia – religiose delusions and auditory hallucinations (command – "If the Lord says it's no, it's no. ”) • Chronic foot ulcer over 18 months • Hospitalised x 3 – rehab units; Sectioned Psychiatric Hospital • Systemically unwell – acute hospital; osteomyelitis • Amputation of foot/BKA advised (if not 1 -2 weeks prognosis) 20
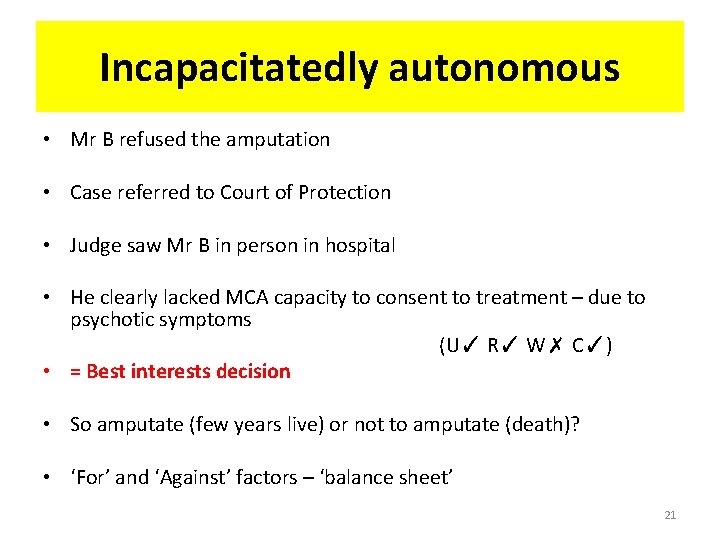
Incapacitatedly autonomous • Mr B refused the amputation • Case referred to Court of Protection • Judge saw Mr B in person in hospital • He clearly lacked MCA capacity to consent to treatment – due to psychotic symptoms (U✓ R✓ W✗ C✓) • = Best interests decision • So amputate (few years live) or not to amputate (death)? • ‘For’ and ‘Against’ factors – ‘balance sheet’ 21
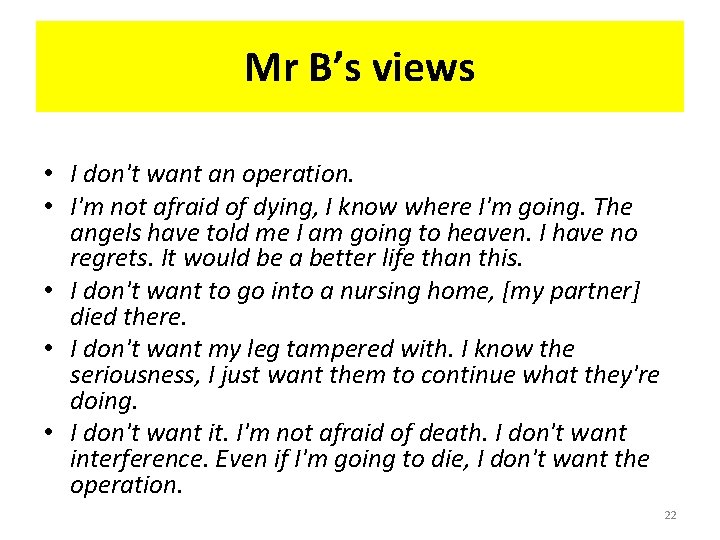
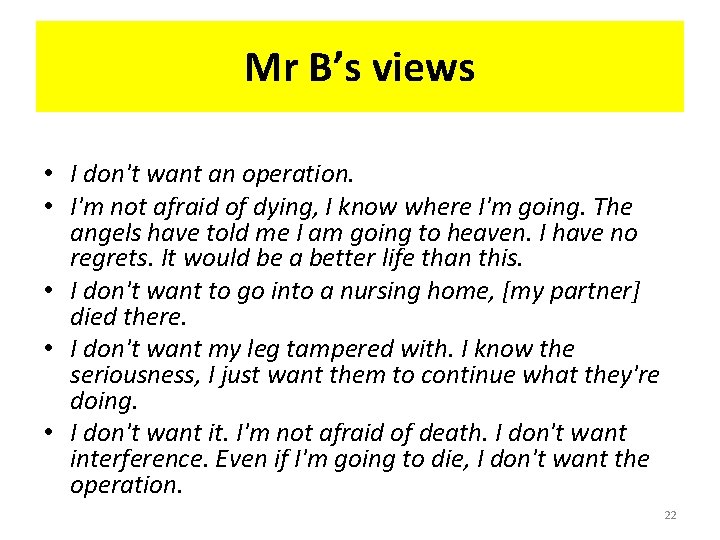
Mr B’s views • I don't want an operation. • I'm not afraid of dying, I know where I'm going. The angels have told me I am going to heaven. I have no regrets. It would be a better life than this. • I don't want to go into a nursing home, [my partner] died there. • I don't want my leg tampered with. I know the seriousness, I just want them to continue what they're doing. • I don't want it. I'm not afraid of death. I don't want interference. Even if I'm going to die, I don't want the operation. 22
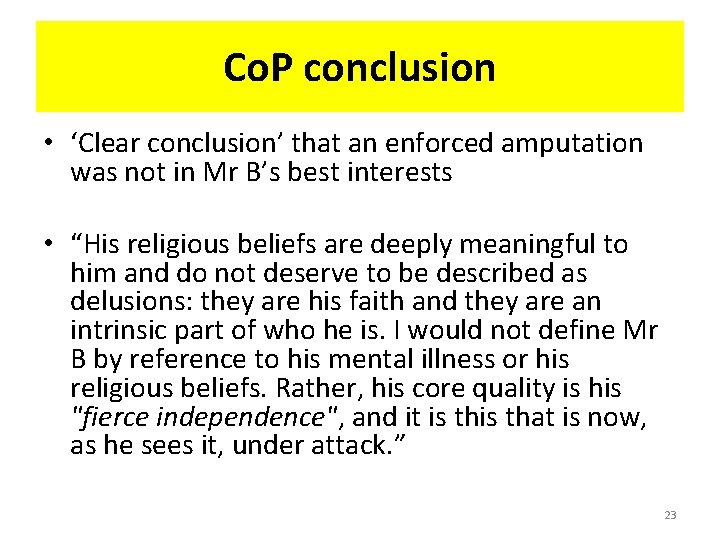
Co. P conclusion • ‘Clear conclusion’ that an enforced amputation was not in Mr B’s best interests • “His religious beliefs are deeply meaningful to him and do not deserve to be described as delusions: they are his faith and they are an intrinsic part of who he is. I would not define Mr B by reference to his mental illness or his religious beliefs. Rather, his core quality is his "fierce independence", and it is that is now, as he sees it, under attack. ” 23
Co. P conclusion • “I am quite sure that it would not be in Mr B's best interests to take away his little remaining independence and dignity in order to replace it with a future for which he understandably has no appetite and which could only be achieved after a traumatic and uncertain struggle that he and no one else would have to endure. There is a difference between fighting on someone's behalf and just fighting them. Enforcing treatment in this case would surely be the latter. ” 24
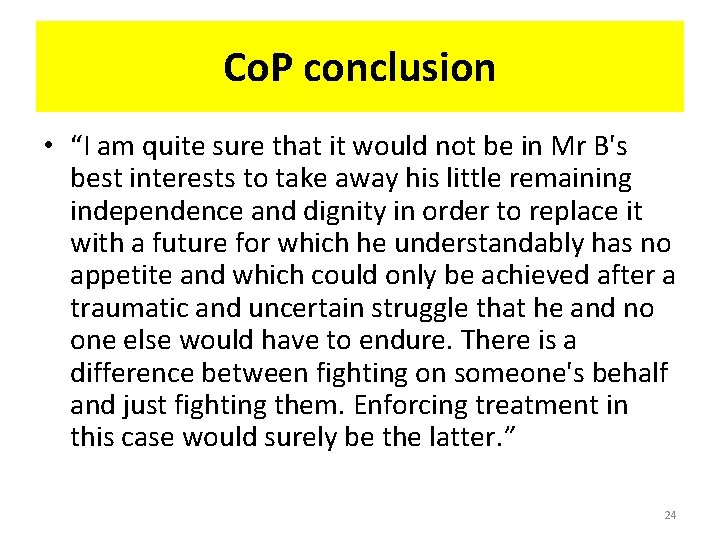
Deprivation of Liberty safeguards Cheshire West 2014 = ‘acid test’ for a Do. L Incapacitous individuals are deprived of their liberty if they are under: 1. Continuous or complete supervision and control, AND, 2. Are not free to leave Over 600+ outstanding DOLs in the County If on DOLs and die inform Coroners Office Informal (voluntary); Do. LS; MHA 25
Do. LS and ICU R (LF) v HM Senior Coroner for Inner South London [2015] EWHC 2990 (Admin) • 29 th October 2015 • Very lengthy judgment (161 paragraphs) • Maria, 45 yo • Severe LD and Down’s Syndrome • Limited mobility and 24 hour care • Died in ITU in December 2013 26
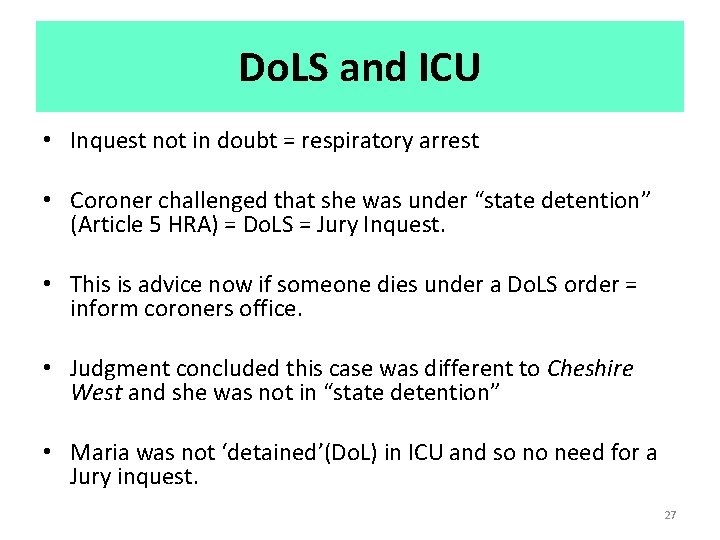
Do. LS and ICU • Inquest not in doubt = respiratory arrest • Coroner challenged that she was under “state detention” (Article 5 HRA) = Do. LS = Jury Inquest. • This is advice now if someone dies under a Do. LS order = inform coroners office. • Judgment concluded this case was different to Cheshire West and she was not in “state detention” • Maria was not ‘detained’(Do. L) in ICU and so no need for a Jury inquest. 27
![Montgomery v Lanarkshire 2015 Diabetic mother shoulder dystocia during birth Mother Montgomery v Lanarkshire [2015] • Diabetic mother – shoulder dystocia during birth • Mother](https://slidetodoc.com/presentation_image/275d772ac839eb5af713bdfcd44abb1f/image-28.jpg)
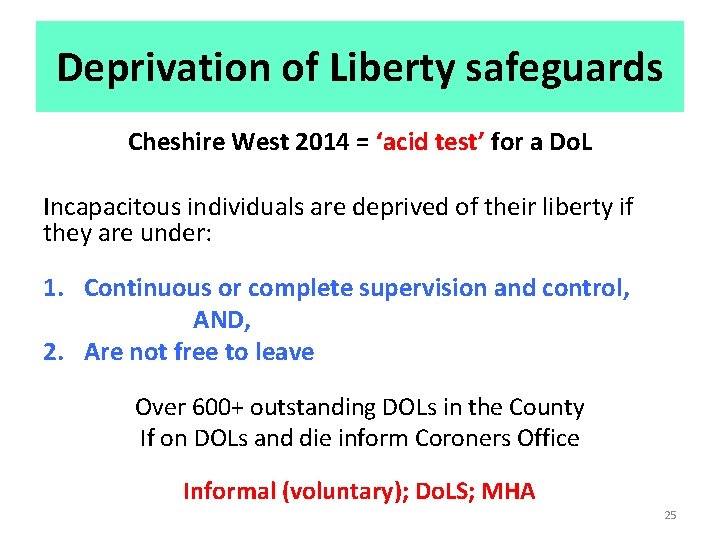
Montgomery v Lanarkshire [2015] • Diabetic mother – shoulder dystocia during birth • Mother not told of the 9 -10% risk by Consultant • Court ruled the mother should have been told of this risk and the option of C section • Bolam Test now no longer applies in issues of consent to treatment • Now a Dr or healthcare professional must take: “…reasonable care to ensure that the patient is aware of any material risks in any recommended treatment, and of any reasonable or variant treatments”. 28
![Montgomery v Lanarkshire 2015 What is a material risk It is a Montgomery v Lanarkshire [2015] • What is a material risk? • It is a](https://slidetodoc.com/presentation_image/275d772ac839eb5af713bdfcd44abb1f/image-29.jpg)
Montgomery v Lanarkshire [2015] • What is a material risk? • It is a risk to which a reasonable person in the patient’s position would be likely to attach significance or a risk that a doctor knows – or should reasonably know – would probably be deemed of significance by the particular patient. • ‘Particular patient’ is important – eye surgery 29
![Montgomery v Lanarkshire 2015 A pro forma scripted approach to consent is a Montgomery v Lanarkshire [2015] • A pro forma ‘scripted’ approach to consent is a](https://slidetodoc.com/presentation_image/275d772ac839eb5af713bdfcd44abb1f/image-30.jpg)
Montgomery v Lanarkshire [2015] • A pro forma ‘scripted’ approach to consent is a common but “ethically and legally dubious practice”. • UK Supreme Court talks of a dialogue between doctor and patient (= pitching the information) • This approach is that advocated by the GMC (2008; 2013). • Need to give information in clear terms and “not bombard” the patient with technical information they cannot reasonably expect to grasp. • GMC – Hot topic: 10 questions about consent 30
![Montgomery v Lanarkshire 2015 Exceptions to disclosure 1 The patient might tell the doctor Montgomery v Lanarkshire [2015] Exceptions to disclosure 1. The patient might tell the doctor](https://slidetodoc.com/presentation_image/275d772ac839eb5af713bdfcd44abb1f/image-31.jpg)
Montgomery v Lanarkshire [2015] Exceptions to disclosure 1. The patient might tell the doctor that he/she would prefer not to know the risks 2. The doctor might reasonably consider that telling the patient something would cause serious harm to the patient’s health (UKSC warns that this “therapeutic exception” should not be abused) 3. No consent is needed in circumstances of necessity e. g. when the patient in need of urgent treatment is unconscious or lacks capacity 31
![Montgomery v Lanarkshire 2015 So for capacitous consenting patients 1 Does the patient Montgomery v Lanarkshire [2015] So for capacitous & consenting patients 1. Does the patient](https://slidetodoc.com/presentation_image/275d772ac839eb5af713bdfcd44abb1f/image-32.jpg)
Montgomery v Lanarkshire [2015] So for capacitous & consenting patients 1. Does the patient know about the material risks of the treatment I am proposing? - What sorts of risks would a reasonable person in the patient’s circumstances want to know? - What sorts of risks would this particular patient want to know? 2. Does the patient know of reasonable alternatives to this treatment? 3. Have I taken reasonable care to make sure the patient actually knows this? 4. Do any of the exceptions to my duty to disclose apply here? 5. Have I properly documented my consent process? (Sokol, BMJ 2015; 350: h 1481) 32
![Do LS and covert administration of medication AG v BMBC Anor 2016 EWCOP Do. LS and covert administration of medication AG v BMBC & Anor [2016] EWCOP](https://slidetodoc.com/presentation_image/275d772ac839eb5af713bdfcd44abb1f/image-33.jpg)
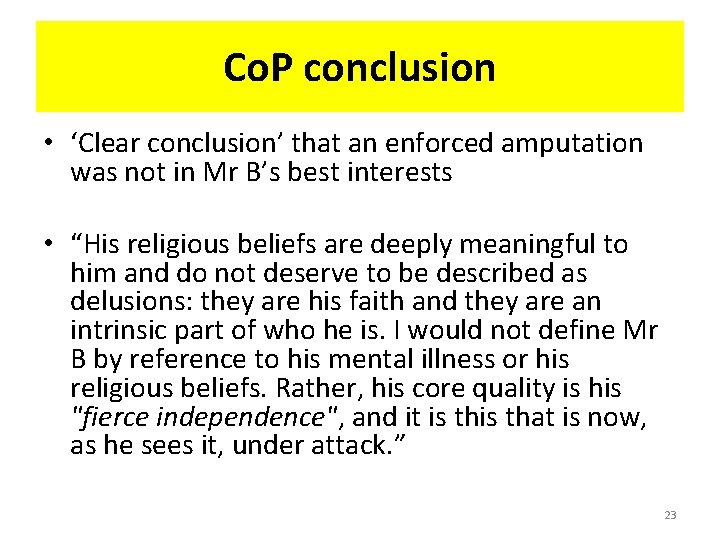
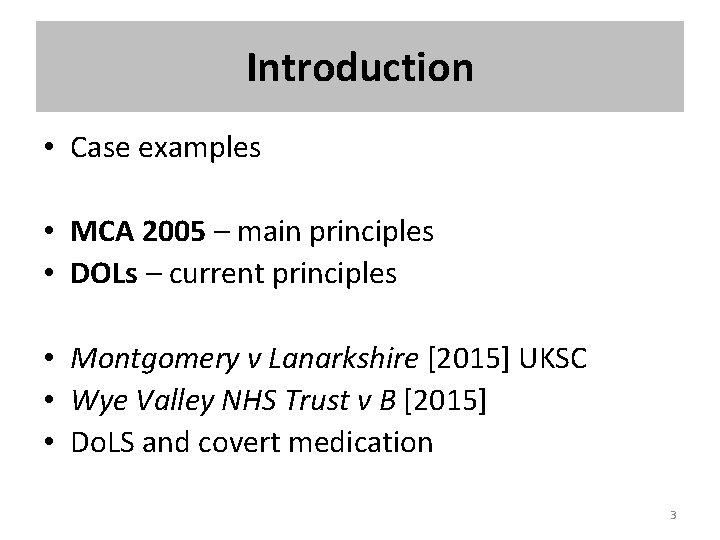
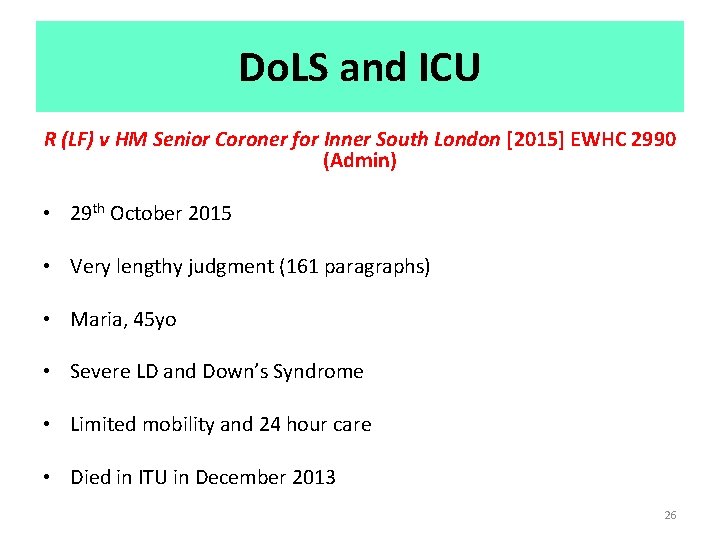
Do. LS and covert administration of medication AG v BMBC & Anor [2016] EWCOP 37 – 6 th July 2016 • s. 21 A application challenging a DOLS authorisation in place in respect of a 92 year old woman, AG (Alzheimer’s dementia; squalor) • Part of AG's care plan at the care home involved the covert administration of promethazine and diazepam. • There were no conditions relating to this medication contained in the care plan. 33
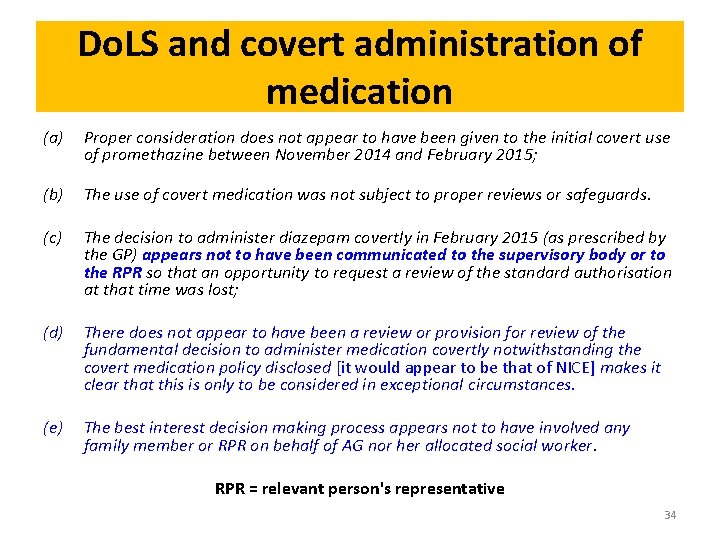
Do. LS and covert administration of medication (a) Proper consideration does not appear to have been given to the initial covert use of promethazine between November 2014 and February 2015; (b) The use of covert medication was not subject to proper reviews or safeguards. (c) The decision to administer diazepam covertly in February 2015 (as prescribed by the GP) appears not to have been communicated to the supervisory body or to the RPR so that an opportunity to request a review of the standard authorisation at that time was lost; (d) There does not appear to have been a review or provision for review of the fundamental decision to administer medication covertly notwithstanding the covert medication policy disclosed [it would appear to be that of NICE] makes it clear that this is only to be considered in exceptional circumstances. (e) The best interest decision making process appears not to have involved any family member or RPR on behalf of AG nor her allocated social worker. RPR = relevant person's representative 34

Do. LS and covert administration of medication – top tips (i) if a person lacks capacity and is unable to understand the risks to their health if they do not take their prescribed medication and the person is refusing to take the medication then it should only be administered covertly in exceptional circumstances; (ii) before the medication is administered covertly there must be a best interest decision which includes the relevant health professionals and the person's family member (RPR) (iii) if it is agreed that the administration of covert medication is in their best interests then this must be recorded and placed in the person's medical records/care home records and there must be an agreed management plan including details of how it is to be reviewed; and (iv) all of the above documentation must be easily accessible on any viewing of the person's records within the care/nursing home. (v) If there is no agreement then there should be an immediate application to Court. 35
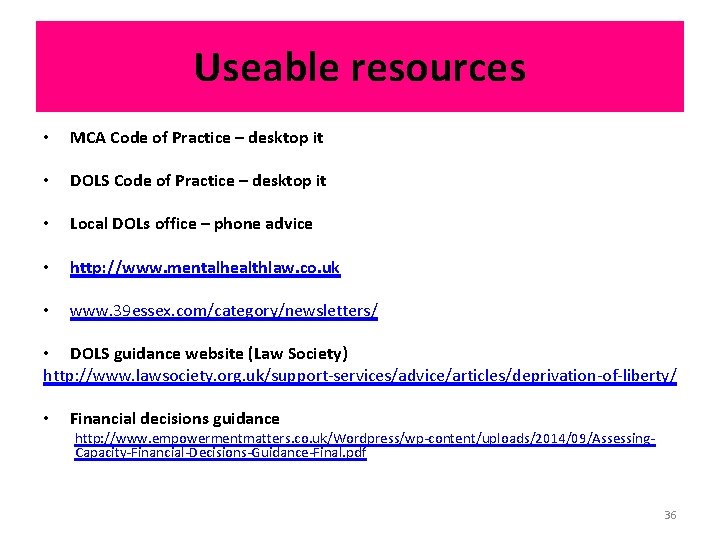
Useable resources • MCA Code of Practice – desktop it • DOLS Code of Practice – desktop it • Local DOLs office – phone advice • http: //www. mentalhealthlaw. co. uk • www. 39 essex. com/category/newsletters/ • DOLS guidance website (Law Society) http: //www. lawsociety. org. uk/support-services/advice/articles/deprivation-of-liberty/ • Financial decisions guidance http: //www. empowermentmatters. co. uk/Wordpress/wp-content/uploads/2014/09/Assessing. Capacity-Financial-Decisions-Guidance-Final. pdf 36
 Mca and dols
Mca and dols Dr martin mca
Dr martin mca 6 assessments for dols
6 assessments for dols Worcestershire dols
Worcestershire dols 5 principles of the mental capacity act
5 principles of the mental capacity act Caen digitizer
Caen digitizer Emav-mca
Emav-mca Hyperdense mca
Hyperdense mca Mca diagram
Mca diagram Statutory principles of the mca
Statutory principles of the mca Mca master 500 workboat
Mca master 500 workboat Aka.ms/mca マイクロソフト
Aka.ms/mca マイクロソフト Mca esm
Mca esm Mca software engineering
Mca software engineering Mca court
Mca court 2005
2005 Mca 172-3
Mca 172-3 Middle cerebral artery branches
Middle cerebral artery branches Stamca
Stamca Florida consent decree summary
Florida consent decree summary Epi pen
Epi pen Consent laws
Consent laws Age of consent kentucky
Age of consent kentucky Contract without free consent
Contract without free consent Broad informed consent
Broad informed consent Which act taxed colonists without their consent? *
Which act taxed colonists without their consent? * Sebutkan dasar hukum informed consent
Sebutkan dasar hukum informed consent Ethical principles governing informed consent process
Ethical principles governing informed consent process Essential elements of informed consent
Essential elements of informed consent What is positive intervention consent
What is positive intervention consent Consent
Consent Emancipated minors definition
Emancipated minors definition The consent elaine kaye
The consent elaine kaye Age of consent la
Age of consent la Age of consent per state
Age of consent per state Wcu irb
Wcu irb Informed consent brochure
Informed consent brochure