Integrated Health Care for Children Families Current Challenges

- Slides: 18
Integrated Health Care for Children & Families: Current Challenges and Opportunities SB 231 Primary Care Payment Reform Collaborative June 10, 2016 E. Dawn Creach, MS Program Manager of Medical Home Delivery & Innovation 1
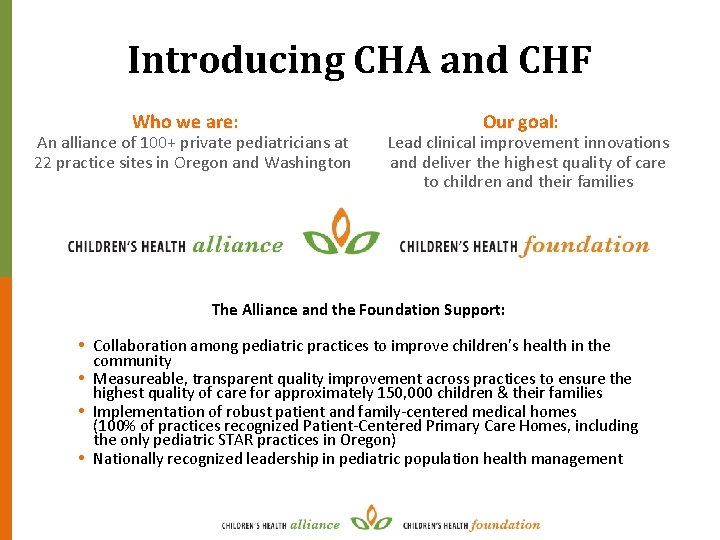
Introducing CHA and CHF Who we are: An alliance of 100+ private pediatricians at 22 practice sites in Oregon and Washington Our goal: Lead clinical improvement innovations and deliver the highest quality of care to children and their families The Alliance and the Foundation Support: • Collaboration among pediatric practices to improve children’s health in the community • Measureable, transparent quality improvement across practices to ensure the highest quality of care for approximately 150, 000 children & their families • Implementation of robust patient and family-centered medical homes (100% of practices recognized Patient-Centered Primary Care Homes, including the only pediatric STAR practices in Oregon) • Nationally recognized leadership in pediatric population health management 2
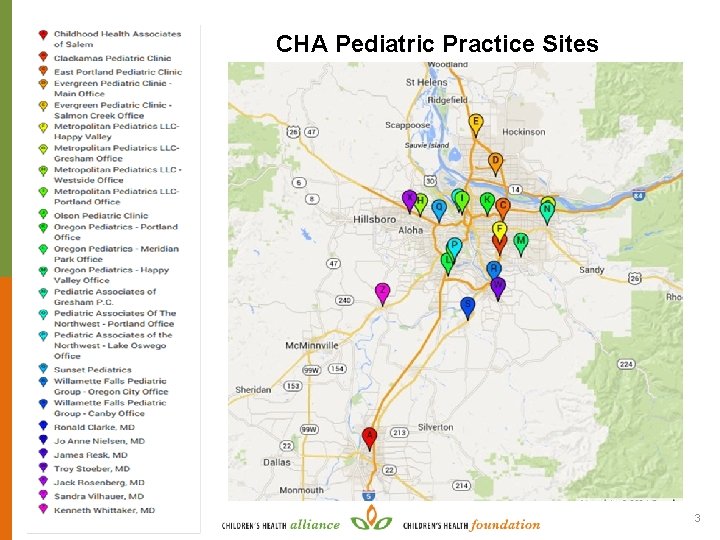
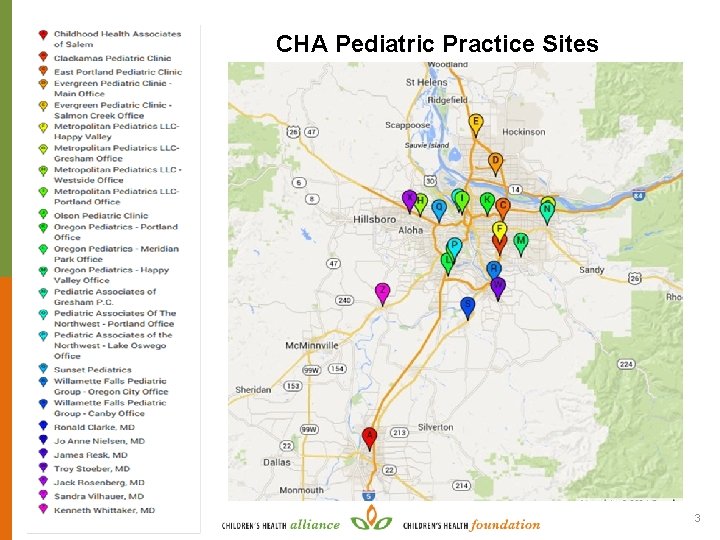
CHA Pediatric Practice Sites 3
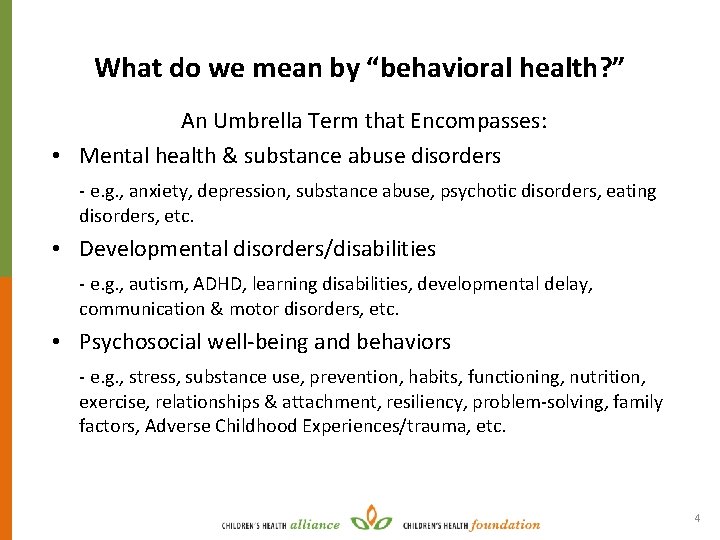
What do we mean by “behavioral health? ” An Umbrella Term that Encompasses: • Mental health & substance abuse disorders - e. g. , anxiety, depression, substance abuse, psychotic disorders, eating disorders, etc. • Developmental disorders/disabilities - e. g. , autism, ADHD, learning disabilities, developmental delay, communication & motor disorders, etc. • Psychosocial well-being and behaviors - e. g. , stress, substance use, prevention, habits, functioning, nutrition, exercise, relationships & attachment, resiliency, problem-solving, family factors, Adverse Childhood Experiences/trauma, etc. 4
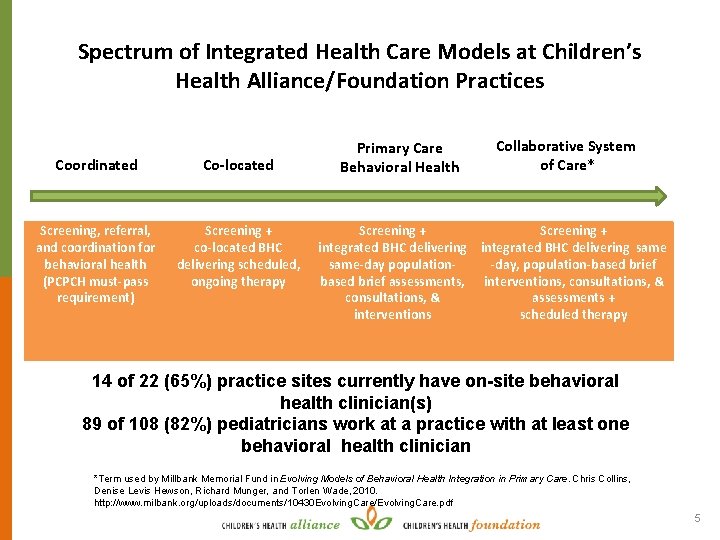
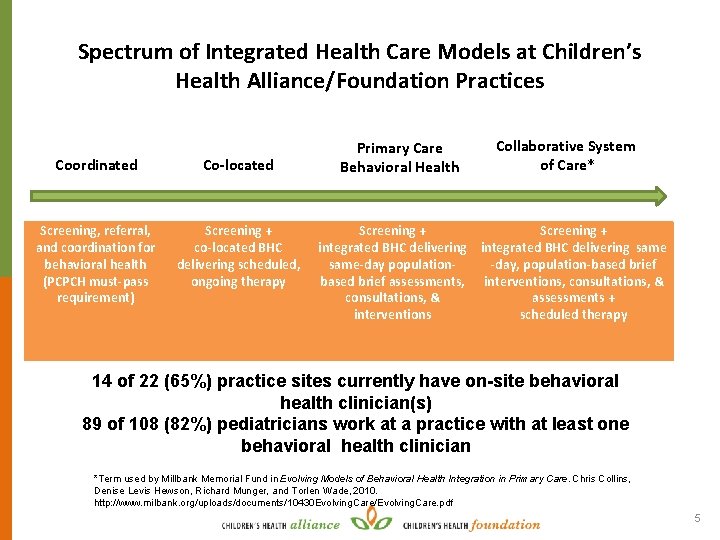
Spectrum of Integrated Health Care Models at Children’s Health Alliance/Foundation Practices Coordinated Co-located Screening, referral, and coordination for behavioral health (PCPCH must-pass requirement) Screening + co-located BHC delivering scheduled, ongoing therapy Primary Care Behavioral Health Collaborative System of Care* Screening + integrated BHC delivering same-day population-day, population-based brief assessments, interventions, consultations, & assessments + interventions scheduled therapy 14 of 22 (65%) practice sites currently have on-site behavioral health clinician(s) 89 of 108 (82%) pediatricians work at a practice with at least one behavioral health clinician *Term used by Millbank Memorial Fund in Evolving Models of Behavioral Health Integration in Primary Care. Chris Collins, Denise Levis Hewson, Richard Munger, and Torlen Wade, 2010. http: //www. milbank. org/uploads/documents/10430 Evolving. Care/Evolving. Care. pdf 5
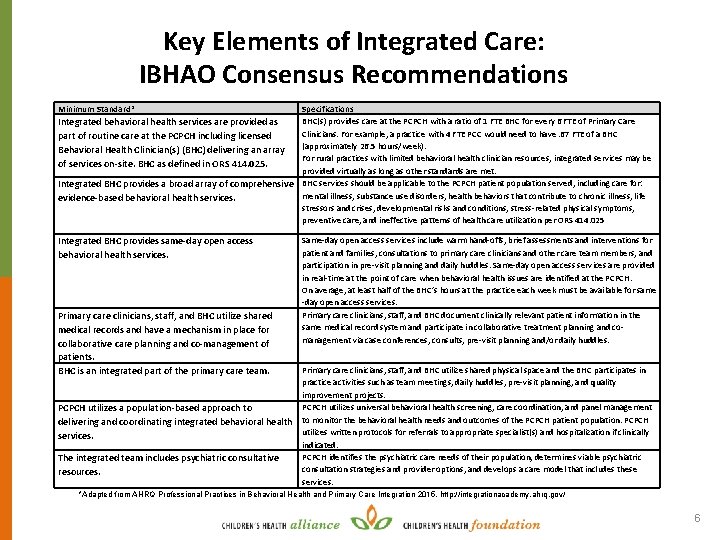
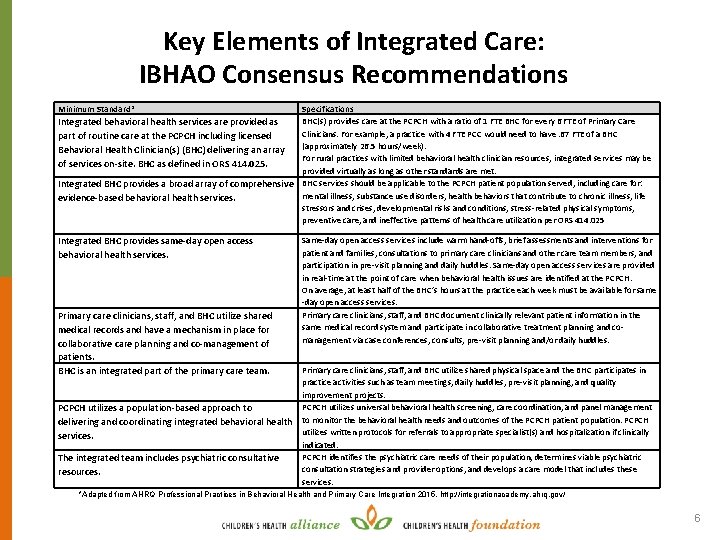
Key Elements of Integrated Care: IBHAO Consensus Recommendations Minimum Standard* Specifications BHC(s) provides care at the PCPCH with a ratio of 1 FTE BHC for every 6 FTE of Primary Care Integrated behavioral health services are provided as Clinicians. For example, a practice with 4 FTE PCC would need to have. 67 FTE of a BHC part of routine care at the PCPCH including licensed (approximately 26. 5 hours/week). Behavioral Health Clinician(s) (BHC) delivering an array For rural practices with limited behavioral health clinician resources, integrated services may be of services on-site. BHC as defined in ORS 414. 025. provided virtually as long as other standards are met. Integrated BHC provides a broad array of comprehensive BHC services should be applicable to the PCPCH patient population served, including care for: mental illness, substance use disorders, health behaviors that contribute to chronic illness, life evidence-based behavioral health services. stressors and crises, developmental risks and conditions, stress-related physical symptoms, preventive care, and ineffective patterns of health care utilization per ORS 414. 025 Integrated BHC provides same-day open access behavioral health services. Primary care clinicians, staff, and BHC utilize shared medical records and have a mechanism in place for collaborative care planning and co-management of patients. BHC is an integrated part of the primary care team. PCPCH utilizes a population-based approach to delivering and coordinating integrated behavioral health services. The integrated team includes psychiatric consultative resources. Same-day open access services include warm hand-offs, brief assessments and interventions for patient and families, consultations to primary care clinicians and other care team members, and participation in pre-visit planning and daily huddles. Same-day open access services are provided in real-time at the point of care when behavioral health issues are identified at the PCPCH. On average, at least half of the BHC’s hours at the practice each week must be available for same -day open access services. Primary care clinicians, staff, and BHC document clinically relevant patient information in the same medical record system and participate in collaborative treatment planning and comanagement via case conferences, consults, pre-visit planning and/or daily huddles. Primary care clinicians, staff, and BHC utilize shared physical space and the BHC participates in practice activities such as team meetings, daily huddles, pre-visit planning, and quality improvement projects. PCPCH utilizes universal behavioral health screening, care coordination, and panel management to monitor the behavioral health needs and outcomes of the PCPCH patient population. PCPCH utilizes written protocols for referrals to appropriate specialist(s) and hospitalization if clinically indicated. PCPCH identifies the psychiatric care needs of their population, determines viable psychiatric consultation strategies and provider options, and develops a care model that includes these services. *Adapted from AHRQ Professional Practices in Behavioral Health and Primary Care Integration 2015. http: //integrationacademy. ahrq. gov/ 6
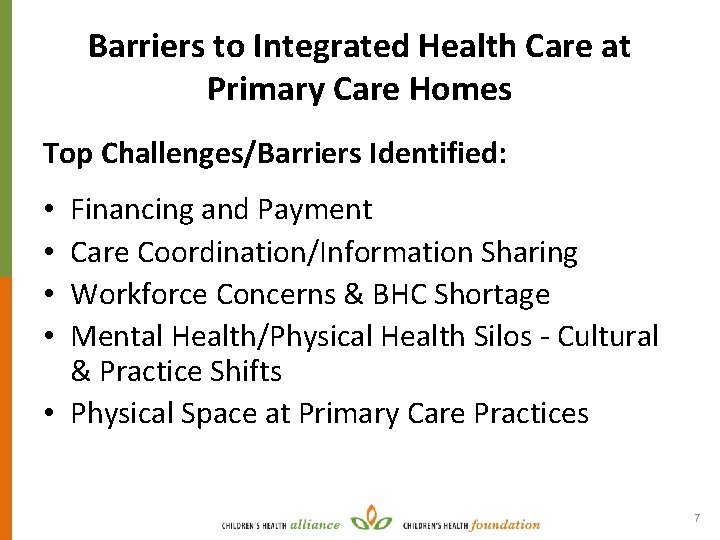
Barriers to Integrated Health Care at Primary Care Homes Top Challenges/Barriers Identified: Financing and Payment Care Coordination/Information Sharing Workforce Concerns & BHC Shortage Mental Health/Physical Health Silos - Cultural & Practice Shifts • Physical Space at Primary Care Practices • • 7
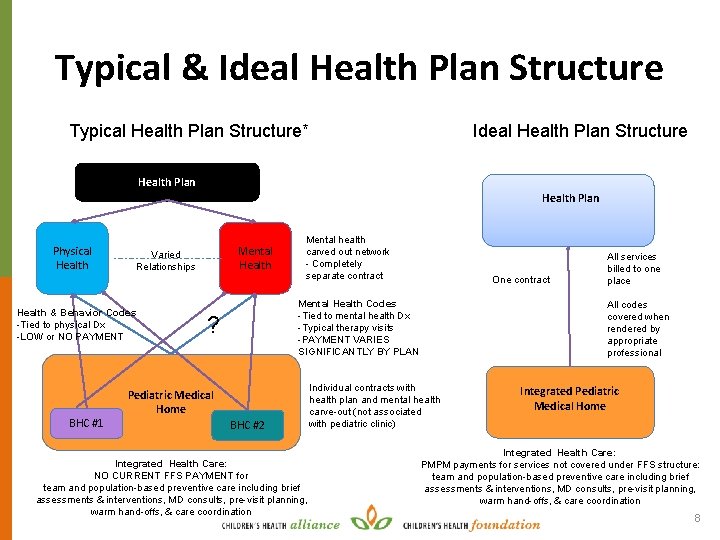
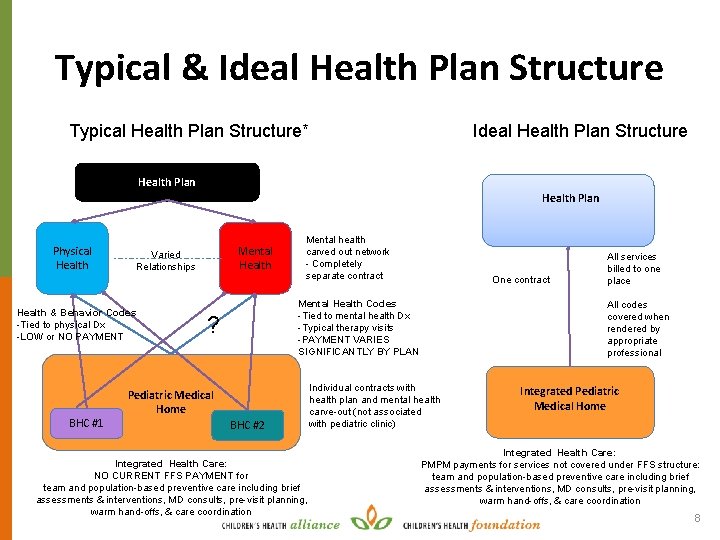
Typical & Ideal Health Plan Structure Typical Health Plan Structure* Health Plan Physical Health Varied Relationships Health & Behavior Codes -Tied to physical Dx -LOW or NO PAYMENT BHC #1 Mental Health Mental health carved out network - Completely separate contract One contract Mental Health Codes -Tied to mental health Dx -Typical therapy visits -PAYMENT VARIES SIGNIFICANTLY BY PLAN ? Pediatric Medical Home BHC #2 Integrated Health Care: NO CURRENT FFS PAYMENT for team and population-based preventive care including brief assessments & interventions, MD consults, pre-visit planning, warm hand-offs, & care coordination All services billed to one place All codes covered when rendered by appropriate professional Individual contracts with health plan and mental health carve-out (not associated with pediatric clinic) Integrated Pediatric Medical Home Integrated Health Care: PMPM payments for services not covered under FFS structure: team and population-based preventive care including brief assessments & interventions, MD consults, pre-visit planning, warm hand-offs, & care coordination 8
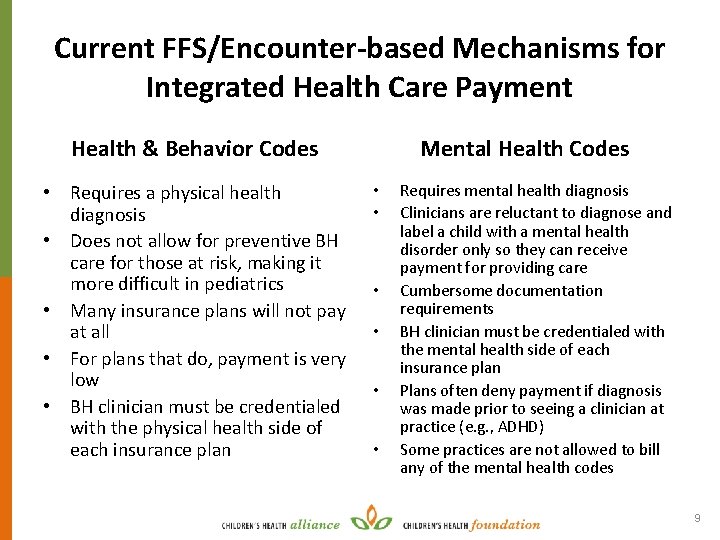
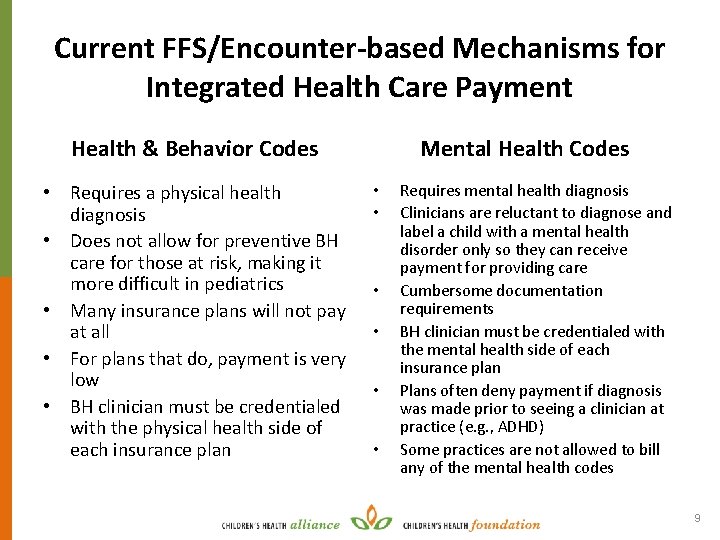
Current FFS/Encounter-based Mechanisms for Integrated Health Care Payment Health & Behavior Codes • Requires a physical health diagnosis • Does not allow for preventive BH care for those at risk, making it more difficult in pediatrics • Many insurance plans will not pay at all • For plans that do, payment is very low • BH clinician must be credentialed with the physical health side of each insurance plan Mental Health Codes • • • Requires mental health diagnosis Clinicians are reluctant to diagnose and label a child with a mental health disorder only so they can receive payment for providing care Cumbersome documentation requirements BH clinician must be credentialed with the mental health side of each insurance plan Plans often deny payment if diagnosis was made prior to seeing a clinician at practice (e. g. , ADHD) Some practices are not allowed to bill any of the mental health codes 9
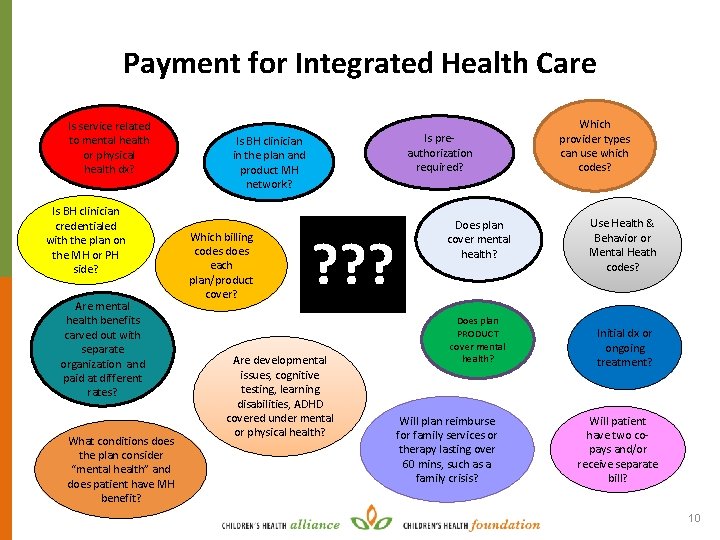
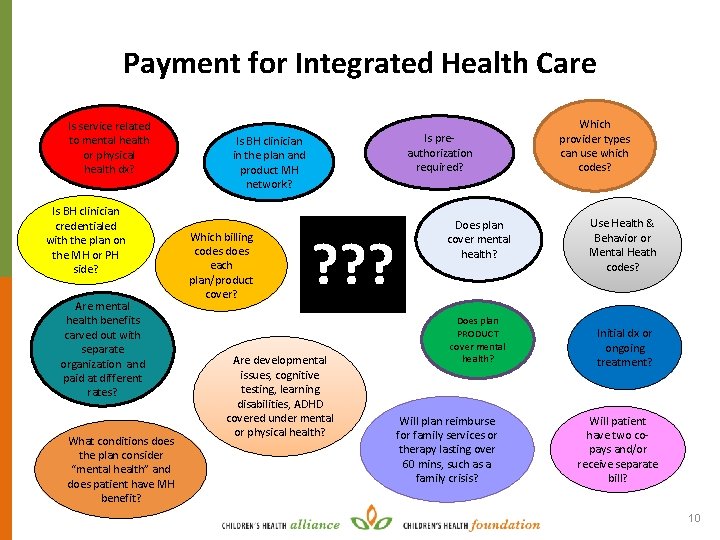
Payment for Integrated Health Care Is service related to mental health or physical health dx? Is BH clinician credentialed with the plan on the MH or PH side? Are mental health benefits carved out with separate organization and paid at different rates? What conditions does the plan consider “mental health” and does patient have MH benefit? Is preauthorization required? Is BH clinician in the plan and product MH network? Which billing codes does each plan/product cover? ? ? ? Are developmental issues, cognitive testing, learning disabilities, ADHD covered under mental or physical health? Does plan cover mental health? Does plan PRODUCT cover mental health? Will plan reimburse for family services or therapy lasting over 60 mins, such as a family crisis? Which provider types can use which codes? Use Health & Behavior or Mental Heath codes? Initial dx or ongoing treatment? Will patient have two copays and/or receive separate bill? 10
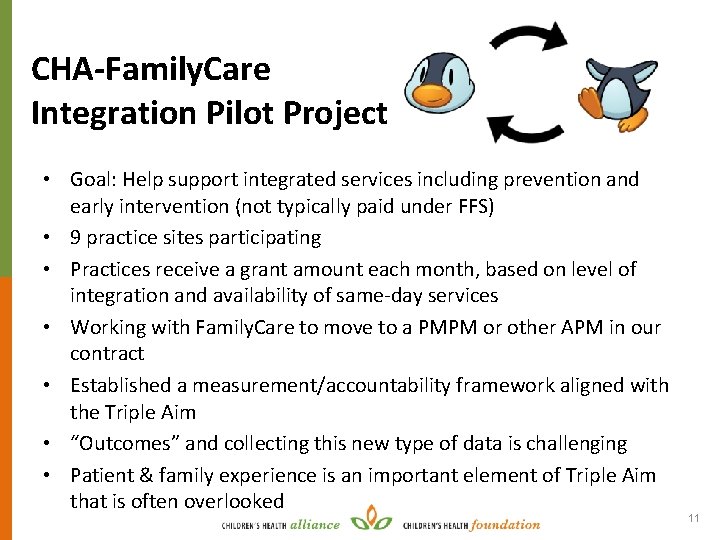
CHA-Family. Care Integration Pilot Project • Goal: Help support integrated services including prevention and early intervention (not typically paid under FFS) • 9 practice sites participating • Practices receive a grant amount each month, based on level of integration and availability of same-day services • Working with Family. Care to move to a PMPM or other APM in our contract • Established a measurement/accountability framework aligned with the Triple Aim • “Outcomes” and collecting this new type of data is challenging • Patient & family experience is an important element of Triple Aim that is often overlooked 11
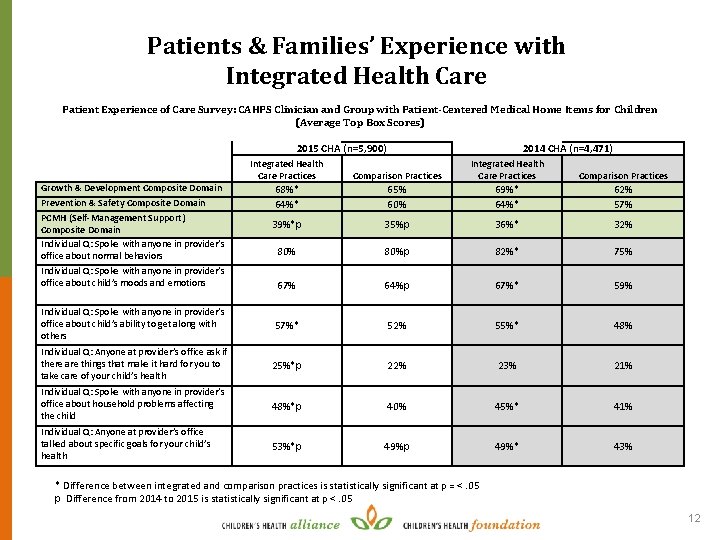
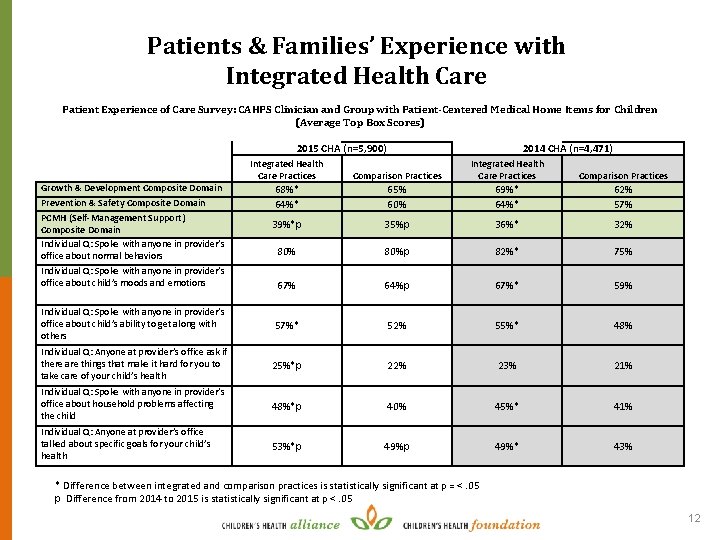
Patients & Families’ Experience with Integrated Health Care Patient Experience of Care Survey: CAHPS Clinician and Group with Patient-Centered Medical Home Items for Children (Average Top Box Scores) 2015 CHA (n=5, 900) 2014 CHA (n=4, 471) Integrated Health Care Practices Comparison Practices 68%* 64%* 65% 60% 69%* 64%* 62% 57% 39%*p 35%p 36%* 32% 80%p 82%* 75% 67% 64%p 67%* 59% Individual Q: Spoke with anyone in provider’s office about child’s ability to get along with others 57%* 52% 55%* 48% Individual Q: Anyone at provider’s office ask if there are things that make it hard for you to take care of your child’s health 25%*p 22% 23% 21% Individual Q: Spoke with anyone in provider’s office about household problems affecting the child 48%*p 40% 45%* 41% Individual Q: Anyone at provider’s office talked about specific goals for your child’s health 53%*p 49%* 43% Growth & Development Composite Domain Prevention & Safety Composite Domain PCMH (Self-Management Support) Composite Domain Individual Q: Spoke with anyone in provider’s office about normal behaviors Individual Q: Spoke with anyone in provider’s office about child’s moods and emotions * Difference between integrated and comparison practices is statistically significant at p = <. 05 p Difference from 2014 to 2015 is statistically significant at p <. 05 12
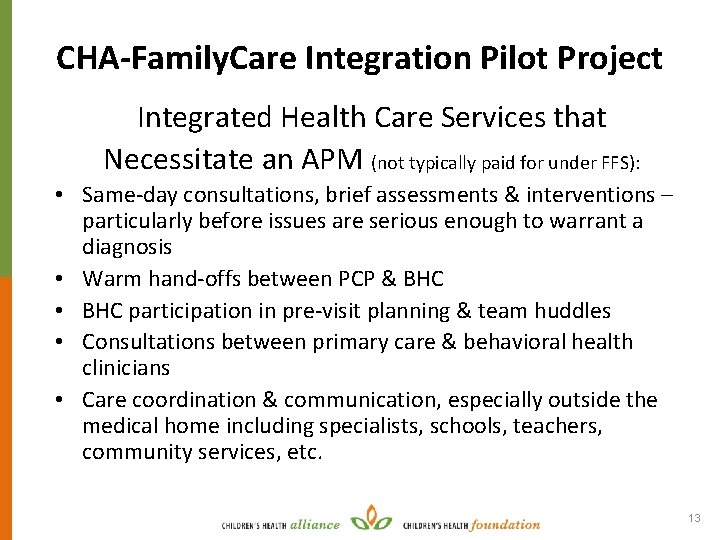
CHA-Family. Care Integration Pilot Project Integrated Health Care Services that Necessitate an APM (not typically paid for under FFS): • Same-day consultations, brief assessments & interventions – particularly before issues are serious enough to warrant a diagnosis • Warm hand-offs between PCP & BHC • BHC participation in pre-visit planning & team huddles • Consultations between primary care & behavioral health clinicians • Care coordination & communication, especially outside the medical home including specialists, schools, teachers, community services, etc. 13
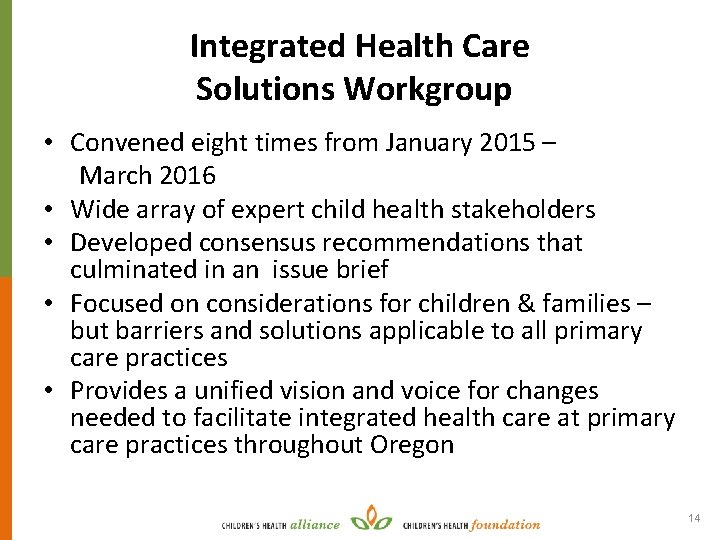
Integrated Health Care Solutions Workgroup • Convened eight times from January 2015 – March 2016 • Wide array of expert child health stakeholders • Developed consensus recommendations that culminated in an issue brief • Focused on considerations for children & families – but barriers and solutions applicable to all primary care practices • Provides a unified vision and voice for changes needed to facilitate integrated health care at primary care practices throughout Oregon 14

Integrated Health Care Solutions Workgroup Participants Expert Contributors: E. Dawn Creach, MS – Principal Author and Facilitator Deborah Rumsey Ken Carlson, MD (Pediatrician) Amy Stoeber, Ph. D (Psychologist) Mike Franz, MD (Psychiatrist) Evan Saulino, MD, Ph. D (Family Physician) Dan Reece, LCSW Colleen Reuland, MS Joe Hromco, Ph. D (Psychologist) R. J. Gillespie, MD (Pediatrician) Kerry Gonzales Sherri Alderman, MD (Developmental-Behavioral Pediatrician) Julie Magers (Parent Advocate) 15
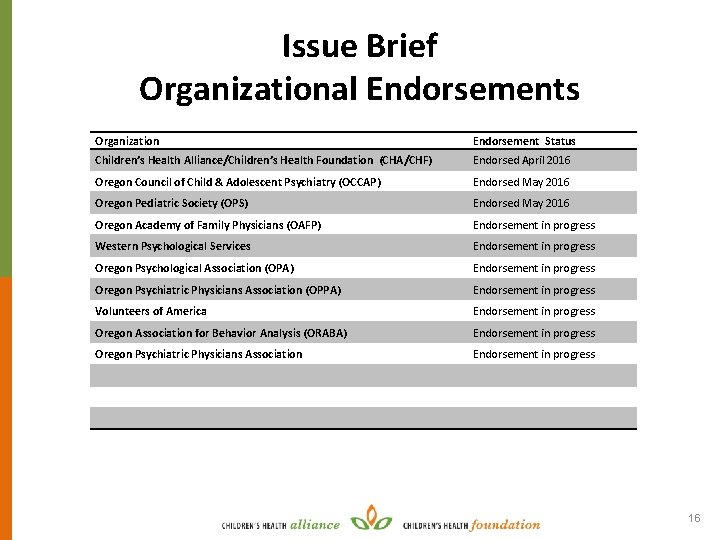
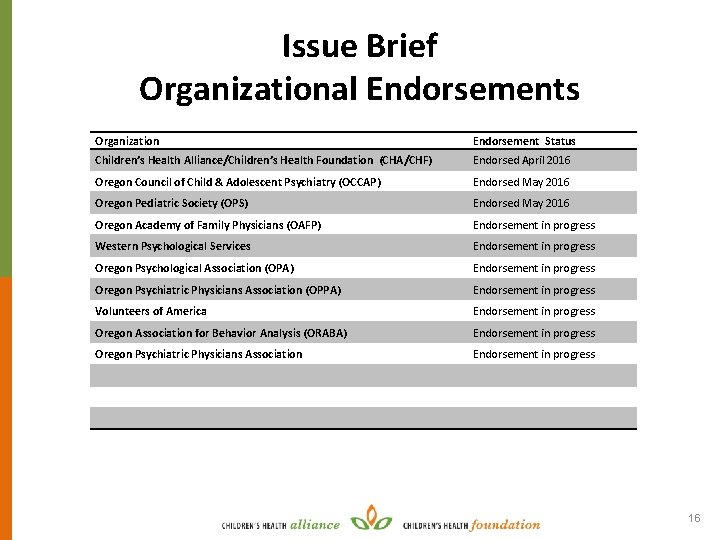
Issue Brief Organizational Endorsements Organization Endorsement Status Children’s Health Alliance/Children’s Health Foundation (CHA/CHF) Endorsed April 2016 Oregon Council of Child & Adolescent Psychiatry (OCCAP) Endorsed May 2016 Oregon Pediatric Society (OPS) Endorsed May 2016 Oregon Academy of Family Physicians (OAFP) Endorsement in progress Western Psychological Services Endorsement in progress Oregon Psychological Association (OPA) Endorsement in progress Oregon Psychiatric Physicians Association (OPPA) Endorsement in progress Volunteers of America Endorsement in progress Oregon Association for Behavior Analysis (ORABA) Endorsement in progress Oregon Psychiatric Physicians Association Endorsement in progress 16
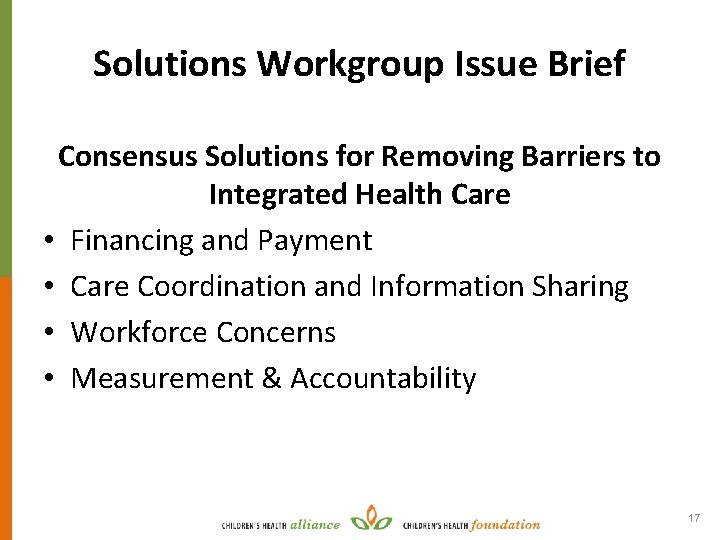
Solutions Workgroup Issue Brief Consensus Solutions for Removing Barriers to Integrated Health Care • Financing and Payment • Care Coordination and Information Sharing • Workforce Concerns • Measurement & Accountability 17
Thank You! www. ch-alliance. org Follow Us on Twitter! @chachfpeds E. Dawn Creach, MS dcreach@ch-alliance. org 18
 Big families vs small families
Big families vs small families Integrated primary health care model
Integrated primary health care model Effective support for children and families in essex
Effective support for children and families in essex Georgia department of children and families
Georgia department of children and families Act for children with autism and emotional challenges
Act for children with autism and emotional challenges Primary secondary and tertiary care
Primary secondary and tertiary care Care value base health and social care
Care value base health and social care Health and social care component 3 health and wellbeing
Health and social care component 3 health and wellbeing Y connected generator
Y connected generator Phase to phase voltage
Phase to phase voltage Drift current and diffusion current
Drift current and diffusion current Ac theory 3 lesson 4
Ac theory 3 lesson 4 Drift vs diffusion current
Drift vs diffusion current What is diffusion current and drift current
What is diffusion current and drift current In this figure
In this figure Balanced delta delta connection
Balanced delta delta connection Infineon
Infineon Diffusion current density
Diffusion current density In alternators the welding current is produced on the ____.
In alternators the welding current is produced on the ____.