Cancer prevention and early detection C Sauvaget MD





- Slides: 25

Cancer prevention and early detection C. Sauvaget MD Screening Group (SCR)
Prevention aims to reduce mortality from cancer 2
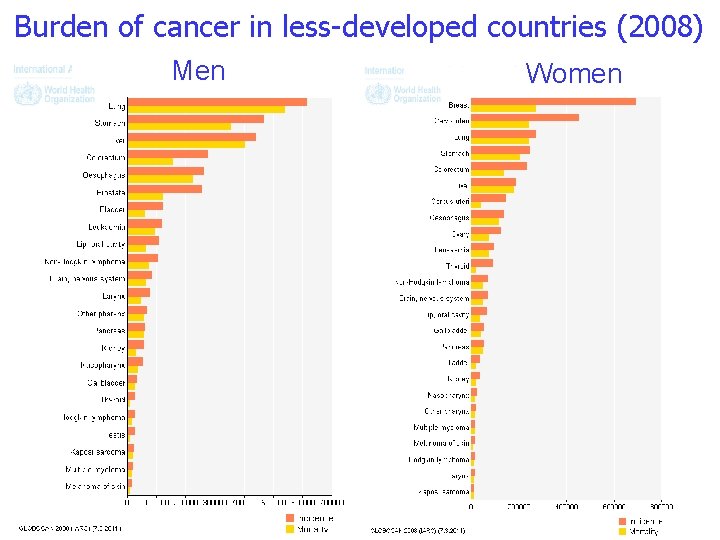
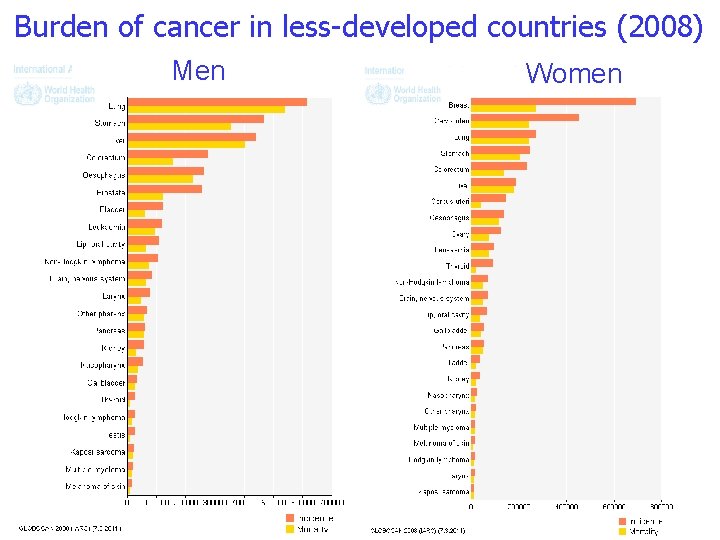
Burden of cancer in less-developed countries (2008) Men 3 Women
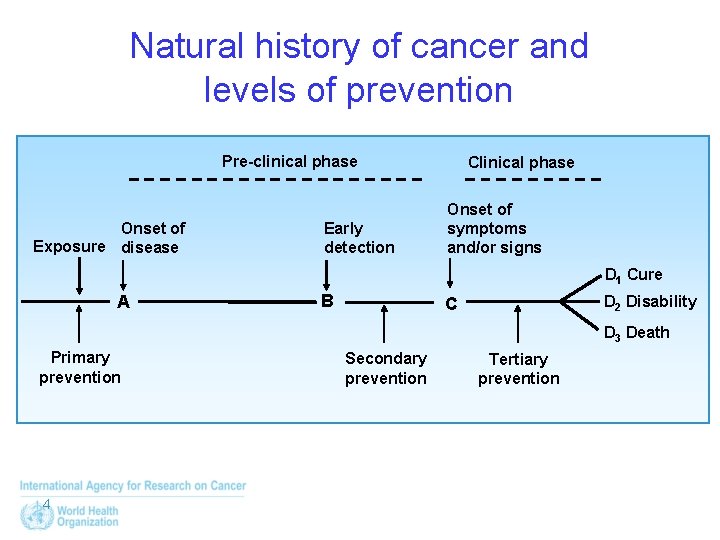
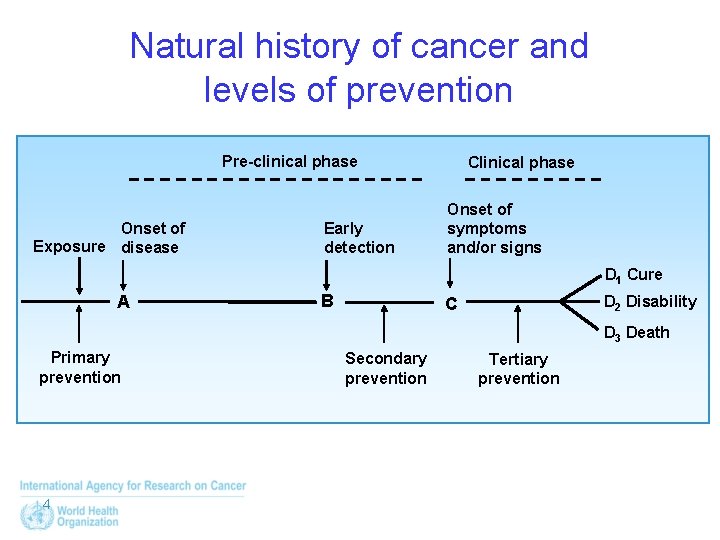
Natural history of cancer and levels of prevention Pre-clinical phase Onset of Exposure disease Early detection Clinical phase Onset of symptoms and/or signs D 1 Cure A B D 2 Disability C D 3 Death Primary prevention 4 Secondary prevention Tertiary prevention
Early detection approaches 1. Screening: Systematic, routine application of a suitable early detection test at specified intervals in a systematically invited asymptomatic population. 2. Early clinical diagnosis: Searching for precancerous or early invasive cancer in symptomatic or asymptomatic individuals in opportunistic settings. Improved awareness and access to health services promote early clinical diagnosis. 5
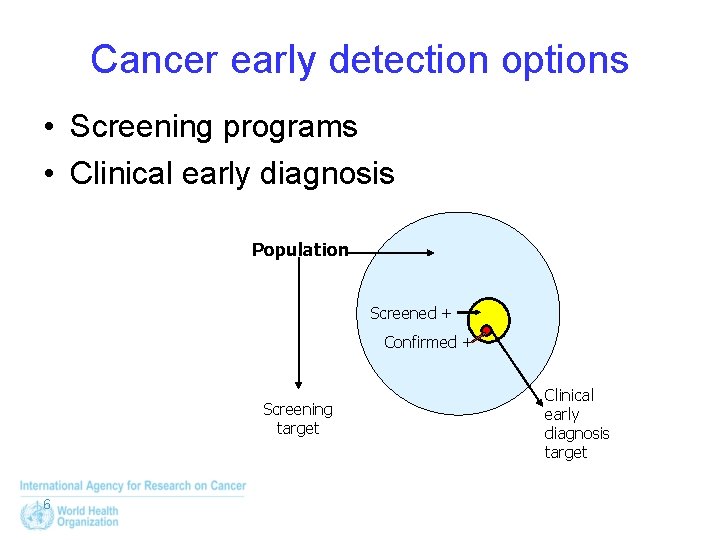
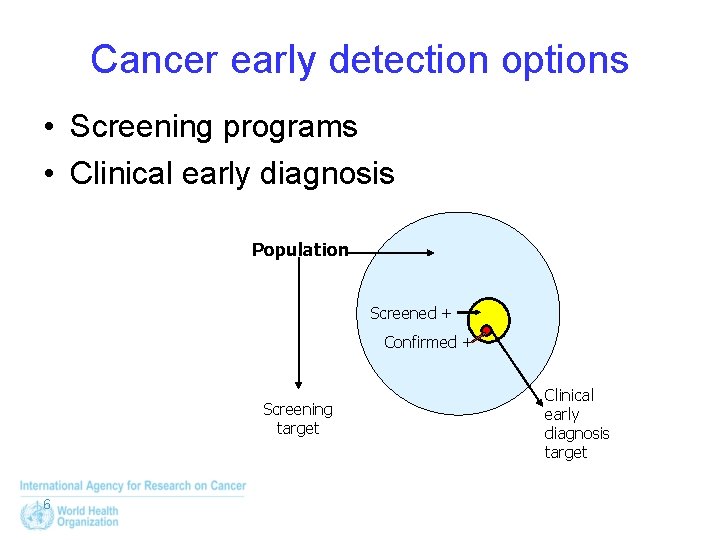
Cancer early detection options • Screening programs • Clinical early diagnosis Population Screened + Confirmed + Screening target 6 Clinical early diagnosis target
Early detection is associated with: • • Benefits/harms Costs to Individual and the Health Services It is important to establish that benefits of early detection, particularly screening, outweigh harms and it is costeffective in reducing incidence/mortality. 7
Screening Requirements 1. Suitable disease 2. Suitable test 3. Suitable screening settings 8
Screening Requirements-1 1. Suitable disease a) Important problem b) Can be detected in preclinical stage c) Effective treatment available d) End result improved by early diagnosis 9
Screening Requirements-2 2. A suitable screening test 2. 1 Adequate validity Sensitivity Specificity 2. 2 Acceptability and cost 10
2. 2 Acceptability and cost • In addition to adequate validity, a screening test should be: ü Low cost ü Convenient ü Simple ü As painless as possible ü Does not cause complications 11
Screening Requirements-3 3. Suitable programme settings a) Adequate infrastructure for diagnosis and treatment in health services b) Adequate trained manpower c) Adequate financial resources 12
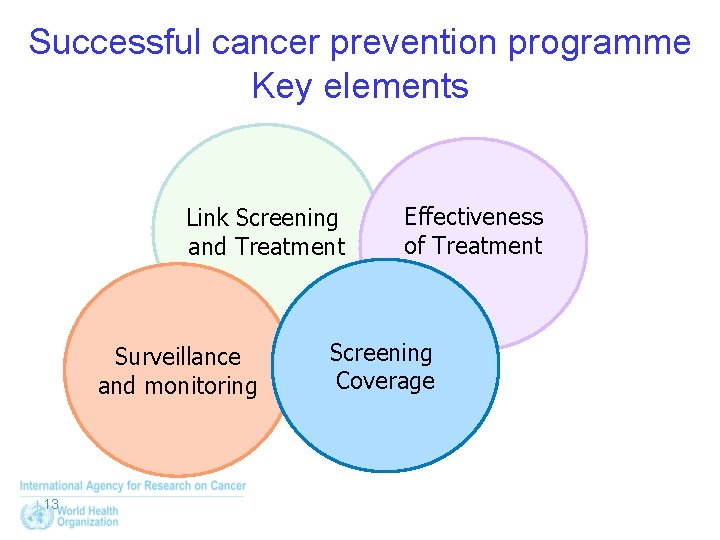
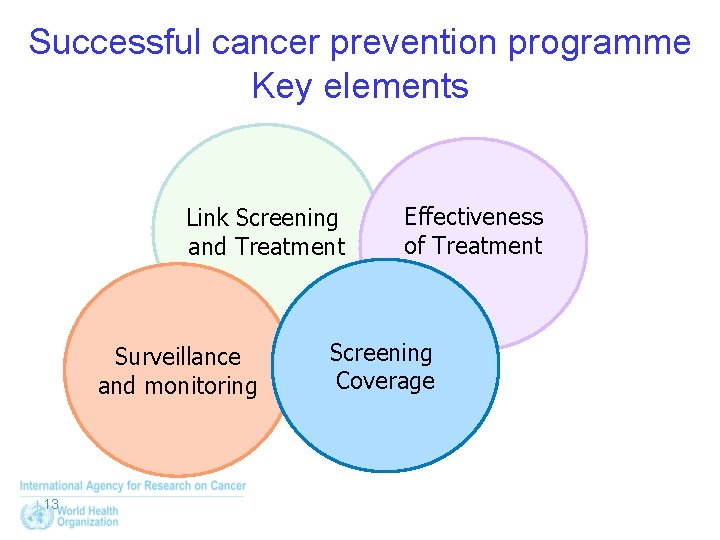
Successful cancer prevention programme Key elements Link Screening and Treatment Surveillance and monitoring 13 Effectiveness of Treatment Screening Coverage

Evaluation of screening programmes Process measures Outcome measures 14
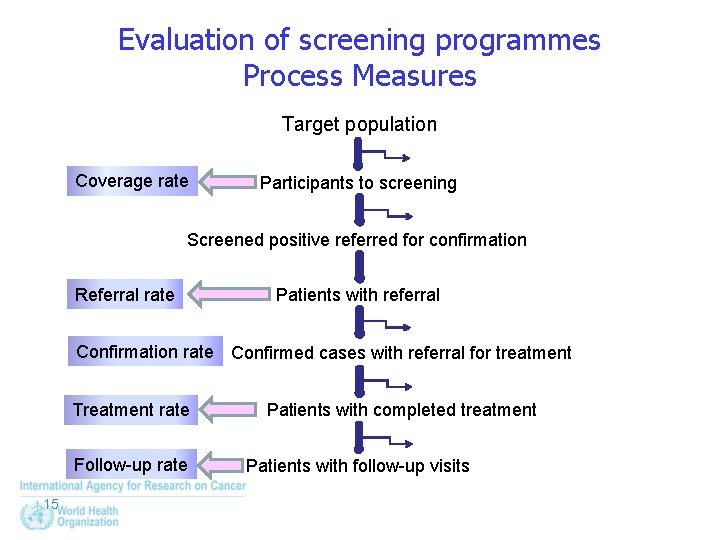
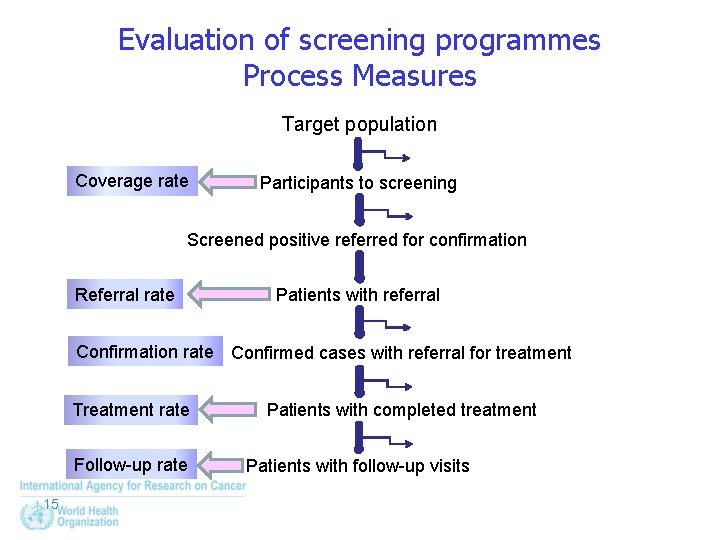
Evaluation of screening programmes Process Measures Target population Coverage rate Participants to screening Screened positive referred for confirmation Referral rate Patients with referral Confirmation rate Confirmed cases with referral for treatment Treatment rate Follow-up rate 15 Patients with completed treatment Patients with follow-up visits
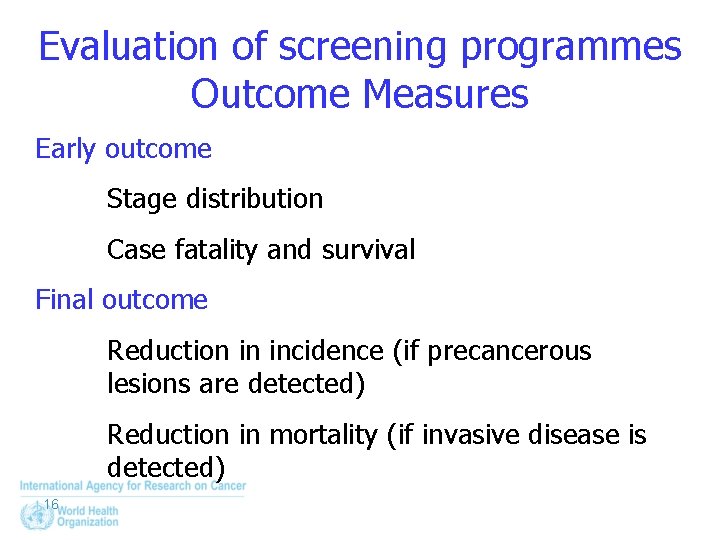
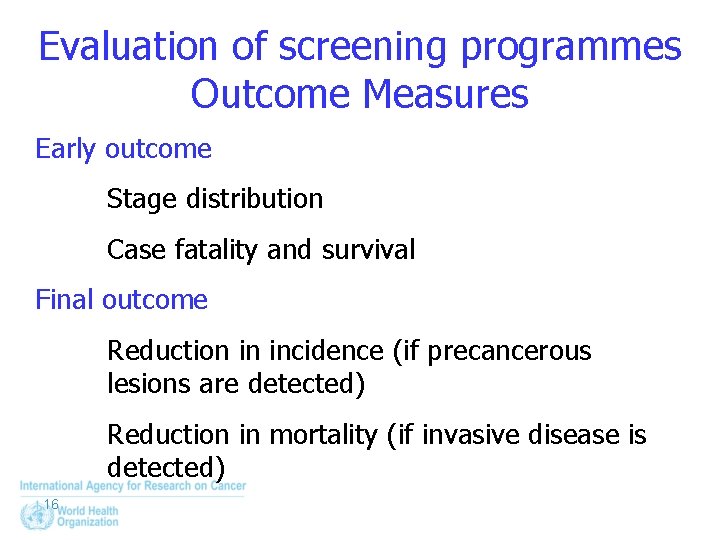
Evaluation of screening programmes Outcome Measures Early outcome Stage distribution Case fatality and survival Final outcome Reduction in incidence (if precancerous lesions are detected) Reduction in mortality (if invasive disease is detected) 16
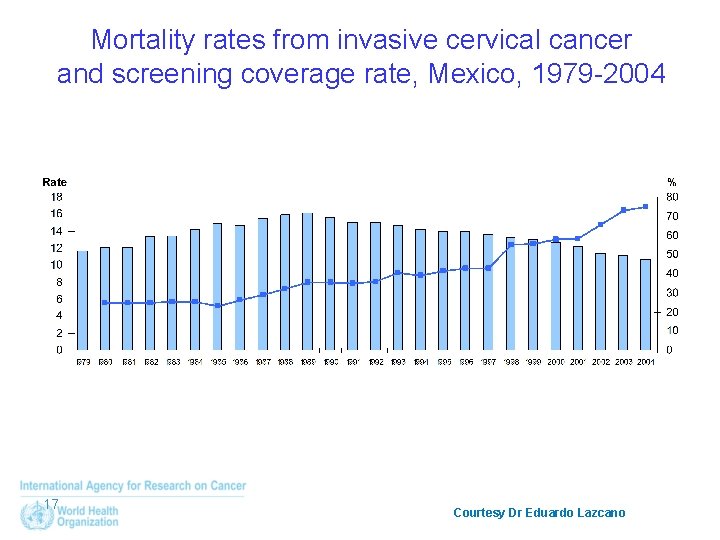
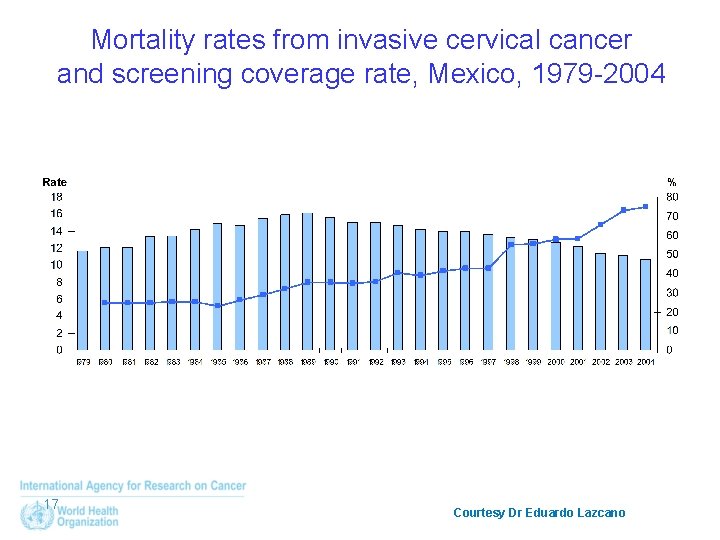
Mortality rates from invasive cervical cancer and screening coverage rate, Mexico, 1979 -2004 17 Courtesy Dr Eduardo Lazcano
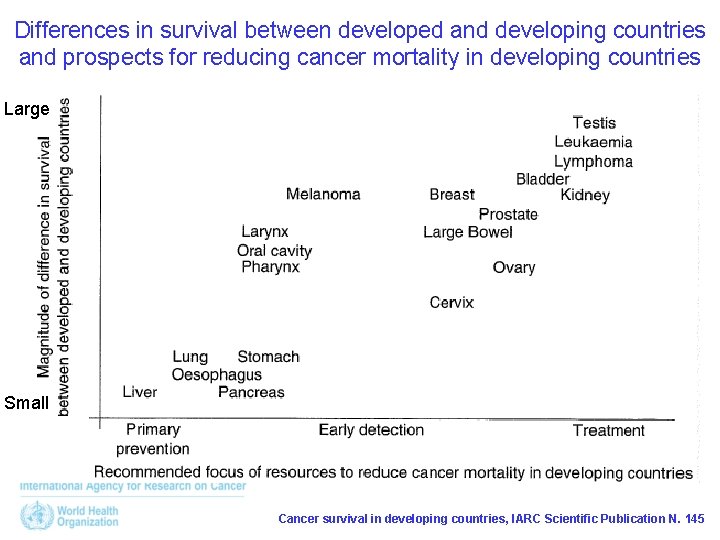
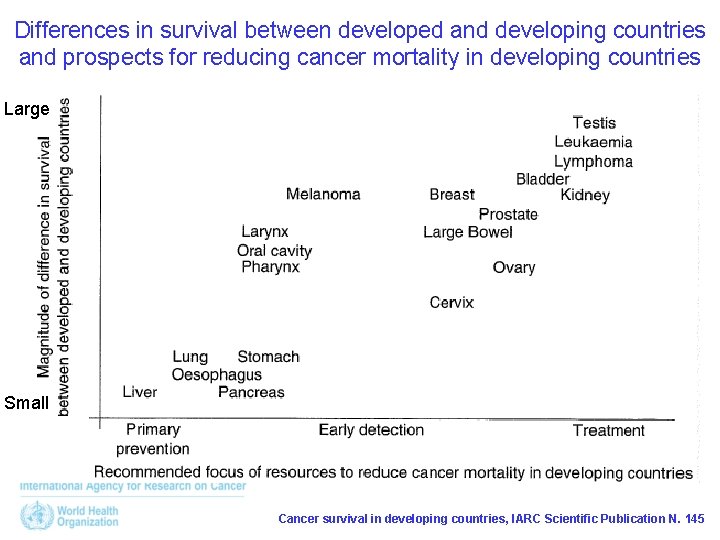
Differences in survival between developed and developing countries and prospects for reducing cancer mortality in developing countries Large Small Cancer survival in developing countries, IARC Scientific Publication N. 145

Suitable cancers for early detection in LMIC • Oral cancer – Visual inspection by trained health workers – Health education to prompt symptomatic high-risk individuals • Cervical cancer – Visual inspection methods and HPV-DNA testing as alternatives of Pap smear – Health education on risk factors, symptoms and signs of cervical carcinoma – See-and-treat approach by trained health workers and physicians • Breast cancer – Health education to improve awareness and to motivate high -risk women to demand early detection – Clinical breast examination and mammography may then be used • Digestive tract cancer – Faecal Occult Blood Test (FOBT) as screening test followed by colonoscopy if FOBT positive 19

Non-suitable cancers for early detection in LMIC • Liver cancer – High fatality rate and ineffective treatment – Primary prevention • Lung cancer – Chest radiography and sputum cytology are ineffective – CT scan screening is not feasible – Tobacco control • Prostate cancer – PSA testing with considerable over-diagnosis – Early detection not recommended for developing countries • Ovarian cancer – Efficacy of α-fetoprotein and ultrasound is not yet known – Screening is not feasible 20
In the context of the WHO action plan • Implementation of tobacco control • Prevention of liver cancer through hepatitis B immunization • Establishment of cancer registration to monitor cancer incidence • Prevention of cervical cancer through screening (visual inspection with acetic acid [VIA]) linked with timely treatment of precancerous lesions • Vaccination against human papillomavirus, as appropriate if cost effective and affordable, according to national programmes and policies 21
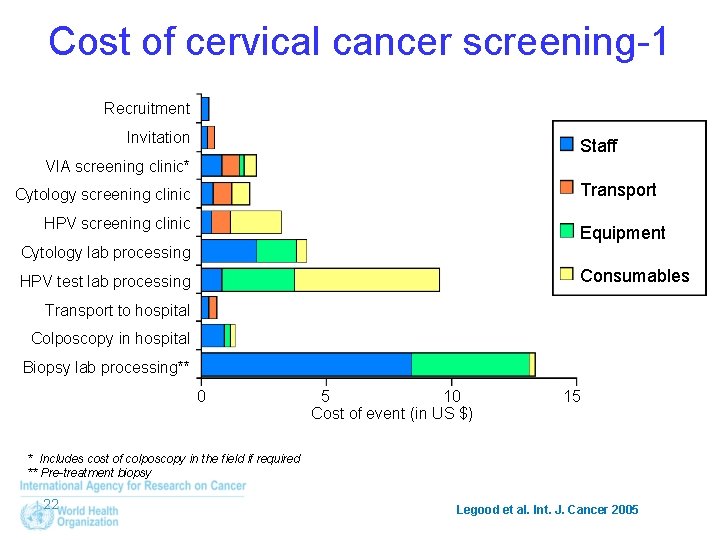
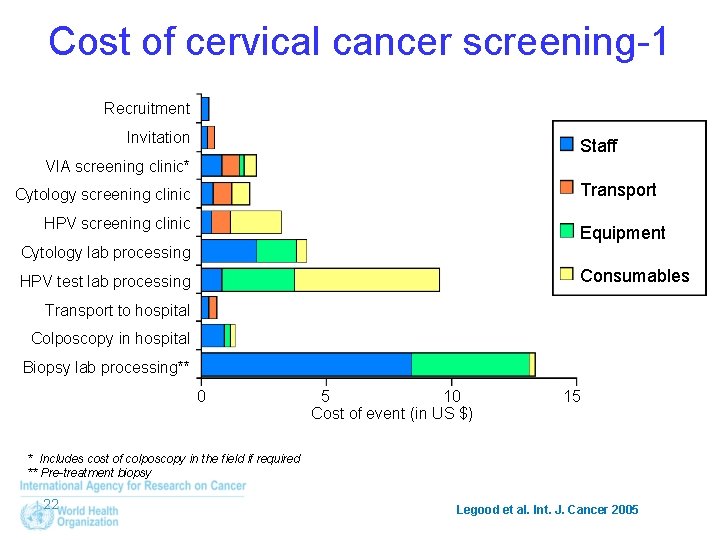
Cost of cervical cancer screening-1 Recruitment Invitation Staff VIA screening clinic* Transport Cytology screening clinic HPV screening clinic Equipment Cytology lab processing Consumables HPV test lab processing Transport to hospital Colposcopy in hospital Biopsy lab processing** 0 5 10 Cost of event (in US $) 15 * Includes cost of colposcopy in the field if required ** Pre-treatment biopsy 22 Legood et al. Int. J. Cancer 2005
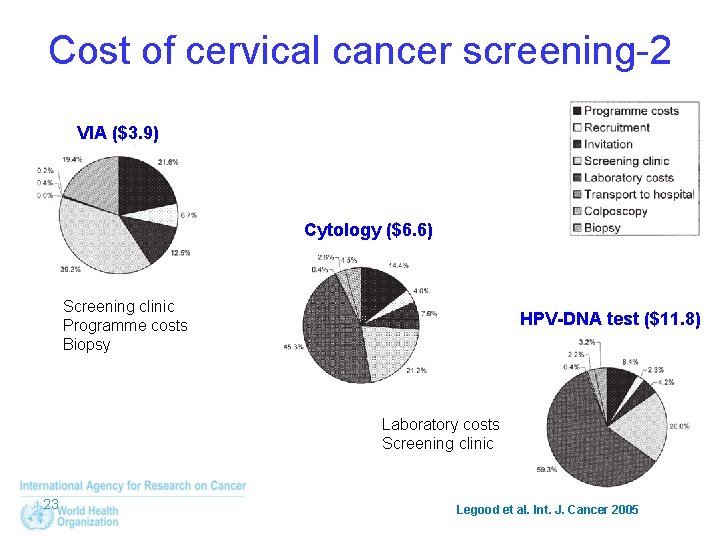
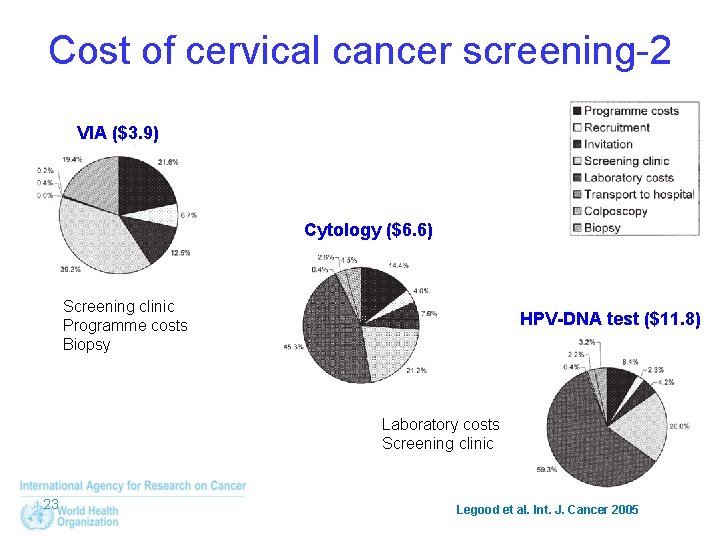
Cost of cervical cancer screening-2 VIA ($3. 9) Cytology ($6. 6) Screening clinic Programme costs Biopsy HPV-DNA test ($11. 8) Laboratory costs Screening clinic 23 Legood et al. Int. J. Cancer 2005
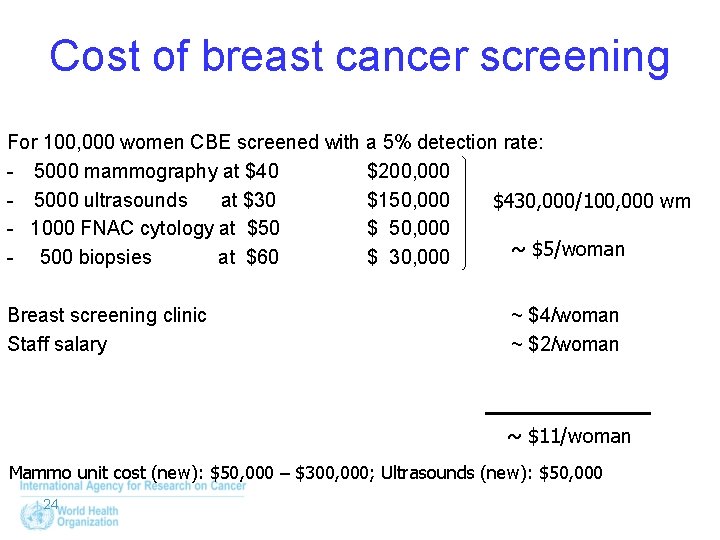
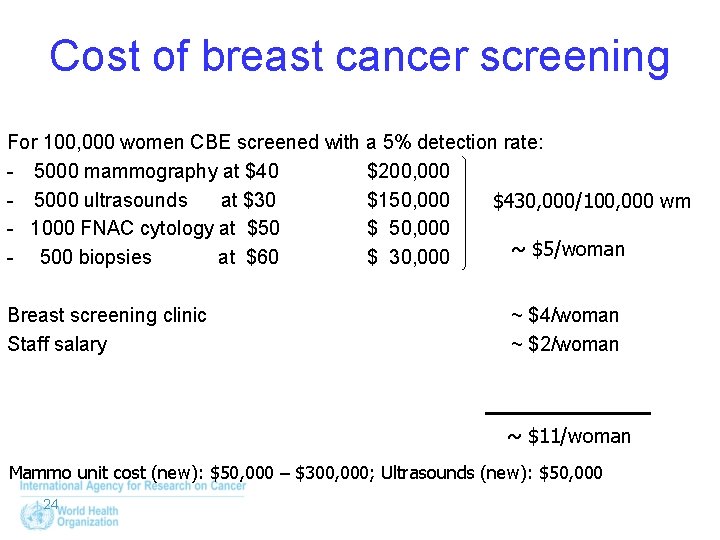
Cost of breast cancer screening For 100, 000 women CBE screened with a 5% detection rate: - 5000 mammography at $40 $200, 000 - 5000 ultrasounds at $30 $150, 000 $430, 000/100, 000 wm - 1000 FNAC cytology at $50 $ 50, 000 ~ $5/woman - 500 biopsies at $60 $ 30, 000 Breast screening clinic Staff salary ~ $4/woman ~ $2/woman ~ $11/woman Mammo unit cost (new): $50, 000 – $300, 000; Ultrasounds (new): $50, 000 24

Thank you for your kind attention! 25
 Primary prevention secondary prevention tertiary prevention
Primary prevention secondary prevention tertiary prevention National breast and cervical cancer early detection program
National breast and cervical cancer early detection program National breast and cervical cancer early detection program
National breast and cervical cancer early detection program Starvation deadlock
Starvation deadlock Deadlock prevention avoidance and detection
Deadlock prevention avoidance and detection Hpv cancer prevention
Hpv cancer prevention Breast structure
Breast structure Ekd system
Ekd system Early cpr and early defibrillation can: *
Early cpr and early defibrillation can: * Chapter 24 the immune and lymphatic systems and cancer
Chapter 24 the immune and lymphatic systems and cancer The lymphatic capillaries are
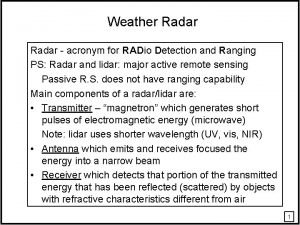
The lymphatic capillaries are Radar stands for
Radar stands for Error detection in computer networks
Error detection in computer networks Hazard detection and resolution
Hazard detection and resolution Hazard detection and resolution
Hazard detection and resolution Deadlock detection and recovery
Deadlock detection and recovery Firewalls and intrusion detection systems
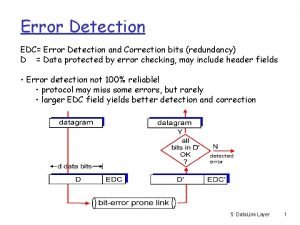
Firewalls and intrusion detection systems Error detection and correction in data link layer
Error detection and correction in data link layer Concept of redundancy in error detection and correction
Concept of redundancy in error detection and correction Collision detection and resolution
Collision detection and resolution Collide and slide algorithm
Collide and slide algorithm 해밍코드 인코더
해밍코드 인코더 Smaller edc field yields better detection and correction
Smaller edc field yields better detection and correction Crc example
Crc example Error correction in computer networks
Error correction in computer networks Crc error detection
Crc error detection