ANC x 6 x 5 TT x 2











- Slides: 41



ANC ����� x 6 ����� x 5 TT x 2 Serology : all negative TWG 10. 6 kg

MH : Interval 28 -30 days Duration 5 days Regular FH : �������� Social History : ������ ���


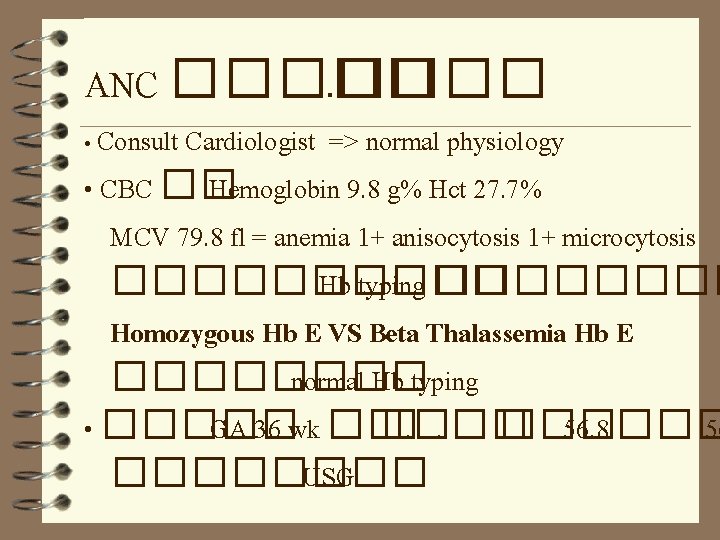
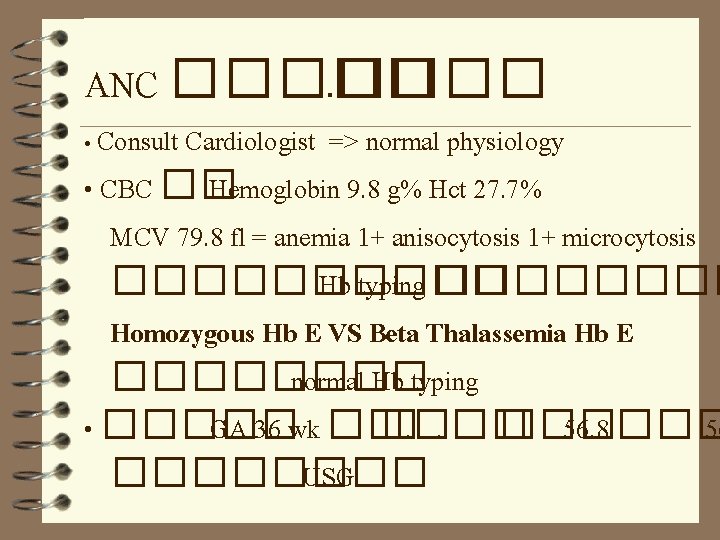
ANC ����� • Consult Cardiologist => normal physiology • CBC �� Hemoglobin 9. 8 g% Hct 27. 7% MCV 79. 8 fl = anemia 1+ anisocytosis 1+ microcytosis ����� Hb typing ���� Homozygous Hb E VS Beta Thalassemia Hb E ���� normal Hb typing • ����� GA 36 wk �� �. �. �� ��� 56. 8 ��� 56 ���� USG
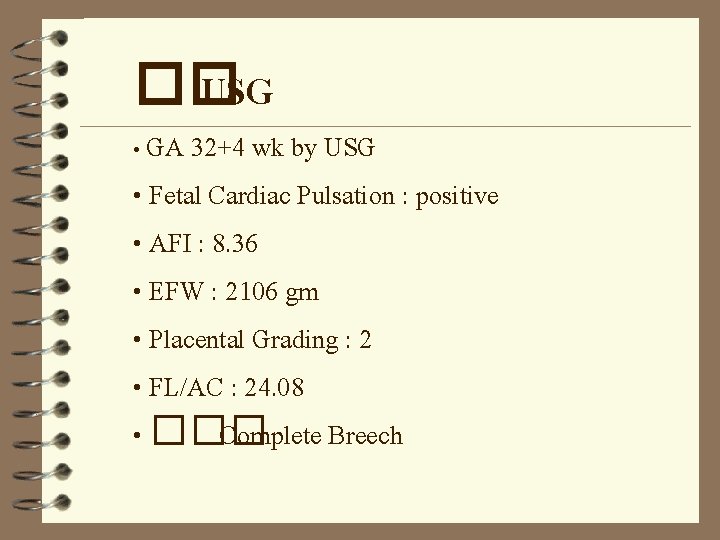
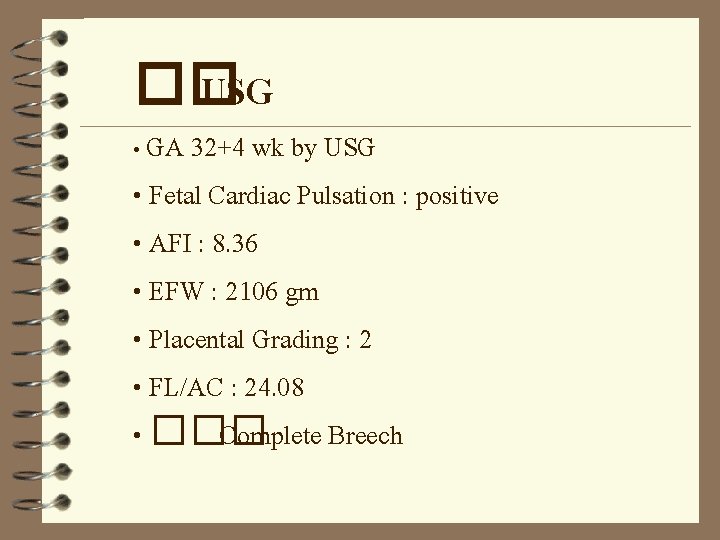
�� USG • GA 32+4 wk by USG • Fetal Cardiac Pulsation : positive • AFI : 8. 36 • EFW : 2106 gm • Placental Grading : 2 • FL/AC : 24. 08 • ��� Complete Breech

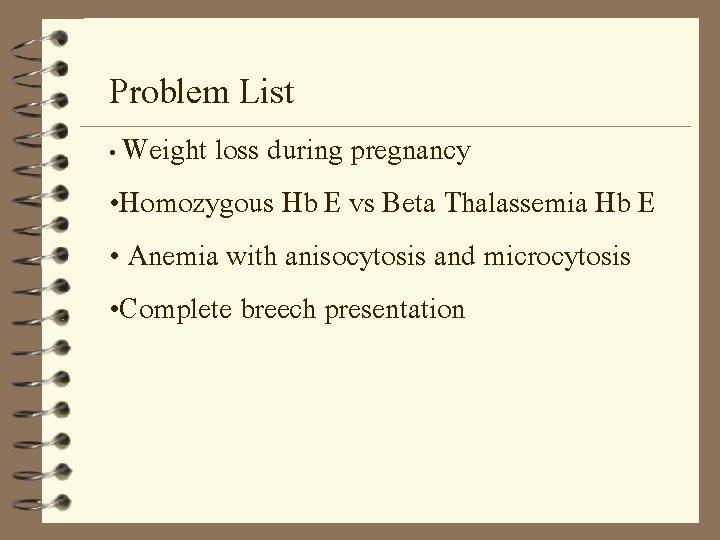
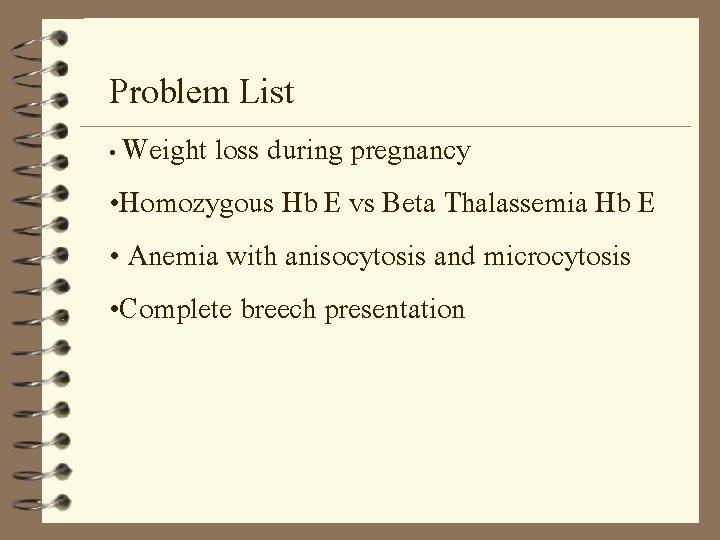
Problem List • Weight loss during pregnancy • Homozygous Hb E vs Beta Thalassemia Hb E • Anemia with anisocytosis and microcytosis • Complete breech presentation
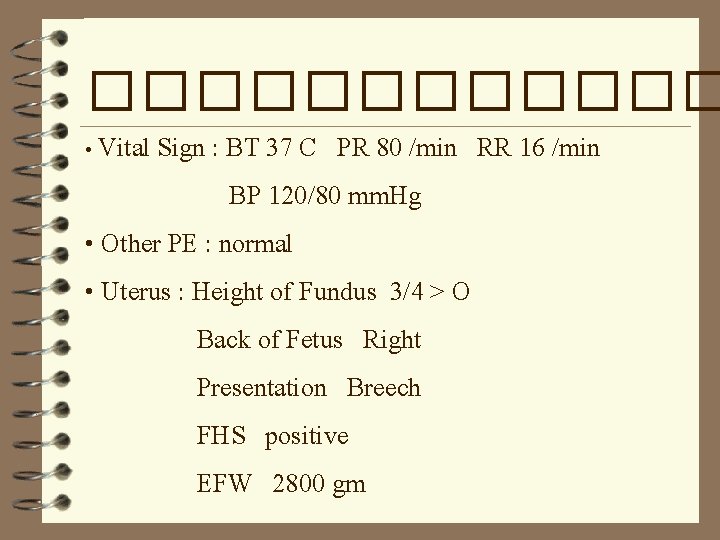
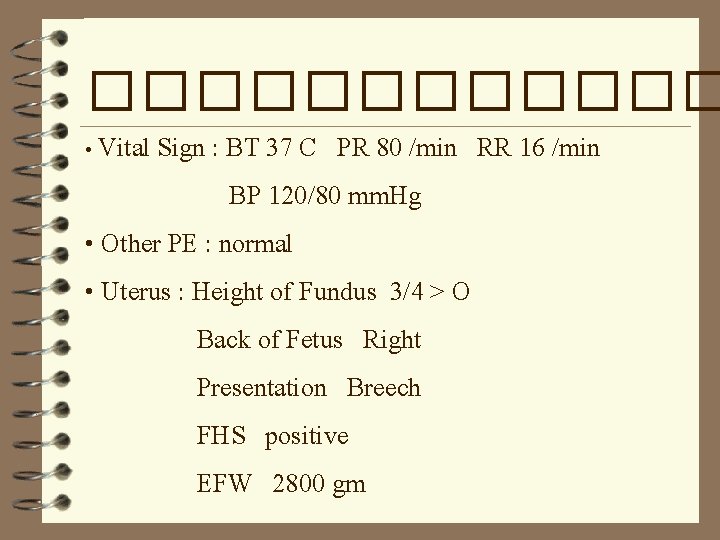
������ • Vital Sign : BT 37 C PR 80 /min RR 16 /min BP 120/80 mm. Hg • Other PE : normal • Uterus : Height of Fundus 3/4 > O Back of Fetus Right Presentation Breech FHS positive EFW 2800 gm
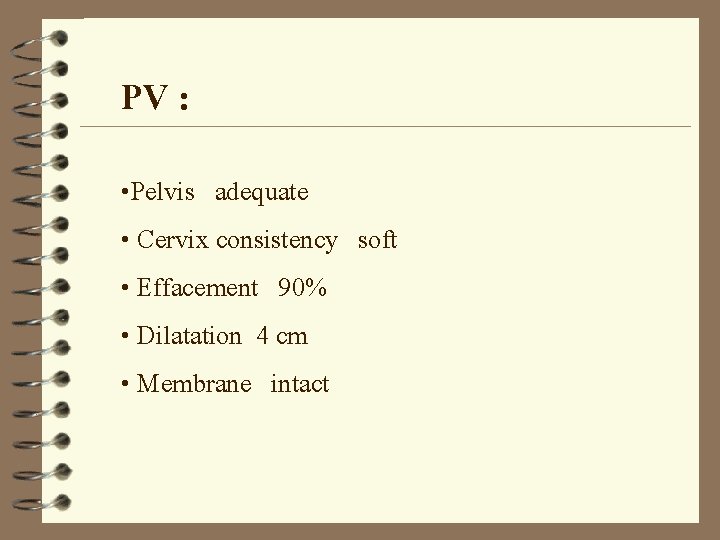
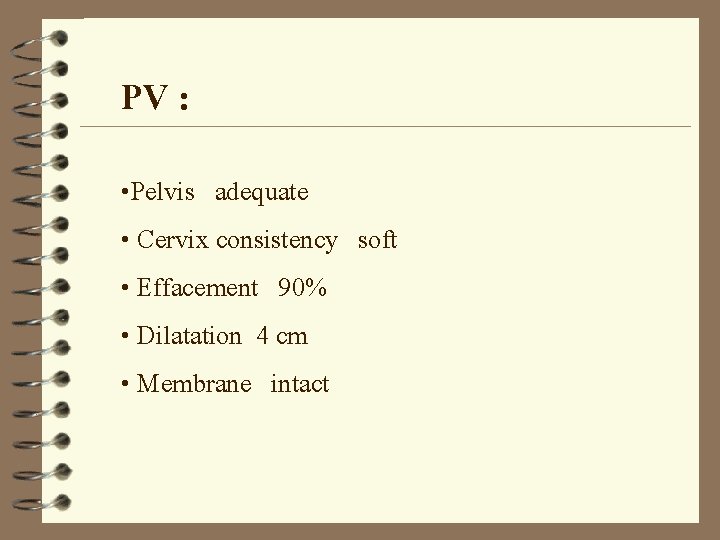
PV : • Pelvis adequate • Cervix consistency soft • Effacement 90% • Dilatation 4 cm • Membrane intact
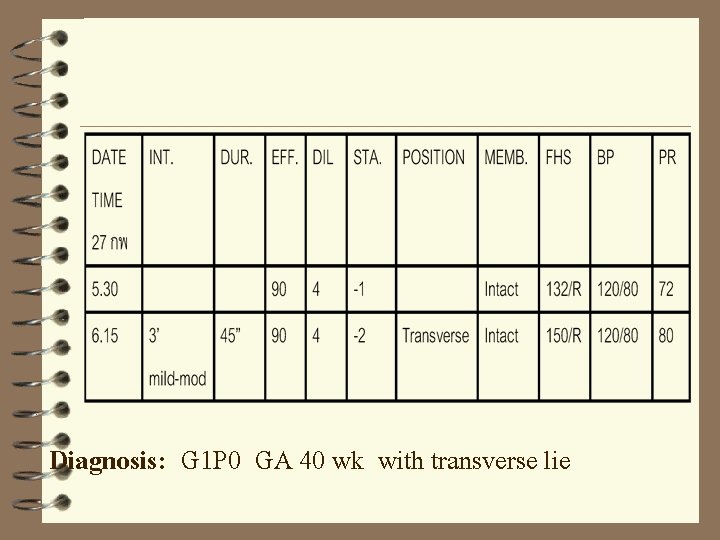
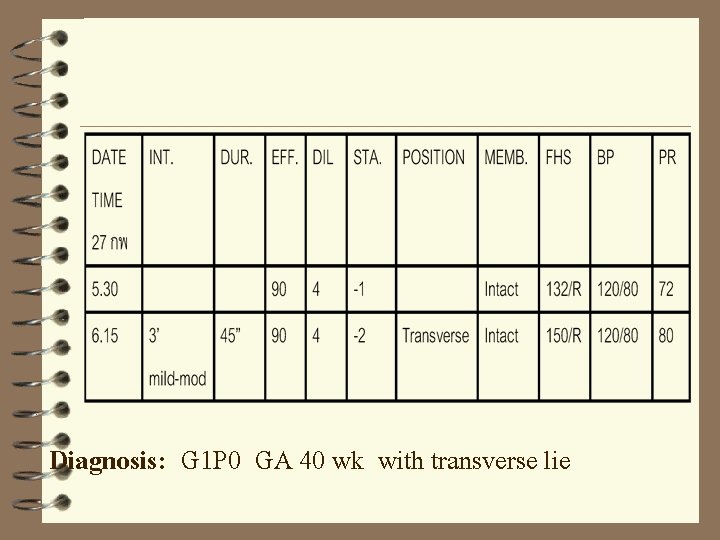
Diagnosis: G 1 P 0 GA 40 wk with transverse lie
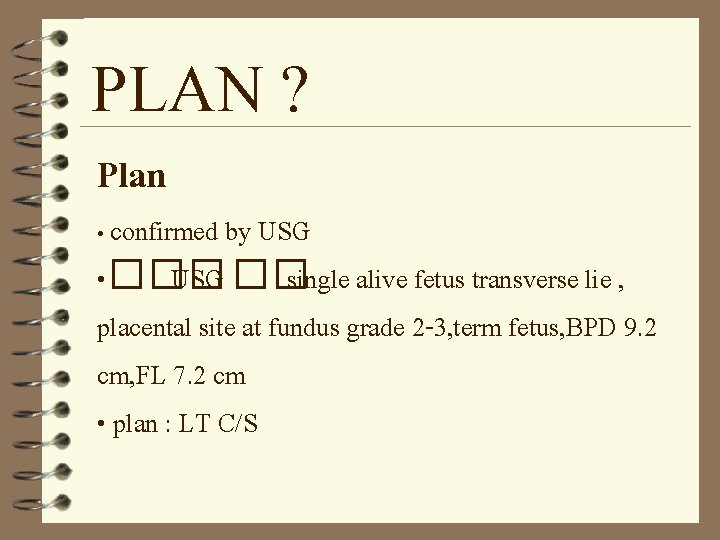
PLAN ? Plan • confirmed by USG • ��� USG �� single alive fetus transverse lie , placental site at fundus grade 2 -3, term fetus, BPD 9. 2 cm, FL 7. 2 cm • plan : LT C/S

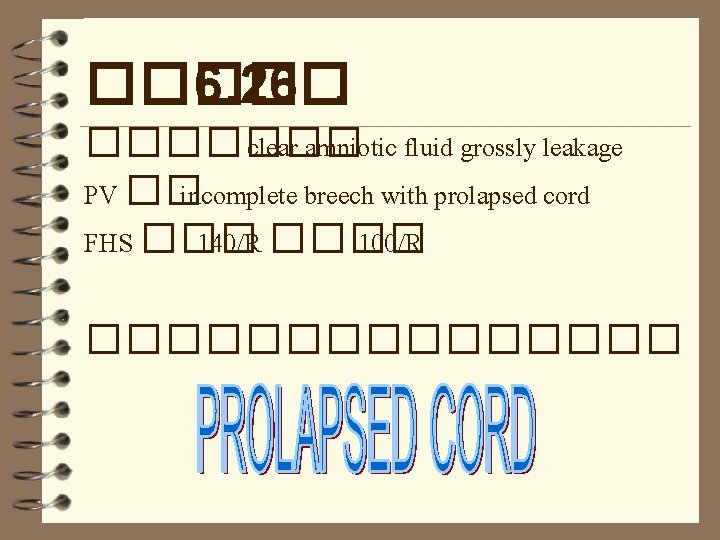
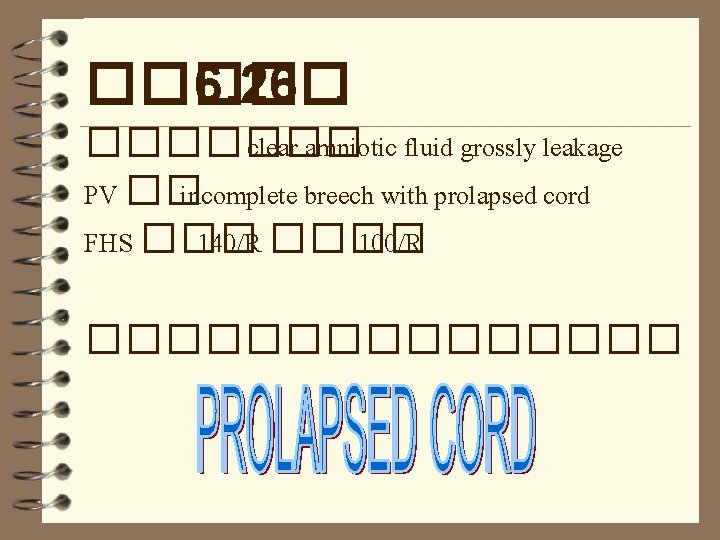
���� 6. 26�. ������� clear amniotic fluid grossly leakage PV �� incomplete breech with prolapsed cord FHS ��� 140/R ���� 100/R ��������
Definition • the cord lies beside the presenting part(occult cord)or below it • the membranes are ruptured
diagnosis • Palpation of the cord or cord pulsation on vaginal examination • visualization of the cord outside the vulva • fetal bradycardia or variable deceleration When the membrane rupture and any of the foregoing predisposing factor are present: PV should be performed to exclude cord prolapse
Fetal Bradycardia Definition – FHR < 120 beats / min for 2 min or longer 4 Prolong bradycardia – sudden drop from normal FHR to value below 120 esp. < 80/min Cause - decrease in maternal oxygen tension eg. apnea of seizure - decrease in umbilical blood flow eg. excessive uterine contraction , maternal hypotension , cord compression, abruptio placentae -fetal hemorrhage eg. vasa previa
Pathophysiology of prolapsed cord 1. Umbilical cord prolapses 1. 2. Follows rupture of membrane 2. 3. Occurs when presenting part is ill fitting
4. Fetal blood supply obstructed when cord out of uterus • Drops in temperature • Vasospasm of umbilical vessels • Compression between pelvic brim and presenting part
Risk factors: Any condition which interfere presenting part engagement in the pelvis : • Malpresentation • Transverse or oblique lie • Breech esp. footling • CPD • Unengaged vertex • polyhydramnios

• Multiple pregnancy • Grand multiparity – anterior uterine obliquity • Prematurity • Pracenta previa • Uterine fibroids • Amniotomy with unengage presenting part • Version of fetus
How to manage? �������� ��� IV fluid �������� notified anesthetist and pediatrist ������ C/S emergency

1. Remain calm , call for help 2. Counseling 3. Turn off syntocinon therapy If cord prolapse is confirmed 4. �������� �� ���
4. 3��� NSS 500 -750 ml ���� ��� clamp ������� full bladde 5. Intrauterine resuscitation • ��� NSS 1000 ml IV • facial O 2 100% via face mask 8 L / min • ������� FHS ����
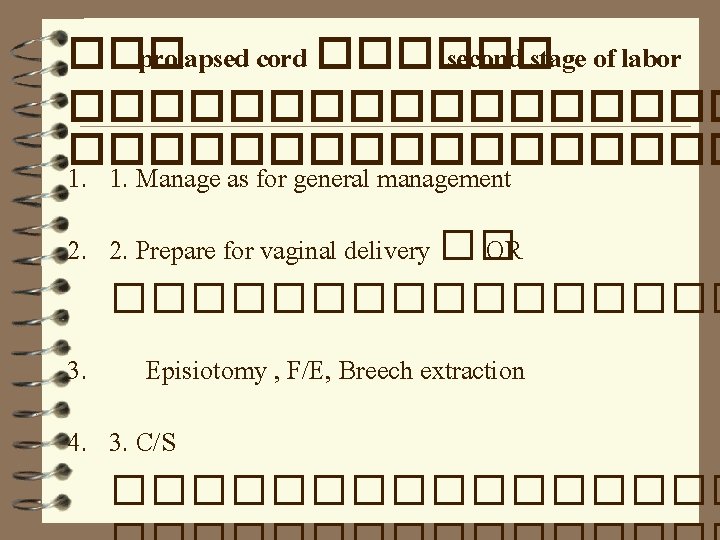
��� prolapsed cord ������ second stage of labor ����������������� 1. 1. Manage as for general management 2. 2. Prepare for vaginal delivery �� OR �������� 3. Episiotomy , F/E, Breech extraction 4. 3. C/S ��������
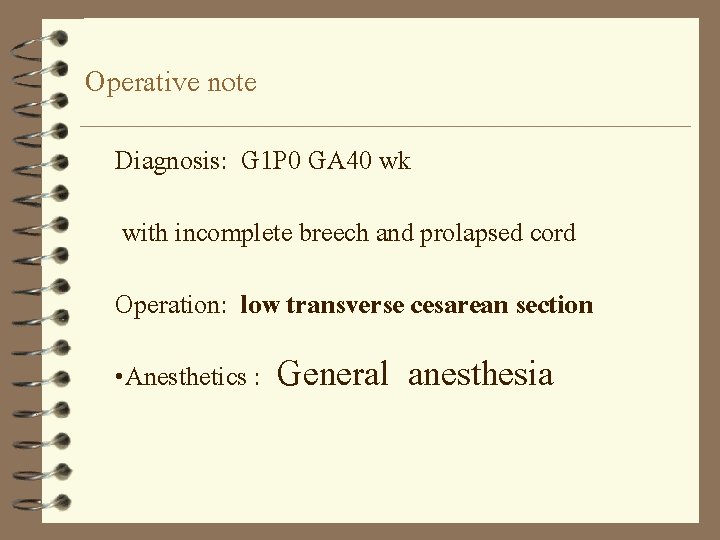
Operative note Diagnosis: G 1 P 0 GA 40 wk with incomplete breech and prolapsed cord Operation: low transverse cesarean section • Anesthetics : General anesthesia
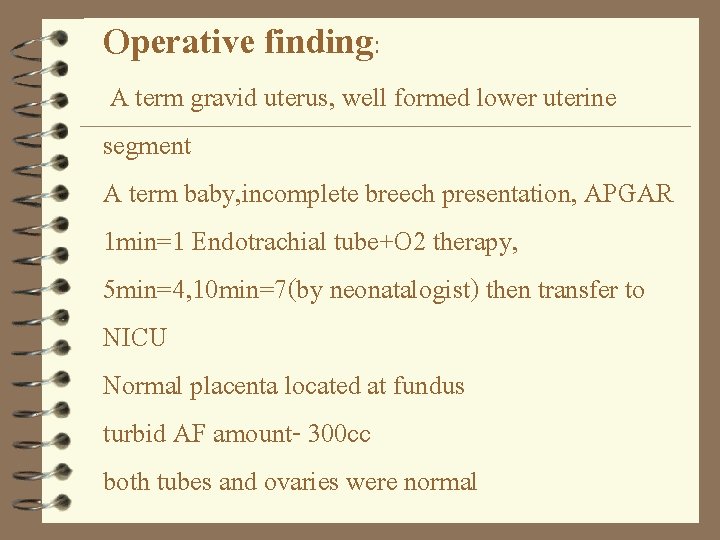
Operative finding: A term gravid uterus, well formed lower uterine segment A term baby, incomplete breech presentation, APGAR 1 min=1 Endotrachial tube+O 2 therapy, 5 min=4, 10 min=7(by neonatalogist) then transfer to NICU Normal placenta located at fundus turbid AF amount- 300 cc both tubes and ovaries were normal
������ 6. 30� ������� 6. 37�. 17)�������� prolapsed cord 11��� Newborn : male, alive, weight 2975 gm. APGAR score(1 min) 1, (5 min) 4 stimulate breathing, resuscitation 5 min ������ tone , ����� HR ��� tube, suction, ��� O 2 pump ������ , HR>100, tone
Placenta: normal placenta : weight 500 gm : cord length 40 cm.
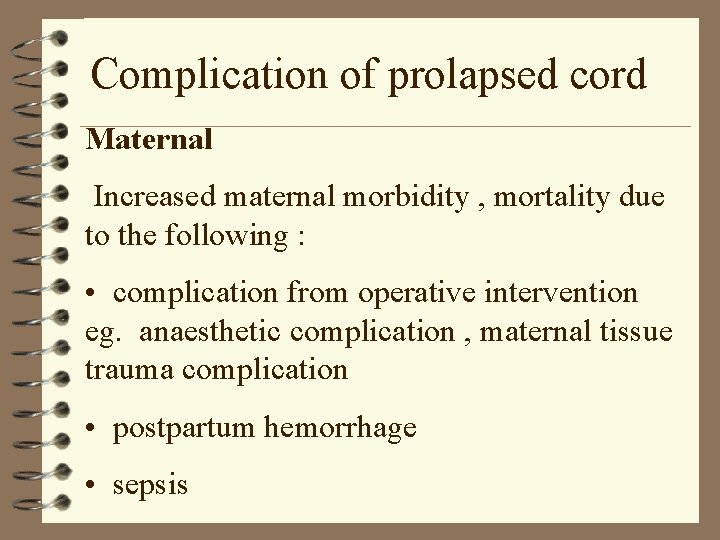
Complication of prolapsed cord Maternal Increased maternal morbidity , mortality due to the following : • complication from operative intervention eg. anaesthetic complication , maternal tissue trauma complication • postpartum hemorrhage • sepsis
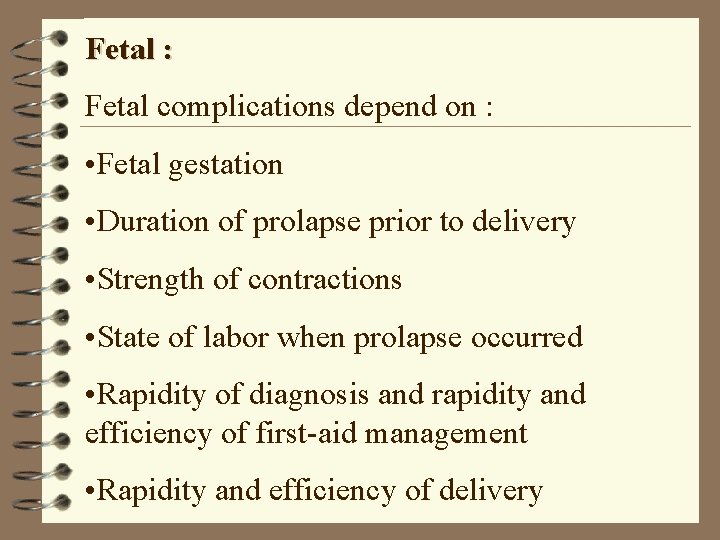
Fetal : Fetal complications depend on : • Fetal gestation • Duration of prolapse prior to delivery • Strength of contractions • State of labor when prolapse occurred • Rapidity of diagnosis and rapidity and efficiency of first-aid management • Rapidity and efficiency of delivery
