Atraumatic Care of Children and Families 2017 What


- Slides: 40

Atraumatic Care of Children and Families 2017
What is, “Atraumatic Care” • Therapeutic care that minimizes or eliminates the psychological and physical distress experienced by children and their families in the health care system • Provide nursing care that decreases the child’s exposure to stressful situations and prevents or minimizes pain and bodily injury.
Atraumatic care • Guiding children and their families through the health care experience using a family-centered approach by: – promoting family roles – fostering family support of the child – providing appropriate information.
Techniques for Providing Atraumatic Care • Pediatric nurses must be vigilant for situations that cause distress and therefore must be able to identify potential stressors
What is, “Atraumatic Care” • Therapeutic communication – Goal directed – Focused and purposeful • Therapeutic play – Provides emotional outlet or coping devices • Child education – Helps child understand the reason for the hospitalization/procedures
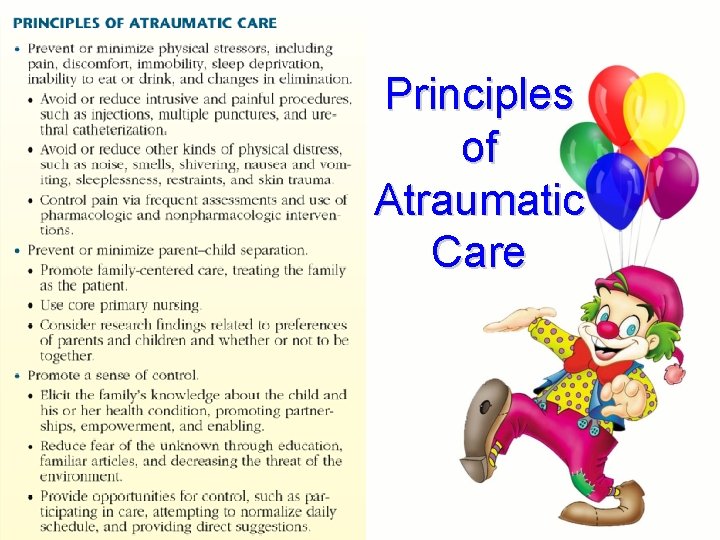
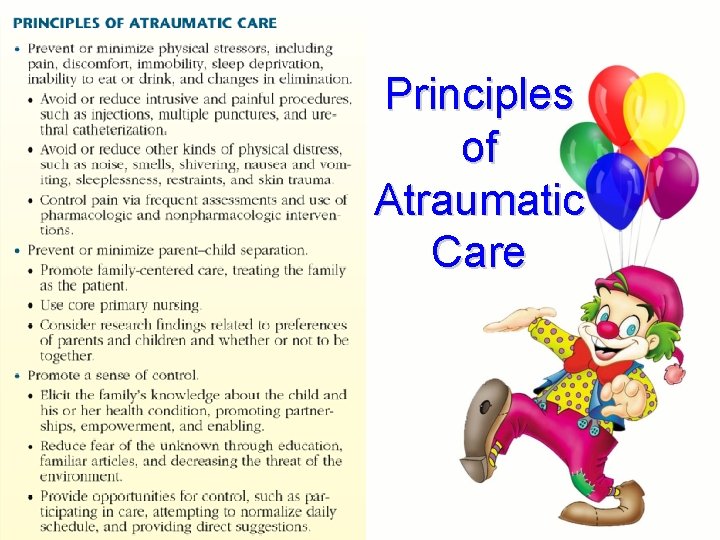
Principles of Atraumatic Care
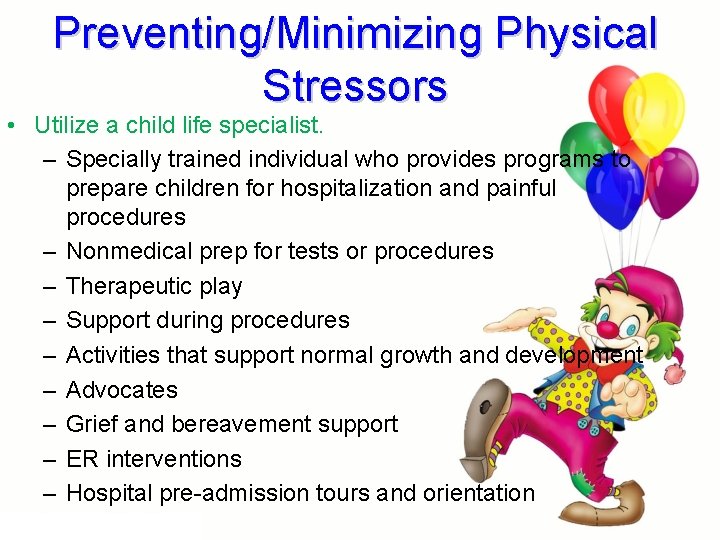
Preventing/Minimizing Physical Stressors • Utilize a child life specialist. – Specially trained individual who provides programs to prepare children for hospitalization and painful procedures – Nonmedical prep for tests or procedures – Therapeutic play – Support during procedures – Activities that support normal growth and development – Advocates – Grief and bereavement support – ER interventions – Hospital pre-admission tours and orientation
Common Procedures • Intravenous lines – Dehydration – Fluid maintenance or replacement – Before diagnostic testing – Blood product placement – Medication administration – Preoperatively – Types • Peripheral line • Normal saline locks
Common Procedures (cont’d) • Intravenous lines (cont’d) – Types (cont’d) • Central venous access devices • Peripherally inserted central catheter line (PICC) • Vascular access port (Infus-A-Port) – Monitor for signs and symptoms of infection: change in temperature, erythema, edema, pain at IV site, tenderness on palpation
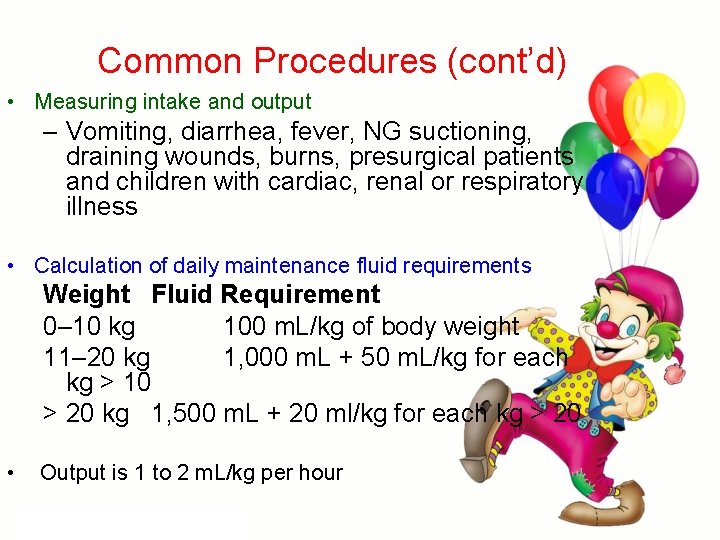
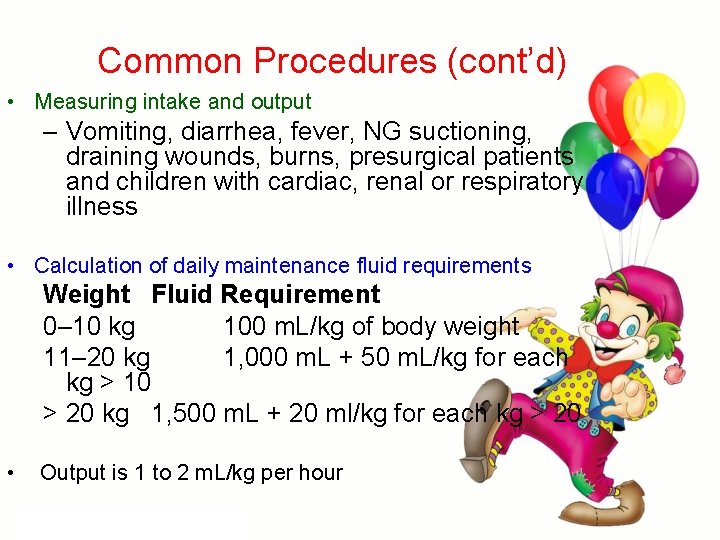
Common Procedures (cont’d) • Measuring intake and output – Vomiting, diarrhea, fever, NG suctioning, draining wounds, burns, presurgical patients and children with cardiac, renal or respiratory illness • Calculation of daily maintenance fluid requirements Weight Fluid Requirement 0– 10 kg 100 m. L/kg of body weight 11– 20 kg 1, 000 m. L + 50 m. L/kg for each kg > 10 > 20 kg 1, 500 m. L + 20 ml/kg for each kg > 20 • Output is 1 to 2 m. L/kg per hour
Common Procedures (cont’d) • X-ray exams – Diagnostic purposes – Checking tube placement • Specimen collection – Urine sample collection – Stool sample collection – Blood sample collection – Throat culture collection – Cerebrospinal fluid collection
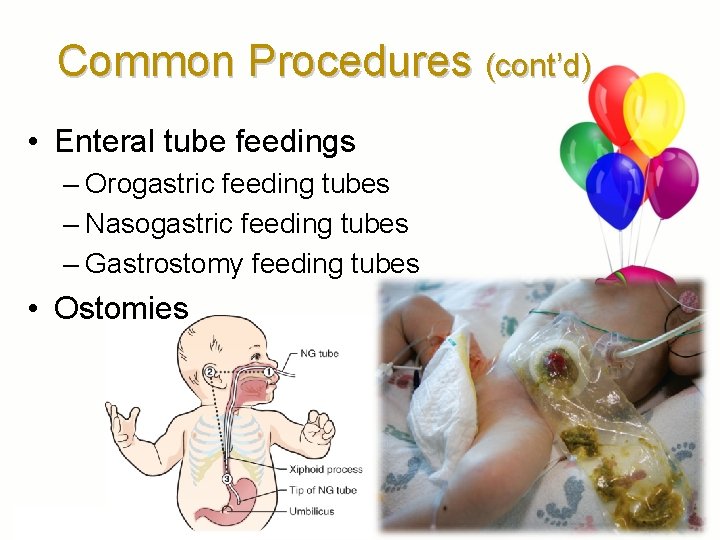
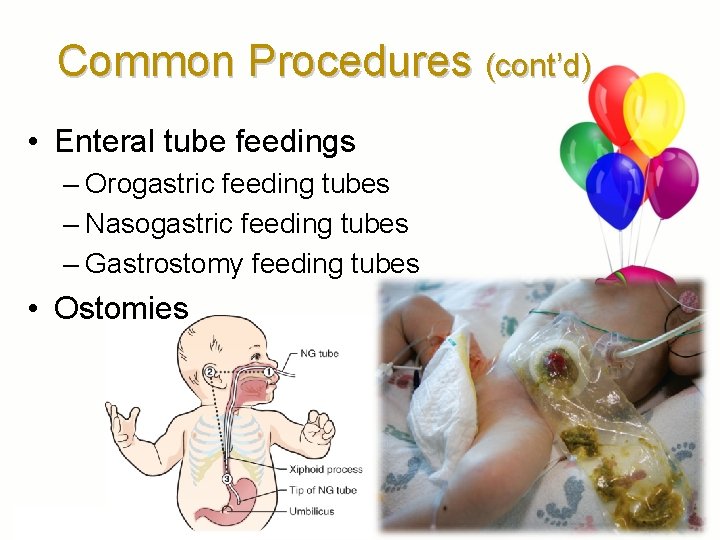
Common Procedures (cont’d) • Enteral tube feedings – Orogastric feeding tubes – Nasogastric feeding tubes – Gastrostomy feeding tubes • Ostomies
Common Procedures (cont’d) • Restraining the child – May be necessary to ensure safety during procedure or to prevent injury to operative site – Inform parents and child why restraint is necessary – Extremity is checked every 15 minutes for first hour after initial application – Child must be checked and skin condition documented every 1– 2 hours – Physical restraint • Elbow restraint • Papoose restraint – Pharmacological restraint • Chloral hydrate (Aquachloral)
Preparing Children for Procedures • Explaining procedures – Preparing an infant, toddler, preschooler, school-age child, and adolescent for procedure – Distraction – Environment – Preparing the parent – Use developmentally appropriate words
Informed Consent • Provides patient with necessary knowledge to make decision regarding health care • Implies that person understands benefits and risks of treatment or refusal of treatment • Legal age is required • Required before diagnostic procedures, medical treatments or surgical procedures, immunizations, or any treatment with inherent risks
Preventing/Minimizing Physical Stressors (cont) • Minimize physical distress during procedures. – Use positions that are comfortable to the child. – Therapeutic hugging – Use distraction methods • Have the child point toes inward and wiggle them. • Ask the child to squeeze your hand. • Encourage the child to count aloud. • Sing a song and have the child sing along. • Point out the pictures on the ceiling. • Have the child blow bubbles. • Play music appealing to the child
Before the Procedure • • • Decrease anxiety (to whom? ? ? ) Promote child’s cooperation Support family Improve coping skills Improve recovery Increase trust
During the Procedure • Use a firm, confident, and positive approach gives family a sense of security • Allow child to express anxiety and feelings (almost all behavior is acceptable) • Toddlers and Preschoolers will resist despite the best prep – • BEING HELD DOWN OR RESTRAINED IS TRAUMATIZING TO THE VERY YOUNG • Older-distraction might help
After the Procedure • Hold and comfort child • Cuddle and soothe baby • Distract with toy or puppet – get the kid to play! • Provide older child to express feelings and be comforted if they want • REMEMBER: praise child regardless of response!
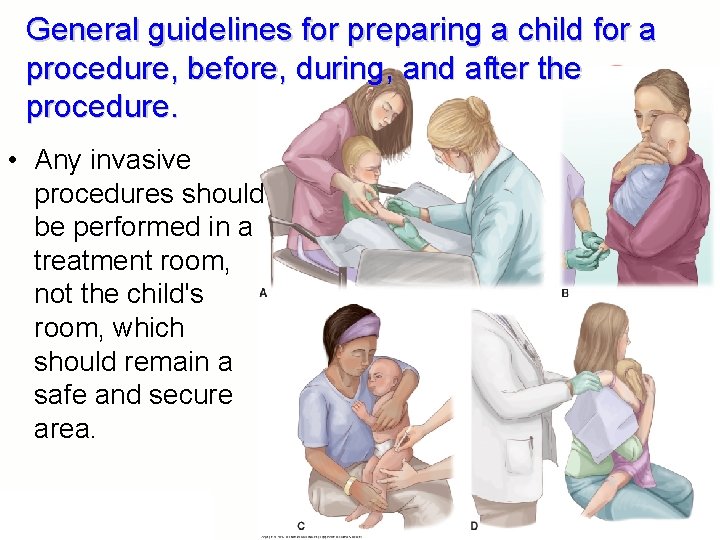
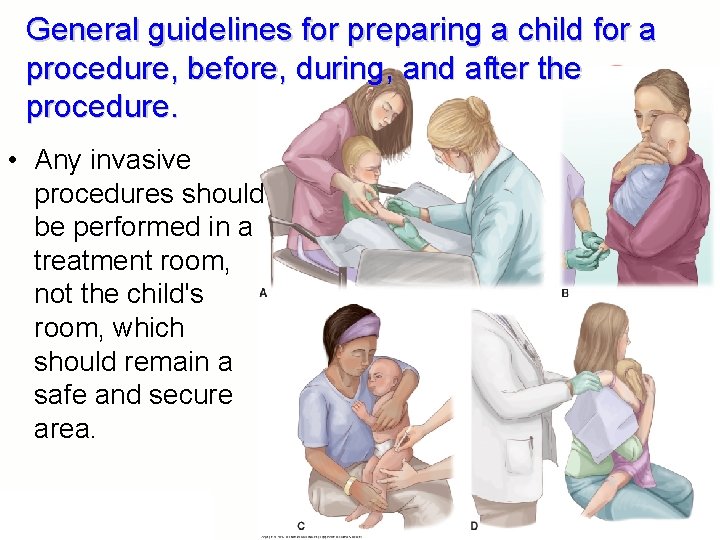
General guidelines for preparing a child for a procedure, before, during, and after the procedure. • Any invasive procedures should be performed in a treatment room, not the child's room, which should remain a safe and secure area.
Restraining a Child – May be necessary to ensure safety during procedure or to prevent injury to operative site – Inform parents and child why restraint is necessary – Extremity is checked every 15 minutes for first hour after initial application – Child must be checked and skin condition documented every 1– 2 hours – Physical restraint • Elbow restraint • Papoose restraint – Pharmacological restraint • Chloral hydrate (Aquachloral)
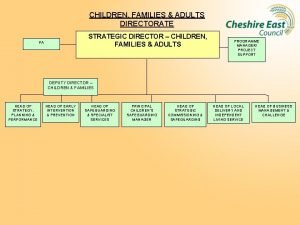
Focus of Family-Centered Care (the American Academy of Pediatrics) • Respect for the child and family • Recognition of the effects of cultural, racial, ethnic, and socioeconomic diversity on the family’s health care experience • Identification of and expansion of the family’s strengths • Support of the family’s choices related to the child’s health care • Maintenance of flexibility
Focus of Family-Centered Care (cont. ) • Provision of honest, unbiased information in an affirming and useful approach • Assistance with the emotional and other support the child and family require • Collaboration with families • Empowerment of families
Positive Outcomes of Family. Centered Care for Children • Anxiety is decreased. • Children are calmer and pain management is enhanced. • Recovery times are shortened. • Families’ confidence and problem-solving skills are improved. • Communication between the health care team and the family is also improved. • A decrease in health care costs is seen. • Health care resources are used more effectively.
Providing a Sense of Control for the Hospitalized Child • Provide effective communication and teaching. – Find a balance between neutral and affective communication. – Use verbal communication and nonverbal communication. – Use developmental techniques for communicating with children. • Assist family to obtain necessary information and resources.
Communication and teaching • • • Open-ended questions that don’t restrict Redirect the conversation to maintain focus Use reflection to clarify parent’s feelings Paraphrase Acknowledge emotions Demonstrate active listening, using the child’s own words • Non-verbal – Relax, allowing time – Eye contact – Demonstrate active listening
The Child’s Culture • Understanding and respecting the child’s culture helps foster good communication and improves child and family education about health care. • Assess each family's beliefs and practices by asking questions and listening. • List of examples of appropriate interview questions for assessing a child's culture.
Working With an Interpreter • Help the interpreter prepare and understand what needs to be done ahead of time. – The interpreter is the communication bridge, not the content expert; the interpreter’s timing may not match that of others involved. • Speak slowly and clearly; avoid jargon. • Pause every few sentences so the interpreter can translate your information. • Talk directly to the family, not the interpreter. • Give the family and the interpreter a break.
Working With an Interpreter (cont. ) • Express the information in two or three different ways if needed. • Use an interpreter to help ensure the family can read and understand translated written materials. • Avoid side conversations during sessions. • Remember that just because someone speaks another language, it doesn’t mean he or she will be a good interpreter. • Do not use children as interpreters.
Goals of Child and Family Education • Improve the child and family’s health literacy • Encourage communication with physicians or nurse practitioners • Improve health outcomes and promote healthy lifestyles • Encourage involvement of child and family in care and decision making about care • Improve compliance with care and treatment plan • Promote a sense of autonomy and control
Specific Learning Principles Related to Parents • Adults are self-directed. • Adults are problem focused and task oriented. • Adults want an immediate need satisfied. • Adults value past experiences and beliefs.
Questions Appropriate to Ask When Performing a Cultural Assessment • • Who is the person caring for the child at home? Who is the authority figure in the family? What is the social support structure? Are there any special dietary needs and concerns? • Are any traditional health practices used? • Are any special clothes or other items used to help maintain health? • What religious beliefs, ceremonies, and spiritual practices are important?
Making Child and Parents Knowledgeable • Families need to be knowledgeable about such things as their child’s condition, the health care management plan, and when and how to contact the physician or nurse practitioner in order to participate fully in making health care decisions • To provide atraumatic care to children, pediatric nurses must focus on teaching goals and begin teaching at the earliest opportunity.
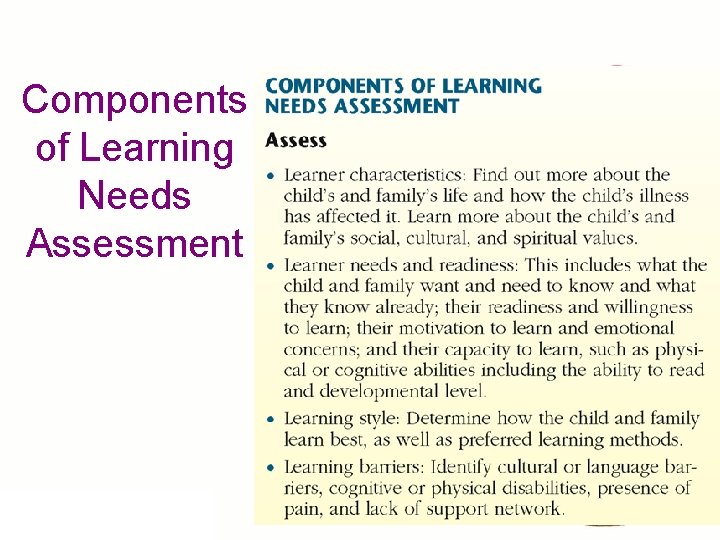
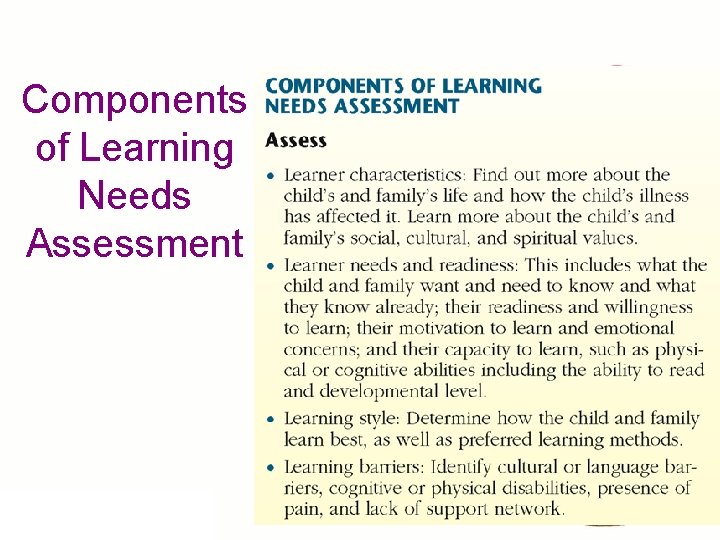
Components of Learning Needs Assessment
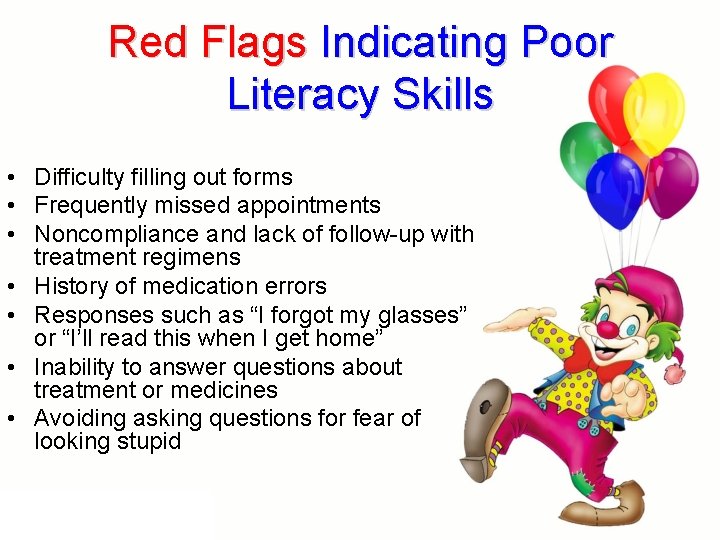
Red Flags Indicating Poor Literacy Skills • Difficulty filling out forms • Frequently missed appointments • Noncompliance and lack of follow-up with treatment regimens • History of medication errors • Responses such as “I forgot my glasses” or “I’ll read this when I get home” • Inability to answer questions about treatment or medicines • Avoiding asking questions for fear of looking stupid
Helping Poor Literacy Skills • • • Use pictures Use videos Color-coded medications Record audiotape Repeat verbal instructions and have them repeat it • Return demonstration • Utilize a “back-up” family member-not the kid!
Techniques to Improve Learning • Slow down and repeat information often. • Speak in conversational style using plain language. • “Chunk” information and teach in small bites. • Prioritize information and teach “survival skills” first. • Use visuals. • Teach using an interactive, “hands on” approach.
Evaluating Learning • The child or family demonstrates a skill. • The child or family repeats back or teaches back the information in own words. • The child or family answers open-ended questions. • The child or family responds to a pretend scenario in their home.
Documentation of Child and Family Teaching • The learning needs assessment • Information on the child’s medical condition and plan of care • Goals of child education; date goal is met • Teaching method used and how received by child and family • Medications, including drug–drug and drug –food interactions • Modified diets and nutritional needs • Safe use of medical equipment • Follow-up care and community resources discussed

That’s It!
 Autramatic care
Autramatic care Atraumatic care meaning
Atraumatic care meaning Atraumatic care definition
Atraumatic care definition Konsep atraumatic care
Konsep atraumatic care Big families vs small families
Big families vs small families Effective support for children and families in essex
Effective support for children and families in essex Georgia department of children and families
Georgia department of children and families Types of care primary secondary tertiary
Types of care primary secondary tertiary Juvenile act
Juvenile act Tycare
Tycare Prairie cardiovascular consultants springfield il
Prairie cardiovascular consultants springfield il Hornak home improvement
Hornak home improvement Safeguarding children care certificate
Safeguarding children care certificate Nj children's system of care
Nj children's system of care Characteristics of logic families
Characteristics of logic families Compare and contrast the bach and marsalis families
Compare and contrast the bach and marsalis families Compare and contrast the bach and marsalis families
Compare and contrast the bach and marsalis families Marriages and families changes choices and constraints
Marriages and families changes choices and constraints Marriages and families changes choices and constraints
Marriages and families changes choices and constraints Unit 2 equality diversity and rights
Unit 2 equality diversity and rights Families professionals and exceptionality
Families professionals and exceptionality Family of orientation
Family of orientation Dugdale
Dugdale The interlopers summary
The interlopers summary Successful marriages and families
Successful marriages and families Families and periods of the periodic table
Families and periods of the periodic table Chapter 9. voices and instrument families
Chapter 9. voices and instrument families Arizona fair wages and healthy families act
Arizona fair wages and healthy families act Serving individuals and families
Serving individuals and families Serving individuals and families
Serving individuals and families The needs of families and suitability for the local
The needs of families and suitability for the local Working with culturally and linguistically diverse families
Working with culturally and linguistically diverse families Vanier institute of the family definition
Vanier institute of the family definition Families professionals and exceptionality
Families professionals and exceptionality Work and families act 2006
Work and families act 2006 Care certificate standard 3
Care certificate standard 3 Este fenomenul prin care corpurile care contin fier
Este fenomenul prin care corpurile care contin fier Palliative care vs hospice care
Palliative care vs hospice care Clasificarea mamiferelor dupa modul de hranire
Clasificarea mamiferelor dupa modul de hranire Care sunt simturile prin care sunt evocate
Care sunt simturile prin care sunt evocate Care certificate 13 answers
Care certificate 13 answers