Increasing Access to Mental Health Addictions MHA Services


- Slides: 23
Increasing Access to Mental Health & Addictions (MH&A) Services in Rural Areas BC Patient Safety & Quality Council Quality Forum, Vancouver, Feb 2015 Presenters: Kathleen Collins, Selina Tsang
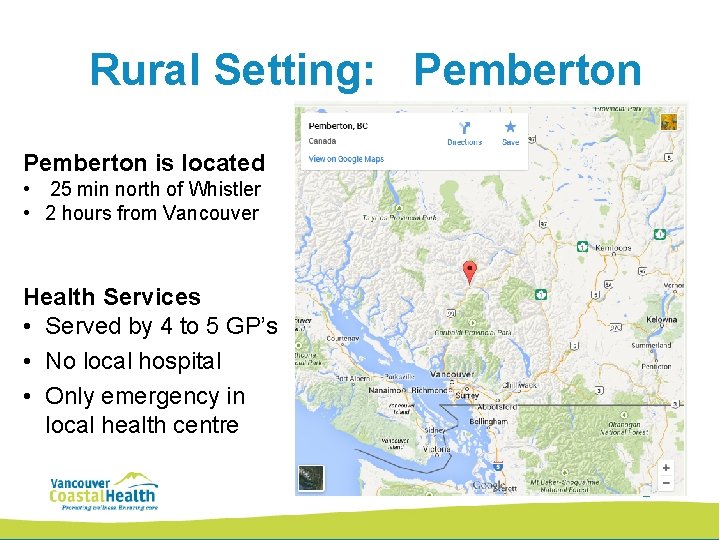
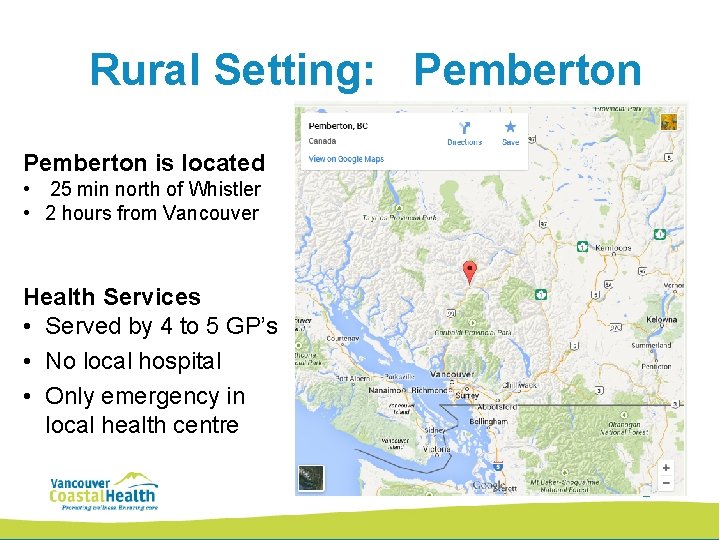
Rural Setting: Pemberton is located • 25 min north of Whistler • 2 hours from Vancouver Health Services • Served by 4 to 5 GP’s • No local hospital • Only emergency in local health centre 2
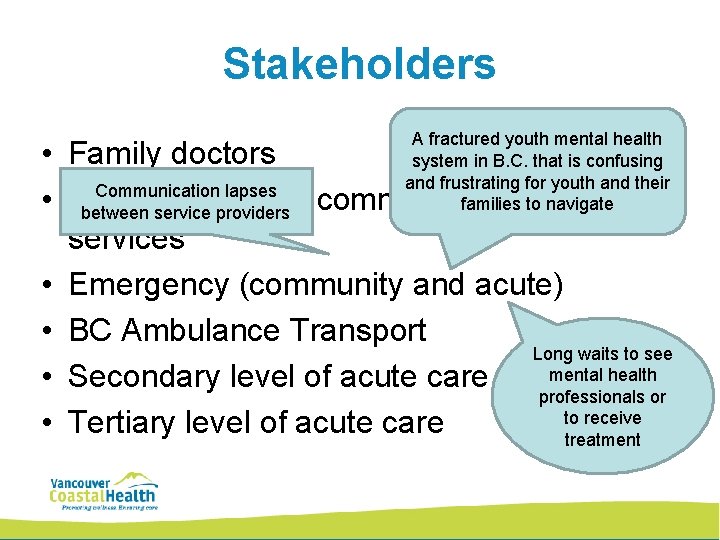
Stakeholders A fractured youth mental health system in B. C. that is confusing and frustrating for youth and their families to navigate • Family doctors Communication lapses • MCFD / CYMH – community mental health between service providers services • Emergency (community and acute) • BC Ambulance Transport Long waits to see mental health • Secondary level of acute care professionals or to receive • Tertiary level of acute care treatment 3
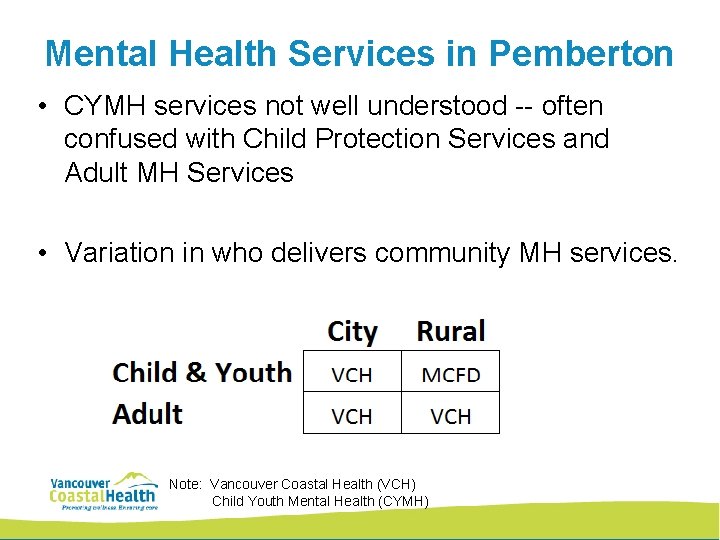
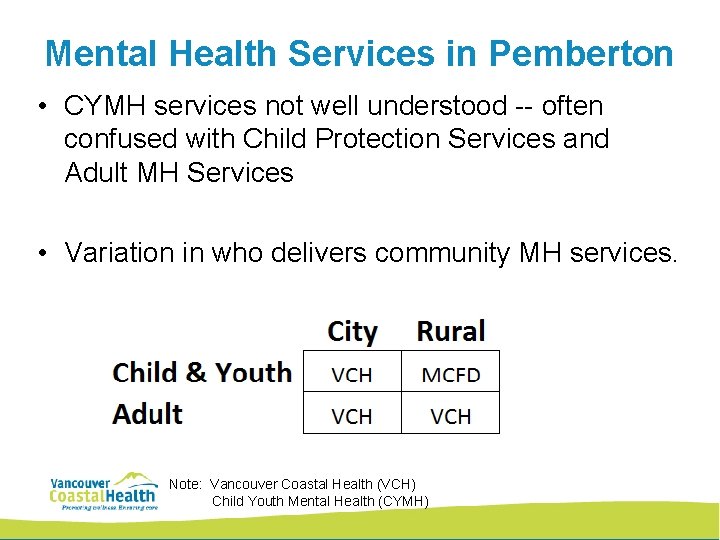
Mental Health Services in Pemberton • CYMH services not well understood -- often confused with Child Protection Services and Adult MH Services • Variation in who delivers community MH services. Note: Vancouver Coastal Health (VCH) Child Youth Mental Health (CYMH) 4
Barriers to Access • CYMH services available only during weekday office hours • Inadequate child psychiatrist coverage – only available in Squamish – up to 2 months wait 5
Lack of coordination between systems Unsupported vulnerable youth • GP not following protocol to certify kids under the MH Act • Nearest hospital (LGH) not staffed with child psychiatrist • GP confused why they can’t refer directly to BCCH (CAPE unit) Child & Adolescent Psychiatric Emergency 6
Project Goals Establish standardized process for Pemberton children, youth and families to access psychiatric assessment • Emergent need • Urgent need 7
Lean Approach • Assembled design team GP, psychiatrists, nurses, leadership from Regional Mental Health, Lion’s Gate Hospital, CYMH • Established clarity and shared understanding • Clarified roles and responsibilities 8
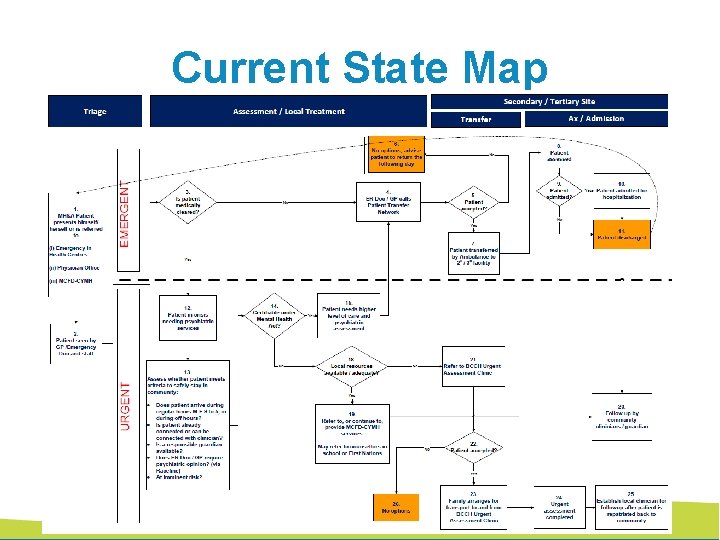
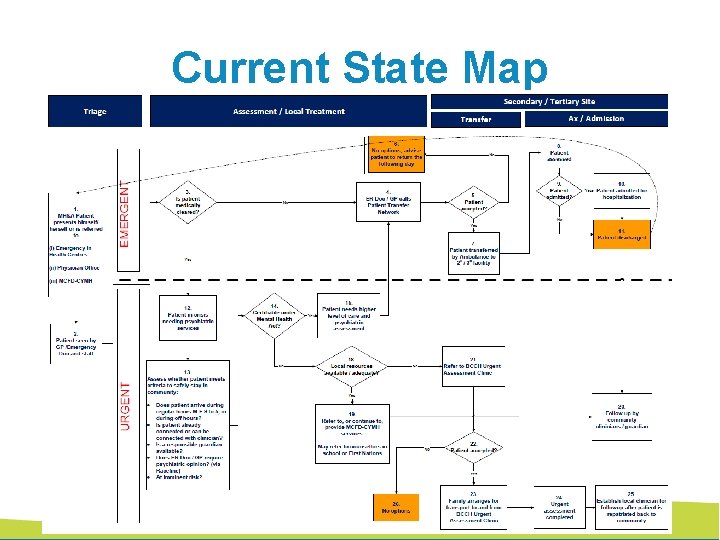
Current State Map 9
An emergent patient may be… Refused transport to secondary hospital if ER Doc refuses to accept patient Typically only accepted for medical issues 10
Even if an emergent patient is brought to hospital, he/she may be de-certified and not admitted. Now patient needs to find transport home 11
An urgent patient • Ideally accesses local help • But when local resources are unavailable / inadequate • Cannot escalate to Emergency (do not fit Emergent criteria) Take their chances to get seen by BCCH Urgent Assessment Clinic 12
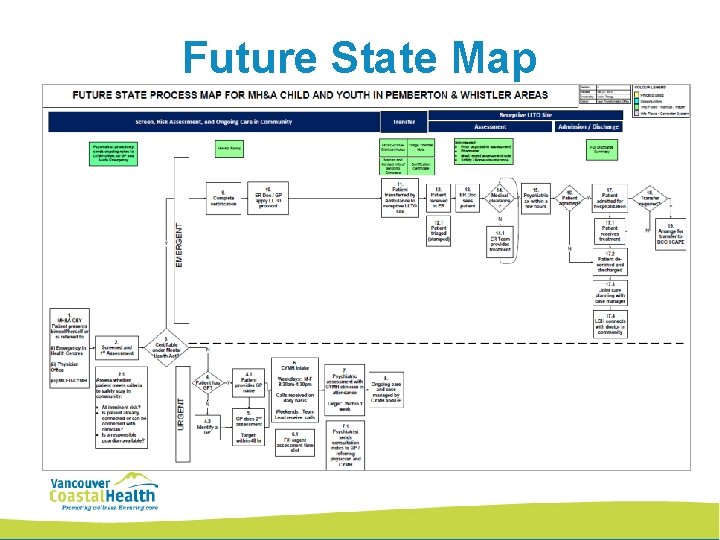
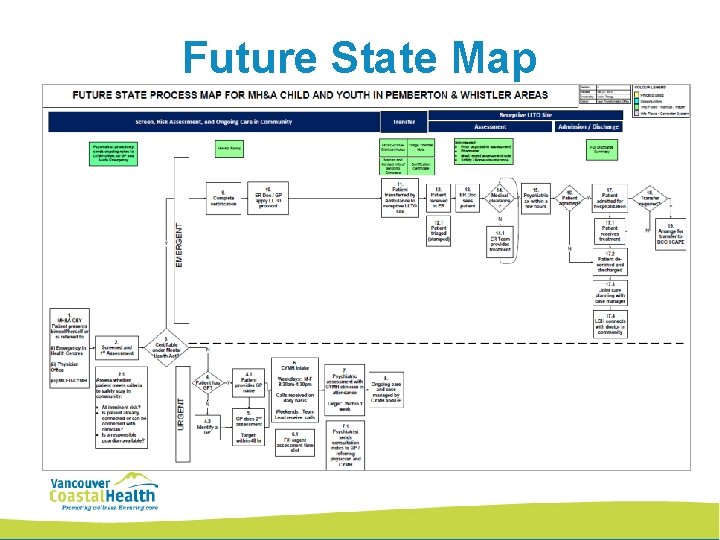
Future State Map 13
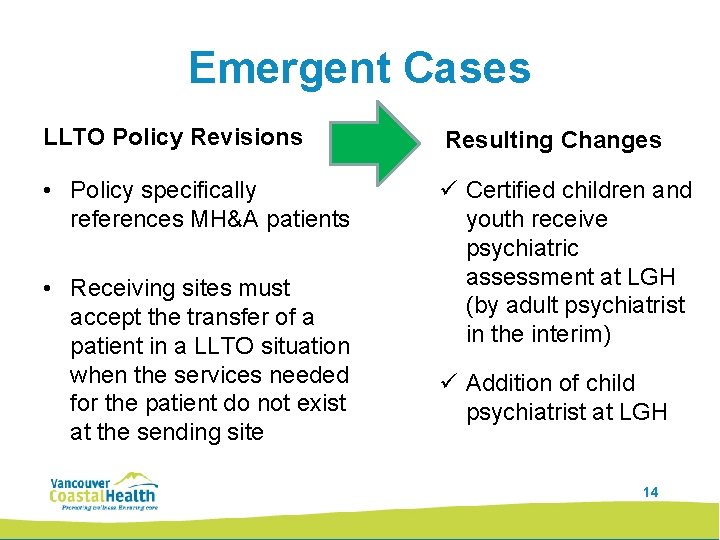
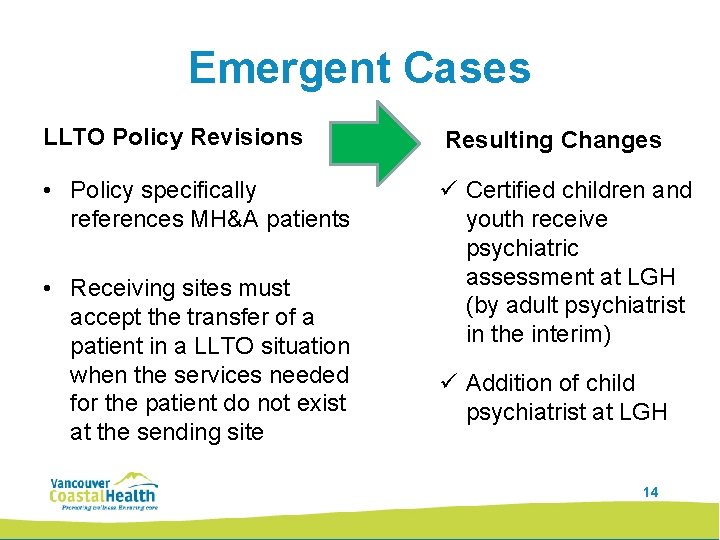
Emergent Cases LLTO Policy Revisions Resulting Changes • Policy specifically references MH&A patients ü Certified children and youth receive psychiatric assessment at LGH (by adult psychiatrist in the interim) • Receiving sites must accept the transfer of a patient in a LLTO situation when the services needed for the patient do not exist at the sending site ü Addition of child psychiatrist at LGH 14
What does it take to … • Create a New Urgent Assessment Clinic? • In a rural setting (aka lack of resources)? 15
Unleash the Power & Passion of a Committed Team 16

Private office space in Whistler (child psych) CYMH office space (child psych) Same space used by adult MH - VCH Combination of adult & child psychiatrists PLACE TIME CONSULT NOTES COST VCH covers cost of psychiatrist time for noshows CYMH + VCH staff PEOPLE CYMH covers transcription Psychiatrist bills MSP for seeing patient costs Charts held by CYMH Clinic available every 1– 2 weeks Hold time or book lunch time slots 17
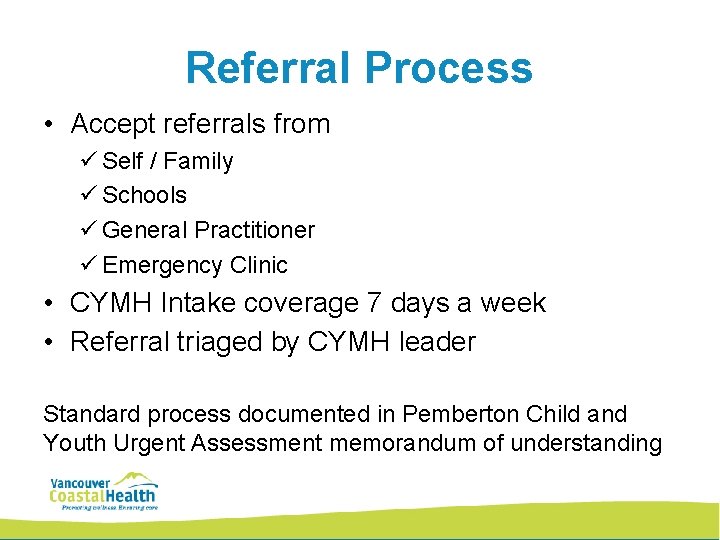
Referral Process • Accept referrals from ü Self / Family ü Schools ü General Practitioner ü Emergency Clinic • CYMH Intake coverage 7 days a week • Referral triaged by CYMH leader Standard process documented in Pemberton Child and Youth Urgent Assessment memorandum of understanding 18
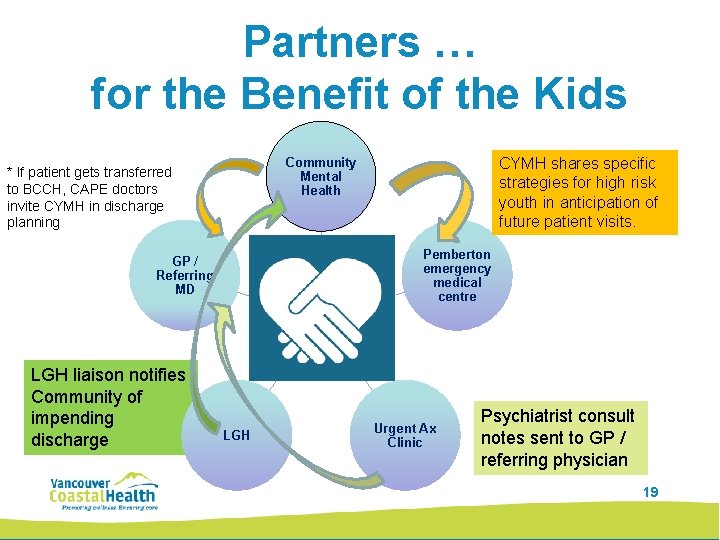
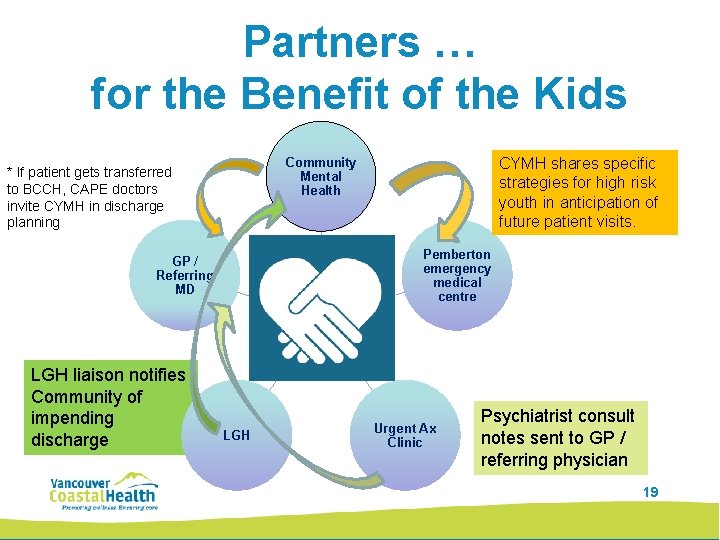
Partners … for the Benefit of the Kids Pemberton emergency medical centre GP / Referring MD LGH liaison notifies Community of impending discharge CYMH shares specific strategies for high risk youth in anticipation of future patient visits. Community Mental Health * If patient gets transferred to BCCH, CAPE doctors invite CYMH in discharge planning LGH Urgent Ax Clinic Psychiatrist consult notes sent to GP / referring physician 19
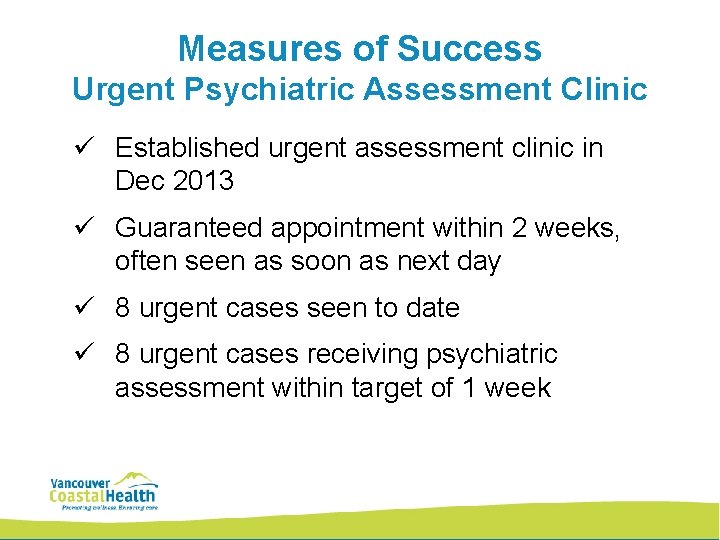
Measures of Success Urgent Psychiatric Assessment Clinic ü Established urgent assessment clinic in Dec 2013 ü Guaranteed appointment within 2 weeks, often seen as soon as next day ü 8 urgent cases seen to date ü 8 urgent cases receiving psychiatric assessment within target of 1 week 20
Voice of Providers Knowing there are local psychiatric services we can access makes it much easier to make decisions about urgent patients. We know we can call CYMH when we need help with a patient We now have much more confidence that patients will receive the urgent care they need in their own community within a quick time frame. 21
Voice of Patient They were going to send me to the city. . . to Lion's Gate. . . They phoned someone from the Ministry and found out I could see a psychiatrist in Pemberton. Then someone came to the clinic to help my parents understand how to help me. My parents let me come home with them. . . I am doing much better now. I am glad I didn't have to go to the city. " 22

Design Team • Project Sponsors: – Yasmin Jetha, Regional Director, MH&A Program – Dr. Steve Mathias, Regional Youth Medical Lead – Olga O’Toole, Regional Manager, CYMH Vancouver Coastal Region – Rena van der Wal, Executive Director, Lean Transformation Services • Process Champion: Elizabeth Stanger, Director MH&A Coastal • Project Owner: Kathleen Collins, CYMH Team Leader • Physicians: Dr. Lance Patrick, Dr. Apu Chakraborty, Dr. Rebecca Lindley, Dr. Helen Rosenauer, Dr. Bobbie Rathbun • Health Centre: • Lean Advisor: Tracey Kavanagh, Janet Hamer Selina Tsang 23
 Foundations of addictions counseling 3rd edition
Foundations of addictions counseling 3rd edition Supracultural model of addiction
Supracultural model of addiction Foundations of addictions counseling
Foundations of addictions counseling Substance use addictions and related behaviours
Substance use addictions and related behaviours Mental health and mental illness chapter 20
Mental health and mental illness chapter 20 Mental health jeopardy questions
Mental health jeopardy questions Bexar county mental health services
Bexar county mental health services Discharge letter from mental health services
Discharge letter from mental health services West cork mental health services bantry
West cork mental health services bantry Cal mhsa
Cal mhsa Renapan
Renapan Health informatics gmu
Health informatics gmu Db ha
Db ha Mha outlook
Mha outlook Mha equipment
Mha equipment Mha carrie
Mha carrie Tonya mha
Tonya mha Sue mha
Sue mha Mha discussion
Mha discussion Mha kaç cilt
Mha kaç cilt Terminal access controller access control system plus
Terminal access controller access control system plus Terminal access controller access-control system
Terminal access controller access-control system Astro access services
Astro access services Cleaning service access rope
Cleaning service access rope