Aminotransferases AMINOTRANSFERASES Definition Interconversion of amino acids to


- Slides: 15
Aminotransferases
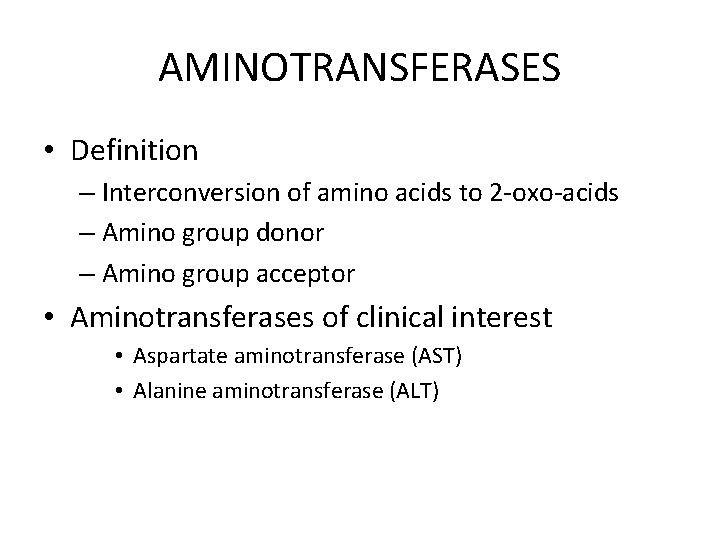
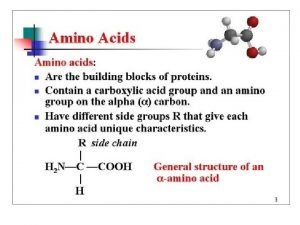
AMINOTRANSFERASES • Definition – Interconversion of amino acids to 2 -oxo-acids – Amino group donor – Amino group acceptor • Aminotransferases of clinical interest • Aspartate aminotransferase (AST) • Alanine aminotransferase (ALT)

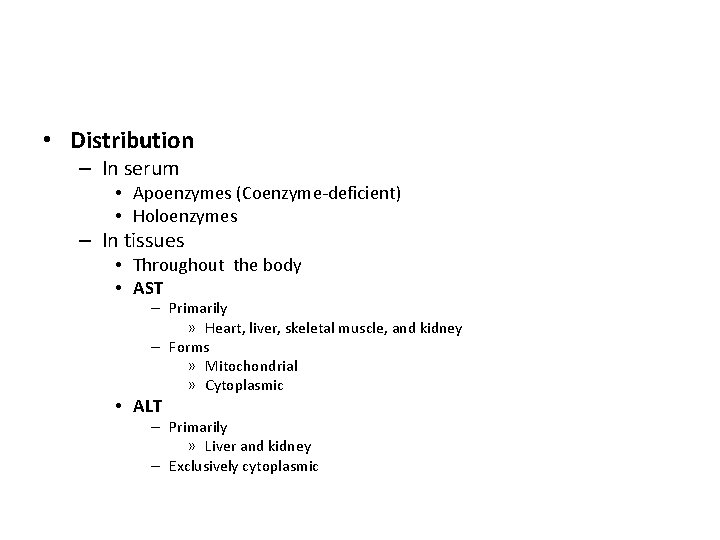
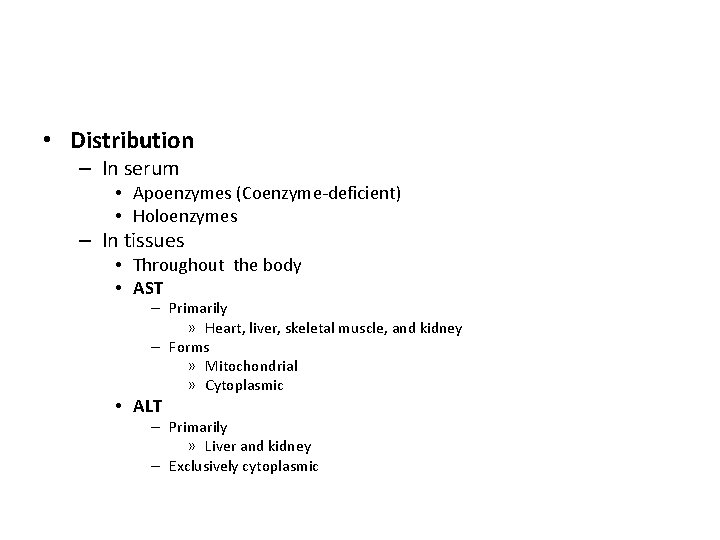
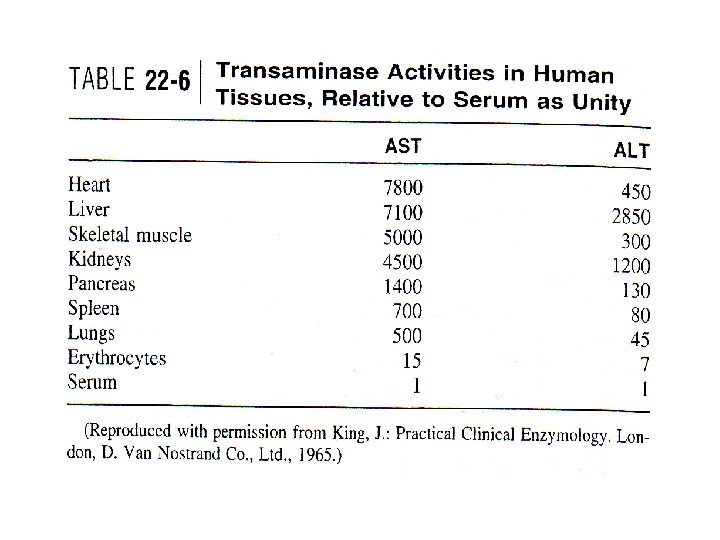
• Distribution – In serum • Apoenzymes (Coenzyme-deficient) • Holoenzymes – In tissues • Throughout the body • AST – Primarily » Heart, liver, skeletal muscle, and kidney – Forms » Mitochondrial » Cytoplasmic • ALT – Primarily » Liver and kidney – Exclusively cytoplasmic
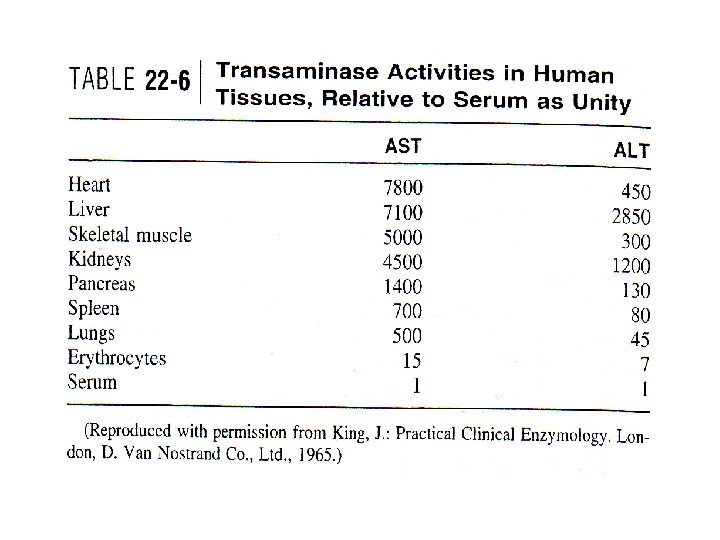
Tissue distribution
• ALT is the more liver-specific enzyme • Elevations of ALT activity persist longer than do those of AST activity
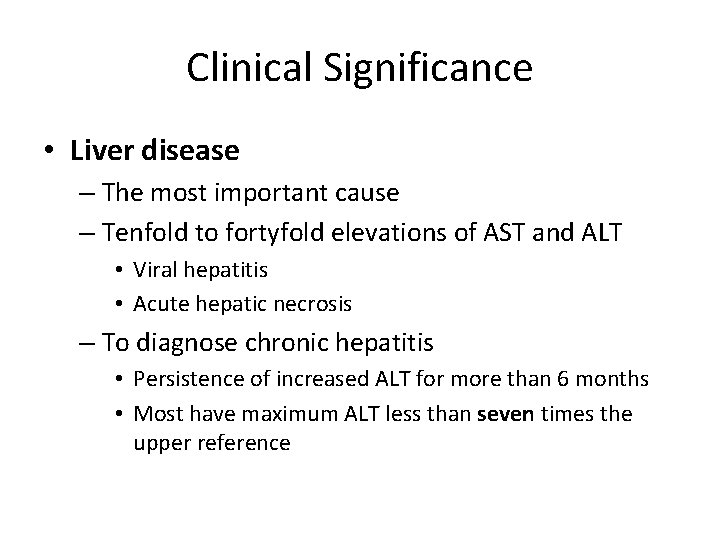
Clinical Significance • Liver disease – The most important cause – Tenfold to fortyfold elevations of AST and ALT • Viral hepatitis • Acute hepatic necrosis – To diagnose chronic hepatitis • Persistence of increased ALT for more than 6 months • Most have maximum ALT less than seven times the upper reference
Clinical Significance • Toxic hepatitis • Acetaminophen-induced hepatic injury • Transaminase 85 times the upper reference limit in 90% of case – AST and ALT » Peak early and fall rapidly
• Carcinoma of the liver – Twofold to fivefold elevations – AST usually being higher than ALT • Various medications – Slight or moderate elevations of both AST and ALT • Less common causes – – – Hemochromatosis Wilson's disease Autoimmune hepatitis Primary biliary cirrhosis α 1 -antitrypsin deficiency
Clinical Significance • Increased AST activity – AMI – Progressive muscular dystrophy • Up to eight times normal • With serum CK • Mitochondrial AST (m-AST) – Extensive liver cell degeneration and necrosis – Ratio between m-AST and total AST • Typical of alcoholic hepatitis • Macro-AST – No known clinical relevance
Methods for the Measurement of Transaminase Activity • The assay system – Two amino acids and two oxo-acids • Formation or consumption of the oxo-acids is measured • Various photometric substrates and dyes coupled to the transaminase reactions – Continuous-monitoring methods • • • Transaminase reactions Oxo-acids formed Dehydrogenase reactions Reduction to hydroxy acids Change in NADH

• Supplementation with P-5' –p • NADH, MD or LD, must be present in sufficient quantity • A preliminary incubation – Endogenous oxo-acids • AST activity in serum – Up to 48 hours at 4°C – Frozen if they are to be kept longer • ALT activity should be assayed on the day of sample collection
• ALT stability – at -70°C. • Hemolyzed specimens • Reference Intervals – AST (upper reference limits for adults) • 31 U/L for women • 35 U/L for men – ALT • 34 U/L • 45 U/L
• m-AST – 5% to I 0% of the activity of total AST in serum – Reference limit • 3. 0 U/L
 Interconversion of states of matter
Interconversion of states of matter Interconversion of plastids
Interconversion of plastids Translation
Translation Titration curves of all 20 amino acids
Titration curves of all 20 amino acids Titration curve of amino acids
Titration curve of amino acids Deamination of amino acids
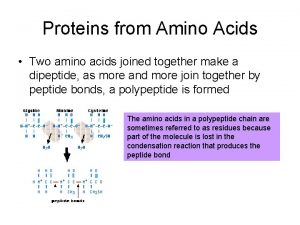
Deamination of amino acids Two amino acids joined
Two amino acids joined Transdeamination of amino acids
Transdeamination of amino acids Amino acids groups
Amino acids groups Early man
Early man Carbohydrates gives
Carbohydrates gives Titration plot
Titration plot Gluconeogenesis importance
Gluconeogenesis importance Ketogenic vs glucogenic amino acids
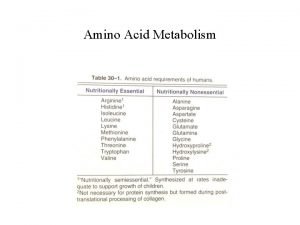
Ketogenic vs glucogenic amino acids Pvt tim hall
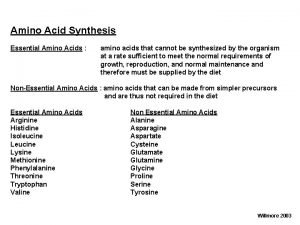
Pvt tim hall Neutral amino acids
Neutral amino acids