Acute PE Management How to Choose your Lytic

- Slides: 24
Acute PE Management: How to Choose your Lytic Strategy Jay Giri, MD MPH Assistant Professor of Medicine Director, Pulmonary Embolism Response Team Associate Director, Penn Cardiovascular Quality, Outcomes & Evaluative Research Center Hospital of the University of Pennsylvania 1
Disclosure w. Nothing to Disclose 2
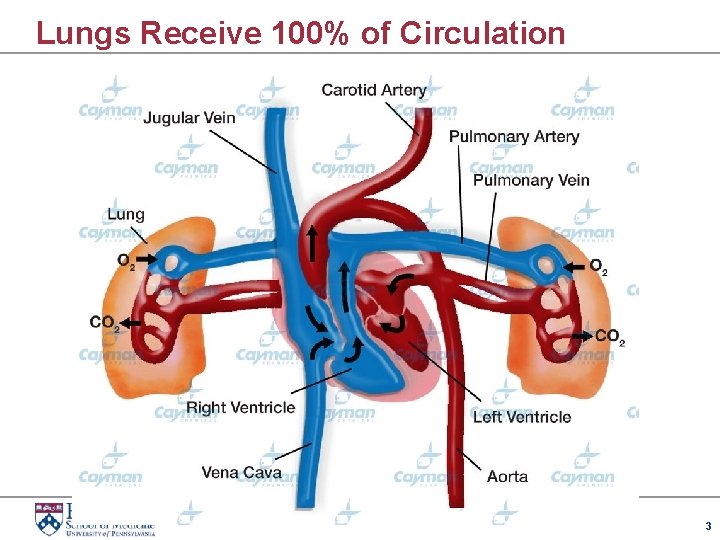
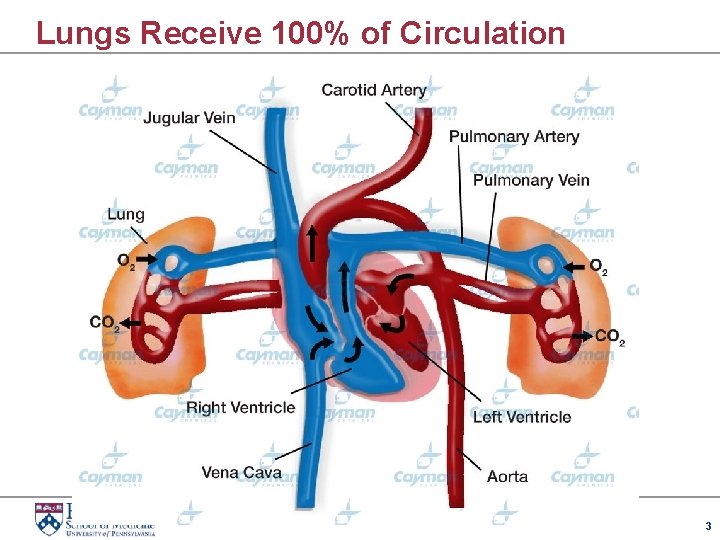
Lungs Receive 100% of Circulation 3
CDT Claims w. Increased Efficacy w. Better Safety 4

Theoretical Advantages for Local Lytic w. Higher local concentration w. Lower overall dose w. Ability to fragment clot if desired w. PA pressure monitoring Blinc, et 1998; 21: 199 -204 al. Thromb Haemost. 1991 May 6; 65(5): 549 -52. Scmitz-Rode CVIR 5
Who Knows? Longer Infusion Reduced Dose 6
Increased Efficacy? 7
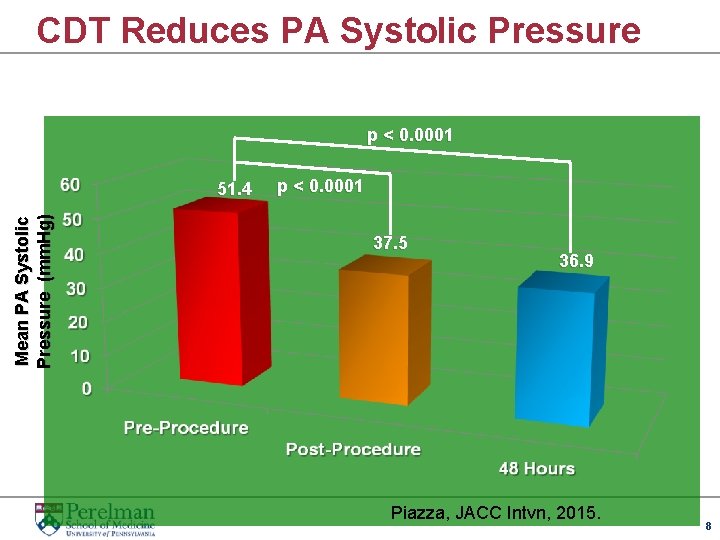
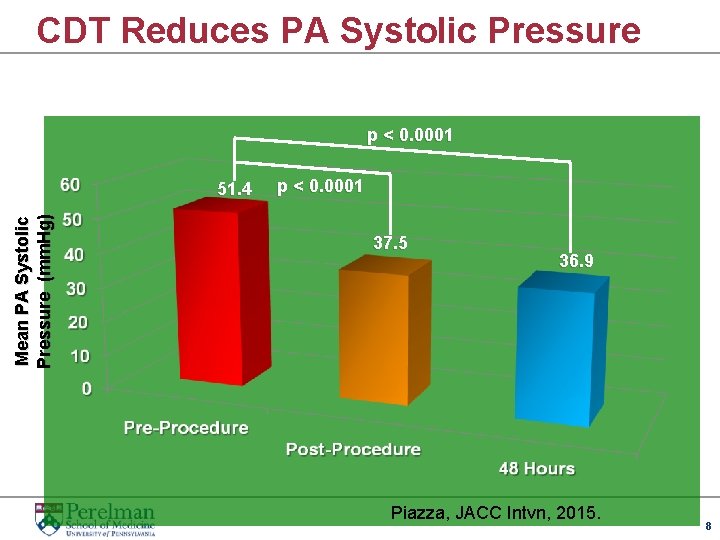
CDT Reduces PA Systolic Pressure p < 0. 0001 Mean PA Systolic Pressure (mm. Hg) 51. 4 p < 0. 0001 37. 5 36. 9 Piazza, JACC Intvn, 2015. 8
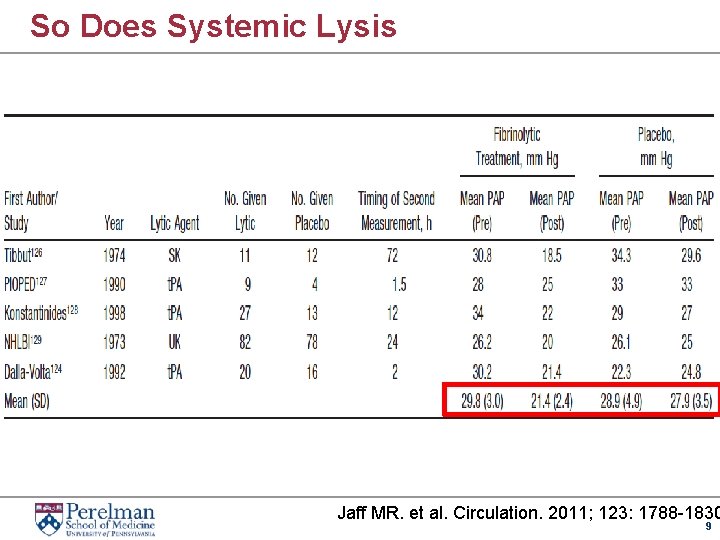
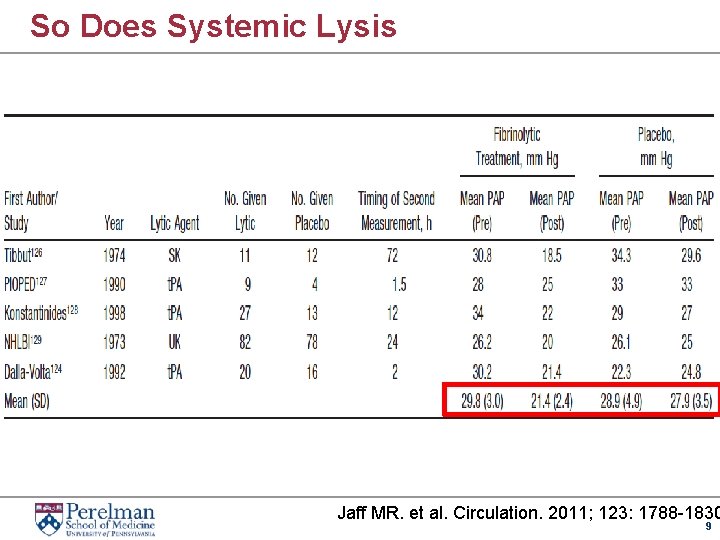
So Does Systemic Lysis Jaff MR. et al. Circulation. 2011; 123: 1788 -1830 9
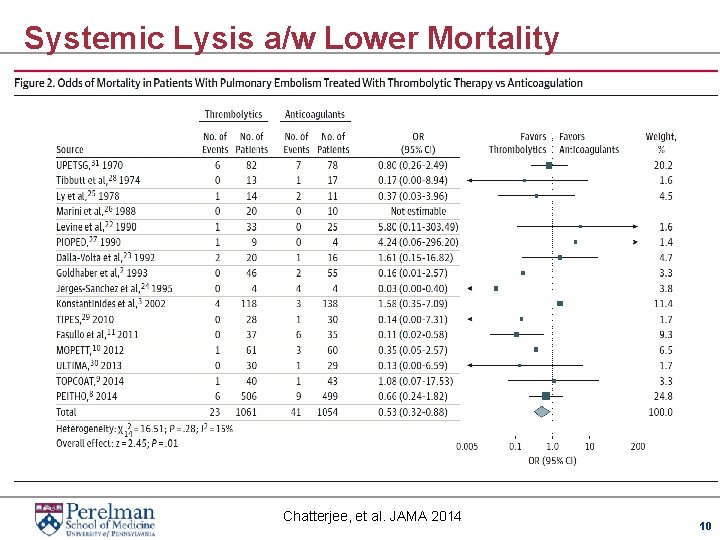
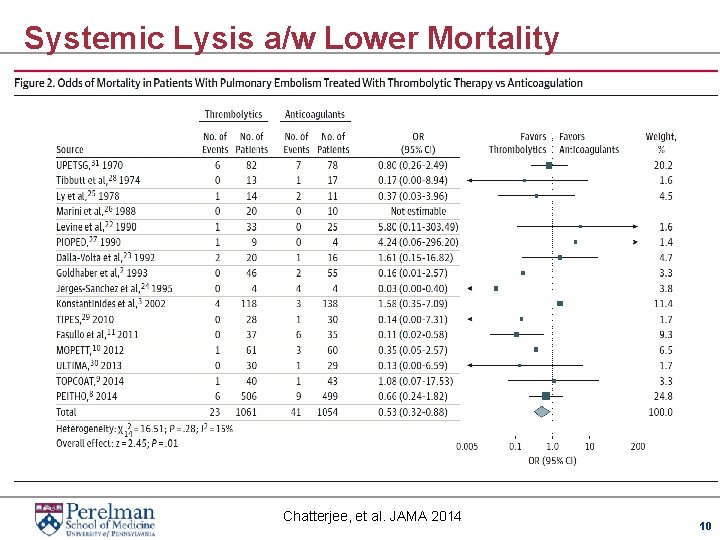
Systemic Lysis a/w Lower Mortality Chatterjee, et al. JAMA 2014 10
Catheter-Directed Lysis No Data 11
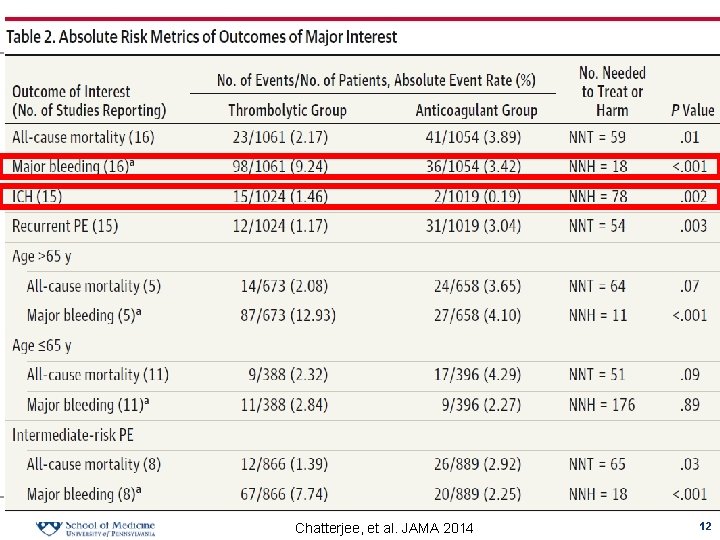
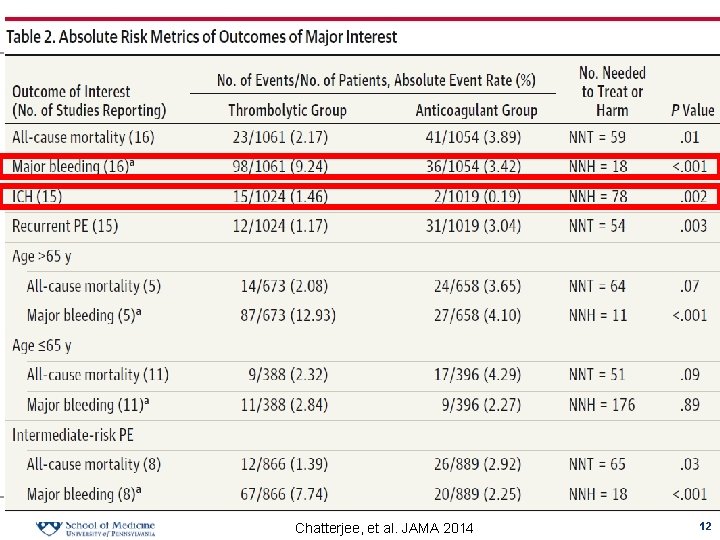
Chatterjee, et al. JAMA 2014 12
Better Safety? w. Decrease Overall Bleeding Complications? w. Decrease ICH rates? 13
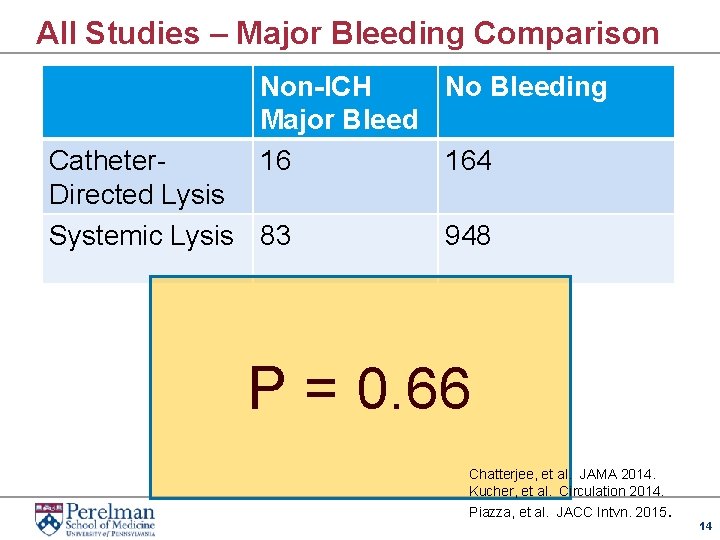
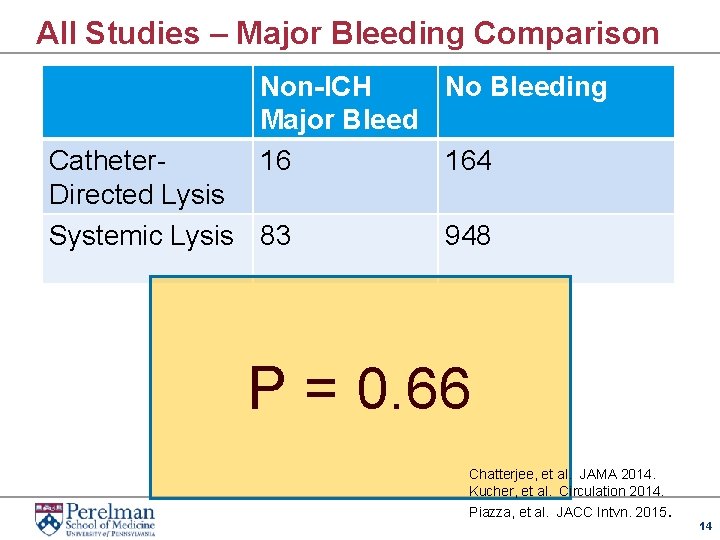
All Studies – Major Bleeding Comparison Non-ICH No Bleeding Major Bleed 16 164 Catheter. Directed Lysis Systemic Lysis 83 948 P = 0. 66 Chatterjee, et al. JAMA 2014. Kucher, et al. Circulation 2014. Piazza, et al. JACC Intvn. 2015. 14
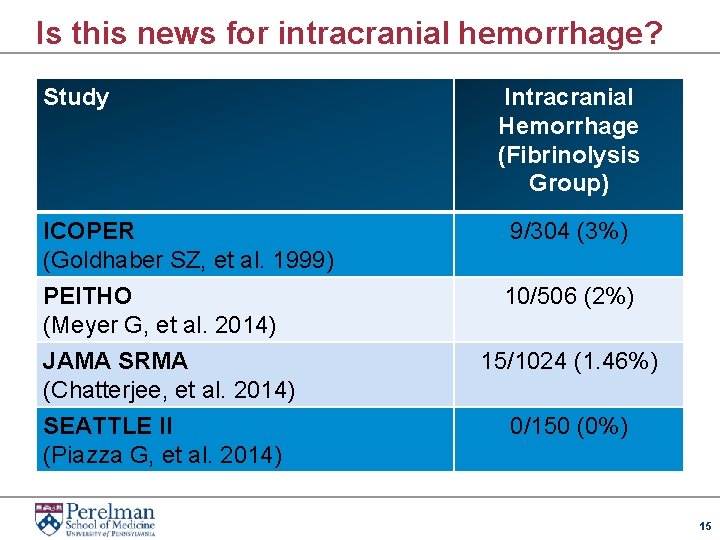
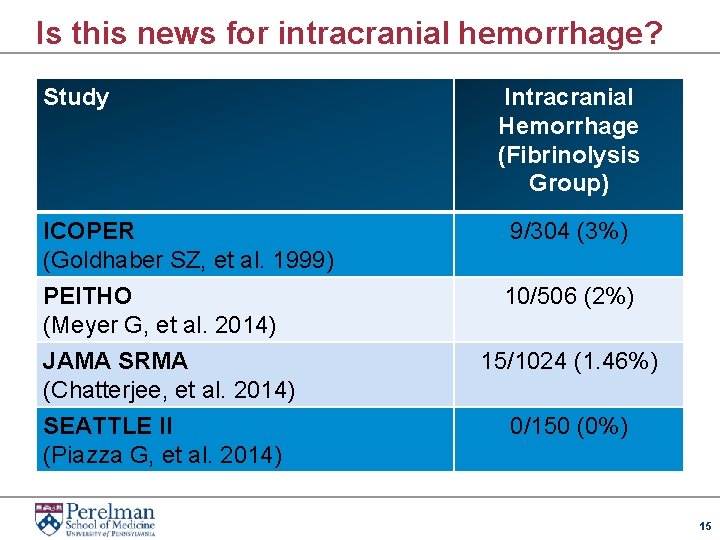
Is this news for intracranial hemorrhage? Study ICOPER (Goldhaber SZ, et al. 1999) PEITHO (Meyer G, et al. 2014) JAMA SRMA (Chatterjee, et al. 2014) SEATTLE II (Piazza G, et al. 2014) Intracranial Hemorrhage (Fibrinolysis Group) 9/304 (3%) 10/506 (2%) 15/1024 (1. 46%) 0/150 (0%) 15
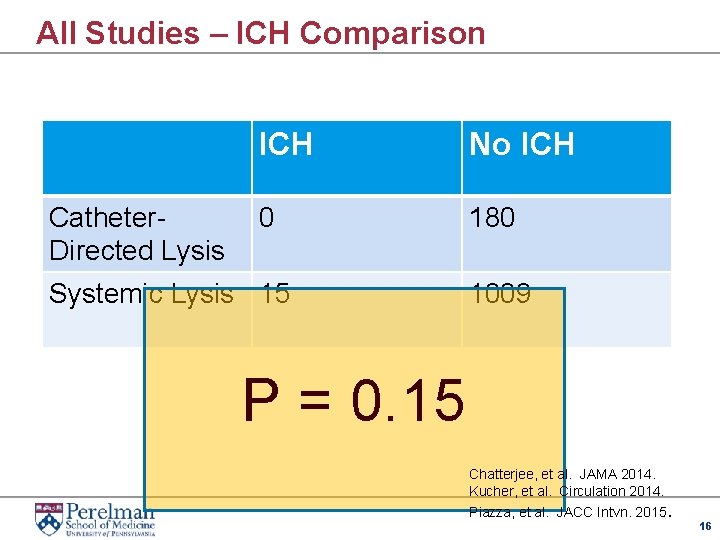
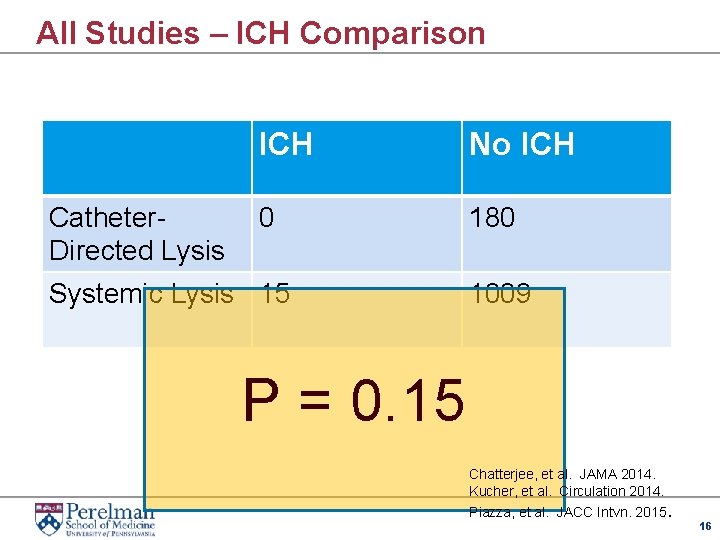
All Studies – ICH Comparison Catheter. Directed Lysis ICH No ICH 0 180 Systemic Lysis 15 1009 P = 0. 15 Chatterjee, et al. JAMA 2014. Kucher, et al. Circulation 2014. Piazza, et al. JACC Intvn. 2015. 16
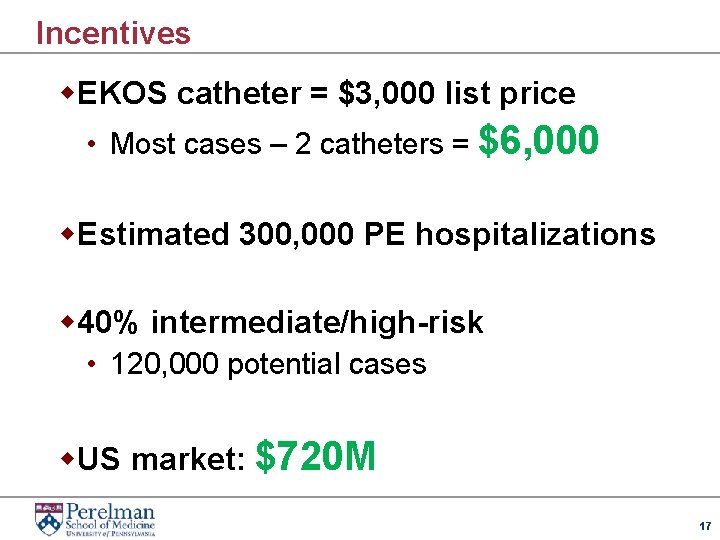
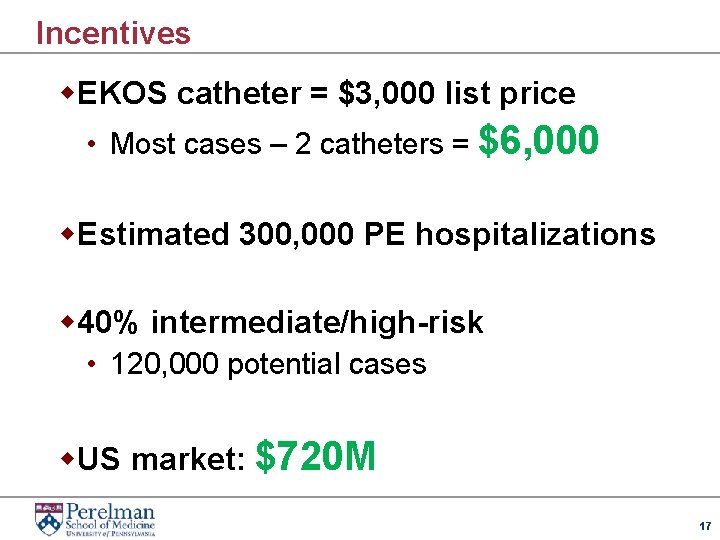
Incentives w. EKOS catheter = $3, 000 list price • Most cases – 2 catheters = $6, 000 w. Estimated 300, 000 PE hospitalizations w 40% intermediate/high-risk • 120, 000 potential cases w. US market: $720 M 17
Marketing 18
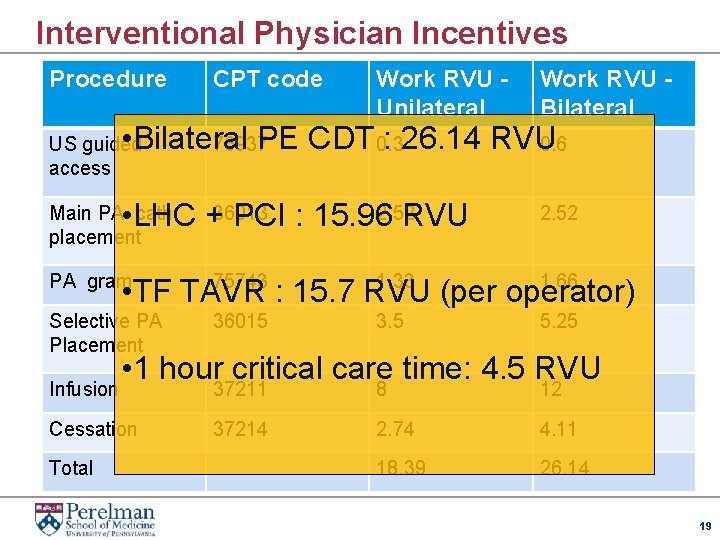
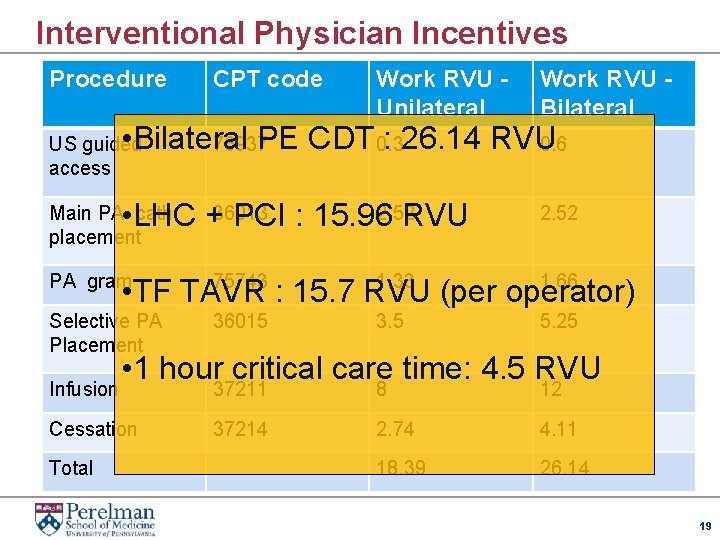
Interventional Physician Incentives Procedure CPT code Work RVU Unilateral Work RVU Bilateral • Bilateral PE CDT 0. 3 : 26. 14 RVU 76937 0. 6 US guided access 2. 52 • LHC +36013 PCI : 15. 96 RVU Main PA cath placement 2. 52 PA gram 75743 1. 33 1. 66 • TF TAVR : 15. 7 RVU (per operator) Selective PA Placement 36015 Infusion 37211 8 12 5. 25 37214 2. 74 4. 11 18. 39 26. 14 • 1 hour critical care time: 4. 5 RVU Cessation Total 3. 5 19
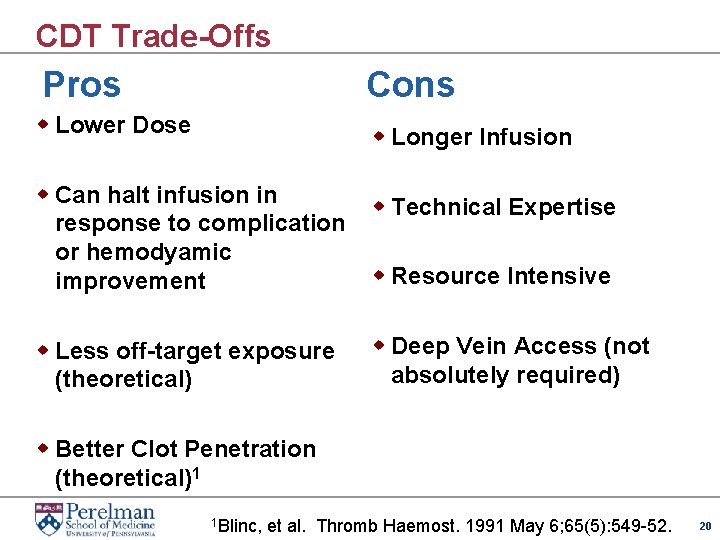
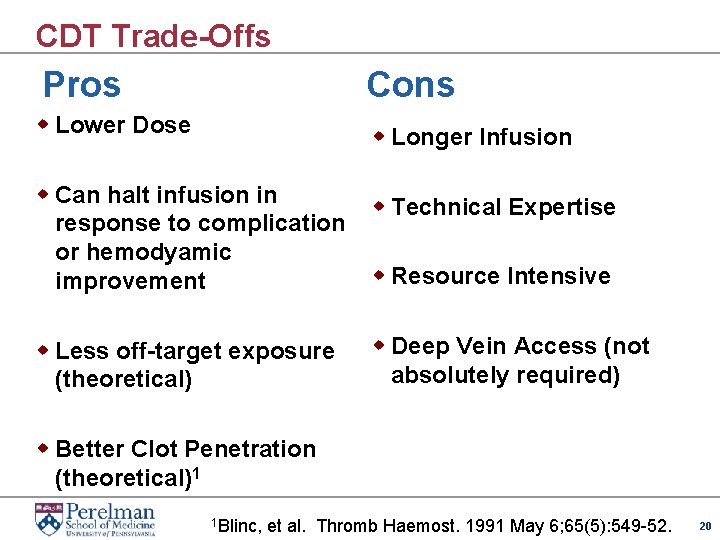
CDT Trade-Offs Pros Cons w Lower Dose w Longer Infusion w Can halt infusion in response to complication or hemodyamic improvement w Technical Expertise w Less off-target exposure (theoretical) w Deep Vein Access (not absolutely required) w Resource Intensive w Better Clot Penetration (theoretical)1 1 Blinc, et al. Thromb Haemost. 1991 May 6; 65(5): 549 -52. 20
CDT vs. USAT 21
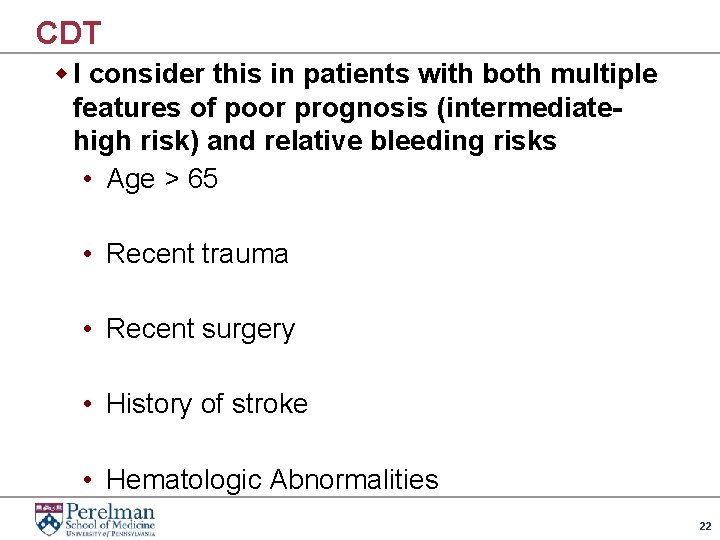
CDT w I consider this in patients with both multiple features of poor prognosis (intermediatehigh risk) and relative bleeding risks • Age > 65 • Recent trauma • Recent surgery • History of stroke • Hematologic Abnormalities 22
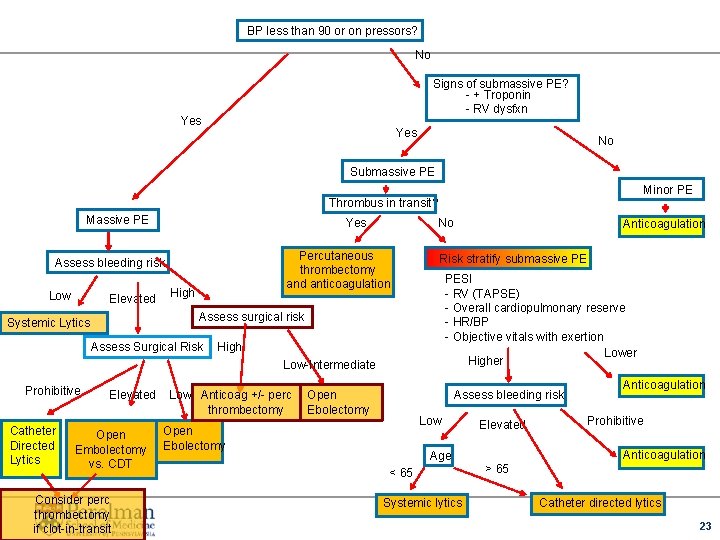
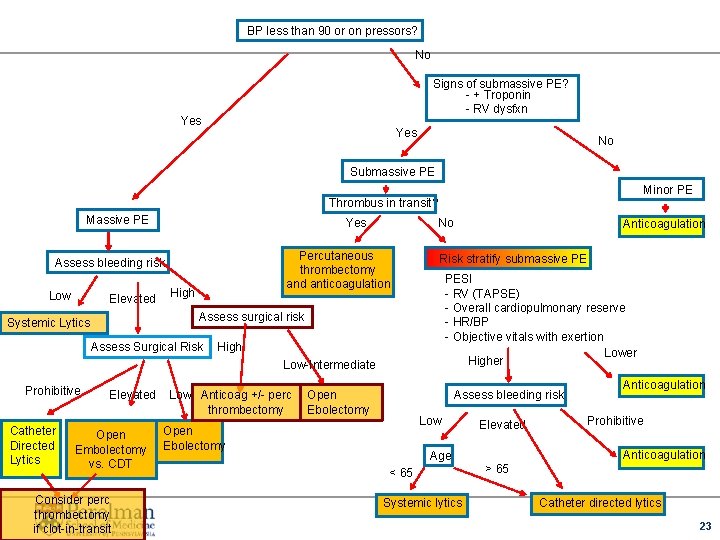
BP less than 90 or on pressors? No Signs of submassive PE? - + Troponin - RV dysfxn Yes No Submassive PE Minor PE Thrombus in transit? Massive PE Yes Percutaneous thrombectomy and anticoagulation Assess bleeding risk Low Elevated No High Risk stratify submassive PE PESI - RV (TAPSE) - Overall cardiopulmonary reserve - HR/BP - Objective vitals with exertion Lower Higher Assess surgical risk Systemic Lytics Assess Surgical Risk High Low-Intermediate Prohibitive Catheter Directed Lytics Elevated Open Embolectomy vs. CDT Consider perc thrombectomy if clot-in-transit Low Anticoag +/- perc thrombectomy Open Ebolectomy Anticoagulation Assess bleeding risk Low Open Ebolectomy Elevated Systemic lytics Prohibitive Anticoagulation Age < 65 Anticoagulation > 65 Catheter directed lytics 23
Thank You w Penn Pulmonary Embolism Response Team • • • Akaya Smith Jeremy Mazurek Barry Fuchs Prashanth Vallabhajosyula Nimesh Desai Deepak Sudheendra w PE Research Collaborators • • • Saurav Chatterjee Ido Weinberg Geoffrey Barnes, Chris Kabhrel Bram Geller Srinath Adusumalli 24
 M7rh5si5154 -site:youtube.com
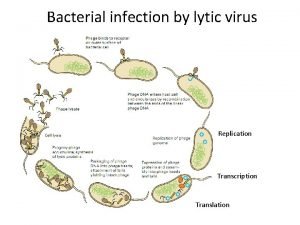
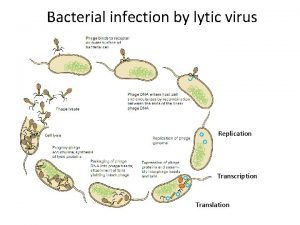
M7rh5si5154 -site:youtube.com Lytic and lysogenic cycle similarities
Lytic and lysogenic cycle similarities Difference between lytic and lysogenic cycle
Difference between lytic and lysogenic cycle Introduction of bacteria
Introduction of bacteria Lytic cycle comic strip
Lytic cycle comic strip Is the zika virus lytic or lysogenic
Is the zika virus lytic or lysogenic Lytic cycle
Lytic cycle Lytic catheter
Lytic catheter Why are viruses considered nonliving
Why are viruses considered nonliving Youtube . com / watch v = roxnvcaezjs
Youtube . com / watch v = roxnvcaezjs Watch?v=pnrscqkn3vw
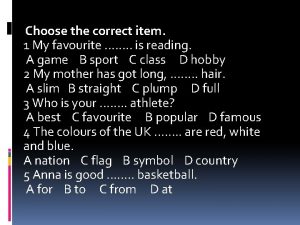
Watch?v=pnrscqkn3vw Choose the correct item look he has just
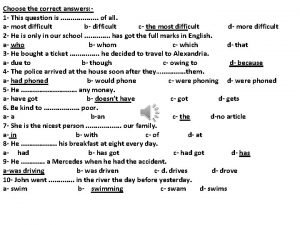
Choose the correct item look he has just 3.choose the correct answers
3.choose the correct answers Pancreatitis nursing
Pancreatitis nursing Give us your hungry your tired your poor
Give us your hungry your tired your poor Choose your hero
Choose your hero Choose your own adventure java
Choose your own adventure java Prevent child abuse nevada
Prevent child abuse nevada Choose your own assignment
Choose your own assignment Choosing foods wisely quiz
Choosing foods wisely quiz Choose your words carefully
Choose your words carefully Top management and middle management
Top management and middle management Top management middle management first line management
Top management middle management first line management Middle level management
Middle level management Name 2 objects with acute angles
Name 2 objects with acute angles